Abstract
Purpose
The authors evaluate the prevalence of malnutrition and its effect on the postoperative morbidity of patients after surgery for colorectal cancer.
Methods
Three hundred fifty-two patients were enrolled prospectively. Nutritional risk screening 2002 (NRS 2002) score was calculated through interview with patient on admission. Clinical characteristics, tumor status and surgical procedure were recorded.
Results
The prevalence of patients at nutritional risk was 28.1 per cent according to the NRS 2002. The rate of postoperative complication was 27%. There was a significant difference in postoperative complication rates between patients at nutritional risk and those not at risk (37.4% vs. 22.9%, P = 0.006). Nutritional risk was identified as an independent predictor of postoperative complications (odds ratio, 3.05; P = 0.045). Nutritional risk increased the rate of anastomotic leakage (P = 0.027) and wound infection (P = 0.01).
Conclusion
NRS may be a prognostic factor for postoperative complication after surgery for colorectal cancer. A large scaled prospective study is needed to confirm whether supplementing nutritional deficits reduces postoperative complication rates.
Keywords: Colorectal neoplasms, Complication, Malnutrition, Morbidity
INTRODUCTION
The stress of surgery can increase the rate of perioperative morbidity and mortality [1]. Especially, the rate of postoperative complication is higher in gastrointestinal surgery, which results in increased hospital stay and cost [2]. The reported prevalence of malnutrition in gastrointestinal surgery patients ranges from 30% to 50% [3]. Malnutrition has been consistently associated with poor clinical outcomes, for example; impaired wound healing, higher infection rates and mortality as well as longer hospital stay, leading to increased overall costs [4,5]. Perioperative nutritional support in malnourished patients decreases postoperative complications such as wound infections and sepsis [4,6]. Therefore, nutritional risk screening (NRS) may be helpful to decrease the rate of postoperative complications. Routine screening of patients to identify risk of malnutrition has been recommended by many national, international, and specialist organizations [7].
NRS 2002 was introduced at the European Society for Clinical Nutrition and Metabolism (ESPEN) in 2002 [8]. This method is a reliable, easily applied and reproducible tool for identifying patients at nutritional risk in hospital. Its predictive value was documented by a retrospective analysis of 128 randomized controlled trials of nutritional support [9].
The aims of the present study were to evaluate the prevalence of malnutrition, by means of screening tool, NRS 2002, and to analyze the role of malnutrition in predicting postoperative complications in patients undergoing surgery for colorectal cancer.
METHODS
All patients diagnosed with colorectal cancer and scheduled for elective surgery in a single center between February 2010 and July 2011 were enrolled this study. During this period, a total of 545 patients went into hospital for surgery. We interviewed all patients at admission. Three hundred fifty-two patients who precisely answered their weight status and amount of oral intake status were enrolled in this study. There were no restrictions with regard to tumor stage or comorbidity. Data of patient characteristics, operative findings, pathologic reports, and postoperative outcome records were collected retrospectively. In addition, preoperative weight loss and amount of oral intake during 3 months before admission, nutritional risk as determined by the NRS 2002 at hospital admission, and patient social history: smoking status (active smoker) and alcohol consumption (intake over 70 g/day) were recorded. We defined a group of weight loss as decreased more than 5% in 3 months. A group of decrease of food oral intake was defined as decreased more than 25% in 3 months. Body height and weight were measured on the day of admission, and body mass index (BMI) was calculated. Serum albumin level was determined on the day of admission to hospital. Postoperative complications during hospital stay includes anastomotic leakage, intra-abdominal bleeding, ileus (more than two weeks), wound infection, intra-abdominal abscess, pneumonia, chylous leakage and so on.
Nutritional risk screening 2002
The NRS 2002 is used to predict outcome based on risk parameters identified in the nutritional assessment [8]. Nutritional risk is evaluated by two components: impaired nutritional status and severity of disease. The NRS 2002 is based on four variables-weight loss, BMI, general condition and amount of food intake in the preceding week-in addition to the patient's age and the severity of the underlying disease. The total score, calculated from the impaired nutritional status section (score, 0-3), the score for severity of disease (indicator of stress metabolism and increased nutritional requirements; score 0-3) and age adjustment (score + 1 for age over 70 years), ranges from 0 to 7. Patients are classified as being at nutritional risk (score 3 or more) or not (score less than 3) according to the total score obtained.
