Abstract
Post-traumatic epilepsy accounts for 10–20 % of symptomatic epilepsy in the general population and 5 % of all epilepsy. During the last decade, an increasing number of laboratories have investigated the molecular and cellular mechanisms of post-traumatic epileptogenesis in experimental models. However, identification of critical molecular, cellular, and network mechanisms that would be specific for post-traumatic epileptogenesis remains a challenge. Despite of that, 7 of 9 proof-of-concept antiepileptogenesis studies have demonstrated some effect on seizure susceptibility after experimental traumatic brain injury, even though none of them has progressed to clinic. Moreover, there has been some promise that new clinically translatable imaging approaches can identify biomarkers for post-traumatic epileptogenesis. Even though the progress in combating post-traumatic epileptogenesis happens in small steps, recent discoveries kindle hope for identification of treatment strategies to prevent post-traumatic epilepsy in at-risk patients.
Electronic supplementary material
The online version of this article (doi:10.1007/s13311-014-0260-7) contains supplementary material, which is available to authorized users.
Keywords: Biomarker, Controlled cortical impact, Epileptogenesis, Epigenetics, Lateral fluid-percussion, Magnetic resonance imaging, microRNA, Traumatic brain injury
Introduction
Traumatic brain injury (TBI) refers to a brain injury caused by an external mechanical force such as a blow to the head, concussive forces, acceleration–deceleration forces, blast injury, or a projectile missile, such as a bullet [1]. TBI is recognized as a critical public health problem worldwide [1, 2]. According to the World Health Organization, TBI will surpass many other diseases as the major cause of death and disability by the year 2020 [3]. Though the problems experienced by those suffering TBI are often not visible (e.g., impairments in memory or cognition), the disease is often referred to as the “silent epidemic” [4].
TBI can be classified based on the injury mechanism [5]. Depending on the characteristics of the mechanical force (amplitude, duration, velocity, acceleration), injury can be static or dynamic. The severity of brain injury is commonly rated using the 15-point Glasgow Coma Scale (GCS), which assesses 3 major parameters: verbal, motor, and eye-opening reactions to stimuli [6]. In mild TBI, the GCS score is ≥13, in moderate TBI it is 9–12, and in severe TBI it is ≤8. Importantly, the same injury severity may represent different pathological and clinical endophenotypes that depend on the injury mechanism (e.g., static vs dynamic) or distribution and type of damage (e.g., gray vs white matter) (see [7]). In some endophenotypes, post-traumatic epilepsy (PTE) is a significant life-compromising component [8].
In this review we will summarize the concepts and mechanisms proposed to be associated with the development of PTE, existing animal data, and key questions that remain open.
From TBI to PTE
Process of Epileptogenesis in Humans
Epilepsy is a disorder of the brain characterized by an enduring predisposition to generate epileptic seizures, and by the neurobiological, cognitive, psychological, and social consequences of this condition. The definition of epilepsy requires the occurrence of at least one unprovoked seizure [9]. Depending on the time delay from the TBI to the occurrence of the first seizure, post-TBI seizures have been categorized into immediate (<24 h), early (1–7 days), or late seizures (>1 week after TBI) [8]. Thus, when TBI is associated with one unprovoked late seizure it qualifies for diagnosis of PTE.
PTE accounts for 10–20 % of symptomatic epilepsy in the general population and 5 % of all epilepsy [10, 11]. Based on epidemiologic studies on civilian or military populations, most of which were conducted before modern imaging era, the risk factors for PTE include old age, penetrating injuries, injury severity (GCS < 10), biparietal or multiple contusions, intracranial hemorrhage, frontal or temporal location of the lesion, >5 mm brain midline shift, duration of coma >24 h, loss of consciousness >24 h, prolonged length of post-traumatic amnesia, multiple intracranial procedures, and the occurrence of early post-traumatic seizures [10, 12–17]. Related to methodology, many of the identified risk factors directly or indirectly reflect the severity of brain injury, and strengthen the view that the risk for PTE increases with the severity of TBI.
The latency from the TBI to the occurrence of the first seizure can vary largely. Epidemiologic studies show that a 30-year cumulative incidence of epilepsy is 2.1 % for mild, 4.2 % for moderate, and 16.7 % for severe injuries [8, 18]. After the first late seizure, 86 % of patients have been reported to develop a second seizure within 2 years, suggesting the establishment of an epileptogenic process [19]. Moreover, the risk of developing epilepsy remains higher for a longer period of time after severe than moderate TBI (10 vs 30 years) [8]. Further, recent magnetoencephalography studies have revealed that some patients without reported seizures after mild TBI have epileptiform spikes when assessed at 12–140 months after TBI [20].
Information on genetic risk factors for outcome from TBI are emerging, but few studies have assessed the linkage of genes to PTE [21]. One study found that the ApoE4 allele is associated with a 2.4-fold increased risk of late post-traumatic seizures after moderate-to-severe TBI [22]. This was not, however, confirmed by another study [23, 24]. The study by Anderson et al. [24] also did not reveal any association between PTE and polymorphism in HP2-2. Wagner et al. [25] found two single nucleotide polymorphisms in the adenosine A1 receptor that were associated with later seizures in civilian population of patients with severe TBI. More recently, they reported that polymorphisms in the GAD1 gene (but not in GAD2) were associated with the occurrence of late post-traumatic seizures [26]. One study found an association between variation in a gene encoding methylenetetrahydrofolate reductase and the risk of PTE in a military population [27].
The detailed information about the endophenotypes of patients that associate with the highest risk of PTE would be of great value for attempts to model PTE in clinically relevant ways. Such information would also guide the search of mechanisms and biomarkers (or surrogate markers) for epileptogenesis.
Process of Epileptogenesis in Experimental Models
Data from several laboratories are now available to demonstrate that several models commonly used to investigate the molecular and cellular mechanisms of TBI have chronically lowered seizure threshold or even spontaneous seizures (Table 1). Chronically increased seizure susceptibility to chemoconvulsants or electroshock has been demonstrated in weight-drop, fluid-percussion (FP), controlled cortical impact (CCI), and closed skull models of TBI (Table 1). Chronic spontaneous seizures were reported after FP- and CCI-induced TBI, both in rats and mice. Acute epileptiform activity/seizures (up to 3 days after injury) has been reported in a rat model of penetrating ballistic injury [28–31] and blast injury [32], but whether late spontaneous seizures develop after these injury mechanisms remains to be studied. So far, studies have not found acute/late seizures after repeated mild concussive TBI [33]. We will next focus on models in which spontaneous seizures develop after TBI.
Table 1.
