Abstract
Angiomyxoma is a rare tumour found predominantly in pelvis of young females. Less than 150 cases have been reported, more than 90% in females and only few cases in males. Its surgical excision is a big challenge and usually leads to recurrence due to incomplete excision. We report a case of retrovesical Angiomyxoma in an elderly male. The aim of this report is to highlight the rarity of this disease, especially in males, and robotic assisted excision as an evolving option of treatment.
Keywords: Angiomyxoma, retrovesical, robotic assistance
INTRODUCTION
Angiomyxomas are benign, locally infiltrative mesenchymal neoplasms with a predilection for the female pelvis and perineum in their reproductive age group. These tumours often reach too large dimensions before becoming clinically symptomatic and they usually tend to recur after excision. Accurate preoperative diagnosis should alert the surgeon to the need for wide excision, which is essential for prevention of local recurrence.[1] This is easily done with robotic assistance due to its advantages like three dimentional vision and advanced degree of freedom within the pelvic cavity. Angiomyxoma presenting as retrovesical tumor in a male patient has only once been reported.[2] We report here a similar case presenting as a retrovesical tumor in a male patient, which was excised with robotic assistance.
CASE REPORT
A 62-years-old male presented to us with mild obstructive lower urinary tract symptoms (LUTS) since last 1 year, with a history of acute retention of urine 3 month back with failed catheter free trial. He underwent holmium laser enucleation of prostate (HOLEP) elsewhere with histopathology reporting as benign prostatic hyperplasia. Patient failed to void after catheter removal and on further evaluation he was found to have pelvic mass. Digital rectal examination revealed a cystic mass simulating benign prostatic hyperplasia (grade 3). Transrectal ultrasonography showed a heterogeneous mass arising from prostate. Magnetic resonance imaging (MRI) pelvis revealed a well-marginated lesion within the prostate gland resulting into significant prostatomegaly with no extra prostatic extension [Figure 1]. Transrectal biopsy was done, which was inconclusive with no identifiable prostatic tissue. In view of discrepancy between MRI report and biopsy report we performed cystoscopy which showed a hump in the prostatic urethra extending into the trigone, with prostatic lobes not visible (because of previous HOLEP). Hence he was planned for Robotic assisted excision of the mass. Intraoperatively a globular mass was present posterior to bladder. Mass was densely adherent to the posterior wall of the bladder. Complete excision of the mass was done. Tumor was ~6 cm × 4 cm × 2.5 cm in size [Figure 2]. We were not able to separate the mass from bladder due to difficulty in entering into proper plane. Hence we opened bladder deliberately and resected from within the bladder, closed cystostomy and drained bladder. Histo-pathological examination [Figure 3] revealed moderately cellular tumor composed of sheets of spindle to stellate shaped cells with vascular channels in between. On immunohistochemistry cells were positive for desmin, focal positivity with smooth muscle antibody (SMA), S100 and Ki-67. The results are suggestive of angiomyxoma. Patient is on regular follow-up with no recurrence until date.
Figure 1.
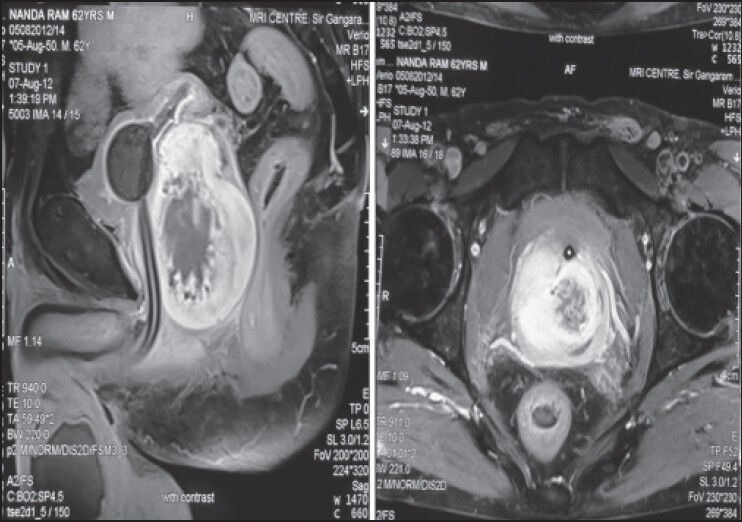
magnetic resonance imaging showing a well-marginated lesion within the prostate gland resulting into significant prostatomegaly, with no extra prostatic extension.
