Abstract
Introduction
We describe a novel, clinically applicable conduction study of the laryngeal nerves.
Methods
17 normal volunteer subjects were included. Activation of the sensory territory of the superior laryngeal nerve was performed by administration of low level, brief electrical stimulus. The laryngeal closure reflex (LCR) evoked by this stimulus was recorded by needle electrodes. Mean minimal latencies were calculated for each response, and proposed values for the upper limit of normal were determined.
Results
Uniform consistent early ipsilateral responses and late bilateral responses, which exhibit greater variation in latency and morphology, were recorded. Significant side-to-side difference in latencies is observed, consistent with the length discrepancy between right and left recurrent laryngeal nerves.
Discussion
This technique yields clear, quantifiable data regarding neurologic integrity of laryngeal function, heretofore unobtainable in the clinical setting. This study may yield clinically relevant information regarding severity and prognosis in patients with laryngeal neuropathic injury.
Keywords: Laryngeal electromyography, vagus nerve, laryngeal closure reflex, brainstem reflexes, neurolaryngology
Introduction and Background
Normal functioning of the larynx is necessary for breathing, voice production and airway protection during swallowing. Disease or injury resulting in laryngeal dysfunction can have devastating consequences for the affected patient, at times requiring invasive procedures such as tracheostomy and/or gastrostomy tube placement, and predisposing the patient to serious pulmonary infections. Further, by limiting a person's ability to communicate and/or eat and drink, these disorders are accompanied by a substantive decrease in quality of life.
Dysfunction of the laryngeal apparatus on the basis of peripheral neuropathic injury is fairly common. Due to the circuitous route of the recurrent laryngeal nerve, this nerve is particularly vulnerable to injury from tumor compression or destruction along its path as a complication of a variety of common surgical procedures, including thyroidectomy, anterior approach to the cervical spine, and cardiac and pulmonary surgery. In addition, idiopathic laryngeal neuropathy, typically in the postviral setting, is a well-recognized clinical entity analogous to Bell's palsy. Yet, no means of directly diagnosing and quantitatively evaluating such nerve dysfunction exists. Clinical assessment depends on endoscopic visualization of the end organ. Although symptom-based therapies to treat these disorders have evolved over the past few decades, identification and quantification of peripheral laryngeal nerve dysfunction remains relatively poor, contributing little to clinical decision-making.
Reflexes involving cranial nerve-brainstem pathways have long been identified and are well-described 1,2,3. The corneal/blink reflex, gag reflex, and oculocephalic reflex have important clinical relevance as part of the neurologic examination. A nerve conduction study of the blink reflex (Blink Reflex Study, BRS) was described by Kimura in 1969 4. This electrodiagnostic study provides quantifiable parameters allowing for evaluation and assessment of the peripheral afferent and efferent limbs of the blink reflex, as well as information regarding relay of this reflex through the central nervous system. Today, this study is performed frequently along with nerve conduction studies and electromyography as a routine component of a clinical electrodiagnostic examination. This study can provide essential information regarding localization and degree of neuropathic injury involving cranial nerves V and VII, as well as provide information regarding relay through the brainstem.
We propose that determination of the electrophysiological parameters of the nerves subserving the larynx will have similar clinical value for diagnosis and prognosis in patients with laryngeal dysfunction. The laryngeal closure reflex (LCR) ensures protection of the airway via bilateral laryngeal adduction resulting in closure of the bilateral vocal folds in response to irritative stimulation of distal laryngeal mucosa. The afferent and efferent limbs of this reflex are subserved by different branches of CN X; the afferent limb by sensory fibers of the superior laryngeal nerve (SLN) and the efferent limb by motor fibers of the recurrent laryngeal nerve (RLN). As with the Blink Reflex Study, it is proposed that deviations from normative values can provide precise localization and information regarding the extent of neurological injury to the larynx, lending greater insight into the mechanisms of laryngeal dysfunction than previously available via current diagnostic tools.
