Abstract
Purpose
The present study aims to elucidate the treatment strategies of laparoscopic resection for gastroduodenal submucosal tumors (SMTs).
Methods
Data of 125 gastroduodenal STMs were collected retrospectively resected from August, 2004 to February, 2013. Surgical outcomes according to tumor locations, pathologic results and survival data for gastrointestinal stromal tumors (GISTs) were collected and analyzed.
Results
There were 55 male and 70 female patients with mean age 57.9 ± 12.7 years old. Mean tumor size of gastric SMTs was 2.7 ± 1.64 cm (range, 0.4-8.5 cm). GIST was the most common (n = 70, 56%). Regarding the tumor location, all the fundic lesions were GISTs and leiomyoma was occurred 58.8% of cardiac lesions. Ectopic pancreas and schwannomas were mostly located at body portion, 73% and 80%, respectively. SMTs located at duodenal bulb comprise 4 GISTs and 3 carcinoids. Surgical results comparing between lesions located at cardia, near-pylorus and else had no difference in operation time, hospital stay and complications. In terms of outcome of GIST, all patients underwent curative resection except one case of peritoneal sarcomatosis. There was one recurrence in a high risk group following resection. The cumulative 5-year disease free survival rate was 93.5% in all GISTs. There were two postoperative complications, one gastric outlet obstruction and one leakage following wedge resection.
Conclusion
Laparoscopic wedge resection is a safe and feasible procedure for the small to medium sized gastroduodenal SMTs even their locations are near cardia or pylorus.
Keywords: Stomach neoplasms, Gastrointestinal stromal tumor, Laparoscopy
INTRODUCTION
Standard treatment for gastroduodenal SMTs is surgical resection due to difficulties in pathologic confirmation before operation [1]. Several surgical approaches are recommended according to their size and locations [2]. Among them, laparoscopic wedge resection is most widely performed for gastric SMTs and has become a main treatment option for small to medium size gastric SMTs [3,4]. However, treatment controversies still exist, from observation to surgical resection, especially for the small sized SMTs. Additionally, location near esophagogastric junction (EGJ) and pylorus can be a challenging issue for laparoscopic resection. Herein we aimed to show experience of laparoscopic surgery for gastroduodenal SMTs to evaluate and introduce the safety and efficacy of laparoscopic resection with reasonable treatment strategies for the small to medium sized gastroduodenal SMTs, especially located near EGJ and pylorus.
METHODS
We reviewed the prospectively collected data of 137 consecutive patients who underwent surgical resection for the gastric submucosal tumors from August 2004 until March 2013 at Yeouido St. Mary's Hospital, The Catholic University of Korea. Current study protocol was reviewed and approved by the Catholic University of Korea Institutional Review Board. We excluded 12 cases including 7 epithelial origin tumors (6 inflammatory fibroid polyps and 1 hyperplastic polyp), 2 GISTs treated by conventional open method due to large size and perforated state and 2 duodenal SMTs located at duodenal 2nd and 3rd portion. In this study, we analyzed patients' demographics, tumor locations, tumor morphologic characteristics, operation types, operative results, and perioperative outcomes. Tumor location was differentiated into duodenal bulb, antrum, body, cardia, and fundus. Cardia was defined from EGJ to 3-cm distal from EGJ. To evaluate the efficacy and appropriateness of applying laparoscopic resection for the SMTs located near EGJ and pylorus, we divided all lesions into three area according to surgical concerns; area I, cardiac SMTs; area II, SMTs located no more than 3 cm from pylorus including duodenal bulb; area III, else area except area I or area II. We classified the locations in to areas I and II with the nearest margin of the tumor. In case of GIST, recurrence and survival analysis were performed.
Statistic analyses were performed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA). All continuous variables were expressed as mean ± standard deviation. Continuous variables were compared with unpaired Student t-test and nominal variables were compared with chi-square test. Correlation between size and mitotic figure of GISTs was estimated with linear regression analysis. Survival analysis was done with Kaplan-Meier and log-rank test. Null hypotheses of no difference were rejected if P-values were less than 0.05.
