Abstract
Objective. To assess the impact of high-fidelity patient simulation on pharmacy resident knowledge, confidence, and competency with advanced resuscitation algorithms and interventions.
Design. An overview of the institutional cardiopulmonary arrest algorithm and a review of pertinent medications and calculations were presented to postgraduate year 1 (PGY1) pharmacy residents, followed by participation in 3 simulated clinical scenarios using a high-fidelity mannequin.
Assessment. An improvement of pharmacy resident knowledge, confidence, and competency with advanced resuscitation skills was observed. In addition, pharmacy residents demonstrated high performance levels with skills requiring advanced competency and proactive interactions with the cardiac arrest team.
Conclusion. Incorporating high-fidelity patient simulation into an advanced resuscitation training program can help pharmacy residents achieve competency through the active learning of practical skills.
Keywords: patient simulation, advanced cardiac life support, resuscitation, competency-based education, active learning
INTRODUCTION
Pharmacist participation in advanced cardiovascular life support (ACLS) reduces adverse drug events and hospital mortality.1,2 As members of the resuscitation team, pharmacists are expected to assist with medication preparation and dose calculations, but their roles may also be expanded to provide chest compressions, analyze rhythms, administer medications, and provide pharmacotherapy recommendations based on the patient’s clinical status.2 This team-based approach to advanced resuscitation has impacted pharmacy education with emphasis on critical thinking, problem solving, communication, and interprofessional teamwork skills.3-6 A consensus on the best method to develop these abilities, however, has not been reached.
To meet the increasing demand for a mode of education that supports the application of knowledge and skill sets, the use of simulation-based training in medical education is expanding at a rapid rate.7-10 The Accreditation Council for Pharmacy Education recommends the use of educational technologies to aid in experiential learning.11 The technique of imitating a clinical scenario for the purpose of medical training began in the 1960s with Resusci-Anne.7,12 Since then, simulation has expanded from the use of partial-task trainers for the development of a specific skill to high-fidelity, full-body mannequins with sophisticated computer-based capacities to provide both physiological and electrical outputs.7
A major benefit of clinical simulation is the provision of a safe and supportive educational environment so that learners can enhance their performance without inflicting adverse clinical outcomes.12 In addition, high-fidelity patient simulation (HFPS) may render an elevated degree of reality to provide feedback and portray clinical variation. Its impact on learning is comprehensively described by the Best Evidence Medical Education review, which identified many successful features of HFPS, such as the ability to capture clinical variation, provide individualized learning, and offer feedback.7,8
Simulation can play an important role for students and healthcare professionals.5,13-16 A prospective randomized controlled trial demonstrated that HFPS improved ACLS performance, and medical residents were more adherent to American Heart Association standards during cardiac arrest events.17-19 High-fidelity simulation in pharmacy education has also been well received with a significant improvement in knowledge and problem-solving skills.4,20-23 One study showed that pharmacy students felt HFPS enhanced their understanding of ACLS but they demonstrated poor knowledge retention at 3 months.4 In contrast, Seybert and colleagues established that using HFPS with pharmacy students can lead to a significant improvement in knowledge, confidence, and ability to interpret data.21-23
We are unaware of any studies demonstrating the effectiveness of HFPS with pharmacists participating in resuscitation teams. The purpose of our investigation was to evaluate how this mode of education can impact advanced resuscitation knowledge, competency, and confidence of acute care PGY1 pharmacy residents from the University of California San Diego Medical Center (UCSDMC). The outcomes of this study may be used to guide further use of HFPS for advanced resuscitation education and training.
DESIGN
This study analyzed the impact of high-fidelity simulation as an adjunctive training instrument for improving knowledge, confidence, and competency with advanced resuscitation skills in 12 acute care PGY1 pharmacy residents. The University of California San Diego Institutional Review Board approved this study.
At the start of the pharmacy residency program, each resident attended the UCSDMC substitute for the American Heart Association ACLS course known as the Advanced Resuscitation Training (ART) workshop. The ART course teaches institution-specific treatment algorithms for arrest situations and basic resuscitation techniques to all trainees. When compared to ACLS, the ART program allows further customization to address discipline-specific skills so that pharmacists may learn the fundamentals of an arrest response and practice skills relevant to their expected responsibilities at a greater depth. As a replacement for ACLS certification, all staff physicians, pharmacists, respiratory therapists, and nurses are required to attend ART and maintain competency biennially.
