Abstract
Scar formation is an inevitable consequence of wound healing from either a traumatic or a surgical intervention. The aesthetic appearance of a scar is the most important criteria to judge the surgical outcome. An understanding of the anatomy and wound healing along with experience, meticulous planning and technique can reduce complications and improve the surgical outcome. Scar revision does not erase a scar but helps to make it less noticeable and more acceptable. Both surgical and non-surgical techniques, used either alone or in combination can be used for revising a scar. In planning a scar revision surgeon should decide on when to act and the type of technique to use for scar revision to get an aesthetically pleasing outcome. This review article provides overview of methods applied for facial scar revision. This predominantly covers surgical methods.
KEYWORDS: Scar revision, surgical scar revision, W-plasty, Z-plasty
INTRODUCTION
The origin of the word ‘scar’ can be traced to Greek word “eskhara” (in French “escharre”). The word ‘scar’ was first used in English in the 14th century.
A scar can be defined as a fault or blemish resulting from some former condition, wound, sore or burn. Scar formation is an inevitable consequence of wound healing in which the normal skin is replaced by a fibrous tissue. This scar tissue lacks the characteristics of the normal uninjured skin.
As per the International Advisory Panel on Scar Management, scar is classified into mature scar, immature scar, linear hypertrophic scar, widespread hypertrophic scar, minor keloid and major keloid. This review covers management issues related to only scars and not keloids.
ASSESSMENT OF SCAR
There are a large number of tools available for scar assessment. The most important features which should be assessed are: colour, vascularity, light reflection, texture, contour, pliability, height, distortion, relation to the relaxed skin tension lines (RSTLs) [Figure 1] and relation with important landmarks in the area of the body.
Figure 1.

Exaggerated wrinkle lines in a patient with Muir-Torre Syndrome depicting relaxed skin tension lines
The various subjective scar assessment tools are:
Vancouver burn scar assessment score — limited application to burn scars only.[1]
Clinical scar assessment scale — validated compared to histological findings and is applicable to a wide variety of scars.[2]
MCFONTZL classification — complex system of classification of facial lacerations.[3]
Patient and Observer Scar Assessment Scale — it has both an observer and a patient scale.[4]
Histological scar assessment requires biopsy of the scar and assessment of orientation of the collagen fibres in the scar.
The various objective scar assessment tools are:
Colour — spectrophotometry
Vascularity — laser Doppler flowmeter
Contour — optical or mechanical profilometers
Area — 3-D computer reconstruction of scanned images of scar
Thickness — ultrasonography
Tissue stiffness — anisotropy using noninvasive sound waves
These objective methods are for research purposes and not commonly used in clinical practice.
The ideal scar
The characteristics of an ideal scar which makes it cosmetically favourable are:[5]
It should be an imperceptible fine line
It should be parallel to skin creases, folds and RSTLs [Figure 1]
It should have similar colour and contour as the surrounding skin
There should be no distortion of the adjacent structures[6]
It should be at the level of the skin
It should be well-positioned on the face (peripherally located, at transition between two cosmetic units or directly in the midline)[7]
A scar that limits the mobility is functionally unfavourable. Less than ideal scars may be wide, erythematous or pigmented, raised or depressed or may transect natural creases, folds and junctions. The goal of scar revision is to create an ideal scar.
The various factors which should be considered before doing scar revision are:
-
Patients with unrealistic expectation
It is important to explain to the patient that scar revision will improve and not erase the scar and it may require multiple surgical procedures along with adjunct treatment in order to obtain an optimal result over a period of many months or years.
-
Time of scar revision
Due to continuous collagen remodelling it takes around 12-18 months for the scar to mature and gain tensile strength of 70-80% of uninjured skin. Immature scars are prone to hypertrophy and give poor results after scar revision.[8] Adjunct treatments like use of silicone sheet and intralesional steroid injections can be given during this period. However, if early intervention is needed it is wiser to do it only after 8-12 weeks in adults and 6 months in children smaller than 7 years of age.
-
Nutritional status and medical history of the patient
A well-balanced diet is essential for good protein synthesis. Vitamin A, C, E and zinc help in wound healing. Herbal supplements and medicines which increase bleeding should be stopped 3 days to 2 weeks before scar revision.[9] Medical conditions like diabetes mellitus and immunosuppression negatively effects wound healing.
-
Tobacco
Tobacco use causes hypoxia, thrombogenesis, vasoconstriction, aberrant cell function[10] and delays wound healing.[11,12] It is preferable to abstain the patients from smoking from 4 weeks before to 4 weeks after scar revision.
SCAR REVISION TECHNIQUES
There are both surgical and non-surgical techniques for scar management.
Non–surgical techniques
-
Camouflage
Make-up, hair, accessories like scarves and tattooing can help to camouflage the scar.
-
Topical therapy
Hyperpigmented scars can be lightened by using hydroquinone, kojic acid, alpha hydroxyl acid, hydrocortisone and retinoic acid.[7] Use of topical silicone gel or silicone sheet improves the contour, texture and the colour of the scar. Topical application of mitomycin C 0.4 mg/ml and 1 mg/ml improves hypertrophic scar and keloid.[13,14]
-
Intralesional agents
- Intralesional corticosteroids: They reduce scar formation by inhibition of inflammatory mediators, fibroblast proliferation, collagen synthesis (COL4A1 and COL7A1), TGF-β1 and β2 and by enhancing collagen degradation. In hypertrophic scars, 0.1 ml of low dose (5-10 mg/ml) triamcinolone acetonide is injected into the bulkiest area of the scar at 3-weeks interval for a maximum of 6 injections and is started 1 month post-operatively. This treatment does not decrease the width of the scar, but helps to flatten it. Although studies have shown the efficacy of monotherapy with intralesional triamcinolone to be 50-100%, these studies lacked standardised controls and objective measures of scar outcome.[15,16,17] Adverse effects like hypopigmentation, atrophy, telangiectasia, delayed wound healing and scar widening has been reported in 63% patients.[17,18] When used in combination with other modalities like 5-flurouracil and pulsed dye laser, adverse effects due to corticosteroids were reduced.[17,19,20]
- Intralesional 5-Flurouracil (5-FU): Intralesional 5-FU has been shown to be effective in many studies,[21,22,23,24] though most of these studies are of limited value due to lack of adequate controls. 5-FU in combination with intralesional corticosteroids, radiation or pulse dye laser has shown good results in hypertrophic scars.[17,23,24] It acts by inhibiting fibroblast proliferation[25] and expression of TGF-β1 induced type 1 collagen gene in human fibroblast.[26] Side effects are transient hyperpigmentation, sloughing, burning sensation and pain at site of injection.