Surgical techniques for laparoscopic wedge resection
A day before surgery, endoscopic clipping was performed in cases of small endophytic SMTs less than 2 cm, for accurate tumor localization during operation. Each patient was placed in the reverse Trendelenburg position. A carbon dioxide pneumoperitoneum was performed from the umbilical port with pressure maintenance between 12-14 mmHg. Usually 4 trocars (10 mm for scope, 5 mm and 12 mm for operator, 5 mm for assistant) were placed. Easily detected exophytic or dumb-bell shape tumors were resected by laparoscopic wedge resection using linear staplers with exogastric approach. In cases of small, endophytic, posterior wall intraluminal lesions were explored through anterior gastrotomy, and resected while the traction was done. In case of SMTs near EGJ, tumor traction using thread and identification of the EGJ was mandatory to make secure resection for prevention of further stenosis.
RESULTS
Clinicopathologic characteristics
There were 55 males and 70 females with a mean age of 57.9 ± 12.7 years (range, 19-83 years). The mean tumor size was 2.8 ± 1.7 cm (range, 0.4-8.5 cm). Histopathologic results revealed 70 GISTs, 18 leiomyomas, 15 ectopic pancreases, 11 schwannomas, 10 carcinoids and 1 glomus tumor. Among all cases, 115 wedge resections (92%), 9 Billroth-II distal gastrectomies (7.2%), and one total gastrectomy were performed via laparoscopic approach. There was no resection margin positive case and the majority of cases (95 cases) had resected margin within 10 mm. In addition, there was no tumor recurrence at the resection margin during the median 13 months (range, 1-100 months) of follow-up. Seven patients underwent concurrent operations (Table 1), such as cholecystectomy for gall bladder stones, herniorrhaphy for inguinal hernia, right hemicolectomy for right colon cancer, Nissen fundoplication for gastroesophageal reflux disease, and total thyroidectomy for thyroid