Summary of in vivo recorded changes in excitability in different models of traumatic brain injury. Only the data that were collected at least 1 week after injury are included
| Model | Species, age, strain, preparation | Seizure susceptibility in vivo | Epilepsy | Reference | ||||
|---|---|---|---|---|---|---|---|---|
| Animals with epilepsy (%) | Latency to spontaneous seizure | Seizure frequency | Seizure duration (s) | Epileptiform spiking or EDs in EEG | ||||
| Weight-drop (Feeney) | Rat, adult | increased susceptibility to PTZ-induced seizures, 15 weeks post-TBI | n.d. | n.d. | n.d. | n.d. | n.d. | [83] |
| Weight-drop (Marmarou) | Mouse, adult | Increased seizure susceptibility to ECS-induced seizures, 7 days post-TBI | n.d. | n.d. | n.d. | n.d. | n.d. | [71] |
| Central FPI | Rat, adult | No difference in PTZ-kindling, started 24 h post-TBI | n.d. | n.d. | n.d. | n.d. | n.d. | [51] |
| Parasagittal FPI | Rat, P32-35 | n.d. | 100 % (follow-up: 7 months) | ~2 weeks | Up to 7 seizures/h | Ictal episodes ≤10 s (up to 99 s) | n.d. | [37, 38, 75] |
| Rat, adult | Increased susceptibility to PTZ-induced seizures, 12 weeks post-TBI | n.d. | n.d. | n.d. | n.d. | n.d. | [74] | |
| Rat, adult | Increased susceptibility to PTZ-induced seizures, 2 weeks post-TBI | No | n.d. | n.d. | n.d. | n.d. | [50] | |
| Lateral FPI | Rat, adult | Granule cell hyperexcitability, 1 week post-TBI | n.d. | n.d. | n.d. | n.d. | n.d. | [84] |
| Rat, adult | Increased inhibition in dentate gyrus, 15 days post-TBI | n.d. | n.d. | n.d. | n.d. | n.d. | [85] | |
| Rat, P19 | No change in PTZ-seizure threshold, 20 weeks post-TBI | 0 % (behavioral observation) | n.d. | n.d. | n.d. | n.d. | [86] | |
| Rat, adult | Increased susceptibility to PTZ-induced seizures, 12 months post-TBI | 50 % (follow-up: 12 months) | 4–11 weeks | 0.3/day | 104 | 80 % | [36, 65] | |
| Rat, P21-22 | Increased susceptibility to kainate-induced seizures, 6 weeks post-TBI | n.d. | n.d. | n.d. | n.d. | n.d. | [70] | |
| Rat, adult | No change in susceptibility to fluorothyl-induced seizures, 3 and 6 weeks post-TBI | n.d. | n.d. | n.d. | n.d. | n.d. | [72] | |
| Mouse, adult | Increased susceptibility to PTZ-induced seizures, 6 months post-TBI | 6 % (follow-up: 9 months) | n.d. | 0.1/d | 91 | yes | [39] | |
| Rat, adult | n.d. | 52 % spontaneous seizures (30 %) or ED (22 %) | n.d. | 6.3/2 week | 53 | 11.5/2 week | [67] | |
| Mouse, adult | Increased susceptibility to PTZ-induced seizures, 30 days post-TBI | n.d. | n.d. | n.d. | n.d. | n.d. | [60] | |
| CCI | Rat, P16-18 | Unchanged threshold for tonic hindlimb extension or minimal clonic seizures in electroconvulsive seizure threshold test, testing on P34-40 | n.d. | n.d. | n.d. | n.d. | n.d. | [87] |
| Reduced threshold for minimal clonic seizures, testing on P60-63 | ||||||||
| Rat, P17 | n.d. | 1 of 8 (13 %) (follow-up: 11 months) | n.d. | n.d. | 45–60 s | 88 % had epileptiform spiking | [44] | |
| Mouse, adult | n.d. | 20 % (mild) – 36 % (severe injury ) | n.d. (monitoring 42–71 days post-TBI) | n.d | ~90 s (behavioral assessment) | n.d. | [41] | |
| Mouse, adult | n.d. | 40 % | 6.5 ± 1.3 weeks | n.d. | n.d. | n.d. | [42] | |
| Mouse, adult | Increased susceptibility to PTZ-induced seizures, 6 months post-TBI | 9 % (follow-up: 9 months) | n.d. | 0.2/day | 50 | Yes | [39] | |
| Mouse, adult | 50 % of vehicle* treated animals | 82.3 ± 10.2 days | 0.55 ± 0.16/day | 35.5 ± 2.8 | Rare | [43] | ||
ED = epileptiform discharges; EEG = electroencephalography; FPI = fluid-percussion injury; CCI = controlled cortical impact; PTZ = pentylenetetrazol; ECS = electroconvulsive shock; n.d. = no data
*Data from vehicle-treated mice that were included in rapamycin treatment study.
Epilepsy in the FP Model
Lateral FP-induced TBI produces both focal and diffuse (mixed) brain injury [34]. It reproduces several aspects of human TBI, including focal contusion, petechial intraparenchymal and subarachnoid hemorrhages, tissue tears, and traumatic axonal injury. The sequelae include blood–brain-barrier disruption, white matter damage, neuronal loss, gliosis, altered cerebral metabolism, altered cerebral blood flow, and altered brain electrical activity. The damage appears most severe in the ipsilateral cortex, hippocampus, and thalamus, but milder lesions can also be detected contralaterally. More chronic network alterations include neurogenesis with axonal and dendritic plasticity. The molecular and cellular changes can continue for weeks and months, and they associate with behavioral impairments and cognitive comorbidities [35].
Kharatishvili et al. [36] monitored adult Sprague–Dawley rats with lateral FP injury (FPI) over a period of 12 months with periodic 24/7 video electroencephalography (EEG), and demonstrated that 50 % of rats developed PTE. The seizures were partial or secondarily generalized, and lasted for about 60–110 s. A substantial proportion of animals had lowered seizure thresholds. These data have now been reproduced by several laboratories (Table 1). Rostral parasagittal FP was also reported to trigger epileptogenesis and the occurrence of spontaneous seizures [37, 38]. Data from several laboratories show that lateral FP can trigger increased seizure susceptibility, which can be detected after administration of pentylenetetrazol (PTZ) or kainate. Lateral FPI also triggers susceptibility to seizures induced by PTZ as well as spontaneous seizures in mice [39, 40].
Epilepsy in the CCI Model
CCI injury to the lateral cortex causes a focal brain injury that is associated with a spectrum of contusion injuries, including intraparenchymal petechial hemorrhages that are accompanied by epidural and subdural hematomas. Histologic analysis reveals widespread cortical gray matter damage, as well as axonal injury in the adjacent white matter, corpus callosum, and capsula interna. Degeneration is present not only in the cortex, but also in the hippocampus and thalamus.These anatomical changes associate with a spectrum of cognitive and motor deficits [34]. Recently, elegant studies from Hunt et al. [41, 42] demonstrated that CCI-induced TBI in the lateral cortex triggers the development of PTE in CD1 mice. Behavioral seizures were observed in 20 % of animals with mild injury and in 36 % with severe injury when observed 42–71 days after injury. Guo et al. [43] complemented these data by showing that up to 50 % of CD1 mice developed epilepsy by 4 months after CCI (impact depth = 2 mm) when continuously monitored by video-EEG. Our data show also increased susceptibility to PTZ-induced seizures and the occurrence of electrographic spontaneous seizures after lateral CCI injury in C57BL/6J mice [39]. Statler et al. [44] monitored rats with lateral CCI at postnatal day 17 with video-EEG over a period of 4–11 months after TBI. They reported that 88 % of rats developed epileptiform spiking, and 13 % of animals (1 of 8) had spontaneous recurrent seizures. Recently, Yang et al. [45] recorded spontaneous epileptiform activity in cortical slices that were taken from rats that had experienced CCI injury 14–16 days earlier at postnatal day 24.
Mechanisms of PTE
The aftermath of TBI consist of several phases, including primary injury, evolution of the primary injury, secondary injury, and regeneration [46, 47]. Primary injury occurs at the moment of TBI and is accompanied by massive disturbance of the cellular ion homeostasis, release of the excitatory neurotransmitters, and exacerbation of excitotoxicity. The secondary injury occurs in the hours and days after the primary injury, and is an indirect result of the insult. It includes a complex set of molecular changes and cellular processes, some of which may also be relevant to post-traumatic epileptogenesis. However, few reports have specifically linked the observed post-injury molecular changes with epileptogenesis. Further, little is known of whether the alterations contributing to epileptogenesis are separate or overlapping compared with those relevant to post-injury recovery [46, 48, 49]. For example, PTZ (30 mg/kg)-induced seizures in rats that had experienced lateral FPI 2 weeks earlier exacerbated cortical damage [50]. Another report, however, suggests that exposure of rats with moderate central FPI to PTZ kindling (once daily injections of 25 mg/kg) beginning at 24 h post-injury improved performance in the Morris water-maze when tested at 25–29 days after TBI [51].