Materials/Methods
This study was approved by the Institutional Review Board of Weill Cornell Medical Center. Healthy adult volunteers with no complaints of voice, swallowing or respiratory problems were recruited from the general population. Using the standard percutaneous approach used clinically for diagnostic laryngeal electromyography, hookwire EMG electrodes were placed within the bilateral thyroarytenoid muscles. Accurate electrode placement was confirmed by volitional activation of these laryngeal adductors (asking the patient to phonate a sustained /e/). Reference electrodes were positioned over the lateral aspect of the thyroid cartilage on each side, and a ground electrode was placed midline over the superior sternum. The evoked potentials recorded from these muscles were displayed on a dual trace oscilloscope after conventional amplification using a two-channel amplifier (Nicolet Viking 11.2). Following electrode placement, the larynx was visualized by means of a standard flexible laryngoscope inserted transnasally under topical nasal anesthetic, as is done for routine laryngeal evaluation in the office. Activation of the sensory territory of the superior laryngeal nerve was achieved by means of unilateral irritative stimulation to the laryngeal mucosa in the form of a low level, brief electrical stimulus (5-10 mA, 0.1 ms). The stimulus was delivered via a wire electrode passed through the working channel of the laryngoscope. Location of the stimulating electrode was observed endoscopically, and the stimulus was not delivered until placement was confirmed by the endoscopist. The reflex adduction of bilateral vocal folds evoked by unilateral sensory stimulation (LCR) was recorded by needle electromyography. For each subject, a minimum of 4 recordings was obtained from stimulation of each side. The minimal latencies of the responses were marked as agreed upon by two neurologists with fellowship training in clinical neurophysiology and neuromuscular disease.
Results
17 normal volunteer subjects (8 men, 9 women, ages 20-40) were included in the study. Volunteers were in good health, without symptomatic dysfunction of larynx, and with a normal laryngeal examination by laryngoscopy.
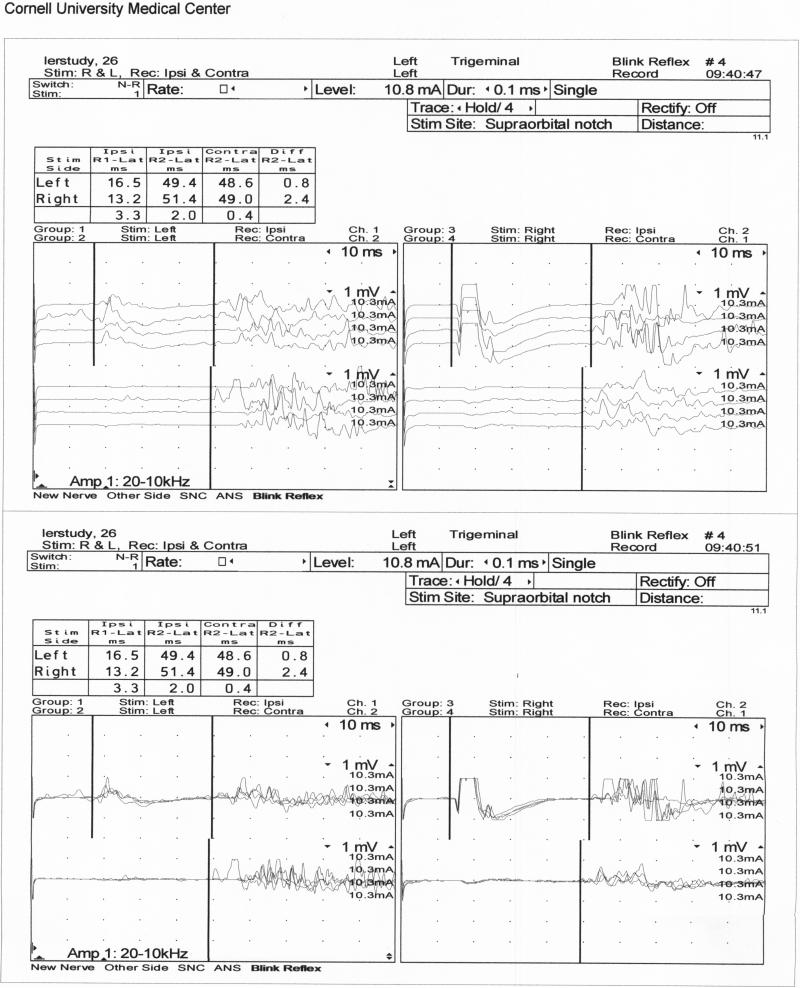
Responses were obtained and recorded following right and left sided stimulation of the laryngeal mucosa. This study yields an early response ipsilateral to the side of stimulation (LR1), which is uniform and consistent, and late bilateral responses (ipsilateral LR2 (LR2i) and contralateral LR2 (LR2c)), which exhibit greater variation in latency and morphology (Figure 1).