Statistical analysis
Statistical analyses were performed using PASW version 18.0 (SPSS Inc., Chicago, IL, USA). Continuous variables (age, BMI, and operative time) were dichotomized, using the mean value of each variable. Chi-square or Fisher exact test for categorical variables was used for statistical comparisons of clinical parameters, operative time, operative methods, preoperative nutritional status and NRS 2002. Multivariate analysis to detect risk factors for postoperative complications was conducted with a logistic regression model. Chi-square tests were also used to analyze morbidity variables associated with weight loss. A value of P < 0.05 was deemed statistically significant.
RESULTS
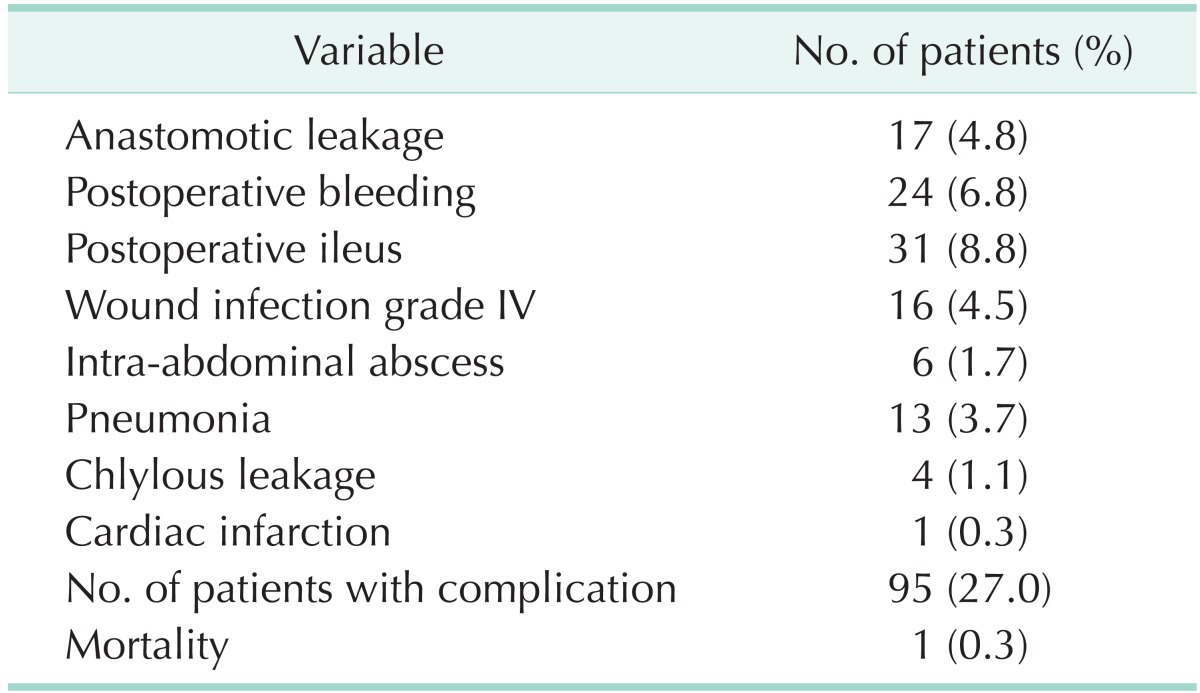
Ninety-five of 352 patients (27.0%) had complications; deaths were excluded from this analysis. There was one death in hospital (mortality rate 0.3%). The cause of death was acute myocardial infarction. Major postoperative complications are shown in Table 1.
Table 1.