Even though data from human PTE is meager, available studies show hippocampal neurodegeneration, as well as mossy fiber sprouting [52]. Approximately 53 % of patients with post-traumatic temporal lobe epilepsy have mesial temporal lobe sclerosis on magnetic resonance imaging (MRI). It is, however, important to note that it is not uncommon that TBI results in multifocal pathology [53, 54]. Moreover, Vespa et al. [55] suggest that hippocampal atrophy detected at the chronic post-injury phase could be caused by (prolonged) seizures at the acute post-TBI phase. Tomkins et al. [56] pointed out the possible role of BBB damage in PTE by showing that cortical BBB permeability was higher in TBI patients with epilepsy than those without, whereas the size of cortical lesion did not differ. Interestingly, a recent analysis of the resected pericontusional cortex demonstrated remarkable degeneration of subpopulations of inhibitory neurons, but no information was available about whether any of these patients developed epilepsy in follow-up [57, 58].
What are the molecular changes underlying circuitry reorganization during epileptogenesis? We recently conducted a meta-analysis of published gene array data after TBI and status epilepticus (SE) [59]. When the lists of genes regulated during post-TBI and post-SE epileptogenesis were compared, only 46 out of 624 regulated genes were found to have abnormal regulation in more than one study. Seventeen of 46 genes (40 %) were regulated in both SE and TBI models, indicating similarity in molecular events during epileptogenesis between different etiologies. The genes regulated by both SE and TBI were CALM3, CAMK2B, CTSB, CTSS, DBI, DNAJC3, DNAJC5, GABRD, GFAP, GRN, HPCA, IL6R, NPC2, NPTX2, PTPN6, S100B, and SPARC. One interesting subcategory of molecular reorganization is the development of various types of channelopathies, which, to date, have been demonstrated to affect both gamma aminobutyric acidA receptors and sodium and potassium channels (see [60]). Further studies are needed to reveal whether any of these genes form a target to combat post-traumatic epileptogenesis.
In addition to changes in transcription, post-translational modifications and epigenetic changes have been described after TBI (Table 2 and references therein). In most of the studies assessing histone modifications, DNA methylation, or microRNAs the analysis has been done within 72 h of TBI, and none of the reports has specifically addressed the contribution of changes to epileptogenesis. As only two studies have been conducted for human TBIs, the data available do not allow any comparisons of experimental and clinical findings.
Table 2.
Effect of traumatic brain injury (TBI) on histone modifications, DNA methylation, and levels of microRNAs (miRNA) in experimental models and in humans
| Model | Species | Tissue | Timing | Finding | Reference |
|---|---|---|---|---|---|
| Histone modification or DNA methylation | |||||
| CCI | Rat (P17) | HC | <72 h | H3 acetylation ⇩, H3 methylation ⇩ | [88] |
| Weight-drop | Rat | Cx | <96 h | Methylation ⇩ | [89] |
| Weight-drop | Rat | Cx | ≤14 days | Dnmt1 localization in astrocytes | [90] |
| CCI | Mouse | HC | ≥ 4 weeks | H3 acetylation +0 | [91] |
| CCI | Rat (P17) | HC | ≤14 days | Methylation of IGF-1B promoter ⇧ | [92] |
| Increase in H3 activation marks at promoter and exon 5 region of IGF-1B | |||||
| microRNAs | |||||
| Parasagittal FPI | Rat | Cx | <72 h | Altogether: 5⇩, 19⇧ | [93] |
| miR-21 ⇧ at all time points | |||||
| CCI | Rat | HC | 3 and 24 h | Altogether: 50⇩, 35⇧ (of 444) | [94] |
| 8 verified (signal transduction, transcriptional regulation, proliferation, differentiation) | |||||
| Severe TBI | Human (n = 47) | Plasma | ASAP | Altogether: 33⇩, 19⇧ (of 875) | [95] |
| 8 miRNAs in TBI only (miR-16, miR-92a, miR-765) | |||||
| CCI | Rat | HC | <15 days | miR-21 (enzyme-linked receptor signaling, transcriptional regulation, developmental processes) | [96] |
| Parasagittal FPI | Rat | Cx | <24 h | Altogether: 8⇩, 7⇧ (of 388) | [97] |
| Modified by therapeutic hypothermia | |||||
| Mild TBI | Human (n = 9) | PBMC | ? | 18 regulated (of 1500) | [98] |
| 3 diagnostic for mTBI | |||||
| Blast injury | Mouse | Cerebellum | 6 h | miR-132⇩ | [99] |
| cholinergic anti-inflammatory signaling | |||||
CCI = controlled cortical impact; FPI = fluid-percussion injury; HC = hippocampus; Cx = cortex; PBMC = peripheral blood mononuclear cells; ASAP = as soon as possible; Dnmt1 = DNA methyl transferase 1; IGF-1B = insulin-like growth factor 1B
Biomarkers for Epileptogenesis After Brain Injury
Currently, we have no biomarkers to identify patients at risk for PTE. Also, studies available on candidate biomarkers that can possibly be used to diagnose TBI and predict post-injury functional outcome provide no information on whether the TBI biomarkers could be used as PTE biomarkers [61, 62].
The most promising data related to biomarking epileptogenesis come from imaging studies. Long-term MRI studies have indicated that the progression of pathology has a different temporal course in the cortex, hippocampus, and thalamus [63, 64]. In addition to apparent neurodegeneration, long-term alterations include changes in axons/myelin, as well as in the vasculature [65, 66]. Importantly, not only epileptogenesis, but also the extent and temporal progression of neuropathologic changes, vary among animals [63].
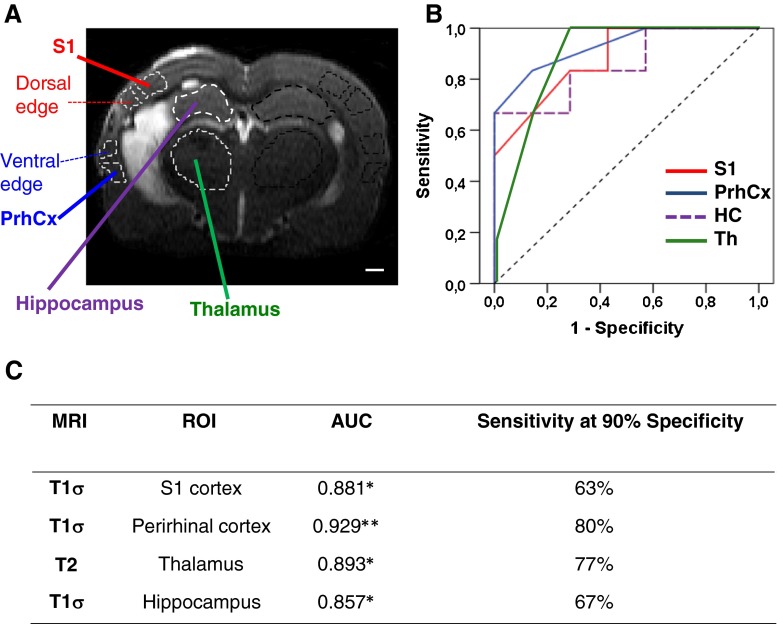
So far, correlations have been found between increased seizure susceptibility and diffusion changes or hypometabolism by arterial spin-labeling in MRI in the hippocampus [65, 66]. Recently, Schultz et al. [67] reported that abnormalities in the surface morphology of the ipsilateral hippocampus present at 1 week after lateral FPI predicted the occurrence of epilepsy 6 months after TBI [67]. We recently investigated whether quantitative T2, T1ρ, and diffusion (Dav) assessed with MRI at 9 days, 23 days, or 2 months after TBI in the peri-lesional cortex, thalamus, and hippocampus would predict seizure susceptibility in the PTZ test at 12 months after TBI [68]. Our data showed that the highest predictive value for the development of seizure susceptibility at 12 months post-TBI was achieved by co-assessment of the Dav in the peri-lesional cortex and the thalamus 2 months after TBI. Importantly, assessment of individual MRI parameters in the peri-lesional cortex or the thalamus at 9 days after TBI also provided high sensitivity and specificity for the prediction of increased seizure susceptibility at 12 months after TBI (Fig. 1).