Figure 1.
Above: Individual Response Tracings
Below: Superimposed Responses
Mean minimal latencies were calculated for each response (Table 1). Proposed preliminary values for the upper limit of normal (ULN) for these latencies were determined by calculating 3 standard deviations above the mean (Table 2).
Table 1.
Mean Minimal Latencies for Early and Late Responses
| Stimulation Side | LR1 Latency Ipsilateral | LR2 Latency Ipsilateral | LR2 Latency Contralateral |
|---|---|---|---|
| Right: | 13.2 ms | 50.5 ms | 50.7 ms |
| Left : | 15.2 ms | 52.2 ms | 50.6 ms |
Table 2.
Proposed Upper Limit of Normal (ULN) = 3 SD above mean for Early and Late Responses
| Stimulation Side | LR1 Latency Ipsilateral | LR2 Latency Ipsilateral | LR2 Latency Contralateral |
|---|---|---|---|
| Right: | 15.6ms | 60.6 ms | 63.5 ms |
| Left : | 18.8 ms | 61.1 ms | 62.8 ms |
Discussion
The presence of an early consistent unilateral response ipsilateral to the side of stimulation and more variable late bilateral responses is analogous to the results seen in the Blink Reflex Study. Extrapolating from the neuroanatomical understanding of the BRS, we postulate that the early ipsilateral LR1 response in this study represents a disynaptic connection between the nucleus solitarius and the ipsilateral nucleus ambiguus in the medulla, whereas the late bilateral LR2 responses are mediated by a polysynaptic pathway between the activated sensory nucleus (presumably the solitary nucleus, although some general afferent vagal sensory fibers are understood to synapse in the spinal trigeminal nucleus) and the ipsilateral and contralateral nuclei ambiguus. 4,5,6,7
The recurrent laryngeal nerve has a unique anatomical feature of significant right to left length disparity due to its embryologically mediated course under the aortic arch on the left, while “recurring” under the subclavian artery on the right. In man, the average difference in length between the right and left recurrent laryngeal nerves is approximately 11 cm (for comparison, right to left differences average 0.8 cm in rat, 13 cm in dog, 30 cm in giraffe).8 This is reflected in our data, in that a significant side-to-side difference in LR1 latencies is observed in our study (p < 0.001), with longer left LR1 latencies compared with right LR2 latencies, consistent with the longer anatomical pathway the left sided response must travel. Significant lateralized differences were not observed for the LR2 responses, perhaps as a result of polysynaptic relays within the brainstem that may mitigate this difference. It is also possible that the variation of these responses will require that a larger population is studied before a pattern emerges.
This normative data is intended as a foundation for clinical study of patients with laryngeal neuropathies. The current electrodiagnostic assessment of laryngeal neuropathy is limited to electromyography. While capable of demonstrating motor neuropathy, and of establishing whether the nerve is in continuity in cases of trauma, electromyography has proved disappointing in prognostication. Certainly, the absence of motor units and presence of spontaneous activity suggests a lower probability of satisfactory recovery than its opposite. However, the information provided by electromyography is approximate, and complicated by the potential for synkinetic reinnervation from adductor and abductor fibers commixed in the same nerve. In numerous studies, electromyography has not yet proved a reliable guide to clinical treatment. 9,10,11,12,13,14,15,16,17
Accurate prognostic information would be invaluable in the selection of treatment of patients with laryngeal neuropathy. For example, treatment of patients with unilateral laryngeal neuropathy consists of procedures aimed at positioning the paralyzed vocal fold in the midline so that the mobile vocal fold may effect glottic closure to prevent aspiration and optimize voice production. Treatment is divided roughly into office-based, minimally invasive but temporary measures and operating-room based open neck procedures which are permanent. 18,19 The current standard, imposed more by a century's tradition of practice than by any evidence, is to manage patients in expectation of recovery for one year. Prognostic information is of obvious importance in selecting patients for early definitive treatment and sparing them unnecessary and repeated temporary procedures.