cancer. Mean operation time for all cases and wedge resection cases were 106.8 ± 73.9 minutes (range, 27-375 minutes) and 95.8 ± 46.3 minutes (range, 27-270 minutes), respectively. The mean postoperative hospital stay was 5.4 ± 3.8 days (range, 2-23 days). The average number of linear staples used during laparoscopic wedge resection was 2.1 ± 1.9 (range, 0-5) (Table 1). There were 2 postoperative complications out of 125 patients (1.6%) which were gastric outlet obstruction and leakage of staple line in wedge resection cases which are located at antrum lesser curvature side. Those complications were treated with reoperative laparoscopic gastrojejunostomy and primary closure, respectively. There was no perioperative mortality.
Table 1.
Clinicopathologic and surgical outcomes of 125 gastroduodenal submucosal tumors underwent laparoscopic resection
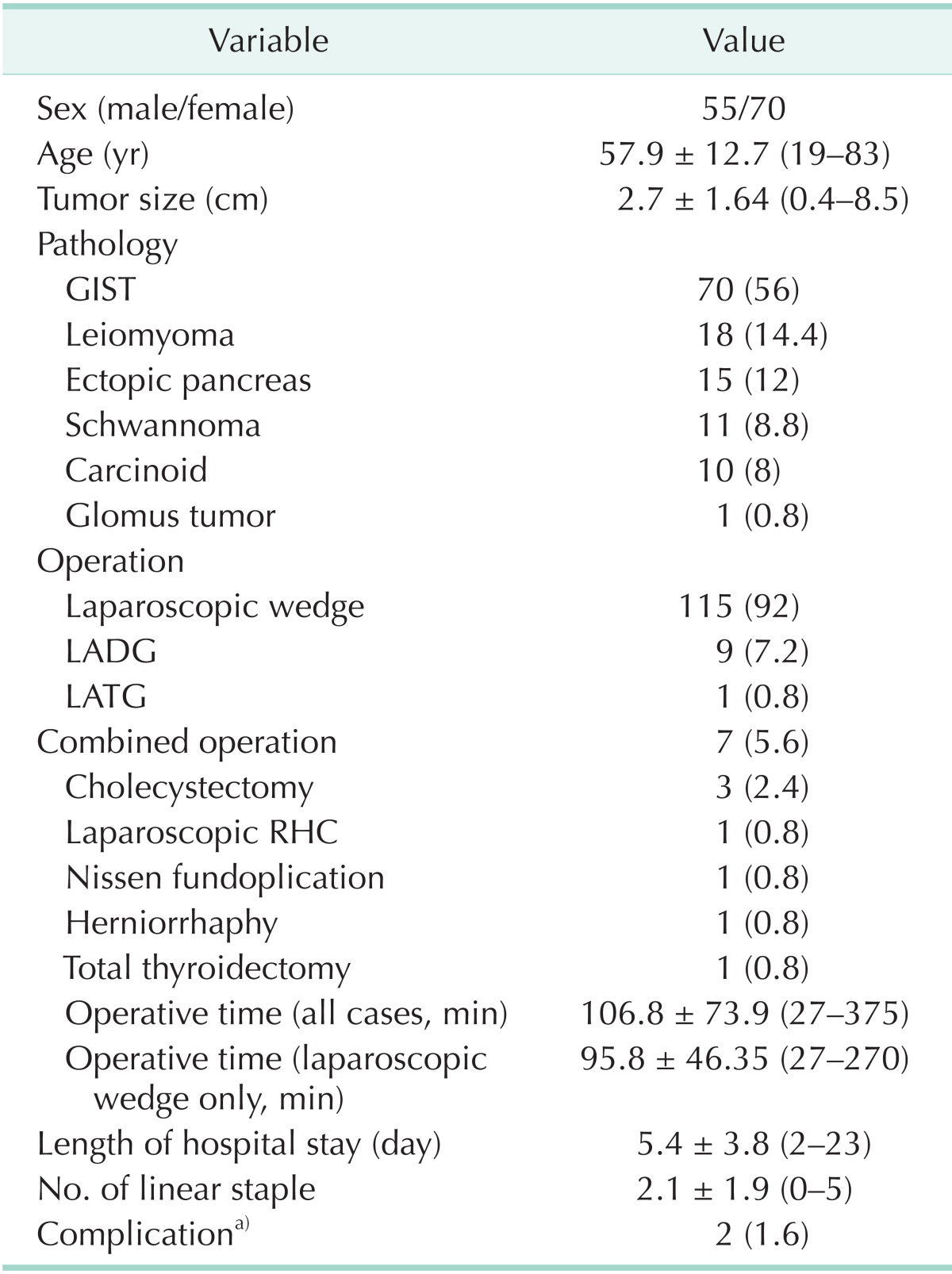
Values are presented as mean ± standard deviation (range) or number (%).
GIST, gastrointestinal stromal tumor; LADG, laparoscopy assisted-distal gastrectomy; LATG, laparoscopy assisted total gastrectomy; RHC, right hemicolectomy.
a)Pyloric stricture (1) and leakage (1) in gastric submucosal tumor.
Characteristics of tumors (location, growth pattern, and size)
The pattern of tumor location according to pathologic diagnosis was significantly different (Table 2). The body was the most frequent site of gastric SMTs. GIST was most frequently distributed except cardia. All the fundic lesions were GISTs. Leiomyoma was predominantly located at the cardia; 58.8% of cardiac lesions were leiomyoma. Ectopic pancreas and schwannomas were usually located at distal part of the stomach. Four out of 23 antral SMTs located near pyloric ring. One of them involved the pyloric ring.
Table 2.
Prevalence of gastroduodenal submucosal tumors by tumor location
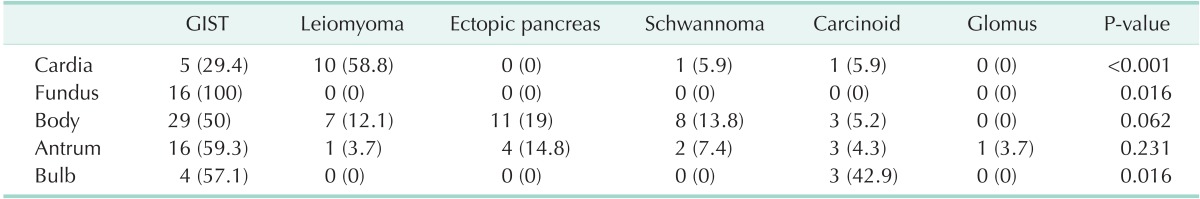
Values are presented as number (%).
GIST, gastrointestinal stromal tumor.