Fig. 1.
(a) Coronal T2-weighted image from a rat with lateral fluid-percussion-induced TBI 23 days earlier, demonstrating the regions of interests (dashed lines), from which T2 and T1σ (c) were analyzed. (b) Receiver–operating characteristics for parameters in (c). Note that including data from the hippocampus (HC) for the calculation of the area under curve (AUC) did not increase sensitivity. (c) Summary of parameters with the highest sensitivity at 90 % specificity 9 days after TBI regarding prediction of seizure susceptibility 12 months after TBI. *P ≤ 0.05, **P ≤ 0.01 AUC compared with the area under diagonal line. For details, see [68]. PrhCx = perirhinal cortex; S1 = somatosensory cortex 1, Th=thalamus
Taken together, studies from different laboratories provide great hope that it will be possible to follow specific molecular or network changes related to epileptogenesis, and that the first applications of MRI biomarkers could become available for preclinical use.
Proof-of-Concept Antiepileptogenesis Studies After TBI
A large number of preclinical trials have been conducted to improve motor and cognitive recovery from TBI, but none of these studies has assessed seizure susceptibility or epilepsy as an outcome measure [59, 69]. Recently, however, 9 studies have made attempts to modify post-traumatic epileptogenesis in experimental models (Table 3). The first was the study conducted by Echegoyen et al. [70], who induced epileptogenesis by lateral FP-induced TBI, and administered the cannabinoid receptor 1 antagonist, SR141716A (Rimonabant) as a single injection 2 mins after injury. The threshold for kainate-induced seizures was assessed at 6 weeks after TBI. The TBI-associated reduction in the latency to kainate-induced seizures was prevented by SR141716A. Also, the total time spent in seizures after kainate administration was reduced in the SR141716A group compared with the vehicle group. Importantly, no positive effect of treatment was found if SR141716A was administered 20 mins after TBI.
Table 3.
Disease-modifying effects of different treatments after traumatic brain injury (TBI) in experimental models
| Drug | Mechanism | Model | Disease-modifying effect | Reference | |
|---|---|---|---|---|---|
| Antiepileptogenesis | Comorbidity modification* | ||||
| SR141716A | CB1 receptor antagonist | Lateral FPI-induced TBI in rats | Seizure susceptibility to kainate ⇩ | n.d. | [70] |
| Minozac | Reduction of pro-inflammatory cytokine production by activated glia | Closed skull TBI (CD1 mouse) | Seizure susceptibility to PTZ and electroshock ⇩ | Yes | [71] |
| Ketogenic diet | Multiple | Lateral FPI-induced TBI in rats | No effect on fluorothyl-induced seizures | n.d. | [72] |
| Hypothermia | Multiple | Parasagittal FPI-induced TBI in rats | Seizure susceptibility to PTZ ⇩ | n.d. | [74] |
| Focal passive cooling | Multiple | Parasagittal FPI-induced TBI in rats | Yes | n.d. | [75] |
| Creatine | Reduction of oxidative stress | Parasagittal FPI-induced TBI in rats | No effect on seizure susceptibility to PTZ | Yes | [76] |
| Ceftriaxone | Stimulation of glutamate transporter in astrocytes | Lateral FPI-induced TBI in rats | Yes | Yes | [78] |
| Rapamycin | mTOR inhibition | Controlled cortical impact in CD1 mice | Yes | Yes | [43] |
| Treadmill exercise | Reduction of oxidative stress | Parasagittal FPI-induced TBI in rats | Seizure susceptibility to PTZ ⇩ | Yes | [80] |
mTOR = mammalian target of rapamycin; FPI = fluid percussion injury; PTZ = pentylenetetrazol; n.d. = no data
*Included change in biochemical or structural pathology
Chrzaszcz et al. [71] used the closed-skull midline impact model of TBI in mice and administered minozac, a small molecule that suppressed the increased production of pro-inflammatory cytokines in glial cultures, at 3 or 6 h after injury. One week after TBI, minozac-treated mice showed less susceptibility to electroconvulsive shock-induced seizures than sham-operated rats. Whether minozac treatment prevents long-term increase in seizure susceptibility and the occurrence of late seizures remains to be explored.
Schwartzkroin et al. [72] triggered lateral FPI to 8-week-old rats and administered a ketogenic diet for 3 weeks after injury. Seizure susceptibility to flurothyl was no different from that in rats on a standard diet when assessed 3 and 6 weeks after discontinuation of the ketogenic diet. It should be noted, however, that TBI had no effect on seizure susceptibility to flurothyl (seizure threshold, seizure duration) when injured and sham-operated animals on a standard diet were compared.
Hypothermia is considered to be a promising therapy that improves structural and functional outcome measures after experimental and clinical TBI [73]. Atkins et al. [74] induced moderate parasagittal FPI in adult rats. Animals were kept under normothermic or moderate hypothermic temperatures for 4 h starting 30 mins after injury. Susceptibility to PTZ-induced seizures was tested 12 weeks after TBI. Behavioral analysis of data indicated a reduced number of induced seizures during the 60-min period after PTZ injection. The behavioral severity of seizures was not affected. Recently, D’Ambrosio et al. [75] started a 5.5-week focal passive cooling of the peri-lesional cortex 3 days after TBI, causing a 2 °C decrease in the temperature of the peri-lesional cortex. They found a remarkable reduction in the number and duration (from 9.1 s to 3.2 s) of electrographic ictal episodes (for a description, please see [75]), which lasted beyond the cooling treatment, that is, for >10 weeks after TBI [75].
Saraiva et al. [76] induced parasagittal FPI in adult Wistar rats. At 30 mins after TBI, they initiated a treatment with creatine (300 mg/kg, once per day, p.o.) for up to 4 or 7 days in order to reduce oxidative stress and gain neuroprotection. One day after the end of creatine administration (i.e., 4 or 8 days after TBI), a PTZ seizure susceptibility test was performed under EEG. The data obtained did not reveal any effect of creatine treatment on seizure susceptibility.
Ceftriaxone is a β-lactam antibiotic with good BBB penetration. It is a potent stimulator of glutamate transporter 1 expression in astrocytes [77]. Goodrich et al. [78] induced lateral FPI in adult Long–Evans rats and started cetriaxone treatment (200 mg/kg, once a day, i.p.) 30 mins after TBI for 7 days. At 12 weeks post-TBI, the occurrence of epileptiform activity was assessed using a 24-h EEG recording. They found a remarkable decrease in peri-lesional astrocytosis and restoration of the decreased post-TBI glutamate transporter 1 expression. The seizure frequency was lower in the ceftriaxone-treated animals than in controls (151 seizures/24 h vs 47 seizures/24 h). Also, seizure duration was shorter in the ceftriaxone group than in controls (from 22.7 s to 18.5 s).
Rapamycin, a mammalian target of rapamycin inhibitor, has shown disease-modifying effects in several genetic and acquired epilepsy models, even though there are also contradicting results (see [79]). Guo et al. [43] induced CCI in adult CD1 mice. Rapamycin treatment (6 mg/kg, once a day, i.p.) was started 60 mins after TBI and continued for 4 weeks. Mice were continuously monitored by video-EEG. Rapamycin reversed the hyperactivation of mTORC1 pathway, reduced neurodegeneration, and reduced the rate of development of PTE and decreased seizure frequency. However, it did not affect the latency to the occurrence of the first spontaneous seizure after TBI or seizure duration.
