Abstract
Context:
Port-wine stain (PWS) is one of the commonly encountered congenital cutaneous vascular lesions, with an equal sex distribution. Pulsed dye lasers (PDL) have revolutionized the treatment of both congential and acquired cutaneous vascular lesions. The pulsed dye lasers owing to its superior efficacy and safety profile have become the gold standard for the management of port-wine stains.
Aims:
To evaluate the efficacy and side effects of pulsed dye laser for the management of Port-wine stain on Indian skin.
Materials and Methods:
Seventy five patients of Fitzpatrick skin types IV&V with PWS underwent multiple treatments with PDL (V beam-Candela) over a period of six years at monthly intervals. Laser parameters were wavelength 595nm, spot sizes 7-10mm, fluence 6-12 j/cm2, pulse duration 0.45-10ms, along with cryogen cooling. Serial photographs were taken before and after every session. Clinical improvement scores of comparable photographs using a quartile grading (o=<20%, 1=21-40%, 2=41-60%, 3=61-80%, 4=>80%) were judged independently by two dermatologists after the series of treatment. Minimum number of treatments was 6 and maximum 17. They were followed up at six monthly intervals to observe re darkening of PWS.
Results:
No patient showed total clearance.Grade3 improvement was observed in 70 % of children and 50% of adults after 8-10 sessions. Children showed better and faster response than adults. Thirty percent of patients developed post inflammatory hyper pigmentation which resolved over a period of six to eight weeks. Two patients had superficial scarring due to stacking of pulses. None of the patients showed re darkening of PWS till now.
Conclusion:
Pulsed dye laser is an effective and safe treatment for port-wine stain in Indian skin.
KEYWORDS: Indian skin, port-wine stain, pulsed dye laser
INTRODUCTION
The treatment of cutanaeous vascular lesions with lasers have progressed significantly over the past 30 years. Based on the work of Anderson & Parrish in the early 1980s, several vascular specific laser systems have been developed using the principal of selective photo thermolysis. Benign vascular lesions contain abundant amounts of the chromophore oxyhaemoglobin (Oxy-Hb) which can be selectively damaged by the laser at a specific wavelength, pulse duration and fluence. Pulse dye lasers have become the mainstay of therapy for both congenital and acquired vascular lesions. Newer PDL systems with extended pulse duration allow slower, more uniform heating with little or no vessel rupture and less purpura. Hence these lasers offer excellent clinical improvement with a low risk of adverse sequelae.
Port-wine stain (PWS) is a congenital vascular anomaly which presents at birth and which tend to grow with the patient. They exhibit a normal rate of endothelial cell turn over throughout their natural history. Initially appearing as light pink macules, PWS can darken over a period of time as a result of progressive vessel ectasia. The male female ratio is 1:1 and the most common site affected is face, followed by the neck, chest and upper limbs. The incidence in general population varies between 2 and 8%.[1,2]
There are several vascular specific lasers like long-pulsed Nd-Yag, KTP, argon laser, copper vapour laser, alexandrite laser, IPL, but the gold standard for the management of PWS is the pulsed dye laser owing to its superior efficacy and safety profile. There are several studies in the literature which highlights this point but Indian studies are only few. Our study was to evaluate the efficacy and side effects of pulsed dye laser for the treatment of PWS on pigmented skin over a period 6 years.
MATERIALS AND METHODS
Seventy-five patients, 44 females and 31 males ranging in age between 8 months to 43 years with PWS who had not taken any treatment were treated with (V beam-Candela, USA) between January 2005 and December 2010 at our centre. Patients were (advised) to come at monthly intervals at least for a period of 6-8 months. Detailed history including history of consanguinity, convulsions, glaucoma and other neurological symptoms were documented and a thorough clinical examination was conducted. The diagnosis was made clinically and the skin biopsies were not performed. The patients were subjected to appropriate investigations including CT scan and MRI whenever indicated.
All patients were counseled thoroughly prior to the treatment and an informed consent was also taken. Photo documentation was done before and after each session and at 6 monthly intervals after the completion of the treatment.