Major postoperative complications (n = 352)
There were 202 men and 150 female with a median age of 62.9 years (range, 20-92 years). The median BMI was 24.2 kg/m2 (range, 16-33 kg/m2). One hundred fifty-four patients (43.8%) had comorbidity. The most common comorbidities were hypertension (138 patients, 39.2%), diabetes (18 patients, 5.1%), heart problem (7), pulmonary (6), liver cirrhosis (5) and others. Mean length of hospital stay was 8.2 days (range, 3-22 days).
Table 2 shows the results of the univariate and multivariate analyses for factors potentially contributing to postoperative complications. Age, sex, underlying disease and American Statistical Association (ASA) class were not risk factors for complication. Smoking was a significant risk factor of morbidity (18.4% vs. 44.1%, P = 0.001). Tumor location and stage were not risk factors for postoperative complication. The mean operative time was 283 ± 95 minutes. Operative time and laparoscopic procedure were not independent factors for postoperative complication.
Table 2.
Univariate and multivariate analyses for factors potentially contributing to postoperative complication
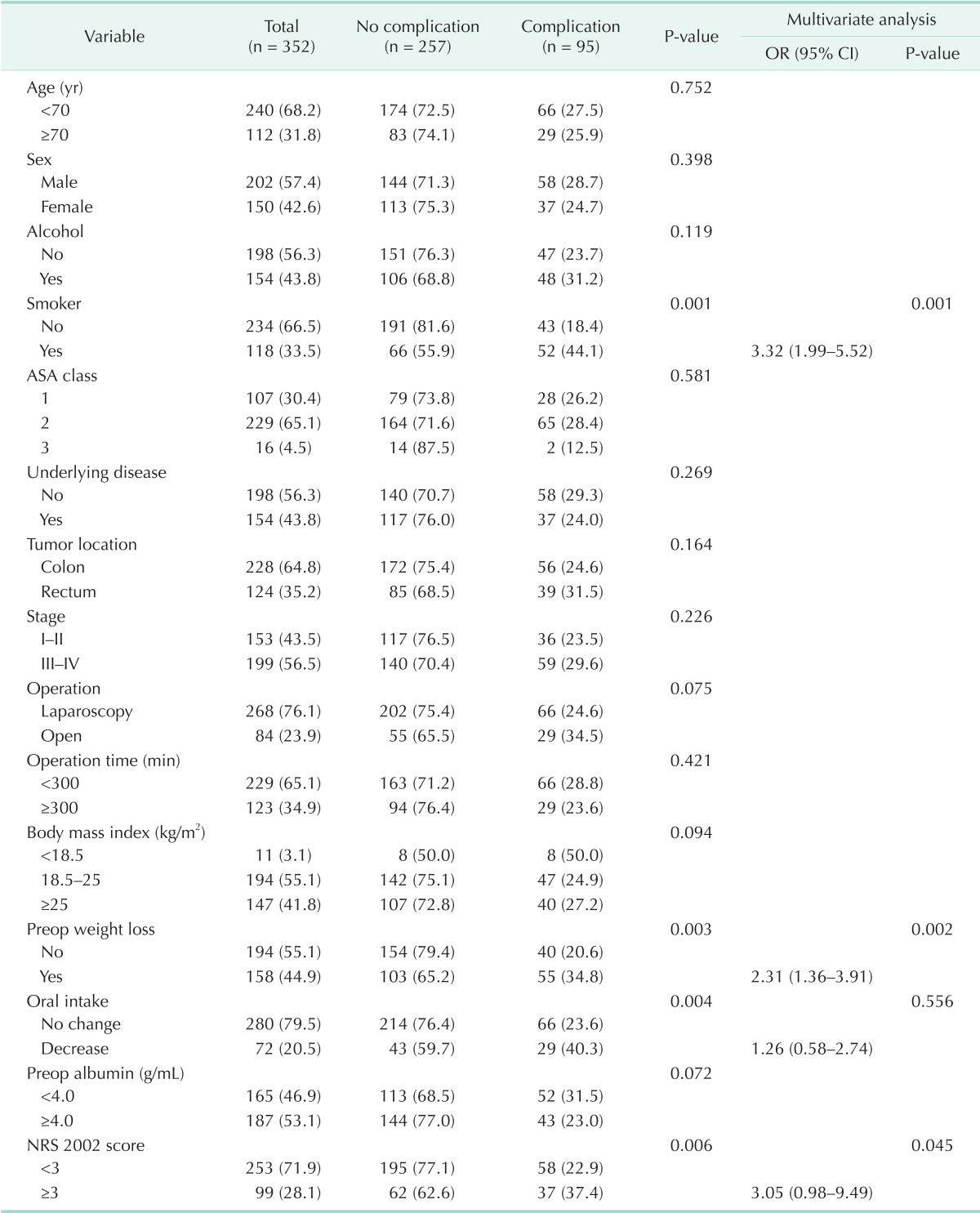
Values are presented as number (%).