In the analogous case of facial neuropathy, electromyography has proven similarly unsatisfactory, yet nerve excitability 20 , latency 21, and amplitude of the muscle action potential 22 have all been shown to add prognostic information.
In addition to prognostic considerations, electromyography is blind to the afferent nerves. Laryngeal sensory neuropathy has been hypothesized to be critically important in swallowing safety. The only means of assessment is currently the administration of a puff of air via the working channel of a laryngoscope, which is poorly reproducible and non quantitative, yielding only the presence or absence of the laryngeal closure reflex. By incorporating the afferent arm of the laryngeal closure reflex, the method presented in this paper may yield improved and more consistent data regarding this aspect of laryngeal neural function.
The authors have already embarked on the application of this technique to patients with laryngeal neuropathy, and expect that data from this investigation will help formulate hypotheses and determine the future direction of study.
Conclusions
This technique yields clear, quantifiable data regarding neurologic integrity of laryngeal function, heretofore unobtainable in the clinical setting. This study is well-tolerated and safe, performed in the outpatient setting with the standard diagnostic equipment routinely used by neurologists and otorhinolaryngologists. By enabling the determination of electrophysiological parameters of the nerves subserving laryngeal function, namely the superior laryngeal and recurrent laryngeal branches of CN X, in combination with routine clinical laryngeal EMG, this procedure is expected to provide earlier and more accurate information regarding extent and grade of nerve injury. Because injury grade relates directly to prognosis, the information derived from this test can have immediate clinical relevance in determining optimal treatment of neuropathic injury in patients with dysfunction of speaking, swallowing, and protection of airway.
Acknowledgements
This investigation was supported by grant UL1 RR024996 of the Clinical and Translational Science Center at Weill Cornell Medical College
Abbreviations
- BRS
Blink Reflex Study
- LCR
Laryngeal Closure Reflex
- LR1
Laryngeal response 1 (early response
- LR2
Laryngeal response 2 (late response)
- RLN
Recurrent laryngeal nerve
- SLN
Superior laryngeal nerve
- ULN
Upper limit of normal
References
- 1.Kugelberg E. Facial Reflexes. Brain. 1952 Sep;75:385–396. doi: 10.1093/brain/75.3.385. [DOI] [PubMed] [Google Scholar]
- 2.Overend W. Preliminary Note on a New Cranial Reflex. Lancet. 1896 (March;1:619. [Google Scholar]
- 3.Wartenberg R. The Examination of Reflexes. Year Book Medical Publishers, Inc.; Chicago: 1945. pp. 25–34. [Google Scholar]
- 4.Kimura J, Powers M, Van Allen MW. Reflex Response of Orbicularis Oculi Muscle to Supraorbital Nerve Stimulation. Arch Neurol. 1969 Aug;21:193–199. doi: 10.1001/archneur.1969.00480140093009. [DOI] [PubMed] [Google Scholar]
- 5.Suzuki M. Laryngeal Reflexes. In: Hirano M, Kirchner JA, Bless DM, editors. Neurolaryngology: recent advances. College-Hill; Boston, MA: 1987. pp. 142–55. [Google Scholar]