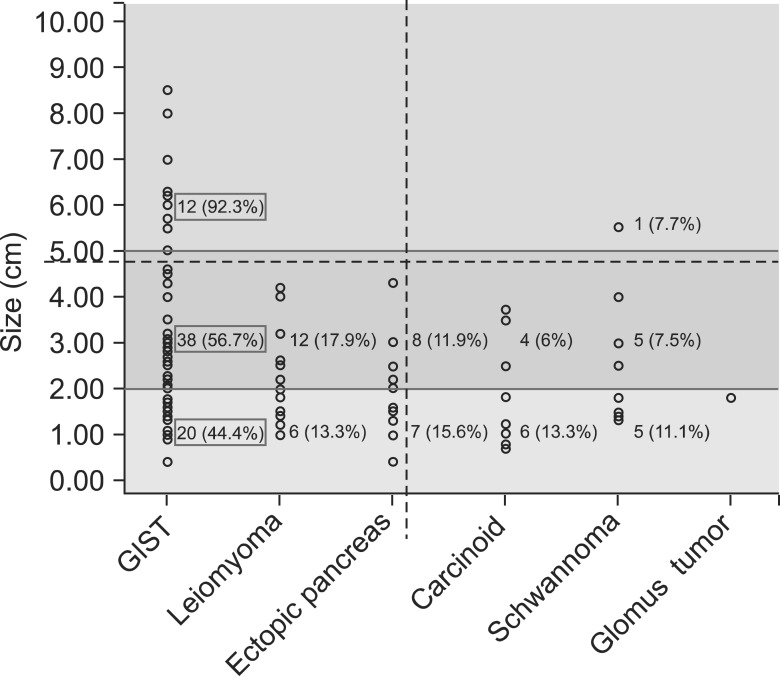
Regarding the growth pattern and size, GIST and neurogenic tumor tended to grow exophytically, while more portions of leiomyoma, carcinoid and ectopic pancreas grow with endophytic feature (Table 3). GIST was the largest (3.1 ± 1.9 cm) among all gastroduodenal SMTs and schwannoma was the next (2.3 ± 1.3 cm). Almost all tumors larger than 5 cm were GISTs except one schwannoma. GIST comprised 20 cases (44.4%) among the SMTs less than 2 cm (Fig. 1).
Table 3.
Growth pattern and size of gastric submucosal tumors by diagnosis
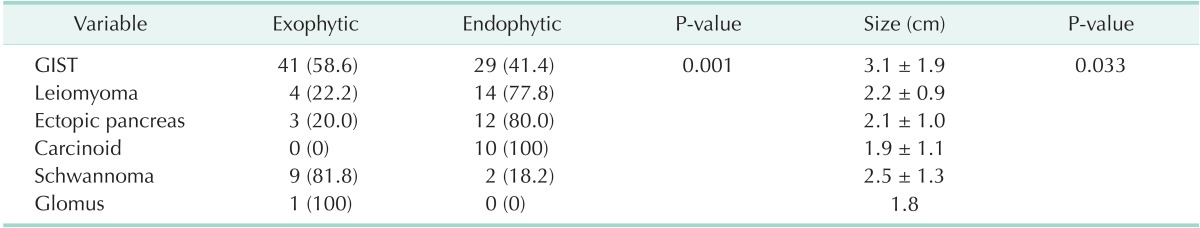
Values are presented as number (%) or mean ± standard deviation.
GIST, gastrointestinal stromal tumor
Fig. 1.
Distribution of gastroduodenal submucosal tumors according to diagnosis and size. GIST, gastrointestinal stromal tumor.
Comparison of clinicopathologic and surgical outcomes according to the tumor location
The comparison of clinicopathologic features and surgical outcomes between three locations are described at Table 4. Among all gastroduodenal SMTs, there were 17 cardiac lesions (area I), 11 peripyloric lesions including 7 duodenal SMTs and 4 prepyloric SMTs (area II) and 97 SMTs located except area I and area II (area III). Mean age of area I group was significantly younger than the others. Regarding disease entity, leiomyoma was the dominant in area I and GIST was dominant at area II and area III. Endophytic lesions were more common in area I and area II rather than area III. There was no significant difference in distribution of tumor size between three groups. In addition, no difference was found in operation time, length of hospital stay and complication. However, less laparoscopic staplers were used for area II SMTs during wedge resection. In area I group, except one patient with huge shwannoma, all patients underwent laparoscopic wedge resection, and there was no stricture or reflux postoperatively. Among area II cases, 1 carcinoid at duodenal bulb and two GISTs involving pyloric ring underwent laparoscopic assisted distal gastrectomy and the others underwent laparoscopic wedge resection including 1 hybrid resection with intraoperative gastrofiberscope in small size duodenal carcinoid. Following wedge resection, concurrent gastrojejunostomy was mandatory in 2 patients resulting structural deformity after wedge resection.
Table 4.