The pharmacist ART course involved 4 hours of formal instruction, 2 hours of medication review, and 2 hours of interactive task-based training for cardiopulmonary resuscitation. Although the course used partial-task trainers and defibrillators with manually adjustable rhythms, the mannequins were incapable of providing real-time feedback and their functions were limited to practicing airway management and chest compressions. The pharmacist ART course was offered annually to pharmacy residents and taught by the UCSD resuscitation director and 2 pharmacists on the University Code Blue Committee. All residents were required to achieve a minimum score of 70% on the approved multiple-choice written examination to be allowed to assist in a cardiac arrest team.
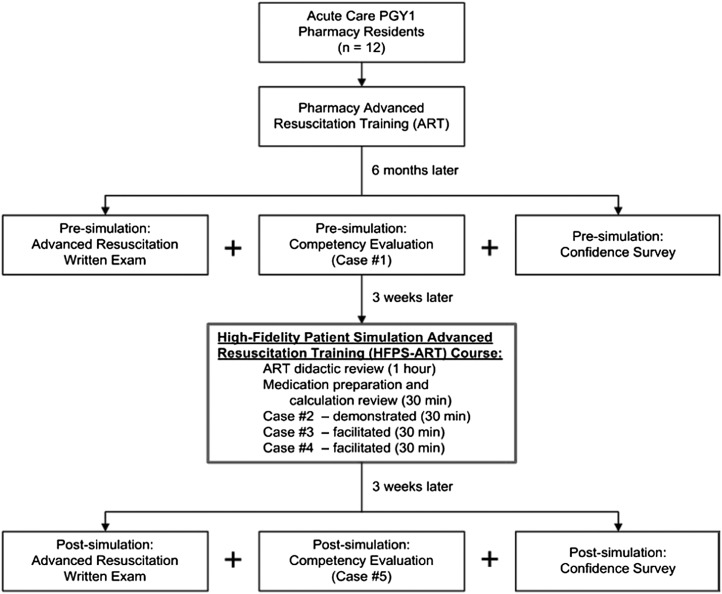
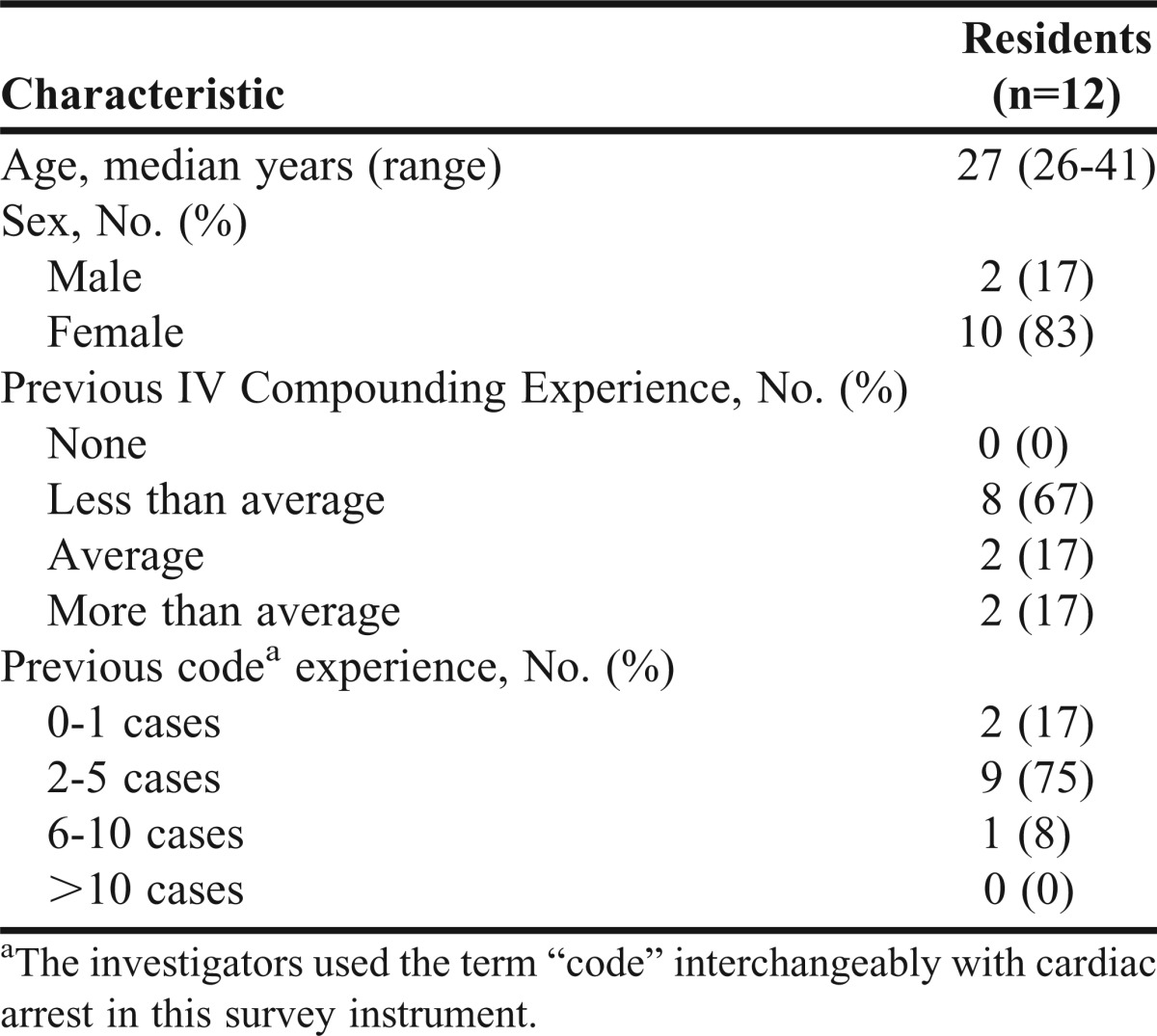
Six months following the initial ART course, a high-fidelity simulator became available for the first time as an adjunctive training tool for pharmacy residents. Because the primary purpose of incorporating HFPS into ART was to enhance resident education, only pharmacy residents participated in this study. The whole-body mannequin is an iStan and is operated with the Müse interface (CAE Healthcare, Sarasoto, FL). The high-fidelity human patient simulator has a functional airway, palpable pulses, and a synchronized display for physiologic variables such as an electrocardiogram, pulse oximetry, and blood pressure. Its ability to respond to medications and progress to different clinical scenarios based on the participant’s interventions allows for the incorporation of complex medical conditions and the creation of intricate simulated cases. Three weeks prior to the implementation of the HFPS-ART course, baseline knowledge, confidence, and competency in performing advanced resuscitation skills were evaluated. Informed consent was obtained and demographic data including age, gender, previous intravenous admixture experience, and prior emergency response experience were collected (Table 1).