- 6.Wilson-Pauwels, editor. Cranial Nerves in Health and Disease. BC Decker Inc; Ontario: 2002. pp. 182–201. [Google Scholar]
- 7.Brodal A. Neurological anatomy in relation to clinical medicine. 3rd ed. Oxford University Press; New York: 1981. pp. 460–464. [Google Scholar]
- 8.Harrison DFN. The Anatomy and Physiology of the Mammalian Larynx. Cambridge University Press; 1995. [Google Scholar]
- 9.Gupta SR, Bastian RW. Use of laryngeal electromyography in prediction of recovery after vocal cord paralysis. Muscle Nerve. 1993 Sep;16(9):977–8. doi: 10.1002/mus.880160917. [DOI] [PubMed] [Google Scholar]
- 10.Hydman J, Björck G, Person JK, Zedenius J, Mattsson P. Diagnosis and prognosis of iatrogenic injury of the recurrent laryngeal nerve. Ann Otol Rhinol Laryngol. 2009 Jul;118(7):506–11. doi: 10.1177/000348940911800709. [DOI] [PubMed] [Google Scholar]
- 11.Grosheva M, Wittekindt C, Pototschnig C, Lindenthaler W, Guntinas-Lichius O. Evaluation of peripheral vocal cord paralysis by electromyography. Laryngoscope. 2008 Jun;118(6):987–90. doi: 10.1097/MLG.0b013e3181671b2d. [DOI] [PubMed] [Google Scholar]
- 12.Sittel C, Stennert E, Thumfart WF, Dapunt U, Eckel HE. Prognostic value of laryngeal electromyography in vocal fold paralysis. Arch Otolaryngol Head Neck Surg. 2001;127:155–160. doi: 10.1001/archotol.127.2.155. [DOI] [PubMed] [Google Scholar]
- 13.Munin MC, Rosen CA, Zullo T. Utility of laryngeal electromyography in predicting recovery after vocal cord paralysis. Arch Phys Med Rehabil. 2003;84:1150–1153. doi: 10.1016/s0003-9993(03)00146-1. [DOI] [PubMed] [Google Scholar]
- 14.Parnes SM, Satya-Murti S. Predictive value of laryngeal electromyography in patients with vocal cord paralysis of neurogenic origin. Laryngoscope. 1985 Nov;95(11):1323–6. doi: 10.1288/00005537-198511000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Wang CC, Chang MH, Wang CP, Liu SA. Prognostic indicators of unilateral vocal fold paralysis. Arch Otolaryngol Head Neck Surg. 2008 Apr;134(4):380–8. doi: 10.1001/archotol.134.4.380. [DOI] [PubMed] [Google Scholar]
- 16.Min YB, Finnegan EM, Hoffman HT, Luschei ES, McCulloch TM. A preliminary study of the prognostic role of electromyography in laryngeal paralysis. Otolaryngol Head Neck Surg. 1994 Dec;111(6):770–5. doi: 10.1177/019459989411100612. [DOI] [PubMed] [Google Scholar]
- 17.Hirano M, Nosoe I, Shin T, Maeyama T. Electromyography for laryngeal paralysis. In: Hirano M, Kirchner J, Bless D, editors. Neurolaryngology: recent advances. 1st ed. College Hill; Boston: 1987. pp. 232–48. [Google Scholar]
- 18.Sulica L, Blitzer A, editors. Vocal Fold Paralysis. Springer; 2006. [Google Scholar]
- 19.Blitzer A, Brin MF, Ramig LO. Neurologic Disorders of the Larynx. second edition. Thieme; 2009. [Google Scholar]
- 20.Campbell EDR, Hickey RP, Nixon KH, Richardson AT. Value of nerve excitability measurements in prognosis of facial palsy. Br Med J. 1962;2:7. doi: 10.1136/bmj.2.5296.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Langworth EP, Taverner D. The prognosis in facial palsy. Brain. 1963;86:465. doi: 10.1093/brain/86.3.465. [DOI] [PubMed] [Google Scholar]
- 22.Olsen PZ. Prediction of recovery in Bell's palsy. Acta Neurol Scand. 1975;52(Suppl 61) doi: 10.1111/j.1600-0404.1975.tb01402.x. 1. [DOI] [PubMed] [Google Scholar]