OR, odds ratio; CI, confidence interval; Preop, preoperative; NRS, nutritional risk screening.
The prevalence of patients at nutritional risk in this surgical population was 99 (28.1%) with NRS 2002. NRS 2002 was used to classify nutritional risk, the complication rate was higher for patients at risk and those not at risk (37.4% [37 of 99] vs. 22.9% [58 of 253], P = 0.006). BMI and serum albumin were not risk factors of postoperative complication. Weight loss and decrease of food oral intake were risk factors of postoperative complication (20.6% vs. 34.8%, P = 0.003 and 23.6% vs. 40.3%, P = 0.004). Multivariate analysis indicated that malnutrition (odds ration [OR], 3.05; P = 0.045), heavy smoking (OR, 3.32; P = 0.001) and weight loss (OR, 2.31; P = 0.002) were independent risk factors influencing postoperative complications.
The postoperative hospital stays were longer in the nutritional risk group (8.9 ± 4.2 days) than in the no risk group (7.8 ± 3.5 days) (P = 0.019). Results of analysis of the relationship between risk factors for postoperative complication and duration of hospital stays are detailed in Table 3.
Table 3.
The length of hospital stays and risk factors for postoperative complication
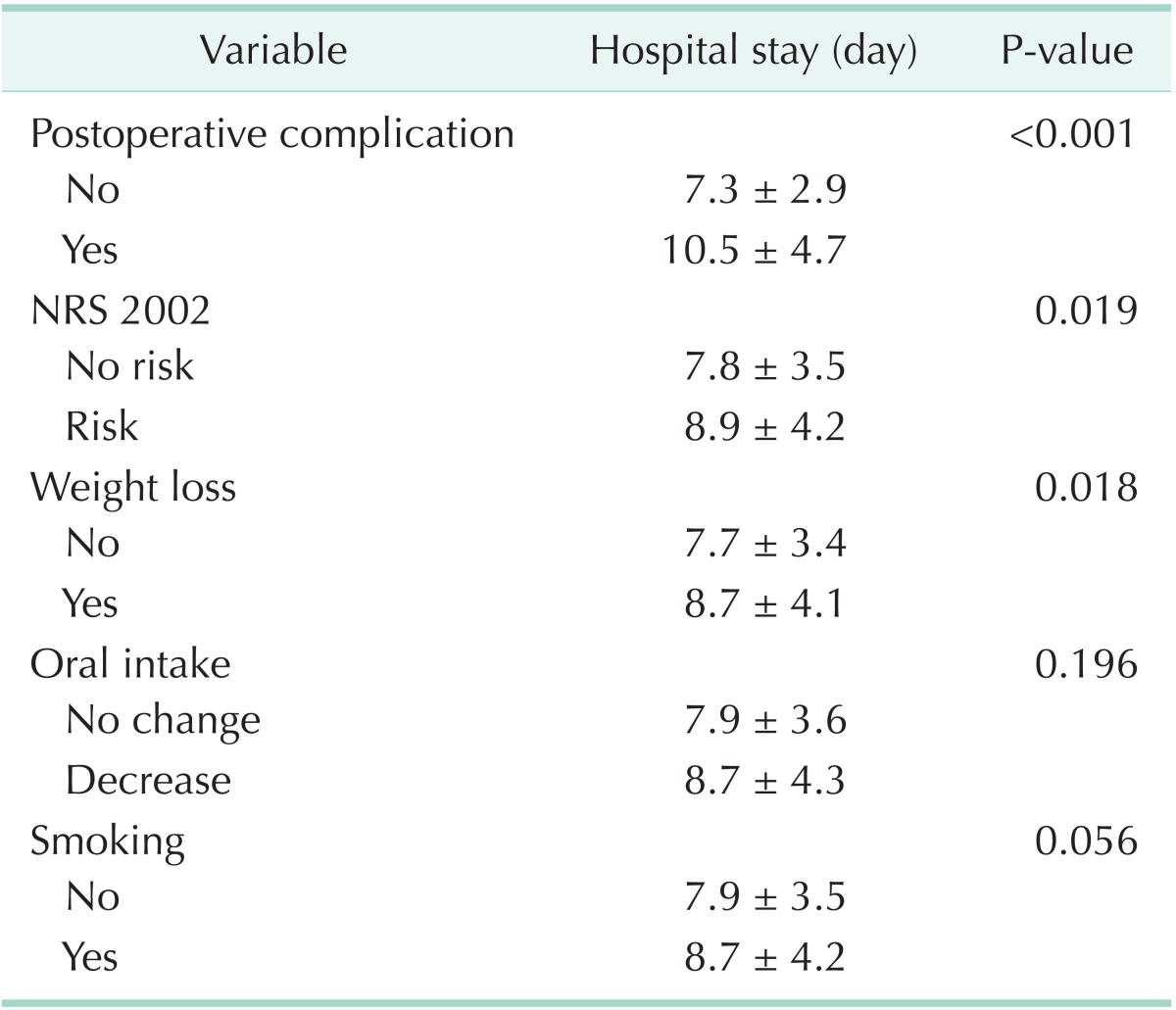
Values are presented as mean ± standard deviation.
NRS, nutritional risk screening.