Silva et al. [80] investigated the effect of physical exercise on the development of epilepsy after TBI. Treadmill exercise (5 mins + 5 mins + 20 mins each day) was started 7 d after induction of parasagittal TBI in adult male Wistar rats, and continued for 4 weeks (5 days a week). A PTZ seizure susceptibility test performed 3 days after the end of the exercise period showed reduced seizure susceptibility. Histologic analysis of brain tissue did not reveal evidence of neuroprotection. However, favorable effects were observed on markers of oxidative stress.
Taken together, proof-of-concept studies in experimental models have shown that post-TBI seizure susceptibility can be modified by treatments affecting different targets, which is in line with the complexity of molecular and cellular changes underlying post-traumatic epileptogenesis. There are also several previous, recently completed, or new studies that aim to prevent epilepsy after TBI in humans ([81]; Table 4). Interestingly, however, there is no overlap between treatments applied in preclinical laboratories and in the clinic. The challenge is how to harmonize the antiepileptogenesis efforts made in laboratories and clinics to take favorable proof-of-concept studies to clinical practice. The roadmap prepared by the International League Against Epilepsy/American Epilepsy Society task force was recently provided to guide such efforts [82].
Table 4.
Summary of clinical trials including development of seizures after traumatic brain injury as primary or secondary outcome. Data were collected from www.clinicaltrials.gov
| Study | Identifier | Status | PTE |
|---|---|---|---|
| Seizure prophylaxis with lacosamide | NCT01110187 | Terminated | Secondary outcome |
| Levetiracetam to prevent PTE | NCT01463033 | Completed and reported [100–102] | Secondary outcome |
| Preventing epilepsy after TBI with topiramate | NCT00598923 | Unknown | Secondary outcome |
| Use of biperiden for the prevention of PTE | NCT01048138 | Not yet recruiting | Secondary outcome |
| Allopregnanolone for the treatment of TBI | NCT01673828 | Recruiting | Secondary outcome |
| Prevention of post-traumatic seizures with levetiracetam | NCT00566046 | Terminated | Secondary outcome |
| Effects of huperzine A in treatment of moderate-to-severe TBI | NCT01676311 | Not yet recruiting | Secondary outcome |
PTE = post-traumatic epilepsy; TBI = traumatic brain injury
Conclusions
Recent advances in model development provide a platform for studies that aim at a better understanding of the molecular and cellular mechanisms leading to PTE. Experimental imaging studies have offered encouraging results to maintain a spirit that discovery of biomarkers that can be used to predict and diagnose post-traumatic epileptogenesis is possible. Finally, several proof-of-concept studies have already had favorable results, suggesting that post-TBI seizure susceptibility can be modified. Even though the progress happens in small steps, prevention of PTE appears as a feasible goal.
Electronic supplementary material
(PDF 78kb)
Acknowledgement
This work was supported by the Academy of Finland, the Sigrid Juselius Foundation, and CURE (A.P.).
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
References
- 1.Maas AI, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008;8:728–741. doi: 10.1016/S1474-4422(08)70164-9. [DOI] [PubMed] [Google Scholar]
- 2.Hyder AA, Wunderlich CA, Puvanachandra P, Gururaj G, Kobusingye OC. The impact of traumatic brain injuries: a global perspective. NeuroRehabilitation. 2007;22:341–53. [PubMed] [Google Scholar]
- 3.World Health Organization. Projections of mortality and burden of disease to 2030: deaths by income group. Available at: http://www.who.int/healthinfo/global_burden_disease/en/
- 4.Langlois JA, Marr A, Mitchko J, Johnson RL. Tracking the silent epidemic and educating the public: CDC's traumatic brain injury-associated activities under the TBI Act of 1996 and the Children's Health Act of 2000. J Head Trauma Rehabil. 2005;20:196–204. doi: 10.1097/00001199-200505000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Graham DI, McIntoshTK, Maxwell WL, Nicoll JA. Recent advances in neurotrauma. J Neuropathol Exp Neurol 2000;59:641-651. [DOI] [PubMed]
- 6.Marion DW. Management of traumatic brain injury: past, present, and future. Clin Neurosurg. 1999;45:184–191. [PubMed] [Google Scholar]
- 7.Saatman KE, Duhaime AC, Bullock R, Maas AI, Valadka A, Manley GT. Workshop Scientific Team and Advisory Panel Members. Classification of traumatic brain injury for targeted therapies. J Neurotrauma. 2008;25:719–738. doi: 10.1089/neu.2008.0586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Annegers JF, Hauser A, Coan SP, Rocca WA. A population-based study of seizures after traumatic brain injuries. N Engl J Med. 1998;338:20–24. doi: 10.1056/NEJM199801013380104. [DOI] [PubMed] [Google Scholar]
- 9.Fisher RS, van Emde Boas W, Blume W, et al. Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE) Epilepsia. 2005;46:470–472. doi: 10.1111/j.0013-9580.2005.66104.x. [DOI] [PubMed] [Google Scholar]
- 10.Herman ST. Epilepsy after brain insult: targeting epileptogenesis. Neurology. 2002;59:21–26. doi: 10.1212/WNL.59.9_suppl_5.S21. [DOI] [PubMed] [Google Scholar]
- 11.Frey LC. Epidemiology of posttraumatic epilepsy: a critical review. Epilepsia. 2003;10:11–17. doi: 10.1046/j.1528-1157.44.s10.4.x. [DOI] [PubMed] [Google Scholar]
- 12.Brandvold B, Levi L, Feinsod M, George ED. Penetrating craniocerebral injuries in the Israeli involvement in the Lebanese conflict, 1982-1985. Analysis of a less aggressive surgical approach. J Neurosurg. 1990;72:15–21. doi: 10.3171/jns.1990.72.1.0015. [DOI] [PubMed] [Google Scholar]
- 13.Asikainen I, Kaste M, Sarna S. Early and late posttraumatic seizures in traumatic brain injury rehabilitation patients: brain injury factors causing late seizures and influence of seizures on long-term outcome. Epilepsia. 1999;40:584–589. doi: 10.1111/j.1528-1157.1999.tb05560.x. [DOI] [PubMed] [Google Scholar]
- 14.Englander J, Bushnik T, Duong TT, et al. Analyzing risk factors for late posttraumatic seizures: a prospective, multicenter investigation. Arch Phys Med Rehabil. 2003;84:365–373. doi: 10.1053/apmr.2003.50022. [DOI] [PubMed] [Google Scholar]
- 15.Messori A, Polonara G, Carle F, Gesuita R, Salvolini U. Predicting posttraumatic epilepsy with MRI: prospective longitudinal morphologic study in adults. Epilepsia. 2005;46:1472–1481. doi: 10.1111/j.1528-1167.2005.34004.x. [DOI] [PubMed] [Google Scholar]
- 16.Skandsen T, Ivar Lund T, Fredriksli O, Vik A. Global outcome, productivity and epilepsy 3–8 years after severe head injury. The impact of injury severity. Clin Rehabil. 2008;22:653–662. doi: 10.1177/0269215508089067. [DOI] [PubMed] [Google Scholar]
- 17.Scheid R, von Cramon DY. Clinical findings in the chronic phase of traumatic brain injury: data from 12 years’ experience in the Cognitive Neurology Outpatient Clinic at the University of Leipzig. Dtsch Arztebl Int. 2010;107:199–205. doi: 10.3238/arztebl.2010.0199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Annegers JF, Grabow JD, Groover RV, Laws ER, Jr, Elveback LR, Kurland LT. Seizures after head trauma: a population study. Neurology. 1980;30:683–689. doi: 10.1212/WNL.30.7.683. [DOI] [PubMed] [Google Scholar]