Table 1.
Demographics of Postgraduate Year 1 Acute Care Pharmacist Residents Who Participated in Simulated Advanced Resuscitation Training
The HFPS-ART course consisted of a lecture-based overview of institution-specific cardiopulmonary life support algorithms, a review of pertinent medications and drip calculations, a demonstration of a simulated case, and participation in 2 HFPS scenarios (Figure 1). An intensive care unit (ICU) pharmacist demonstrated the first case and paused intermittently to discuss the proposed interventions. The residents were then divided into groups of 4, with each group independently participating in 2 simulated advanced resuscitation scenarios. Each resident was given the opportunity to be the primary cardiac arrest team pharmacist, assist as the secondary cardiac arrest team pharmacist, perform chest compressions, and operate the bag-valve mask. These cases were facilitated by 3 pharmacists experienced with advanced resuscitation; 1 to operate the high-fidelity patient simulator, 1 to represent the physician in charge, and another to represent the cardiac arrest team nurse. The facilitators were allowed to intervene in order to offer guidance and emphasize teaching points. Following each case, the residents were debriefed and received suggestions to improve their performance as a pharmacist on the cardiac arrest team. Three weeks after the HFPS-ART course, the pharmacy residents were tested again for advanced resuscitation knowledge, confidence, and competency.
Figure 1.
Research design.