The relationship between malnutrition and each complication are shown in Table 4. Malnutrition was an independent risk factor for anastomotic leakage (P = 0.027) and wound infection (P = 0.01).
Table 4.
Postoperative complications by malnutrition
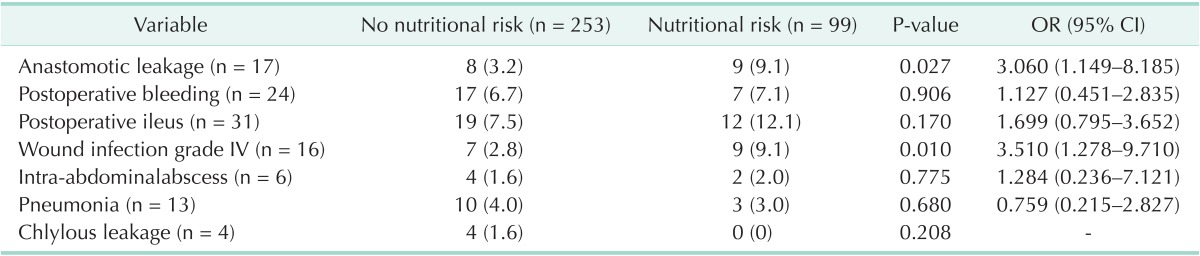
Values are presented as number (%).
OR, odds ratio; CI, confidence interval.
DISCUSSION
In this study, the overall morbidity rate was 27.0% and the mortality rate was 0.3% after elective surgery for colorectal cancer. This study supports the finding that measurements of nutritional risk can predict postoperative outcomes. NRS 2002 was a statistically significant predictor of morbidity. Similar to the present findings, a recent prospective study demonstrated that the NRS 2002 was successful in predicting postoperative complications in 186 patients undergoing elective surgery for colorectal cancer (OR, 2.43) [10]. The authors reported a nutritional risk prevalence of 39.2% in patients with NRS 2002, was higher to the data here.
Hendry et al. [11] reported that morbidity was related to ASA III-IV (P = 0.004), male sex (P = 0.023) and rectal surgery (P = 0.002) in which 1,035 patients underwent colorectal surgery. And, this study demonstrated that low BMI is not an independent risk factor. However, there are clear limitations to the use of BMI for screening nutritional status. Some patients weigh less than is usual for their height but are otherwise fit and healthy, and a normal BMI does not exclude the presence of malnutrition.