- Others: agents such as intralesional bleomycin,[27,28] intralesional interferon, hyaluronidase,[29,30] Iathyrogenic agents, tretinoin and prostaglandins have been used for scar modification. Various studies have shown the beneficial effects of injection Botulinum toxin type A in improving the outcome for facial scars. It acts by causing temporary muscular paralysis which decreases the tension vectors on the wound edges and helps in wound healing.[31,32,33,34]
-
Cryotherapy
Cryotherapy either alone or in combination with intralesional corticosteroids or surgical excision is used in the management of hypertrophic scars and keloids.[35] Due to small sample size and inadequate controls the studies combining cryotherapy with surgical excision for hypertrophic scars and keloids are difficult to evaluate.[36,37,38] An uncontrolled study of 135 patients with 166 keloids showed improvement in 79.5% patients with 80% reduction in the volume of scar. Adverse effects like atrophic depressed scars and hypopigmentation were reported in 75% cases.[39] Intralesional cryotherapy maximises the destruction in the deeper part of the scar and minimises the damage to the epithelium.[36,40,41]
-
Non-ablative lasers
The flashlamp-pumped pulsed dye laser (585 nm) decreases the redness of the scar by destroying the blood vessels and use of lower sub-purpuric fluence (5.0-7.0 J/cm2)[7] stimulates collagen remodelling[42] and softens the scar. Treatment should be initiated at the time of suture removal.[43,44] Although numerous studies have reported its beneficial effects, majority of them lack a well-designed controls.[17,45,46] Post-treatment purpura[47] and hyperpigmentation were seen in 1-24% patients.[20]
-
Ablative laser resurfacing
Pulsed carbon dioxide and pulsed erbium:YAG laser cause superficial scar ablation.[48,49,50] Raised edges of the scar can be ablated using an erbium:YAG laser. Carbon dioxide laser induces collagen remodelling and wound contraction by 20-60%. Scar revision using ablative lasers can cause pigment alteration and scar deterioration from overaggressive treatment.
-
Soft tissue fillers
Bovine collagen, homologous human collagen, fat and hyaluronic acid and other synthetic fillers can be used for elevating depressed and pitted scars [Figure 2a and b].
-
Others
Electrocurrent using positive-polarity electrical stimulation, radiation therapy and pressure dressings have also been used for treating scars.[7,35]
Figure 2.

Depressed scars on face due to lupus panniculitis (left). Good improvement persisting 6 years after injection of Polyacrylamide hydrogel filler (right)
Surgical techniques for scar revision
A fundamental principle of surgical scar revision is to minimise as much as possible both incorporation and deformation of the normal tissue. Certain factors which should be kept in mind in order to obtain favourable outcome in scar revision are:[5]
-
Incision
Most commonly the incision is made perpendicular to the skin surface with the exception being the hair-bearing areas where the incision is in the direction of the hair follicle in order to prevent permanent loss of hair. Also the incision should be parallel to RSTLs.
-
Tissue handling
Atraumatic handling of the soft tissues using fine toothed tissue forceps, skin hooks, minimal manipulation and good hydration (using moist sponge) of wound margins during surgery promote wound healing and prevents excessive scarring.
-
Judicious undermining and tension-free wound repair
Undermining helps to detach the skin from the deeper tissues and allows for tension-free closure of the wound.
-
Layered wound repair
Suturing the deep dermal layer with buried knots increases the strength of the repair, causes accurate opposition of the dermis, releases the tension from the interrupted superficial sutures and allows for early superficial suture removal to prevent cross hatching.[51]
-
Suture size and needle
Smallest possible suture should be used. Suture size 5/0 or 6/0 is appropriate for face and hand and a size of 4/0 or 3/0 for trunk or limbs. For an atraumatic skin repair, a cutting or a reverse cutting needle should be used.
-
Everted wound edges
Edges can be everted by taking a larger bite of the deeper dermis while inserting the needle vertically through the skin.
-
Good haemostasis
For achieving good haemostasis, epinephrine containing local anaesthetic can be used and during the surgery, bleeding can be minimised with application of pressure or judicious use of bipolar electrocautery.[5]
The various surgical techniques of revising the scar are:
Fusiform elliptical excision
It is the most appropriate technique for revising a mature depressed or spread scar which is present along the RSTLs [Figure 1] and respects the facial subunits.[7]
In this technique a fusiform elliptical incision is made to excise the scar. The ratio of length to breadth is kept as 3:1 and the ends of the fusiform should have an angle of 30° or less in order to prevent ‘dog-ear’ formation. The ends of the fusiform are placed parallel to the RSTLs in order to promote blending.
Extramarginal scar excision involves excision of small margin of the normal tissue along with the scar in order to get normal tissue at the wound margins.
Intramarginal scar excision using serial excisions done at intervals of 6-12 weeks is used for revising a wide and/or rounded scar (caused by burn or ulcer) that cannot be excised completely in one sitting, in scars with surrounding inextensible skin and if the length of the ellipse creates an unfavourable scar. This method is particularly useful for facial scars where aim is to preserve normal skin as much as possible.
To minimise scarring in sebaceous skin, ‘tongue and groove’ effect is created by bevelling one edge of the scar and counter-bevelling the other. In tight hair bearing areas like the vertex of the scalp, serial excisions using triangulation should be performed. Triangulation allows intramarginal containment of scar and minimises excision of healthy hair-bearing scalp.[43]
Z-plasty
This technique is based on geometrical principles and is the most commonly used technique for scar revision.
This technique has several advantages: it irregularises a linear scar, making it less noticeable; changes the direction of the scars and aligns them to the RSTLs; helps in lengthening of the webbed or contracted scar; and it helps changing the position of a displaced anatomical point by elevating or depressing it.
Two components determine the performance and tissue lengthening of Z-plasty-the size of the angle and the length of the centre line of ‘Z’, called as the common diagonal (common limb or common member).[43] While doing Z-plasty, the original scar is used as the common diagonal. In the classical Z-plasty, from each end of this common diagonal, two arms of same length (in order to avoid puckering)[52] as the common diagonals are extended in opposite directions. An angle of 60° is formed between the arm and the common diagonal. This angle determines the degree of lengthening of the tissue, the larger the angle, the greater the length gain. An angle of 60° in Z-plasty gives a gain of 75% in tissue length and changes the scar direction by 90°. An angle of 30° lengthens the scar by 25%, an angle of 45° by 50%, angle of 75° by 100% and an angle of 90° by 125%.[53] An angle < 60° though easier to transpose, results in less scar lengthening and realignment of < 90°. Whereas, angle > 60° is avoided as it increases the force required for transposing the flaps, making the closure difficult.