- 19.Haltiner AM, Temkin NR, Dikmen SS. Risk of seizure recurrence after the first late posttraumatic seizure. Arch Phys Med Rehabil. 1997;78:835–840. doi: 10.1016/S0003-9993(97)90196-9. [DOI] [PubMed] [Google Scholar]
- 20.Lewine JD, Davis JT, Bigler ED, et al. Objective documentation of traumatic brain injury subsequent to mild head trauma: multimodal brain imaging with MEG, SPECT, and MRI. J Head Trauma Rehabil. 2007;22:141–155. doi: 10.1097/01.HTR.0000271115.29954.27. [DOI] [PubMed] [Google Scholar]
- 21.Dardiotis E, Fountas KN, Dardioti M, et al. Genetic association studies in patients with traumatic brain injury. Neurosurg Focus. 2010;28:E9. doi: 10.3171/2009.10.FOCUS09215. [DOI] [PubMed] [Google Scholar]
- 22.Diaz-Arrastia R, Gong Y, Fair S, et al. Increased risk of late posttraumatic seizures associated with inheritance of APOE epsilon4 allele. Arch Neurol. 2003;60:818–822. doi: 10.1001/archneur.60.6.818. [DOI] [PubMed] [Google Scholar]
- 23.Miller MA, Conley Y, Scanlon JM, et al. APOE genetic associations with seizure development after severe traumatic brain injury. Brain Inj. 2010;24:1468–1477. doi: 10.3109/02699052.2010.520299. [DOI] [PubMed] [Google Scholar]
- 24.Anderson GD, Temkin NR, Dikmen SS, et al. Haptoglobin phenotype and apolipoprotein E polymorphism: relationship to posttraumatic seizures and neuropsychological functioning after traumatic brain injury. Epilepsy Behav. 2009;16:501–506. doi: 10.1016/j.yebeh.2009.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wagner AK, Miller MA, Scanlon J, Ren D, Kochanek PM, Conley YP. Adenosine A1 receptor gene variants associated with post-traumatic seizures after severe TBI. Epilepsy Res. 2010;90:259–272. doi: 10.1016/j.eplepsyres.2010.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Darrah SD, Miller MA, Ren D, et al. Genetic variability in glutamic acid decarboxylase genes: associations with post-traumatic seizures after severe TBI. Epilepsy Res. 2013;103:180–194. doi: 10.1016/j.eplepsyres.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scher AI, Wu H, Tsao JW, et al. MTHFR C677T genotype as a risk factor for epilepsy including post-traumatic epilepsy in a representative military cohort. J Neurotrauma. 2011;28:1739–1745. doi: 10.1089/neu.2011.1982. [DOI] [PubMed] [Google Scholar]
- 28.Williams AJ, Hartings JA, Lu XC, Rolli ML, Dave JR, Tortella FC. Characterization of a new rat model of penetrating ballistic brain injury. J Neurotrauma. 2005;22:313–331. doi: 10.1089/neu.2005.22.313. [DOI] [PubMed] [Google Scholar]
- 29.Lu XC, Hartings JA, Si Y, Balbir A, Cao Y, Tortella FC. Electrocortical pathology in a rat model of penetrating ballistic-like brain injury. J Neurotrauma. 2011;28:71–83. doi: 10.1089/neu.2010.1471. [DOI] [PubMed] [Google Scholar]
- 30.Lu XC, Mountney A, Chen Z, et al. Similarities and differences of acute nonconvulsive seizures and other epileptic activities following penetrating and ischemic brain injuries in rats. J Neurotrauma. 2013;30:580–590. doi: 10.1089/neu.2012.2641. [DOI] [PubMed] [Google Scholar]
- 31.Mountney A, Shear DA, Potter B, et al. Ethosuximide and phenytoin dose-dependently attenuate acute nonconvulsive seizures after traumatic brain injury in rats. J Neurotrauma. 2013;30:1973–1982. doi: 10.1089/neu.2013.3001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cheng J, Gu J, Ma Y, et al. Development of a rat model for studying blast-induced traumatic brain injury. J Neurol Sci. 2010;294:23–28. doi: 10.1016/j.jns.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 33.Kane MJ, Angoa-Pérez M, Briggs DI, Viano DC, Kreipke CW, Kuhn DM. A mouse model of human repetitive mild traumatic brain injury. J Neurosci Methods. 2012;203:41–49. doi: 10.1016/j.jneumeth.2011.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thompson HJ, Lifshitz J, Marklund N, et al. Lateral fluid percussion brain injury: a 15-year review and evaluation. J Neurotrauma. 2005;22:42–75. doi: 10.1089/neu.2005.22.42. [DOI] [PubMed] [Google Scholar]
- 35.Kharatishvili I, Pitkänen A. Posttraumatic epilepsy. Curr Opin Neurol. 2010;23:183–188. doi: 10.1097/WCO.0b013e32833749e4. [DOI] [PubMed] [Google Scholar]
- 36.Kharatishvili I, Nissinen JP, McIntosh TK, Pitkänen A. A model of posttraumatic epilepsy induced by lateral fluid-percussion brain injury in rats. Neuroscience. 2006;140:685–697. doi: 10.1016/j.neuroscience.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 37.D'Ambrosio R, Fairbanks JP, Fender JS, Born DE, Doyle DL, Miller JW. Post-traumatic epilepsy following fluid percussion injury in the rat. Brain. 2004;127:304–314. doi: 10.1093/brain/awh038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.D'Ambrosio R, Fender JS, Fairbanks JP, et al. Progression from frontal-parietal to mesial-temporal epilepsy after fluid percussion injury in the rat. Brain. 2005;128:174–188. doi: 10.1093/brain/awh337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bolkvadze T, Pitkänen A. Development of post-traumatic epilepsy after controlled cortical impact and lateral fluid-percussion-induced brain injury in the mouse. J Neurotrauma. 2012;29:789–812. doi: 10.1089/neu.2011.1954. [DOI] [PubMed] [Google Scholar]
- 40.Mukherjee S, Zeitouni S, Cavarsan CF, Shapiro LA. Increased seizure susceptibility in mice 30 days after fluid percussion injury. Front Neurol 2013;4:28. [DOI] [PMC free article] [PubMed]
- 41.Hunt RF, Scheff SW, Smith BN. Posttraumatic epilepsy after controlled cortical impact injury in mice. Exp Neurol. 2009;215:243–252. doi: 10.1016/j.expneurol.2008.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hunt RF, Scheff SW, Smith BN. Regionally localized recurrent excitation in the dentate gyrus of a cortical contusion model of posttraumatic epilepsy. J Neurophysiol. 2010;103:1490–1500. doi: 10.1152/jn.00957.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guo D, Zeng L, Brody DL, Wong M. Rapamycin attenuates the development of posttraumatic epilepsy in a mouse model of traumatic brain injury. PLoS One. 2013;8:e64078. doi: 10.1371/journal.pone.0064078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Statler KD, Scheerlinck P, Pouliot W, Hamilton M, White HS, Dudek FE. A potential model of pediatric posttraumatic epilepsy. Epilepsy Res. 2009;86:221–223. doi: 10.1016/j.eplepsyres.2009.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yang L, Afroz S, Michelson HB, Goodman JH, Valsamis HA, Ling DS. Spontaneous epileptiform activity in rat neocortex after controlled cortical impact injury. J Neurotrauma. 2010;27:1541–1548. doi: 10.1089/neu.2009.1244. [DOI] [PubMed] [Google Scholar]
- 46.Pitkänen A, McIntosh TK. Animal models of post-traumatic epilepsy. J Neurotrauma. 2006;23:241–61. doi: 10.1089/neu.2006.23.241. [DOI] [PubMed] [Google Scholar]