The largest prospective randomized trial of preoperative total parenteral nutrition (TPN) was a multiinstitutional study conducted by the Veterans Administration [12]. Only in severely malnourished patients, significantly fewer nonseptic complications (e.g., anastomotic leaks, bronchopleural fistulas) occurred in patients receiving TPN (5% vs. 43%, P = 0.03). Shukla et al. [13] studied 110 patients with benign or malignant gastrointestinal, breast, or oropharyngeal disease by comparing preoperative enteral nutrition with standard oral diets in patients undergoing major surgical procedures. Control patients received a standard oral diet and were compared to patients receiving 10 days of nasogastric enteral nutrition. Major complications were reduced from 30% in the control group to 10% in the enteral nutrient group in this study.
A recent meta-analysis of 107 studies reported that preoperative smoking was found to be associated with an increased risk of the following postoperative complications: general morbidity, wound complications, general infections, pulmonary complications, neurological complications, and admission to the intensive care unit [14]. Another meta-analysis of 140 studies investigated preoperative smoking and postoperative wound healing complications and found a higher risk of wound healing complications among smokers than among nonsmokers and smoking cessation intervention reduced surgical site infections (OR, 0.43; 95% confidence interval [CI], 0.21-0.85) [15]. In the present study, we confirmed that smoking was a high risk factor for ileus, wound infection, intra-abdominal abscess, pneumonia and anastomotic leakage.
Malnutrition was found to be associated with a significant risk of anastomotic leakage and wound infection. Zhu et al. [16] reported that preoperative malnutrition increased the rate of anastomotic leakage in which 132 patients underwent low anterior resection. In the series by Zhu et al. [16], anastomotic leakage increased hospital length and cost. Kang et al. [17] further supported this finding that malnutrition (OR, 2.81; 95% CI, 2.32-3.40), on multivariate analysis, was an independent risk factor for anastomotic leakage after anterior resection for rectal cancer in 72,055 patients. Putwatana et al. [18] reported that malnutrition is an important risk factor for postoperative infectious and wound complications in patients undergoing major surgery.
In conclusion, the present study has demonstrated that patients at nutritional risk have higher complication rates after surgery for colorectal cancer. Especially, malnutrition increases the rate of anastomotic leakage and wound infection. Malnutrition was also a significant risk factor for the length of hospital stay. A large scaled prospective study of whether supplementing nutritional deficits reduces postoperative complication rates is required. It is expected that NRS 2002 would be helpful in screening malnutrition.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Hill AG, Hill GL. Metabolic response to severe injury. Br J Surg. 1998;85:884–890. doi: 10.1046/j.1365-2168.1998.00779.x. [DOI] [PubMed] [Google Scholar]
- 2.Shulkin DJ, Kinosian B, Glick H, Glen-Puschett C, Daly J, Eisenberg JM. The economic impact of infections: an analysis of hospital costs and charges in surgical patients with cancer. Arch Surg. 1993;128:449–452. doi: 10.1001/archsurg.1993.01420160091015. [DOI] [PubMed] [Google Scholar]