Technique
In performing Z-plasty, the original scar as the common limb of ‘Z’ is excised and an incision is made along the two outlined arms. The wound is widely undermined at the level of subcutaneous fat in order to loosen the scar. Then the direction of the common diagonal is changed into ‘transverse diagonal’ (the new scar is perpendicular to the original scar) by simultaneously lifting the full thickness triangular flaps of equal size and transposing them [Figure 3].
Figure 3.
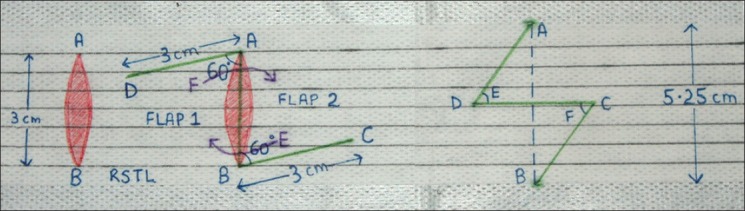
Technique of Classic Z-plasty
For correction of the contracted or asymmetric anatomical landmarks, one triangle is the anatomical point that needs to be moved while the other triangle is the point it moves to. By switching these points, the landmark is either raised or lowered.
Multiple Z-plasty: Single Z-plasty is not suitable for revision an inelastic skin and large scars as it creates significant tension at the transverse diagonal due to the longer length of the common diagonal and arms. Also a large ‘Z’ makes the scar more prominent. Hence to camouflages the Z shape, multiple Z-plasties should be done. In this a long linear scar is divided into smaller segments each of which undergo separate Z-plasty which distributes the tension across various smaller transverse diagonals.[36] Multiple Z-plasty gives the same zigzagging lines as the W-plasty; however, unlike W-plasty there is gain of length in Z-plasty. Correction of contractures and ‘pincushioning’ can be done using consecutive Z-pasties. For correction of pincushioned scar, placing the Z-plasties around the wound periphery enables interdigitation and release of contracture.
Variations of Z-plasty
Double opposing Z-plasties: In this mirror images of Z-plasty incision are made back to back and flaps of each are interposed.[53] It offers the advantage of significant lengthening in areas with limited skin availability such as release of a medial canthal web or scar contracture.
Unequal triangles (skew Z-plasty): Areas of varying skin elasticity such as the scar edges can be revised using unequal triangular flaps by changing the angle. The limb of ‘Z’ on the less elastic side is kept longer than the other one.
Half Z-plasty
It is used when the surrounding skin on one side of the scar is elastic and the other side is inelastic. Here the inelastic side is incised to release the scar and a triangular flap from the normal side is transposed to fill the defect created. This is especially useful to release scar contractures at the burn-normal skin interface.
Four flap Z-plasty (Limberg flap)
The angles of the ‘Z’ at both ends of the scar are kept 90 and then each flap is subdivided into 45 angled flaps. This 4 flap Z-plasty gives an advantage of good gain in length and is particularly helpful for releasing severe scar contractures that tether or restrict normal flexion like first web space contracture and post-burn axillary contractures.
Planimetric Z-plasty
In this the central incision of the Z-plasty is extended. It is used for scar interruption and elongation of skin on a planer surface.[53]
S-plasty
It is used for managing oval contracted scar (e.g., tracheostomy scar) when large triangular flaps are required to be transposed. Rounding of the flap ends ensure better survival.
Jumping man procedure
It is a combination of Z-plasty with V-Y advancement described to manage epicanthal fold.
W-plasty
The principle behind W-plasty is that the visibility of an irregular broken line is less due to insignificant light reflection and less easier for the eyes to follow as compared to a straight scar.[54]
Indications of W-plasy:[54]
For linear scar measuring greater than 2 cm[7] which are at an angle > 35° to the RSTLs. This makes it more prominent and causes it to spread.
Short scars present on relatively unforgiving areas like the forehead and cheeks.
Closures in pretrichial areas (following a browlift or forehead flap).
Closure over curved surfaces like the inferior mandibular border.
Disadvantages
It is not suitable for revising longer scars, as the regularity of zigzags after W-plasty would make it more noticeable. Also the excision of some normal tissue causes increase in the wound size.
Technique
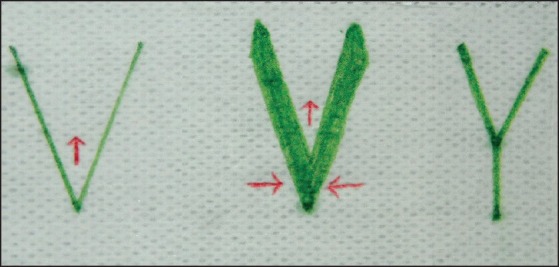
In W-plasty series of consecutive triangles are made on one side of the scar with its mirror image on the other side [Figure 4].
Figure 4.
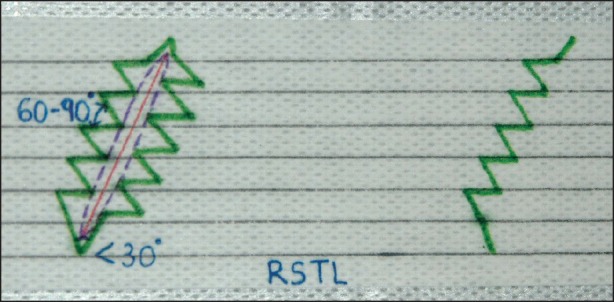
Technique of W-plasty
The ‘dots’ of the apex of the triangles are placed 5-6-mm apart from each other and at a distance of 3-5 mm from the scar. The limbs of each triangle should be 3-5-mm long as length of < 3 mm will not break the scar adequately and > 5 mm will make it more conspicuous. Ideally one arm of the triangle should be parallel to the RSTLs. The angle of the triangular apex is usually angled between 60-90° and should be determined according to the angle the scar makes with the RSTLs. In order to avoid “dog ear’ or ‘standing cone deformity’ formation, the angle at the ends of W-plasty should be < 30°.[54] To prevent extension of the incision, an M-plasty can be done at the end of the incision. After excising the scars along these lines and undermining it, re-approximation is done by interdigitating the triangles to form a single zigzag line [Figures 4–9].