Comparison of clinicopathologic and surgical results according to the tumor location
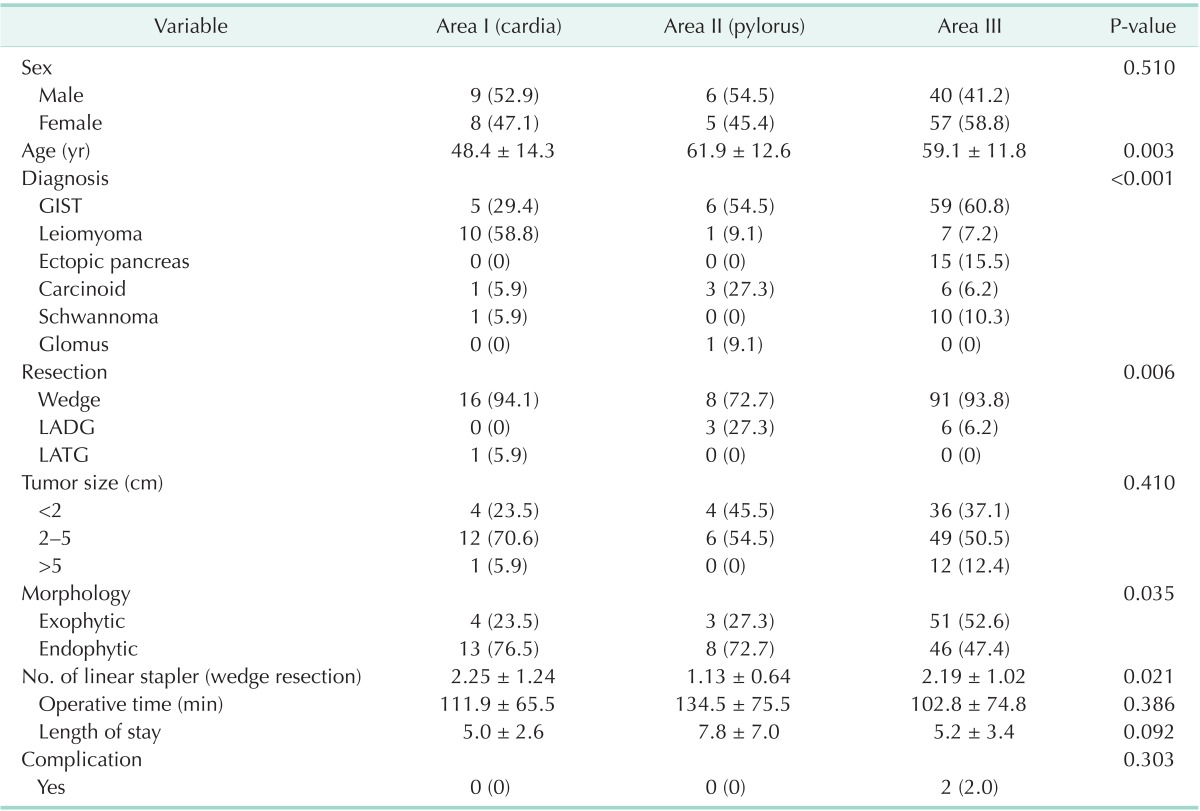
Values are presented as number (%) or mean ± standard deviation.
GIST, gastrointestinal stromal tumor; LADG, laparoscopy assisted-distal gastrectomy; LATG, laparoscopy assisted total gastrectomy.
Characteristics of 70 GISTs and their oncologic outcomes
Among 70 GISTs there were 8 patients in high, 17 in intermediate, 32 in low, and 13 in the very low risk group, according to NIH GIST risk classification [5].