- 3.Schiesser M, Kirchhoff P, Muller MK, Schafer M, Clavien PA. The correlation of nutrition risk index, nutrition risk score, and bioimpedance analysis with postoperative complications in patients undergoing gastrointestinal surgery. Surgery. 2009;145:519–526. doi: 10.1016/j.surg.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 4.Beattie AH, Prach AT, Baxter JP, Pennington CR. A randomised controlled trial evaluating the use of enteral nutritional supplements postoperatively in malnourished surgical patients. Gut. 2000;46:813–818. doi: 10.1136/gut.46.6.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mourao F, Amado D, Ravasco P, Vidal PM, Camilo ME. Nutritional risk and status assessment in surgical patients: a challenge amidst plenty. Nutr Hosp. 2004;19:83–88. [PubMed] [Google Scholar]
- 6.Bozzetti F, Gavazzi C, Miceli R, Rossi N, Mariani L, Cozzaglio L, et al. Perioperative total parenteral nutrition in malnourished, gastrointestinal cancer patients: a randomized, clinical trial. JPEN J Parenter Enteral Nutr. 2000;24:7–14. doi: 10.1177/014860710002400107. [DOI] [PubMed] [Google Scholar]
- 7.La Torre M, Ziparo V, Nigri G, Cavallini M, Balducci G, Ramacciato G. Malnutrition and pancreatic surgery: prevalence and outcomes. J Surg Oncol. 2013;107:702–708. doi: 10.1002/jso.23304. [DOI] [PubMed] [Google Scholar]
- 8.Kondrup J, Rasmussen HH, Hamberg O, Stanga Z Ad Hoc ESPEN Working Group. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22:321–336. doi: 10.1016/s0261-5614(02)00214-5. [DOI] [PubMed] [Google Scholar]
- 9.Johansen N, Kondrup J, Plum LM, Bak L, Norregaard P, Bunch E, et al. Effect of nutritional support on clinical outcome in patients at nutritional risk. Clin Nutr. 2004;23:539–550. doi: 10.1016/j.clnu.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 10.Schwegler I, von Holzen A, Gutzwiller JP, Schlumpf R, Muhlebach S, Stanga Z. Nutritional risk is a clinical predictor of postoperative mortality and morbidity in surgery for colorectal cancer. Br J Surg. 2010;97:92–97. doi: 10.1002/bjs.6805. [DOI] [PubMed] [Google Scholar]
- 11.Hendry PO, Hausel J, Nygren J, Lassen K, Dejong CH, Ljungqvist O, et al. Determinants of outcome after colorectal resection within an enhanced recovery programme. Br J Surg. 2009;96:197–205. doi: 10.1002/bjs.6445. [DOI] [PubMed] [Google Scholar]
- 12.The Veterans Affairs Total Parenteral Nutrition Cooperative Study Group. Perioperative total parenteral nutrition in surgical patients. N Engl J Med. 1991;325:525–532. doi: 10.1056/NEJM199108223250801. [DOI] [PubMed] [Google Scholar]
- 13.Shukla HS, Rao RR, Banu N, Gupta RM, Yadav RC. Enteral hyperalimentation in malnourished surgical patients. Indian J Med Res. 1984;80:339–346. [PubMed] [Google Scholar]
- 14.Grønkjær M, Eliasen M, Skov-Ettrup LS, Tolstrup JS, Christiansen AH, Mikkelsen SS, et al. Preoperative smoking status and postoperative complications: a systematic review and meta-analysis. Ann Surg. 2014;259:52–71. doi: 10.1097/SLA.0b013e3182911913. [DOI] [PubMed] [Google Scholar]
- 15.Sorensen LT. Wound healing and infection in surgery. The clinical impact of smoking and smoking cessation: a systematic review and meta-analysis. Arch Surg. 2012;147:373–383. doi: 10.1001/archsurg.2012.5. [DOI] [PubMed] [Google Scholar]
- 16.Zhu QL, Feng B, Lu AG, Wang ML, Hu WG, Li JW, et al. Laparoscopic low anterior resection for rectal carcinoma: complications and management in 132 consecutive patients. World J Gastroenterol. 2010;16:4605–4610. doi: 10.3748/wjg.v16.i36.4605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kang CY, Halabi WJ, Chaudhry OO, Nguyen V, Pigazzi A, Carmichael JC, et al. Risk factors for anastomotic leakage after anterior resection for rectal cancer. JAMA Surg. 2013;148:65–71. doi: 10.1001/2013.jamasurg.2. [DOI] [PubMed] [Google Scholar]
- 18.Putwatana P, Reodecha P, Sirapo-ngam Y, Lertsithichai P, Sumboonnanonda K. Nutrition screening tools and the prediction of postoperative infectious and wound complications: comparison of methods in presence of risk adjustment. Nutrition. 2005;21:691–697. doi: 10.1016/j.nut.2004.10.015. [DOI] [PubMed] [Google Scholar]