Figure 9.
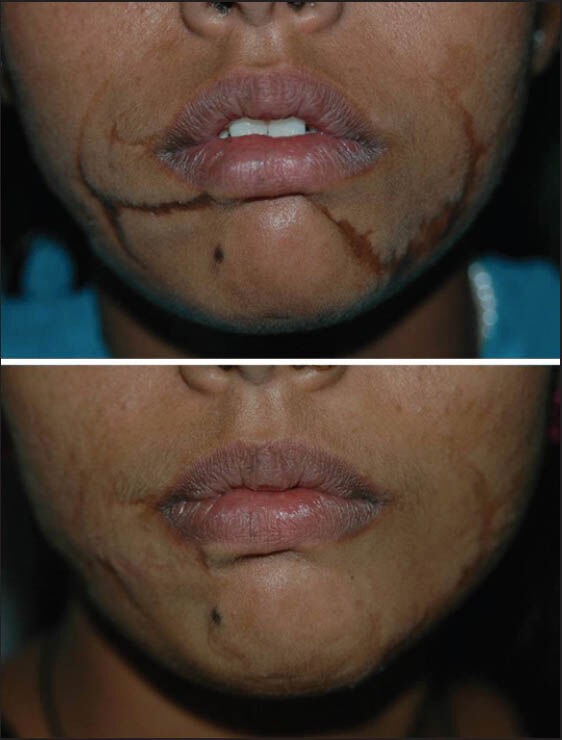
Multiple scars after repair of dog bite wound. Good improvement after multiple sessions of simple excision and W-plasty
Figure 5.

Atrophic scar on right side of face. Post-treatment scar after serial excision and W-plasty
Figure 6.

(a) Linear long atrophic scar running from the left temporal region to the chin (b) Post-treatment scar 7 days after W-plasty (c) Three months later, good improvement
Figure 7.

Hypertrophic scar of chemical burn on right side of face (Left). Post-treatment scar after W-plasty (Right)
Figure 8.

Large infraorbital atropic scar (Left). Scar was initially revised with fusiform excision (Middle). Scar was finally revised with W-plasty. There was no ectropion post-revision (Right)
GEOMETRIC BROKEN-LINE CLOSURE (GBLC)
GBLC is a more sophisticated technique for scar irregularisation and provides maximum camouflage of longer scars, more than that due to W-plasty. The irregularly irregular pattern of the incision line of GBLC is less predictable than the regularly irregular line of W-plasty due to its random twists and turns which makes it difficult for the eyes to follow. However, it is more time consuming and technically more difficult than W-plasty.[55]
Indications of GBLC are revision of relatively longer scars that are at an angle ≥ 45° to the RSTLs and scars involving a convex or a concave surface.[54]
Technique
The perimeter of the scar is marked with a marking pen. A dotted line is made at a distance of 3-6 mm from the scar margin [Figure 10].
Figure 10.
Technique of geometric broken line closure
Then on one side of the excised scar, outline is made using series of random irregular geometric designs (like semicircles, squares, rectangle and triangles) within the dotted line and the markings of RSTLs. The mirror image of this pattern is made on the other side, creating a succession of interposed flaps. Each segment should have length between 3 and 7 mm. The angle at the ends of GBLC should be < 30° and M-plasty can be done at the end of the incision. After wide undermining, re-approximation is done using dermal and subcuticular sutures to coincide the mirror images in a similar fashion to W-plasty. In order to accommodate the geometric design there may be a need to enlarge the wound.
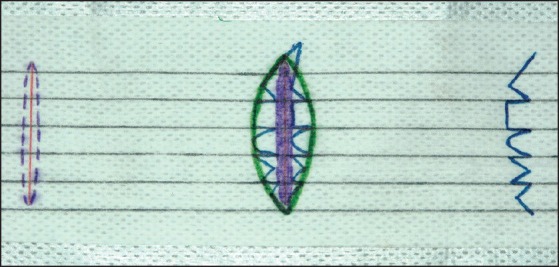
V-Y AND Y-V ADVANCEMENT
These techniques are indicated in scar lengthening in case of a small contracted scar, improving ‘trapdoor’ deformity, and elevation or depression of a free margin such as eyes and mouth in case of a scar causing ectropion or eclabion, respectively. An anatomical point can be raised using a V-Y repair and lowered using a Y-V repair.
Technique
In V-Y advancement, a V-shaped incision is made along the length of the contracted scar[43] followed by wide undermining to loosen the scar and to help in even contraction of the wound base. The V-shaped flap is pulled in the direction of ‘open’ part of the ‘V’ and the defect is closed side to side to form the ‘Y’ [Figure 11].
Figure 11.
Technique of V-Y advancement
In Y-V repair [Figure 12], after making a Y-shaped incision followed by wide undermining, it is pushed and sutured to contract it into a ‘V’ [Figure 13].
Figure 12.
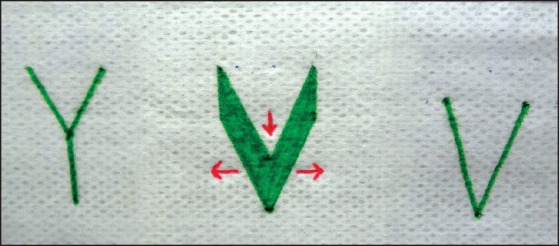
Technique of Y-V advancement
Figure 13.

Traumatic atrophic scar involving the left infraorbital region (Left). Result after scar revision done with Y-V technique (Right)
Another use of V-Y repair is closure of wound after excision of circular or oval defects especially the small defect in the hair bearing skin e.g., scalp and eyebrow. In these areas the limbs of Y are camouflaged by the presence of hair.
DERMABRASION AND MICRODERMABRASION
Dermabrasion is used for smoothing and levelling the textural abnormalities of the scar surface and its uneven edges, to improve the appearance of raised flaps and grafts and for blending the scar with its surroundings. It should ideally be done 6-8 weeks post-operatively so that it can disrupt and reorganise the late proliferative and early remodelling phase of wound healing to improve the appearance of the scar.[5] It is important to dermabrade the entire cosmetic unit or subunit and not just the scar in order to prevent the pigmentary and textural demarcation. Microdermabrasion is performed using either a pressurised stream of aluminium oxide crystals (or other abrasive particles) or by using reusable or disposable diamond tip. It causes superficial abrasion of skin, increases the epidermal turn over, stimulates and remodels the dermal collagen and may also increase the transepidermal drug delivery. It is used in the treatment of superficial acne scars.[56,57,58]
Flaps and grafts
Flaps can be used for revising large scars or scar that is located in critical location in which it is difficult to mobilise the adjacent tissue.