- 47.Pitkänen A, Bolkvadze T. Head trauma and epilepsy. In: Noebels JL, Avoli M, Rogawski MA, Olsen RW, Delgado-Escueta AV (eds) Jasper's basic mechanisms of the epilepsies. 4th edition. Bethesda,MD, National Center for Biotechnology Information, 2012;331–342. Available at http://www.ncbi.nlm.nih.gov/books/NBK98197/ [PubMed]
- 48.Pitkänen A, Lukasiuk K. Molecular and cellular basis of epileptogenesis in symptomatic epilepsy. Epilepsy Behav. 2009;1:16–25. doi: 10.1016/j.yebeh.2008.09.023. [DOI] [PubMed] [Google Scholar]
- 49.Hunt RF, Boychuk JA, Smith BN. Neural circuit mechanisms of post-traumatic epilepsy. Front Cell Neurosci. 2013;7:89. doi: 10.3389/fncel.2013.00089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bao YH, Bramlett HM, Atkins CM, et al. Post-traumatic seizures exacerbates histopathological damage after fluid-percussion brain injury. J Neurotrauma. 2011;28:35–42. doi: 10.1089/neu.2010.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hamm RJ, Pike BR, Temple MD, O'Dell DM, Lyeth BG. The effect of postinjury kindled seizures on cognitive performance of traumatically brain-injured rats. Exp Neurol. 1995;36:143–148. doi: 10.1006/exnr.1995.1091. [DOI] [PubMed] [Google Scholar]
- 52.Swartz BE, Houser CR, Tomiyasu U, et al. Hippocampal cell loss in posttraumatic human epilepsy. Epilepsia. 2006;47:1373–1382. doi: 10.1111/j.1528-1167.2006.00602.x. [DOI] [PubMed] [Google Scholar]
- 53.Hudak AM, Trivedi K, Harper CR, et al. Evaluation of seizure-like episodes in survivors of moderate and severe traumatic brain injury. J Head Trauma Rehabil. 2004;19:290–295. doi: 10.1097/00001199-200407000-00003. [DOI] [PubMed] [Google Scholar]
- 54.Diaz-Arrastia R, Agostini MA, Frol AB, et al. Neurophysiologic and neuroradiologic features of intractable epilepsy after traumatic brain injury in adults. Arch Neurol. 2000;57:1611–1616. doi: 10.1001/archneur.57.11.1611. [DOI] [PubMed] [Google Scholar]
- 55.Vespa PM, McArthur DL, Xu Y, et al. Nonconvulsive seizures after traumatic brain injury are associated with hippocampal atrophy. Neurology. 2010;75:792–798. doi: 10.1212/WNL.0b013e3181f07334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tomkins O, Shelef I, Kaizerman I, et al. Blood-brain barrier disruption in post-traumatic epilepsy. J Neurol Neurosurg Psychiatry. 2008;79:774–777. doi: 10.1136/jnnp.2007.126425. [DOI] [PubMed] [Google Scholar]
- 57.Buriticá E, Villamil L, Guzmán F, Escobar MI, García-Cairasco N, Pimienta HJ. Changes in calcium-binding protein expression in human cortical contusion tissue. J Neurotrauma. 2009;26:2145–2155. doi: 10.1089/neu.2009.0894. [DOI] [PubMed] [Google Scholar]
- 58.Riascos D, Buriticá E, Jiménez E, et al. Neurodegenerative diversity in human cortical contusion: Histological analysis of tissue derived from decompressive craniectomy. Brain Res. 2013;1537:86–99. doi: 10.1016/j.brainres.2013.09.016. [DOI] [PubMed] [Google Scholar]
- 59.Pitkänen A, Lukasiuk K. Mechanisms of epileptogenesis and potential treatment targets. Lancet Neurol. 2011;10:173–186. doi: 10.1016/S1474-4422(10)70310-0. [DOI] [PubMed] [Google Scholar]
- 60.Pitkänen A, Bolkvadze T, Immonen R. Anti-epileptogenesis in rodent post-traumatic epilepsy models. Neurosci Lett. 2011;497:163–171. doi: 10.1016/j.neulet.2011.02.033. [DOI] [PubMed] [Google Scholar]
- 61.Dash PK, Zhao J, Hergenroeder G, Moore AN. Biomarkers for the diagnosis, prognosis, and evaluation of treatment efficacy for traumatic brain injury. Neurotherapeutics. 2010;7:100–114. doi: 10.1016/j.nurt.2009.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kou Z, Wu Z, Tong KA, Holshouser B, Benson RR, Hu J, Haacke EM. The role of advanced MR imaging findings as biomarkers of traumatic brain injury. J Head Trauma Rehabil. 2010;25:267–282. doi: 10.1097/HTR.0b013e3181e54793. [DOI] [PubMed] [Google Scholar]
- 63.Immonen RJ, Kharatishvili I, Gröhn H, Pitkänen A, Gröhn OH. Quantitative MRI predicts long-term structural and functional outcome after experimental traumatic brain injury. Neuroimage. 2009;45:1–9. doi: 10.1016/j.neuroimage.2008.11.022. [DOI] [PubMed] [Google Scholar]
- 64.Liu YR, Cardamone L, Hogan RE, et al. Progressive metabolic and structural cerebral perturbations after traumatic brain injury: an in vivo imaging study in the rat. J Nucl Med. 2010;51:1788–1795. doi: 10.2967/jnumed.110.078626. [DOI] [PubMed] [Google Scholar]
- 65.Kharatishvili I, Immonen R, Gröhn O, Pitkänen A. Quantitative diffusion MRI of hippocampus as a surrogate marker for post-traumatic epileptogenesis. Brain. 2007;130:3155–3168. doi: 10.1093/brain/awm268. [DOI] [PubMed] [Google Scholar]
- 66.Hayward NM, Immonen R, Tuunanen PI, Ndode-Ekane XE, Gröhn O, Pitkänen A. Association of chronic vascular changes with functional outcome after traumatic brain injury in rats. J Neurotrauma. 2010;27:2203–2219. doi: 10.1089/neu.2010.1448. [DOI] [PubMed] [Google Scholar]
- 67.Schultz SR, Cardamone L, Liu YR, et al. Can structural or functional changes following traumatic brain injury in the rat predict epileptic outcome? Epilepsia. 2013;54:1240–1250. doi: 10.1111/epi.12223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Immonen R, Kharatishvili I, Gröhn O, Pitkänen A. MRI biomarkers for post-traumatic epileptogenesis. J Neurotrauma. 2013;30:1305–1309. doi: 10.1089/neu.2012.2815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pitkänen A. Therapeutic approaches to epileptogenesis--hope on the horizon. Epilepsia2010;51(Suppl. 3):2-17. [DOI] [PMC free article] [PubMed]
- 70.Echegoyen J, Armstrong C, Morgan RJ, Soltesz I. Single application of a CB1 receptor antagonist rapidly following head injury prevents long-term hyperexcitability in a rat model. Epilepsy Res. 2009;85:123–127. doi: 10.1016/j.eplepsyres.2009.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chrzaszcz M, Venkatesan C, Dragisic T, Watterson DM, Wainwright MS. Minozac treatment prevents increased seizure susceptibility in a mouse “two-hit” model of closed skull traumatic brain injury and electroconvulsive shock-induced seizures. J Neurotrauma. 2010;27:1283–1295. doi: 10.1089/neu.2009.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Schwartzkroin PA, Wenzel HJ, Lyeth BG, et al. Does ketogenic diet alter seizure sensitivity and cell loss following fluid percussion injury? Epilepsy Res. 2010;92:74–84. doi: 10.1016/j.eplepsyres.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 73.Dietrich WD, Bramlett HM. The evidence for hypothermia as a neuroprotectant in traumatic brain injury. Neurotherapeutics. 2010;7:43–50. doi: 10.1016/j.nurt.2009.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Atkins CM, Truettner JS, Lotocki G, et al. Post-traumatic seizure susceptibility is attenuated by hypothermia therapy. Eur J Neurosci. 2010;32:1912–1920. doi: 10.1111/j.1460-9568.2010.07467.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.D'Ambrosio R, Eastman CL, Darvas F, et al. Mild passive focal cooling prevents epileptic seizures after head injury in rats. Ann Neurol. 2013;73:199–209. doi: 10.1002/ana.23764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Saraiva AL, Ferreira AP, Silva LF, et al. Creatine reduces oxidative stress markers but does not protect against seizure susceptibility after severe traumatic brain injury. Brain Res Bull. 2012;87:180–186. doi: 10.1016/j.brainresbull.2011.10.010. [DOI] [PubMed] [Google Scholar]