EVALUATION AND ASSESSMENT
Presimulation and postsimulation assessments of knowledge, confidence, and competency were respectively obtained through a written examination, survey instrument, and simulated exercise. The 20 multiple-choice questions on the written examination closely resembled those approved by the University Code Blue Committee but were modified by the study investigators to focus on pharmacist-specific responsibilities, such as providing accurate dose recommendations and drip rate calculations. The validity and reliability of the questions were verified by a pharmacist on the committee. Presimulation written examination scores and answers remained undisclosed to maintain the integrity of the postsimulation assessment.
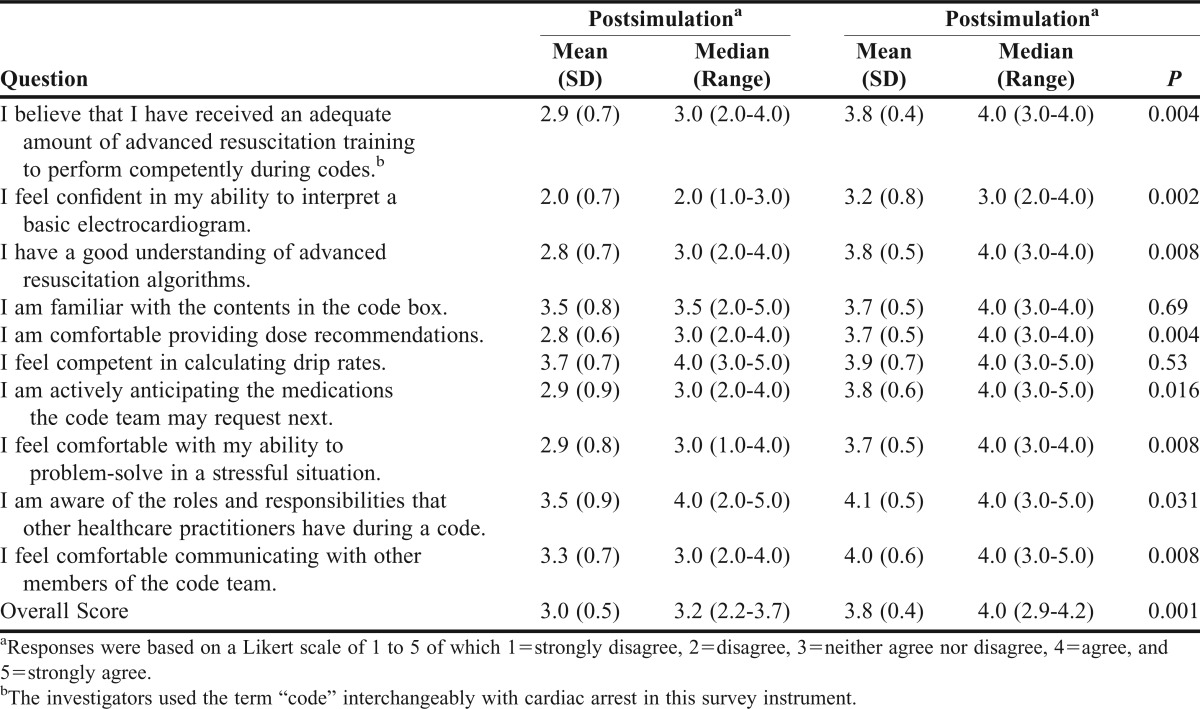
Presimulation and postsimulation confidence with pharmacist advanced resuscitation skills was evaluated using a survey instrument. The 10-question survey instrument was designed by the study investigators and used a 5-point Likert scale for responses, ranging from strongly disagree to strongly agree, similar to the survey instruments used in previous simulation-based studies.4,20-22
The competency assessment was a 20-minute HFPS case designed for the uninterrupted evaluation of pharmacist advanced resuscitation skills. The presimulation case involved ventricular fibrillation, ventricular tachycardia, and hypotension secondary to septic shock, while the postsimulation case consisted of pulseless electrical activity, ventricular tachycardia, and hypotension secondary to septic shock. The presimulation and postsimulation scenarios were different to minimize positive results gained from a repeat evaluation of the same case. Performance was scored based on equivalent timing goals and required interventions to allow for comparison between the 2. To maintain the integrity of the exercise between the pharmacy residents, the participants were required to complete the written examination and confidence survey instrument at an alternate location under pharmacist supervision immediately prior to the competency evaluation.