Surgical debulking
Surgical debulking is indicated for correction of pronounced trapdoor deformity.
Scar revision for large scars
Long linear scars, excessively wide hypertrophic and atrophic scars and scars covering large surface areas and involving significant tissue loss can be revised using serial partial excisions, tissue expansion, skin grafting, flaps and integra artificial skin.[59]
COMPLICATIONS OF SCAR REVISION AND THEIR PREVENTION/CORRECTION
Scar widening and hypertrophy
Widening of the scar can be prevented by proper placement of suture and delaying suture removal in areas prone to stretch and increased movement. Use of Steri-Strips© after suture removal helps in wound protection and approximation of skin edges. In patients prone for developing hypertrophic scars, intralesional steroid injection should be given prophylactically after scar revision.[5]
Haematoma formation
This results from inadequate haemostasis and non-obliterated dead space. In case the risk of haematoma formation is high, a small drain should be left in place.
Infection
Strict aseptic precaution and preincision use of single prophylactic antibiotic is helpful.
Wound dehiscence
This results from excessive tension of epidermal sutures and can be prevented by placing good dermal sutures to relieve the epidermal tension. Trauma to the incision after the suture removal can also cause dehiscence and this can be prevented by use of Steri-Strips© after suture removal.
Hyperpigmentation
It can be prevented by strict sun avoidance and use of sunscreens.
Keloid formation
When revising scars in patients with keloidal tendency, care must be taken during closure to minimise the tension across the wound to reduce the stimulus for keloid formation.[5] Intralesional triamcinolone should be injected immediately after closure and thereafter, at regular bimonthly intervals in the post-operative period to prevent keloid formation.
EMERGING TRENDS IN SCAR REVISION AND REDUCTION
Autologous fat grafting
Adipose stem cells have regenerative potential and can improve scars [Figure 14a and b] and the quality of the overlying tissue.[60] Animal studies have shown improvement in the scar colour and texture, increase in vascular endothelial growth factor and decrease in fibrotic markers.[61]
Figure 14.
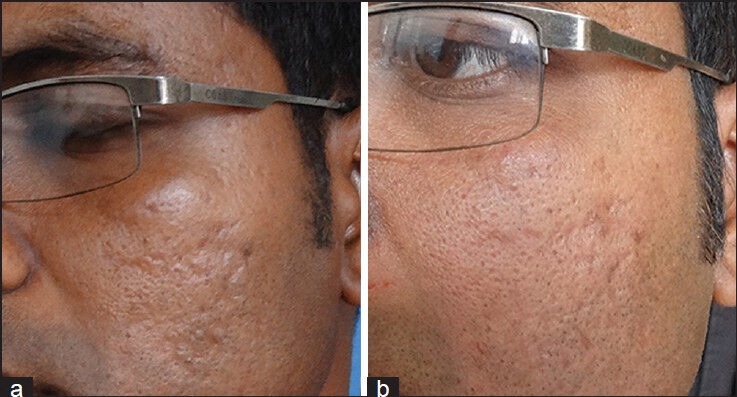
(a) Acne scars (b) Improvement in acne scars after two sessions of fat grafting done 1 month apart (Courtesy: Dr. Niti Khunger)
Gene therapy
Studies using in-vitro adenovirus mediated delivery of fibromodulin into human dermal fibroblast,[62] in-vitro infection of dermal fibroblast by adenovirus encoding a truncated TGF-β receptor II[63] and delivery of dominant negative mutant TGF-β receptor II by retrovirus into a rabbit ear model have shown improvement in wound healing and scar formation.[64]
Others
Studies have shown beneficial effects of oral minocycline given in high doses,[65,66] angiotensin converting enzyme inhibitors,[67,68] angiotensin receptor blockers,[35] topical 1% prolyl 4-hydroxylase inhibitor,[69] procollagen C-proteinase inhibitor,[70] tamoxifin,[71] topical anti-TGF-β1 and 2 antibody, exogenous TGF-β3[72] and topical celecoxib (a selective cyclooxygenase-2 inhibitor)[73] in wound healing and scar formation.
SUMMARY
Scar revision does not erase a scar but helps to make it less noticeable and more acceptable. Both surgical and non surgical techniques can be used for revising a scar. Occurrence of post-operative complications and unsightly scars can be minimised by meticulous planning, sound technique and experience. In planning a scar revision surgeon should decide on when to act and the type of technique to use for scar revision to get an aesthetically pleasing outcome.