Figure 2.
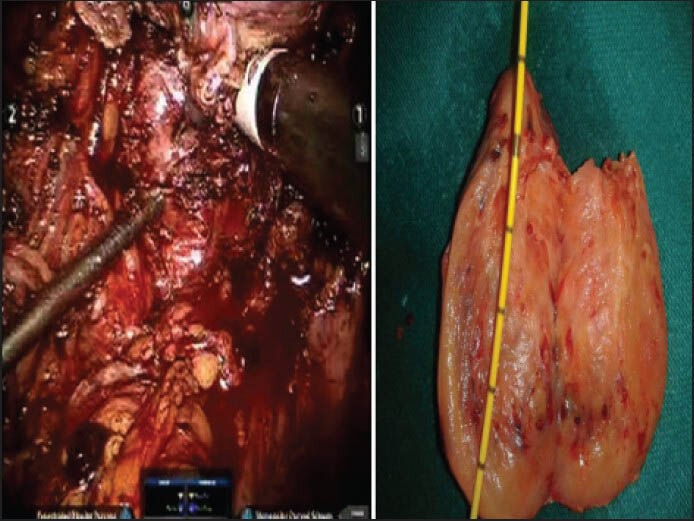
Intra operative still photograph of the mass (tip of suction tube). Also gross specimen of the tumor with gelatinous appearance and size of ~6 cm × 4 cm × 2.5 cm.
Figure 3.
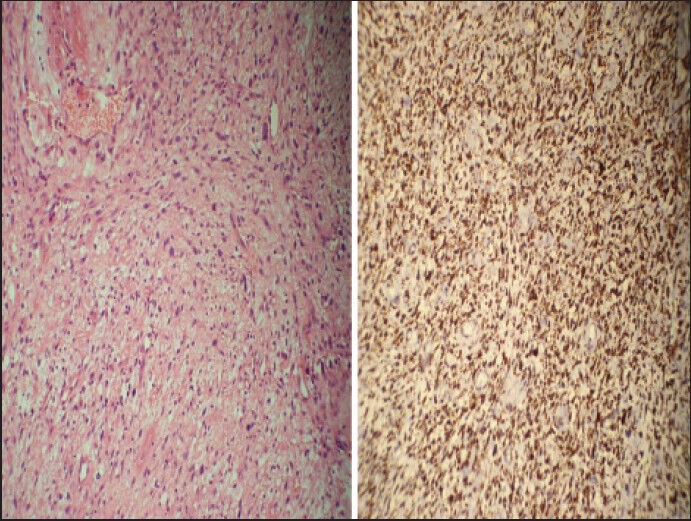
Histopathology revealed moderately cellular tumor composed of sheets of spindle to stellate shaped cells with vascular channels in between. On immunohistochemistry cells were positive for desmin, focal positivity with smooth muscle antibody, S100 and Ki-67. The results are suggestive of angiomyxoma.