During these competency cases, the physician in charge, cardiac arrest team nurse, respiratory therapist, and healthcare practitioner performing compressions were represented by a pharmacist. Each resident was scored by 2 independent evaluators based on a previously validated and reliable checklist.17 The checklist was modified to reflect the pharmacist-specific required interventions assessed in our study , such as providing repeat doses of epinephrine within an appropriate timeframe, recommending correct antiarrhythmic doses, and calculating accurate drip rates. These interventions were reviewed by 2 ICU specialists and listed in the order recommended by institutional algorithms and given equal weight. A dichotomous scoring scale was assigned to each procedure with 0 indicating not done or performed incorrectly, and 1 demonstrating that the resident had completed the task correctly. The final score was based on the averaged result between the 2 evaluators.
Within the competency assessment, the evaluators also investigated the pharmacy residents’ ability to recall knowledge and anticipate medication requests. The former measured the residents’ aptitude for recommending medications and doses during a stressful scenario, while the latter measured their ability to suggest and compound appropriate medications without being prompted by a physician or nurse. Throughout the simulated exercise, open communication with the cardiac arrest team was allowed and encouraged if assistance was needed with clinical interpretation.
Twelve acute care pharmacy residents completed the simulated ART course using the HFPS. The median age was 27 years old and there were more female participants (83%) than male participants (17%). Baseline characteristics were similar, with most residents having little experience with compounding intravenous medications and attending ≤ 5 cardiac arrests prior to the HFPS exercise. Presimulation and postsimulation data were analyzed using the Wilcoxon-signed rank test. Analysis of the competency data was performed using the average score of the 2 evaluators. The significance level was set at 0.05.
Advanced resuscitation knowledge prior to and following the HFPS-ART course was assessed through a written examination. Presimulation scores showed that only half of the residents were performing at or above the minimum competency level of 70%. Of 20 questions, the median scores were 13 before and 18 after high-fidelity simulation training. Following the HFPS-ART course, pharmacy resident advanced resuscitation knowledge scores based on a written examination significantly increased from 65% to 88% (p=0.001). An improvement in score was consistent for all trainees, with the exception of 1 participant who had achieved perfect scores at both the baseline and final evaluation, thereby precluding any chance for improvement on the written examination. Following HFPS-ART, all residents scored at least 70%, with 3 of 12 achieving perfect scores.
Pharmacy residents’ confidence with advanced resuscitation techniques improved overall after HFPS-ART. The median confidence score increased from 3.2 to 4.0 (p=0.001) based on a 5-point Likert scale (Table 2). Residents felt significantly more confident that they had received sufficient advanced resuscitation training, understood institutional algorithms, and recognized the roles of other team members. In addition, they believed they were able to provide accurate dose recommendations, problem solve, and communicate effectively in a stressful scenario. Confidence with becoming more familiar with the cardiac arrest medication box contents and calculating drip rates, however, did not significantly improve.
Table 2.
Confidence Survey Scores of Pharmacy Residents Before and After Advanced Resuscitation Simulation Training
Competency evaluations showed a significant improvement in overall pharmacy resident aptitude with advanced resuscitation skills, based on a comprehensive intervention checklist. The median pre- and post-simulation competency scores were 64% and 77%, respectively (p=0.009). The statistics were adjusted for multiple evaluators. Secondary outcomes measured within the competency evaluation included the capacity to recall knowledge in a disorderly environment, and the ability to anticipate cardiac arrest medication requests through independent clinical assessment or open communication with the team. The median knowledge recall score was 77% before and 84% after the HFPS-ART course (p=0.003). The median medication anticipation score was 52% before and 68% after HFPS-ART (p=0.027).