ACKNOWLEDGEMENT
All clinical pictures except those in Figure 14 are of patients treated at Dermatosurgery Clinic at All India Institute of Medical Sciences, New Delhi. Authors thank faculty, resident doctors and nursing staff for their help in Dermatosurgery clinic.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Sullivian T, Smith J, Kermode J, McIver E, Courtemanche DJ. Rating the burn scar. J Burn Care Rehabil. 1990;11:256–60. doi: 10.1097/00004630-199005000-00014. [DOI] [PubMed] [Google Scholar]
- 2.Beausang E, Floyd H, Dunn KW, Orton CI, Ferguson MW. A new quantitative scale for clinical scar assessment. Plast Reconstr Surg. 1998;102:1954–61. doi: 10.1097/00006534-199811000-00022. [DOI] [PubMed] [Google Scholar]
- 3.Lee RH, Gamble WB, Robertson B, Manson PN. The MCFONTZL classification system for soft-tissue injuries to the face. Plast Reconstr Surg. 1999;103:1150–7. doi: 10.1097/00006534-199904040-00008. [DOI] [PubMed] [Google Scholar]
- 4.Draaijers LJ, Tempelman FR, Botman YA, Tuinebreijer WE, Middelkoop E, Kreis RW, et al. The patient and observer scar assessment scale: A reliable and feasible tool for scar evaluation. Plast Reconstr Surg. 2004;113:1960–5. doi: 10.1097/01.prs.0000122207.28773.56. [DOI] [PubMed] [Google Scholar]
- 5.Watson D, Reuther MS. Scar revision techniques-pearls and pitfalls. Facial Plast Surg. 2012;28:487–91. doi: 10.1055/s-0032-1325642. [DOI] [PubMed] [Google Scholar]
- 6.Rudolph R, Schneider G. Scar revision. In: Georgiade GS, Riefkohl R, Levin LS, editors. Plastic Maxillofacial and Reconstructive Surgery. 3rd ed. Baltimore: Williams and Wilkins; 1997. pp. 85–92. [Google Scholar]
- 7.Moran ML. Scar revision. Otolaryngol Clin North Am. 2001;34:767–80. doi: 10.1016/s0030-6665(05)70018-9. [DOI] [PubMed] [Google Scholar]
- 8.Schweinfurth JM, Fedok F. Avoiding pitfalls and unfavourable outcomes in scar revision. Facial Plast Surg. 2001;17:273–8. doi: 10.1055/s-2001-18822. [DOI] [PubMed] [Google Scholar]
- 9.Broughton G, 2nd, Crosby MA, Coleman J, Rohrich RJ. Use of herbal supplements and vitamins in plastic surgery: A practical review. Plast Reconstr Surg. 2007;119:48–66e. doi: 10.1097/01.prs.0000252661.72071.8d. [DOI] [PubMed] [Google Scholar]
- 10.Krueger JK, Rohrich RJ. Clearing the smoke: The scientific rationale for tobacco abstention with plastic surgery. Plast Reconstr Surg. 2001;108:1063–73. doi: 10.1097/00006534-200109150-00042. [DOI] [PubMed] [Google Scholar]
- 11.Rees TD, Liverett DM, Guy CL. The effect of cigarette smoking on skin-flap survival in the face lift patient. Plast Reconstr Surg. 1984;73:911–5. doi: 10.1097/00006534-198406000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Riefkohl R, Wolfe JA, Cox EB, McCarty KS., Jr Association between cutaneous occlusive vascular diseases, cigarette smoking, and skin slough after rhytidectomy. Plast Reconstr Surg. 1986;77:592–5. doi: 10.1097/00006534-198604000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Cupp C, Gaball CW. Utilizing topical therapies and mitomycin to reduce scars. Facial Plast Surg. 2012;28:513–7. doi: 10.1055/s-0032-1325645. [DOI] [PubMed] [Google Scholar]
- 14.Sanni A, Ikponmwosa S, Golio D, Tehrani K. The use of mitomycin C and keloid scar recurrence. Plast Reconstr Surg. 2010;156:682–6. [Google Scholar]
- 15.Tang YW. Intra and postoperative steroid injection for keloid and hypertrophic scars. Br J Plast Surg. 1992;45:371–3. doi: 10.1016/0007-1226(92)90007-k. [DOI] [PubMed] [Google Scholar]
- 16.Darzi MA, Chowdri NA, Kaul SK, Khan M. Evaluation of various methods of treating keloids and hypertrophic scars: A 10-year follow-up study. Br J Plast Surg. 1992;45:374–9. doi: 10.1016/0007-1226(92)90008-l. [DOI] [PubMed] [Google Scholar]
- 17.Manuskiatti W, Fitzpatrick RE. Treatment response of keloidal and hypertrophic sternotomy scars: Comparison among intralesional corticosteroid, 5-fluorouracil, and 585-nm flashlamp pumped pulsed-dye laser treatments. Arch Dermatol. 2002;138:1149–55. doi: 10.1001/archderm.138.9.1149. [DOI] [PubMed] [Google Scholar]
- 18.Marguire HC., Jr Treatment of keloids with triamcinolone acetonide injected intralesionally. JAMA. 1956;192:325–6. doi: 10.1001/jama.1965.03080170053019. [DOI] [PubMed] [Google Scholar]
- 19.Asilian A, Darougheh A, Shariati F. New combination of triamcinolone, 5-florouracil, and pulsed-dye laser for treatment of keloid and hypertrophic scars. Dermatol Surg. 2006;32:907–15. doi: 10.1111/j.1524-4725.2006.32195.x. [DOI] [PubMed] [Google Scholar]
- 20.Alster TS. Laser scar revision: Comparison study of 585-nm pulsed dye laser with and without intralesional corticosteroids. Dermatol Surg. 2003;29:25–9. doi: 10.1046/j.1524-4725.2003.29024.x. [DOI] [PubMed] [Google Scholar]
- 21.Fitzpatrick RE. Treatment of inflamed hypertrophic scars using intralesional 5-FU. Dermatol Surg. 1999;25:224–32. doi: 10.1046/j.1524-4725.1999.08165.x. [DOI] [PubMed] [Google Scholar]
- 22.Kontochristopoulos G, Stefanaki C, Panagiotopoulos A, Stefanaki K, Argyrakos T, Petridis A, et al. Intralesional 5-flurouracil in the treatment of keloids: An open clinical and histopathological study. J Am Acad Dermatol. 2005;52:474–9. doi: 10.1016/j.jaad.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 23.Gupta S, Kalra A. Efficacy and safety of intralesional 5-fluorouracil in the treatment of keloids. Dermatology. 2002;204:130–2. doi: 10.1159/000051830. [DOI] [PubMed] [Google Scholar]