DISCUSSION
Aggressive angiomyxoma was first described in 1983 by Steeper and Rosai, and fewer than 150 cases have been reported in the world medical literature. It is a soft-tissue tumour of the pelvis and perineum. The recurrence rate is high, and often extensive resections are performed with considerable morbidity.[1] In men, the tumour involves analogous sites including the scrotum and inguinal area and usually appears at an older age.[3] There might be a relation with hormonal status that might explain a female to male ratio of slightly more than 6:1. These lesions are characterized as soft, non-encapsulated tumours with finger-like projections infiltrating the surrounding soft-tissues. The tumour presents as a large multilobular or polypoid mass or swelling. Grossly, it looks rubbery and white or soft and gelatinous. The tumour grows slowly and is benign as suggested by the histology and by the fact that it shows no tendency to metastasize.[4] The low attenuation at unenhanced computed tomography (CT) and high signal intensity at T2-weighted MRI are consistent with a myxoid matrix, high water content within the mass, or both. The enhancement of T1-weighted MRI after administration of gadolinium is related to the vascularity of aggressive angiomyxoma.[5] There is no evidence of gross fat within the mass, which distinguishes this tumor from other fat-containing tumors that also occur in the pelvis of women.[6] Surgery is usually the first line of treatment (open, laparoscopic or robotic assisted), radical surgery with wide margins and long-term follow-up is advised. Hormonal suppression seems to be a plausible treatment option because these tumours occur predominantly in premenopausal women of reproductive age, may grow rapidly during pregnancy and have been shown to express immunohistochemical positivity for oestrogen and progesterone receptors.[7] Their surgery is challenging because of the infiltration and the difficult dissection. In the past, most authors advocated wide excision along with genito-urinary and digestive tract resections if necessary. Laparoscopic approach has been reported by Mera-Velasco et al.[8] and most recently robotic assisted laparoscopic excision has been promising, as seen in our case.
CONCLUSION
Male angiomyxoma, athough a rare benign tumour, should be considered in the diferential diagnosis of pelvic mass in a male patient presenting with severe obstructive LUTS, and robotic assisted excision should be utilised wherever available.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Juan AM, Manuel BJ, María JT, María de CP, Virginia GC, Antonio MO. Aggressive angiomyxoma: An unusual female pelvic tumour. Report of three cases and review of the literature. Surg Sci. 2010;1:40–5. [Google Scholar]
- 2.Hatano K, Tsujimoto Y, Ichimaru N, Miyagawa Y, Nonomura N, Okuyama A. Rare case of aggressive angiomyxoma presenting as a retrovesical tumor. Int J Urol. 2006;13:1012–4. doi: 10.1111/j.1442-2042.2006.01463.x. [DOI] [PubMed] [Google Scholar]
- 3.Behranwala KA, Thomas JM. ‘Aggressive’ angiomyxoma: A distinct clinical entity. Eur J Surg Oncol. 2003;29:559–63. doi: 10.1016/s0748-7983(03)00104-5. [DOI] [PubMed] [Google Scholar]
- 4.Wiser A, Korach J, Gotlieb WH, Fridman E, Apter S, Ben-Baruch G. Importance of accurate preoperative diagnosis in the management of aggressive angiomyxoma: Report of three cases and review of the literature. Abdom Imaging. 2006;31:383–6. doi: 10.1007/s00261-005-0378-5. [DOI] [PubMed] [Google Scholar]
- 5.Outwater EK, Marchetto BE, Wagner BJ, Siegelman ES. Aggressive angiomyxoma: Findings on CT and MR imaging. AJR Am J Roentgenol. 1999;172:435–8. doi: 10.2214/ajr.172.2.9930798. [DOI] [PubMed] [Google Scholar]
- 6.Sarah TS, Shirley MM. Aggressive angiomyxoma. Radiology. 2004;233:697–9. doi: 10.1148/radiol.2333021670. [DOI] [PubMed] [Google Scholar]
- 7.Onaitis M, Ludwig K, Perez-Tamayo A, Gottfried M, Russell L, Shadduck P, et al. The Kraske procedure: A critical analysis of a surgical approach for mid-rectal lesions. J Surg Oncol. 2006;94:194–202. doi: 10.1002/jso.20591. [DOI] [PubMed] [Google Scholar]
- 8.Mera Velasco S, Cabello Burgos AJ, Ruiz López M, González Poveda I, Santoyo Santoyo J. Laparoscopic resection of an aggressive pelvic angiomyxoma. Cir Esp. 2010;88:121–2. doi: 10.1016/j.ciresp.2009.07.006. [DOI] [PubMed] [Google Scholar]