DISCUSSION
This study analyzed the impact of adding HFPS to an existing advanced resuscitation program to improve pharmacy resident knowledge, confidence, and competency with cardiopulmonary resuscitation interventions. Overall, implementation of simulation-based teaching has a positive impact on medical education. Fourth-year medical students showed improved confidence after completing clinical trauma scenarios.16 In 2005, Wayne and colleagues documented that simulation-based education significantly increased medical residents’ adherence to resuscitation guidelines based on intervention checklist scores.17 More importantly, they were able to link performance in the simulated environment with the quality of delivered patient care in a followup report published in 2008.18
Seybert and colleagues described the incorporation of HFPS into pharmacy education. Second-year pharmacy students were extremely satisfied with their experience and 75% felt that the exercise further developed their ability to solve problems.21 In 2008, HFPS was integrated into an Introduction to Critical Care course and the students’ knowledge of and confidence in pharmacotherapy and patient-care skills significantly improved.23
Our study generated similar results and it was the first study to evaluate the effectiveness of simulation-based training on practicing pharmacy residents. While the UCSDMC standard for pharmacist participation on the cardiac arrest team is the biennial completion of a written competency test, several studies have exposed the failure of written examinations to predict the successful acquisition of practical skill sets.8,11,14 By introducing a mode of education that offers a supportive learning environment through repetitive practice, clinical variability, and individualized learning, the goal of incorporating HFPS is to provide an outcomes-based strategy for training.
To achieve our primary objective of evaluating the effectiveness of HFPS for pharmacy resident training, our study assessed both written and practical advanced resuscitation skills. Although our findings for improvement in knowledge and confidence are consistent with those of previous studies, few investigations have explored functional competency as an endpoint. In addition to showing a significant improvement in overall competency, pharmacy residents demonstrated that simulation-based education can enhance performance in a simulated scenario through their ability to recall knowledge in a disorganized environment and proactively respond to the patient’s changing clinical status. This further strengthens study findings that HFPS promotes the practical application of clinical skills and is a useful tool for pharmacist training.
One unexpected finding was that neither residents’ confidence in calculating drip rates or familiarity with the cardiac arrest medication box contents notably improved, but high baseline confidence levels may have left little room for progress. We also appreciated the significant improvement in competency with tasks requiring more advanced skill sets, such as anticipating medication requests and communicating with other members of the code team. Because these abilities cannot be cultivated through a traditional written competency examination, HFPS may help bridge the gap between a passive to an active-learning experience.
The time required for all 12 pharmacy residents to participate in the HFPS-ART course and complete the presimulation and postsimulation assessments was approximately 17 hours. This is similar to the 19 hours required in a study by Mieure and colleagues, with the availability of only 1 high-fidelity patient simulator being the greatest limitation. Total instruction time for the HFPS-ART session was 5 hours and included 1 hour of lecture, 30 minutes of medication review, 30 minutes of HFPS demonstration, and 1 hour for each group of 4 pharmacy residents to complete 2 cases. Although this investigation relied on pharmacy residents as study participants, the same HFPS modules can be used for staff pharmacists. Because of a greater variation in cardiac arrest experience between the ICU and non-ICU clinical specialists, the groups for the simulated exercise may be formed based on self-reported comfort levels with cardiac arrest team participation. In order to implement HFPS as a routine component of ART, technologically advanced skills are required to run the software, build case scenarios, and compile debriefing documents. Also, experienced practitioners should be present to run the high-fidelity simulator and provide appropriate feedback.
Several limitations existed with this study. Because the pharmacy department was interested in piloting a fully functional ART course with the incorporation of HFPS, we were unable to determine whether the improvement in scores could be attributed to the additional lecture provided along with HFPS. The material was a condensed version of the same presentation from the initial ART workshop, however, so the lecture did not contain any new information. With regards to any potential knowledge acquired from the repeat administration of the written examination, the solutions to the test were never revealed, thereby minimizing the possibility of recognizing the most appropriate answer. Also, residents may have gained experience from the baseline competency assessment as a result of additional time spent training with the high-fidelity simulator. Therefore, the combined effect of the HFPS-ART course and the baseline HFPS case could have led to improved advanced resuscitation skills.
Limitations with the competency evaluations included the use of 2 HFPS cases, the variation in pharmacists representing members of the cardiac arrest team, and the different independent evaluators used for the presimulation and postsimulation exercises. The HFPS scenarios, however, were intentionally distinct to reduce the positive effect of repeating the same exercise. More importantly, the timing goals and interventions required from the competency assessment were equivalent. Cardiac arrest team members were represented by pharmacists who volunteered to be present for either the baseline or final assessments. Despite these differences, each team member was given a script with specific instructions to minimize variation. The use of different evaluators was the greatest limitation, but 1 evaluator was consistently present for both assessments and the final score for each resident was based on the averaged findings between the 2 evaluators.