- 24.Nanda S, Reddy BS. Intralesional 5-fluorouracil as a treatment modality of keloids. Dermatol Surg. 2004;30:54–6. doi: 10.1111/j.1524-4725.2004.29382.x. [DOI] [PubMed] [Google Scholar]
- 25.Blumenkranz MS, Ophir A, Claflin AJ, Hajek A. Fluorouracil for the treatment of massive periretinal proliferation. Am J Ophthalmol. 1982;94:458–67. doi: 10.1016/0002-9394(82)90239-2. [DOI] [PubMed] [Google Scholar]
- 26.Wendling J, Marchand A, Mauviel A, Verrecchia F. 5-Fluorouracil blocks transforming growth factor-beta-induced alpha 2 type I collagen gene (COL1A2) expression in human fibroblasts via c-Jun NH2-terminal kinase/activator protein-1 activation. Mol Pharmacol. 2003;64:707–13. doi: 10.1124/mol.64.3.707. [DOI] [PubMed] [Google Scholar]
- 27.España A, Solano T, Quintanilla E. Bleomycin in the treatment of keloids and hypertrophic scars by multiple needle punctures. Dermatol Surg. 2001;27:23–7. [PubMed] [Google Scholar]
- 28.Lee KS, Song JY, Suh MH. Collagen mRNA expression detected by in situ hybridization in keloid tissue. J Dermatol Sci. 1991;2:316–23. doi: 10.1016/0923-1811(91)90056-4. [DOI] [PubMed] [Google Scholar]
- 29.Stucker FJ, Shaw GY. An approach to management of keloids. Arch Otolargygol Head Neck Surg. 1992;118:63–7. doi: 10.1001/archotol.1992.01880010067018. [DOI] [PubMed] [Google Scholar]
- 30.Song C, Shen W, He Q. An experimental study on compound anisodine III for softening scar of mouse skin after burn. Zhunghua Yan Ke Za Zhi. 1996;32:176–8. [PubMed] [Google Scholar]
- 31.Wilson AM. Use of Botulinum toxin type A to present widening of facial scars. Plast Reconstr Surg. 2006;117:1758–66. doi: 10.1097/01.prs.0000209944.45949.d1. [DOI] [PubMed] [Google Scholar]
- 32.Ziade M, Domergue S, Batifol D, Jreige R, Sebbane M, Goudot P, et al. Use of botulinum toxin type A to improve treatment of facial wounds: A prospective randomised study. J Plast Reconstr Aesthet Surg. 2013;66:209–14. doi: 10.1016/j.bjps.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 33.Gassner HG, Brissett AE, Otley CC, Boahene DK, Boggust AJ, Weaver AL, et al. Botulinum toxin to improve facial wound healing. A prospective blinded placebo controlled study. Mayo Clin Proc. 2006;81:1023–8. doi: 10.4065/81.8.1023. [DOI] [PubMed] [Google Scholar]
- 34.Jablonka EM, Sherris DA, Gassner HG. Botulinum toxin to minimize facial scarring. Facial Plast Surg. 2012;28:525–35. doi: 10.1055/s-0032-1325641. [DOI] [PubMed] [Google Scholar]
- 35.Reish RG, Eriksson E. Scars: A review of emerging and currently available therapies. Plast Reconstr Surg. 2008;122:1068–78. doi: 10.1097/PRS.0b013e318185d38f. [DOI] [PubMed] [Google Scholar]
- 36.Har-Shai Y, Amar M, Sabo E. Intralesional cryotherapy for enhancing the involution of hypertrophic scars and keloids. Plast Reconstr Surg. 2003;111:1841–52. doi: 10.1097/01.PRS.0000056868.42679.05. [DOI] [PubMed] [Google Scholar]
- 37.Zouboulis CC, Blume U, Buttner P, Orfanos CE. Outcomes of cryosurgery in keloids and hypertrophic scars: A prospective consecutive trial of case series. Arch Dermatol. 1993;129:1146–51. [PubMed] [Google Scholar]
- 38.Rusciani L, Rossi G, Bono R. Use of cryotherapy in the treatment of keloids. J Dermatol Surg Oncol. 1993;19:529–34. doi: 10.1111/j.1524-4725.1993.tb00386.x. [DOI] [PubMed] [Google Scholar]
- 39.Rusciani L, Paradisi A, Alfano C, Chiummariello S, Rusciani A. Cryotherapy in the treatment of keloids. J Drugs Dermatol. 2006;5:591–5. [PubMed] [Google Scholar]
- 40.Weshahy AH, Abdel Hay R. Intralesional cryotherapy and intralesional steroid injection: a good combination therapy for treatment of keloids and hypertrophic scars. Dermatol Ther. 2012;25:273–6. doi: 10.1111/j.1529-8019.2012.01456.x. [DOI] [PubMed] [Google Scholar]
- 41.Gupta S, Kumar B. Intralesional cryosurgery using lumbar puncture and/or hypodermic needles for large, bulky, recalcitrant keloids. Int J Dermatol. 2001;40:349–53. doi: 10.1046/j.1365-4362.2001.01117.x. [DOI] [PubMed] [Google Scholar]
- 42.Manuskiatti W, Fitzpatrick RE, Goldman MP. Energy density and numbers of treatment affect response of keloidal and hypertrophic sternotomy scars to the 585 nm PDL. J Am Acad Dermatol. 2001;45:557–65. doi: 10.1067/mjd.2001.116580. [DOI] [PubMed] [Google Scholar]
- 43.Lee KK, Mehrany K, Swanson NA. Surgical revision. Dermatol Clin. 2005;23:141–50. doi: 10.1016/j.det.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 44.Nouri K, Jimenez GP, Harrison-Balestra C, Elgart GW. 585 nm pulsed dye laser in treatment of surgical scars starting on the suture removal day. Dermatol Surg. 2003;29:65–73. doi: 10.1046/j.1524-4725.2003.29014.x. [DOI] [PubMed] [Google Scholar]
- 45.Alster TS, Williams CM. Treatment of keloid sternotomy scars with 585 nm flashlamp-pumped pulsed-dye laser. Lancet. 1995;345:1198–200. doi: 10.1016/s0140-6736(95)91989-9. [DOI] [PubMed] [Google Scholar]
- 46.Alster TS. Improvement of erythematous and hypertrophic scars by the 585 nm flash lamp pulsed dye laser. Ann Plast Surg. 1994;32:186–90. doi: 10.1097/00000637-199402000-00015. [DOI] [PubMed] [Google Scholar]
- 47.Lupton JR, Alster TS. Laser scar revision. Dermatol Clin. 2002;20:55–65. doi: 10.1016/s0733-8635(03)00045-7. [DOI] [PubMed] [Google Scholar]
- 48.Wheeland RG. Revision of full-thickness skin grafts using the carbon dioxide laser. J Dermatol Surg Oncol. 1988;14:130–4. doi: 10.1111/j.1524-4725.1988.tb03352.x. [DOI] [PubMed] [Google Scholar]