- 77.Lee SG, Su ZZ, Emdad L, et al. Mechanism of ceftriaxone induction of excitatory amino acid transporter-2 expression and glutamate uptake in primary human astrocytes. J Biol Chem. 2008;283:13116–13123. doi: 10.1074/jbc.M707697200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Goodrich GS, Kabakov AY, Hameed MQ, Dhamne SC, Rosenberg PA, Rotenberg A. Ceftriaxone treatment after traumatic brain injury restores expression of the glutamate transporter, GLT-1, reduces regional gliosis, and reduces post-traumatic seizures in the rat. J Neurotrauma. 2013;30:1434–1441. doi: 10.1089/neu.2012.2712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pitkänen A, Engel J Jr. Past and present definitions of epileptogenesis and its biomarkers. Neurotherapeutics 2014. doi:10.1007/s13311-014-0257-2. [DOI] [PMC free article] [PubMed]
- 80.Silva LF, Hoffmann MS, Gerbatin Rda R, et al. Treadmill exercise protects against pentylenetetrazol-induced seizures and oxidative stress after traumatic brain injury. J Neurotrauma. 2013;30:1278–1287. doi: 10.1089/neu.2012.2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Temkin NR. Preventing and treating posttraumatic seizures: the human experience. Epilepsia. 2009;50:10–13. doi: 10.1111/j.1528-1167.2008.02005.x. [DOI] [PubMed] [Google Scholar]
- 82.Pitkänen A, Nehlig A, Brooks-Kayal AR, et al. Issues related to development of antiepileptogenic therapies. Epilepsia. 2013;54:35–43. doi: 10.1111/epi.12297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Golarai G, Greenwood AC, Feeney DM, Connor JA. Physiological and structural evidence for hippocampal involvement in persistent seizure susceptibility after traumatic brain injury. J Neurosci. 2001;21:8523–8537. doi: 10.1523/JNEUROSCI.21-21-08523.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lowenstein DH, Thomas MJ, Smith DH, McIntosh TK. Selective vulnerability of dentate hilar neurons following traumatic brain injury: a potential mechanistic link between head trauma and disorders of the hippocampus. J Neurosci. 1992;12:4846–4853. doi: 10.1523/JNEUROSCI.12-12-04846.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Reeves TM, Lyeth BG, Phillips LL, Hamm RJ, Povlishock JT. The effects of traumatic brain injury on inhibition in the hippocampus and dentate gyrus. Brain Res. 1997;757:119–132. doi: 10.1016/S0006-8993(97)00170-4. [DOI] [PubMed] [Google Scholar]
- 86.Gurkoff GG, Giza CC, Shin D, Auvin S, Sankar R, Hovda DA. Acute neuroprotection to pilocarpine-induced seizures is not sustained after traumatic brain injury in the developing rat. Neuroscience. 2009;164:862–876. doi: 10.1016/j.neuroscience.2009.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Statler KD, Swank S, Abildskov T, Bigler ED, White HS. Traumatic brain injury during development reduces minimal clonic seizure thresholds at maturity. Epilepsy Res. 2008;80:163–170. doi: 10.1016/j.eplepsyres.2008.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gao WM, Chadha MS, Kline AE, et al. Immunohistochemical analysis of histone H3 acetylation and methylation—evidence for altered epigenetic signaling following traumatic brain injury in immature rats. Brain Res. 2006;1070:31–34. doi: 10.1016/j.brainres.2005.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zhang ZY, Zhang Z, Fauser U, Schluesener HJ. Global hypomethylation defines a sub-population of reactive microglia/macrophages in experimental traumatic brain injury. Neurosci Lett. 2007;429:1–6. doi: 10.1016/j.neulet.2007.09.061. [DOI] [PubMed] [Google Scholar]
- 90.Lundberg J, Karimi M, von Gertten C, Holmin S, Ekström TJ, Sandberg-Nordqvist AC. Traumatic brain injury induces relocalization of DNA-methyltransferase. Neurosci Lett. 2009;457:8–11. doi: 10.1016/j.neulet.2009.03.105. [DOI] [PubMed] [Google Scholar]
- 91.Wang Y, Neumann M, Hansen K, et al. Fluoxetine increases hippocampal neurogenesis and induces epigenetic factors but does not improve functional recovery after traumatic brain injury. J Neurotrauma. 2011;28:259–268. doi: 10.1089/neu.2010.1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Schober ME, Ke X, Xing B, et al. Traumatic brain injury increased IGF-1B mRNA and altered IGF-1 exon 5 and promoter region epigenetic characteristics in the rat pup hippocampus. J Neurotrauma. 2012;29:2075–2085. doi: 10.1089/neu.2011.2276. [DOI] [PubMed] [Google Scholar]
- 93.Lei P, Li Y, Chen X, Yang S, Zhang J. Microarray based analysis of microRNA expression in rat cerebral cortex after traumatic brain injury. Brain Res. 2009;1284:191–201. doi: 10.1016/j.brainres.2009.05.074. [DOI] [PubMed] [Google Scholar]
- 94.Redell JB, Liu Y, Dash PK. Traumatic brain injury alters expression of hippocampal microRNAs: potential regulators of multiple pathophysiological processes. J Neurosci Res. 2009;87:1435–1448. doi: 10.1002/jnr.21945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Redell JB, Moore AN, Ward NH, 3rd, Hergenroeder GW, Dash PK. Human traumatic brain injury alters plasma microRNA levels. J Neurotrauma. 2010;27:2147–2156. doi: 10.1089/neu.2010.1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Redell JB, Zhao J, Dash PK. Altered expression of miRNA-21 and its targets in the hippocampus after traumatic brain injury. J Neurosci Res. 2011;9:212–221. doi: 10.1002/jnr.22539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Truettner JS, Alonso OF, Bramlett HM, Dietrich WD. Therapeutic hypothermia alters microRNA responses to traumatic brain injury in rats. J Cereb Blood Flow Metab. 2011;31:1897–1907. doi: 10.1038/jcbfm.2011.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Pasinetti GM, Ho L, Dooley C, Abbi B, Lange G. Select non-coding RNA in blood components provide novel clinically accessible biological surrogates for improved identification of traumatic brain injury in OEF/OIF Veterans. Am J Neurodegener Dis. 2012;1:88–98. [PMC free article] [PubMed] [Google Scholar]
- 99.Valiyaveettil M, Alamneh YA, Miller SA, et al. Modulation of cholinergic pathways and inflammatory mediators in blast-induced traumatic brain injury. Chem Biol Interact. 2013;203:371–375. doi: 10.1016/j.cbi.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 100.Klein P, Herr D, Pearl PL, et al. Results of phase 2 safety and feasibility study of treatment with levetiracetam for prevention of posttraumatic epilepsy. Arch Neurol. 2012;69:1290–1295. doi: 10.1001/archneurol.2012.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Klein P, Herr D, Pearl PL, et al. Results of phase II pharmacokinetic study of levetiracetam for prevention of post-traumatic epilepsy. Epilepsy Behav. 2012;24:457–461. doi: 10.1016/j.yebeh.2012.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Pearl PL, McCarter R, McGavin CL, et al. Results of phase II levetiracetam trial following acute head injury in children at risk for posttraumatic epilepsy. Epilepsia. 2013;54:e135–137. doi: 10.1111/epi.12326. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 78kb)