Another limitation was the difficulty speculating the overall impact of simulation-based education based on a small sample size of 12 participants. Also, because HFPS was incorporated as an additional training tool for all acute care pharmacy residents, the absence of a control group cannot eliminate the effect of time and emergency response experience gained within the 6 weeks between the baseline and final assessments. Most trainees, however, did not claim any additional experience, except for 1 resident who attended as many as 5 cardiac arrests during this timeframe because of a practice experience in the emergency department. Furthermore, the study did not measure long-term retention of advanced resuscitation knowledge, confidence, or competency since the final evaluations were performed only 3 weeks after HFPS-ART course, which was near the completion of the residency program. Arranging for the course to be taken at the beginning of the year or extending HFPS-ART to staff pharmacists may allow for future opportunities to determine long-term effectiveness.
Regardless of these barriers, our study demonstrated positive outcomes for using HFPS as an adjunctive tool to improve pharmacy resident competency with advanced resuscitation skills. In addition to achieving basic proficiency of advanced resuscitation knowledge and techniques, our investigation corroborated that high-fidelity simulation may be an effective mode of education for acquiring practical experience.
Based on the success of this program, the UCSDMC Resuscitation Director and Code Blue Committee have sanctioned the incorporation of HFPS for the annual training of all pharmacy residents. Invitation to participate in the training program has also been extended to the staff pharmacists at our institution. Although the HFPS cases remained the same, the lecture-based portion was augmented to include neurological, neonatal, and maternal emergencies. Additional directions of HFPS-ART at this institution involve expansion beyond the traditional ACLS algorithms to include stroke and ST-segment elevation myocardial infarction cases.
SUMMARY
This study assessed the impact of adding high-fidelity simulation to an existing ART program to improve pharmacy resident knowledge, confidence, and competency with cardiopulmonary life support algorithms and techniques. The participants successfully demonstrated that HFPS-ART was effective for achieving functional competency with advanced resuscitation, and the use of a high-fidelity simulator may be helpful with the development of practical skill sets.
ACKNOWLEDGMENTS
The investigators thank the UCSDMC Trauma Department for permission to use their high-fidelity simulator for this study.
REFERENCES
- 1.Bond CA, Raehl CL. Clinical pharmacy services, pharmacy staffing, and hospital mortality rates. Pharmacotherapy. 2007;27(4):481–493. doi: 10.1592/phco.27.4.481. [DOI] [PubMed] [Google Scholar]
- 2.Draper HM, Eppert JA. Association of pharmacist presence on compliance with advanced cardiac life support guidelines during in-hospital cardiac arrest. Ann Pharmacother. 2008;42(4):469–474. doi: 10.1345/aph.1K475. [DOI] [PubMed] [Google Scholar]
- 3.Westberg SM, Adams J, Thiede K, Stratton TP, Bumgardner MA. An interprofessional activity using standardized patients. Am J Pharm Educ. 2006;70(2):Article 34. doi: 10.5688/aj700234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mieure KD, Vincent WR, III, Cox MR, Jones MD. A high-fidelity simulation mannequin to introduce pharmacy students to advanced cardiovascular life support. Am J Pharm Educ. 2010;74(2):Article 22. doi: 10.5688/aj740222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hamilton N, Freeman BD, Woodhouse J, Ridley C, Murray D, Klingensmith ME. Team behavior during trauma resuscitation: A simulation-based performance assessment. J Grad Med Educ. 2009;1(2):253–259. doi: 10.4300/JGME-D-09-00046.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shapiro MJ, Morey JC, Small SD, et al. Simulation based teamwork training for emergency department staff: does it improve clinical team performance when added to an existing didactic teamwork curriculum? Qual Saf Health Care. 2004;13(6):417–421. doi: 10.1136/qshc.2003.005447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bradley P. The history of simulation in medical education and possible future directions. Med Educ. 2006;40(3):254–262. doi: 10.1111/j.1365-2929.2006.02394.x. [DOI] [PubMed] [Google Scholar]
- 8.Issenberg SB, McGaghie WC, Petrusa ER, Lee Gordon D, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Med Teach. 2005;27(1):10–28. doi: 10.1080/01421590500046924. [DOI] [PubMed] [Google Scholar]
- 9.Steadman RH, Coates WC, Huang YM, et al. Simulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skills. Crit Care Med. 2006;34(1):151–157. doi: 10.1097/01.ccm.0000190619.42013.94. [DOI] [PubMed] [Google Scholar]
- 10.Ziv A, Ben-David S, Ziv M. Simulation based medical education: An opportunity to learn from errors. Med Teach. 2005;27(3):193–199. doi: 10.1080/01421590500126718. [DOI] [PubMed] [Google Scholar]
- 11.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. Standard 25.7. https://www.acpe-accredit.org/pdf/CPE_Standards_Final.pdf. Accessed February 12, 2011.