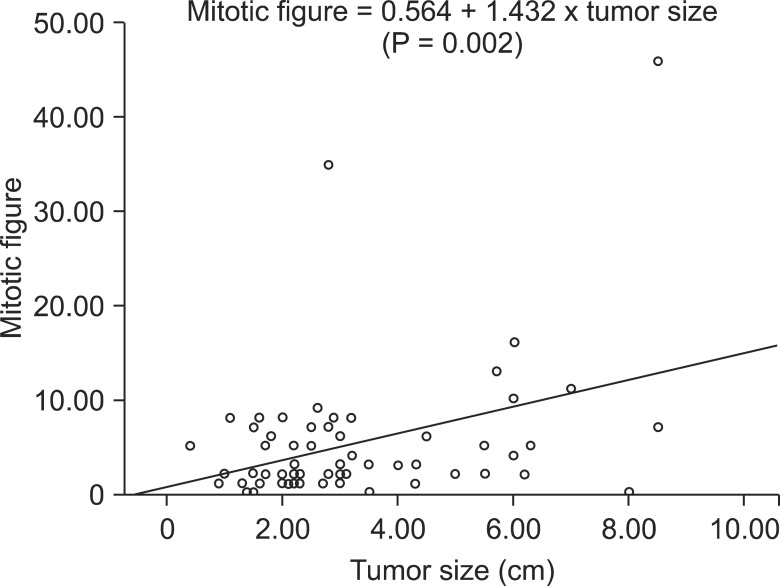
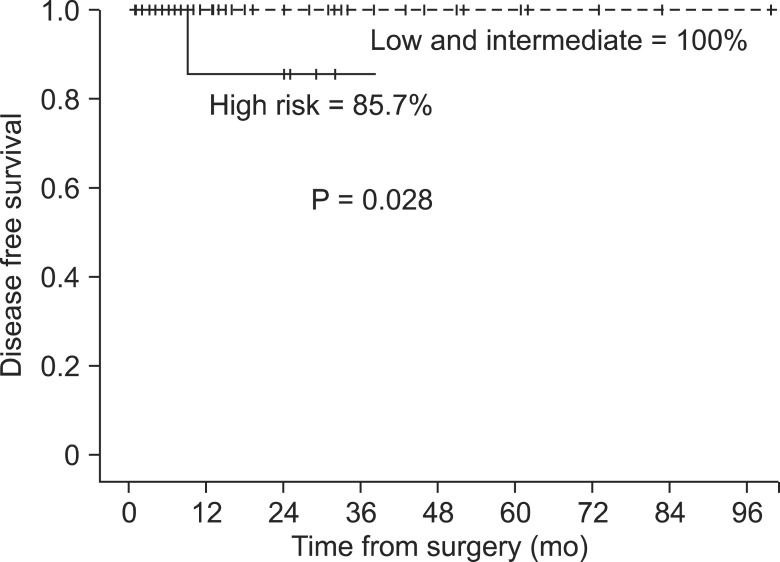
There was no statistical correlation between risk grade and tumor location or morphologic feature. The mean tumor size was 2.7 ± 1.6 cm (range, 0.4-8.5 cm). Linear regression analysis shows the close correlation between mitotic figure and tumor size. (Mitotic figure = 0.564 + 1.432 × tumor size, P = 0.002, R = 0.144) (Fig. 2). All patients underwent R0 curative resection except 1 patient with peritoneal sarcomatosis involved in high risk group. The patient who received palliative resection was diagnosed with gastric SMT 2 years prior to surgery, which increased in size from 1.7 to 8.5 cm. On diagnostic laparoscopy, carcinomotosis nodules were already scattered in the peritoneal cavity and omentum. There was 1 recurrence out of 69 GIST patients who underwent curative surgery (median, 15 months; range, 1-64 months). In addition, survival analysis between high risk group and other groups differed significantly in 3-year disease free survival (Fig. 3) (high risk group vs. intermediate and low risk group: 85.7% vs. 100%, P = 0.028).
Fig. 2.
Linear regression model shows close correlation of tumor size and mitotic figures in gastrointestinal stromal tumor.
Fig. 3.
Disease free survival between high risk versus low and intermediate risk groups of gastrointestinal stromal tumor patients underwent curative resection.
DISCUSSION
Since Fowler and White [6] performed first laparoscopic wedge resection for gastric SMT, laparoscopic surgery for gastric SMT has rapidly increased with the pace of diagnosis. The major concern during operation for gastroduodenal SMTs is GIST.
Because treatment strategy for GIST was not involving lymph node dissection, local resection with grossly negative margin and avoidance of tumor rupture are the recommended treatment option [7]. With satisfaction of those conditions, any type of laparoscopic approach can be justified for the gastric GIST and other SMTs without limitations, theoretically. However there are always some limitations regarding with the tumor size or difficult locations.