The area to be treated was delineated with a skin marker by the treating doctor. Eutectic mixture of lignocaine and prilocaine was applied for those who opted for it. Children below 5 years were given inj. Ketamine intramuscularly under the supervision of an anaesthesiologist. Adequate eye protection was ensured for the patient with metallic eye shield and for all personnel in the laser room. The lesion over the upper eye lid was not treated. Pre-cooling was achieved with the dynamic cooling device (DCD). The laser parameters were selected depending on the area to be treated (location), age of the patient, colour of the lesion, thickness of the lesion and the pain tolerance [Table 1]. The parameters were modified during subsequent sessions based on the therapeutic response and presence or absence of adverse effects. The entire area was treated with a single pass with 10% overlap. The end point of treatment was erythema and purpura. On few occasions stacking pulses were given. Lower fluences were used for the neck and area below the eyes. The minimum number of sessions performed was 2 and maximum 17. Patients who had completed a minimum of 6 sessions were included in the study. All patients were instructed to use a steroid antibiotic combination ointment (Fluticasone propionate 0.05% and Mupirocin 2%) for 5 days after each session and to protect the treated area from ultraviolet rays using a broad spectrum sunscreen, regularly.
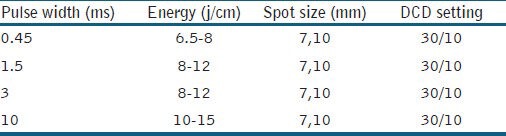
Table 1.
Laser parameters
The therapeutic response to laser treatment was graded on a scale of 0-4 by comparing serial photographs.
0 : <20% improvement
1 : 21-40% improvement
2 : 41-60% improvement
3 : 61-80% improvement
4 : >80% improvement
Side effects such as erythema, oedema, crusting, hyperpigmentation, hypopigmentation and scarring were recorded soon after the treatment and during following up.
RESULTS
Out of 75 patients, 11 patients were lost for follow-up after two to three sessions. Twenty-five patients under went six to eight sittings and the rest came for more than 9 sittings. The youngest patient was 8 months old and the oldest was 43 years. Ninety percent patients had the lesion on the face. The rest had it on the neck, chest, upper arm and the upper back [Table 2].
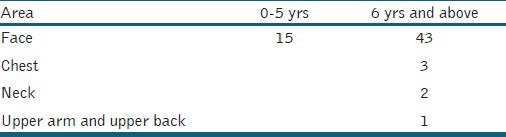
Table 2.
Area of involvement of PWS
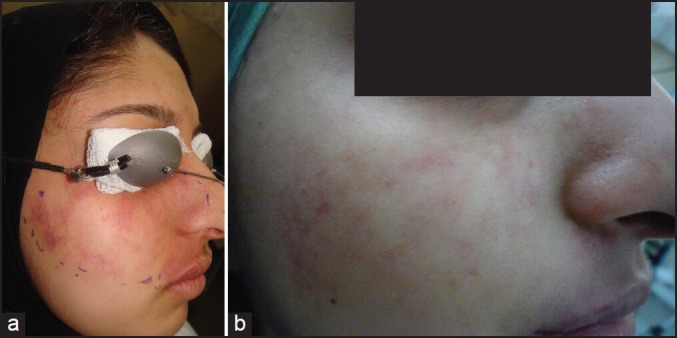
All patients who had six sittings or more showed some improvement. No patient showed total clearance. Maximum response of 4 (>80%) was seen in 13 (20%) patients after a mean of nine sessions and the minimum improvement (<20%) was observed in the (15%) patients even after nine or more treatments. Figures 1–4 demonstrate various grades of clinical improvement. Lesions over the face cleared faster and better than those on the other areas. Lateral aspect of cheek and forehead cleared faster than the medial aspect. The most resistant area was the upper lip.
Figure 1.
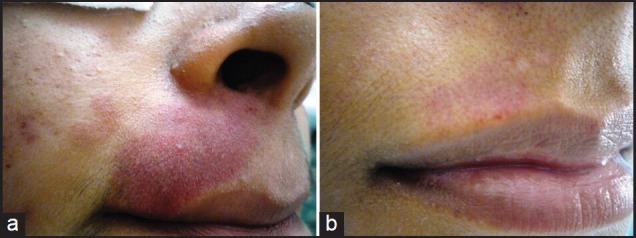
(a) Before treatment (b) After treatment
Figure 4.
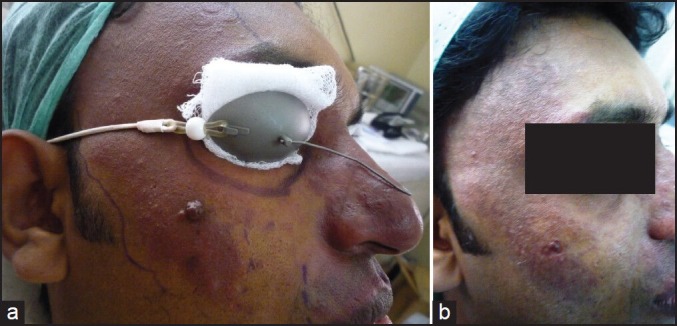
(a) Before treatment (b) After treatment
Figure 2.