- 12.Perkins GD. Simulation in resuscitation training. Resuscitation. 2007;73(2):202–211. doi: 10.1016/j.resuscitation.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 13.Weller JM. Simulation in undergraduate medical education: bridging the gap between theory and practice. Med Educ. 2004;38(1):32–38. doi: 10.1111/j.1365-2923.2004.01739.x. [DOI] [PubMed] [Google Scholar]
- 14.Rogers PL, Jacob H, Rashwan AS, Pinsky MR. Quantifying learning in medical students during a critical care medicine elective: a comparison of three evaluation instruments. Crit Care Med. 2001;29(6):1268–1273. doi: 10.1097/00003246-200106000-00039. [DOI] [PubMed] [Google Scholar]
- 15.Ford DG, Seybert AL, Smithburger PL, Kobulinsky LR, Samosky JT, Kane-Gill SL. Impact of simulation-based learning on medication error rates in critically ill patients. Intensive Care Med. 2010;36(9):1526–1531. doi: 10.1007/s00134-010-1860-2. [DOI] [PubMed] [Google Scholar]
- 16.Gilbart MK, Hutchison CR, Cusimano MD, Regehr G. A computer-based trauma simulator for teaching trauma management skills. Am J Surg. 2000;179(3):223–228. doi: 10.1016/s0002-9610(00)00302-0. [DOI] [PubMed] [Google Scholar]
- 17.Wayne DB, Butter J, Siddall VJ, et al. Simulation-based training of internal medicine residents in advanced cardiac life support protocols: a randomized trial. Teach Learn Med. 2005;17(3):210–216. doi: 10.1207/s15328015tlm1703_3. [DOI] [PubMed] [Google Scholar]
- 18.Wayne DB, Didwania A, Feinglass J, Fudala MJ, Barsuk JH, McGaghie WC. Simulation-based education improves quality of care during cardiac arrest team responses at an academic teaching hospital: a case-control study. Chest. 2008;133(1):56–61. doi: 10.1378/chest.07-0131. [DOI] [PubMed] [Google Scholar]
- 19.Neumar RW, Otto CW, Link MS, et al. Adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 Suppl 3):S729–S767. doi: 10.1161/CIRCULATIONAHA.110.970988. [DOI] [PubMed] [Google Scholar]
- 20.Fernandez R, Parker D, Kalus JS, Miller D, Compton S. Using a human patient simulation mannequin to teach interdisciplinary teams skills to pharmacy students. Am J Pharm Educ. 2007;71(3):Article 51. doi: 10.5688/aj710351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seybert AL, Laughlin KK, Benedict NJ, Barton CM, Rea RS. Pharmacy student response to patient-simulation mannequins to teach performance-based pharmacotherapeutics. Am J Pharm Educ. 2006;70(3):Article 48. doi: 10.5688/aj700348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seybert AL, Barton CM. Simulation-based learning to teach blood pressure assessment to doctor of pharmacy students. Am J Pharm Educ. 2007;71(3):Article 48. doi: 10.5688/aj710348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seybert AL, Kobulinsky LR, McKaveney TP. Human patient simulation in a pharmacotherapy course. Am J Pharm Educ. 2008;72(2):Article 37. doi: 10.5688/aj720237. [DOI] [PMC free article] [PubMed] [Google Scholar]