The SMTs larger than 2 cm are usually recommended for surgical resection [2]. However when the tumor size is less than 2 cm, making a decision for operation is less certain. If SMT is not a GIST or another malignant condition, surgical resection is not mandatory, because most non-GIST SMTs such as leiomyoma, ectopic pancreas or schwannoma are benign condition. In our series, there were 20 GISTs (44.4%) among all STMs less than 2 cm in size, and there was one malignant carcinoid tumor with size less than 2 cm. Especially, the size of the palliative resection case was less than 2 cm when diagnosed 2 year before surgery. For these reasons, it is hard to say that observation is the choice for the gastric SMTs less than 2 cm. Surgical resection is required when the morphologic feature or biopsy is suspicious for GIST or others with malignant potentials.
Regarding the correlation of diagnosis and tumor location, there were some reports showing similar results with our study [8]. According to our data, there are some patterns of tumor location. (1) All the SMTs in fundus are GIST. (2) Leiomyoma is the most frequent tumor among cardiac lesions. (3) Ectopic pancreas and schwannoma are mostly located at the distal part of the stomach. Considering these patterns, we can recommend surgical resection for the SMTs in fundus, even the size is small. For other sites, preoperative endoscopic incisional biopsy or endoscopic ultrasound (EUS)-guided fine needle biopsy can be helpful in making a preoperative diagnosis and avoiding unnecessary surgery, especially in cardia.
Laparoscopic surgical resection cannot be easily applied to tumors located near the EGJ and pylorus, because of high risk of deformity or leakage [9,10]. Lee et al. [8] showed the size of SMTs in cardia is smaller than that of body and fundus. Furthermore endophytic SMTs were significantly more common at cardia. In our study there was no difference in size between cardia and noncardia group, but more endophytic lesions occurred in the cardia. Additionally, younger patients had more cardia tumors. Regarding with area II SMTs, it includes 7 in duodenal bulb and 4 in prepyloric antrum including 2 at pylorus. There was no complication in area I and area II such as reflux or outlet obstruction. However, in two cases of duodenal bulb, we performed preventive laparoscopic gastrojejunostomy due to structural deformity following wedge resection. Actually, a case included in area III showed gastric outlet obstruction. In this case, the lesion was located at antrum, lesser curvature side. Maybe, longitudinal stapling made structural deformity and gastric outlet obstruction. For this reason, thorough consideration for the direction of stapling is needed when exogastric resection for the SMTs located antrum, lesser curvature near pylorus.
Regarding surgical procedures, small, endophytic features and posterior wall location might suggest a need for gastrotomy and transgastric resection. In our group, more transgastric resections were required in cardia group not only for visualization of endophytic morphology and posterior wall mass, but also for visualization of EGJ during resection not to make injury. In our experience, when we perform transgastric resection for endophytic SMTs, traction of the mass was done by suturing the mass before clamping the laparoscopic stapler, so it seems that resection was done with partial thickness of the gastric wall. This technique can minimize the extent of resection and make secure resection away from the injury of EGJ.
In our series, 70 cases of GIST including 8 high risk patients underwent curative laparoscopic resection except 1 peritoneal sarcomatosis case. Among curative resection cases, one female patient who underwent laparoscopic resection for an 8.5 cm GIST (7 mitosis/50 high-power field) developed recurrence. The CT scan performed 6 months postoperatively revealed recurrence at the small bowel mesentery and trocar site. Imatinib was started at the dose of 400 mg per day and the masses regressed after medication for 1 year. She stopped medication for 8 months because of anorexia and general weakness. The trocar site tumor returned, and Imatinib was restarted. Now the patient is in the complete resolution state, and medication is maintained. There are some reports showing oncologic outcomes regarding recurrence following laparoscopic resection for gastric GIST [4,11,12]. However, the sample size is small and there were only small numbers of high risk patients in laparoscopic resection group. Otani et al. [2] reported 3 recurrences among 9 high risk GIST patients and 96.1% of 5-year disease free survival rate. Although our data showed similar rate of recurrence in high risk patients compared with other reports with open surgery, considering the number of recurred cases, larger size (>5 m) high risk GIST should be reconsidered when performing laparoscopic resection.
Other gastric SMTs such as leiomyoma, ectopic pancreas and schwannomas are benign slow growing neoplasms with excellent prognosis after surgical resection. They are usually asymptomatic but may become clinically evident when complicated by pathologic changes such as inflammation, bleeding, obstruction, and malignant transformation. They may occur everywhere in the stomach. In our series, gastric cardia was the most common site for leiomyoma with endophytic nature. Ectopic pancreas and schwannomas were mostly located at the distal part of the stomach, with endophytic growth for ectopic pancreas and exphophytic growth pattern for schwannoma. All these tumors were below 5 cm in size except one 5.5-cm-sized schwannoma located at body anterior wall.