- 49.Cooper JS, Lee BT. Treatment of facial scarring: Lasers, filler, and nonoperative techniques. Facial Plast Surg. 2009;25:311–5. doi: 10.1055/s-0029-1243079. [DOI] [PubMed] [Google Scholar]
- 50.Elsaie ML, Choudhary S. Lasers for scars: A review and evidence-based appraisal. J Drugs Dermatol. 2010;9:1355–62. [PubMed] [Google Scholar]
- 51.Wu T. Plastic surgery made easy - simple techniques for closing skin defects and improving cosmetic results. Aust Fam Physician. 2006;35:492–6. [PubMed] [Google Scholar]
- 52.Salam GA, Amin JP. The basic Z-plasty. Am Fam Physician. 2003;67:2329–32. [PubMed] [Google Scholar]
- 53.Hove CR, Williams EF, 3rd, Rodgers BJ. Z-plasty: A concise review. Facial Plast Surg. 2001;17:289–94. doi: 10.1055/s-2001-18828. [DOI] [PubMed] [Google Scholar]
- 54.Rodgers BJ, Williams EF, Hove CR. W-plasty and geometric broken line closure. Facial Plast Surg. 2001;17:239–44. doi: 10.1055/s-2001-18829. [DOI] [PubMed] [Google Scholar]
- 55.Alsarraf R, Murakami CS. Geometric broken line closure. Facial Plast Surg Clin North Am. 1998;6:163–6. [Google Scholar]
- 56.Shim EK, Barnette D, Hughes K, Greenway HT. Microdermabrasion: A clinical and histopathological study. Dermatol Surg. 2001;27:524–30. doi: 10.1046/j.1524-4725.2001.01001.x. [DOI] [PubMed] [Google Scholar]
- 57.Khunger N. IADVL Task Force. Standard guidelines of care for acne scars. Indian J Dermatol Venereol Leprol. 2008;74:S28–36. [PubMed] [Google Scholar]
- 58.Karimipour DJ, Karimipour G, Orringer JS. Microdermaabrasion: An evidence-based review. Plast Reconstr Surg. 2010;125:372–7. doi: 10.1097/PRS.0b013e3181c2a583. [DOI] [PubMed] [Google Scholar]
- 59.Liotta DR, Costantino PD, Hiltzik DH. Revising large scars. Facial Plast Surg. 2012;28:492–6. doi: 10.1055/s-0032-1325649. [DOI] [PubMed] [Google Scholar]
- 60.Klinger M, Marazzi M, Vigo D, Torre M. Fat injection for cases of severe burn outcomes: A new perspective of scar remodelling and reduction. Aesthetic Plast Surg. 2008;32:465–9. doi: 10.1007/s00266-008-9122-1. [DOI] [PubMed] [Google Scholar]
- 61.Sultan SM, Barr JS, Butala P, Davidson EH, Weinstein AL, Knobel D, et al. Fat grafting accelerates revascularization and decreases fibrosis following thermal injury. J Plast Reconstr Aesthet Surg. 2012;65:219–27. doi: 10.1016/j.bjps.2011.08.046. [DOI] [PubMed] [Google Scholar]
- 62.Stoff A, Rivera AA, Mathis JM, Moore ST, Banerjee NS, Everts M, et al. Effect of adenoviral mediated overexpression of fibromodulin on human dermal fibroblasts and scar formation in full-thickness incisional wounds. J Mol Med (Berl) 2007;85:481–96. doi: 10.1007/s00109-006-0148-z. [DOI] [PubMed] [Google Scholar]
- 63.Liu W, Chua C, Wu X, Wang D, Ying D, Cui L, et al. Inhibiting scar formation in rat wounds by adenovirus-mediated overexpression of truncated TGF-β receptor II. Plast Reconstr Surg. 2005;115:860–70. doi: 10.1097/01.prs.0000153037.12900.45. [DOI] [PubMed] [Google Scholar]
- 64.Reid RR, Roy N, Mogford JE, Zimmerman H, Lee C, Mustoe TA. Reduction of hypertrophic scar via retroviral delivery of a dominant negative TGF-β receptor II. J Plast Reconstr Aesthet Surg. 2007;60:64–72. doi: 10.1016/j.bjps.2005.12.026. [DOI] [PubMed] [Google Scholar]
- 65.Henry SL, Concannon MJ, Kaplan PA, Diaz-Arias AA. The inhibitory effect of minocycline on hypertrophic scarring. Plast Reconstr Surg. 2007;120:80–8. doi: 10.1097/01.prs.0000263325.73400.f8. [DOI] [PubMed] [Google Scholar]
- 66.Yrjanheikki J, Tikka T, Keinanen R, Goldsteins G, Chan PH, Koistinaho J. A tetracycline derivative, minocycline, reduces inflammation and protects against focal cerebral ischemia with a wide therapeutic window. Proc Natl Acad Sci U S A. 1999;96:13496–500. doi: 10.1073/pnas.96.23.13496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Schnee JM, Hsueh WA. Angiotensin II, adhesion, and cardiac fibrosis. Cardiovasc Res. 2000;46:264–8. doi: 10.1016/s0008-6363(00)00044-4. [DOI] [PubMed] [Google Scholar]
- 68.Steckelings UM, Wollschlager J, Peters J, Henz BM, Hermes B, Artuc M. Human skin: Source of and target organ for angiotensin II. Exp Dermatol. 2004;13:148–54. doi: 10.1111/j.0906-6705.2004.0139.x. [DOI] [PubMed] [Google Scholar]
- 69.Kim I, Mogford JE, Witschi C, Nafissi M, Mustoe TA. Inhibition of prolyl 4-hydroxylase reduces scar hypertrophy in a rabbit model of cutaneous scarring. Wound Repair Regen. 2003;11:368–72. doi: 10.1046/j.1524-475x.2003.11509.x. [DOI] [PubMed] [Google Scholar]
- 70.Reid RR, Mogford JE, Butt R, deGiorgio-Miller A, Mustoe TA. Inhibition of procollagen C-proteinase reduces scar hypertrophy in a rabbit model of cutaneous scarring. Wound Repair Regen. 2006;14:138–41. doi: 10.1111/j.1743-6109.2006.00103.x. [DOI] [PubMed] [Google Scholar]
- 71.Mancoll JS, Macauley RL, Phillips LG. The inhibitory effect of tamoxifen on keloid fibroblasts. Surg Forum. 1996;47:718–20. [Google Scholar]
- 72.Brahmatewari J, Serafini A, Serralta V, Mertz PM, Eaglstein WH. The effects of topical transforming growth factor-beta2 and anti-transforming growth factor-beta2,3 on scarring in pigs. J Cutan Med Surg. 2000;4:126–31. doi: 10.1177/120347540000400303. [DOI] [PubMed] [Google Scholar]
- 73.Wilgus TA, Vodovotz Y, Vittadini E, Clubbs EA, Oberyszyn TM. Reduction of scar formation in full-thickness wounds with topical celecoxib treatment. Wound Repair Regen. 2003;11:25–34. doi: 10.1046/j.1524-475x.2003.11106.x. [DOI] [PubMed] [Google Scholar]