There are some limitations to our study. First, this is retrospective and noncomparative study. Since August 2004, we performed gastric SMTs mostly with laparoscopic approach except for very large or complicated cases. For this reason, we had very little data of open resection for gastric SMTs during the contemporary period. Second, we analyzed the diagnosis of SMTs according to only gross features. If we had data of predictive diagnosis according to CT or EUS findings, there may be more valuable results regarding estimation of diagnosis preoperatively.
In conclusion, laparoscopic resection was suitable and safe for relatively small to medium sized gastroduodenal SMTs including GISTs even in the cardia or peripylorus including duodenal first portion. In cardiac lesions, laparoscopic wedge resection is safely adopted. However, stricture should be considered for peripyloric SMTs.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Berindoague R, Targarona EM, Feliu X, Artigas V, Balague C, Aldeano A, et al. Laparoscopic resection of clinically suspected gastric stromal tumors. Surg Innov. 2006;13:231–237. doi: 10.1177/1553350606295960. [DOI] [PubMed] [Google Scholar]
- 2.Otani Y, Furukawa T, Yoshida M, Saikawa Y, Wada N, Ueda M, et al. Operative indications for relatively small (2-5 cm) gastrointestinal stromal tumor of the stomach based on analysis of 60 operated cases. Surgery. 2006;139:484–492. doi: 10.1016/j.surg.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 3.Ryu KJ, Jung SR, Choi JS, Jang YJ, Kim JH, Park SS, et al. Laparoscopic resection of small gastric submucosal tumors. Surg Endosc. 2011;25:271–277. doi: 10.1007/s00464-010-1173-0. [DOI] [PubMed] [Google Scholar]
- 4.Privette A, McCahill L, Borrazzo E, Single RM, Zubarik R. Laparoscopic approaches to resection of suspected gastric gastrointestinal stromal tumors based on tumor location. Surg Endosc. 2008;22:487–494. doi: 10.1007/s00464-007-9493-4. [DOI] [PubMed] [Google Scholar]
- 5.Fletcher CD, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ, et al. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Hum Pathol. 2002;33:459–465. doi: 10.1053/hupa.2002.123545. [DOI] [PubMed] [Google Scholar]
- 6.Fowler DL, White SA. Laparoscopic resection of a submucosal gastric lipoma: a case report. J Laparoendosc Surg. 1991;1:303–306. doi: 10.1089/lps.1991.1.303. [DOI] [PubMed] [Google Scholar]
- 7.DeMatteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, Brennan MF. Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg. 2000;231:51–58. doi: 10.1097/00000658-200001000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee HH, Hur H, Jung H, Jeon HM, Park CH, Song KY. Analysis of 151 consecutive gastric submucosal tumors according to tumor location. J Surg Oncol. 2011;104:72–75. doi: 10.1002/jso.21771. [DOI] [PubMed] [Google Scholar]
- 9.Lee JS, Kim JJ, Park SM. Laparoscopic gastric wedge resection and prophylactic antireflux surgery for a submucosal tumor of gastroesophageal junction. J Gastric Cancer. 2011;11:131–134. doi: 10.5230/jgc.2011.11.2.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Song KY, Kim SN, Park CH. Tailored-approach of laparoscopic wedge resection for treatment of submucosal tumor near the esophagogastric junction. Surg Endosc. 2007;21:2272–2276. doi: 10.1007/s00464-007-9369-7. [DOI] [PubMed] [Google Scholar]
- 11.Goh BK, Chow PK, Chok AY, Chan WH, Chung YF, Ong HS, et al. Impact of the introduction of laparoscopic wedge resection as a surgical option for suspected small/medium-sized gastrointestinal stromal tumors of the stomach on perioperative and oncologic outcomes. World J Surg. 2010;34:1847–1852. doi: 10.1007/s00268-010-0590-5. [DOI] [PubMed] [Google Scholar]
- 12.Lee HH, Hur H, Jung H, Park CH, Jeon HM, Song KY. Laparoscopic wedge resection for gastric submucosal tumors: a size-location matched case-control study. J Am Coll Surg. 2011;212:195–199. doi: 10.1016/j.jamcollsurg.2010.10.008. [DOI] [PubMed] [Google Scholar]