(a) Before treatment (b) After treatment
Figure 3.

(a) Before treatment (b) After treatment
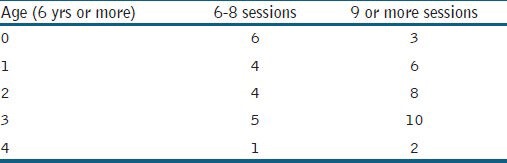
Age of the patient had an influence on the treatment outcome. Children (< 5 yrs) responded faster than adults as they had thinner lesions which were bright pink in colour. Sixty percent of children achieved at least grade 2 improvement after six to eight sessions while majority of adult patients required more than nine sessions to get the same degree of improvement [Tables 3 and 4]. Patients with thick PWS with nodular surface showed poor response even after nine sessions.
Table 3.
Percentage of improvement after six to eight sessions and after nine or more sessions
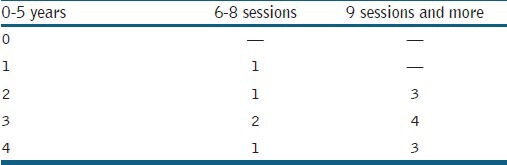
Table 4.
Percentage of improvement after six to eight sessions and after nine or more sessions (6 yrs and above)
No major side effects were seen during or after the treatment. Burning and pricking sensations were felt by all patients (who were conscious during the procedure). Maximum pain was felt over the upper lip (most sensitive area). Post-treatment erythema, oedema and crusting were directly related to the fluence used and inversely related to the pulse duration. These changes resolved within a period of 5-7 days in all the patients. Post-inflammatory hyperpigmentation was observed in 19 (30%) patients which cleared over a period of 1-2 months with the use of bleaching creams and sunscreen. Two patients developed depressed circular (pitted) scars as a result of stacking pulses. These patients had poor response to treatment. These scars improved over a period of 3-5 months without any intervention.
These was no re-darkening of the treated area in any of the patients till date.
DISCUSSION
Surgery, cryotherapy, X-irradiation, Electro cautery and Tattooing were some of the treatments formerly used to ablate vascular lesions. Due to the problems that resulted from these modalities, particularly in children, the concept, of selective photo-thermolysis was proposed in 1983 by R. R Anderson and J. A. Parrish. The ruby laser (694 nm) was the first medical laser used for the treatment of PWS. But the laser machines which were developed earlier had the drawbacks of inducing scarring, textural changes and pigmentary changes.[3] But significant developments in laser and light-based technology has made it possible to achieve a high safety profile and now cutaneous vascular lesions are one of the most common indications for laser treatment in dermatology.
The flash lamp-pumped tunable pulsed dye laser is an excellent treatment option for PWS as the emitted wavelength (585 or 595 nm) is well absorbed by the target chromophore Oxy-Hb (methHb to certain extent) selectively. Pulsed dye lasers contain rhodamine dye dissolved in methanol and emit light in the yellow portion of the visible spectrum. Oxy-Hb has absorption peaks at 420, 540 and 577 nm. Although the highest peak in Oxy-Hb absorption and the greatest difference in absorption melanin occurs at 420 nm, the light energy at 420 nm does not penetrate to reach vessels in the dermis. By using a wavelength of 585 nm early PDLs were able to preferentially heat Oxy-Hb at the depth necessary to treat PWS. Third-generation lasers (Ultra-long pulsed) which are commercially available now emits a wavelength at 595 nm with a variable pulse duration of 0.45-40 ms and with a dynamic cooling device (DCD). They are purpura free, have deeper penetration into the dermis and are more suitable for pigmented skin (type IV –VI) with less risk of epidermal injury and pigmentary alteration. Dual wavelength laser (PDL + Nd-Yag) is a recent addition to the armamentarium.
Multiple studies have demonstrated the efficacy and safety of the PDL on skin types I-IV.[4,5,6] However published data on Indian skin are very few. The efficacy of PDL for PWS on Indian skin was studied by Sharma and Khandpur in 2008 on 25 patients.[6] They found that PDL offers significant improvement for PWS. V beam-Candela laser was used in our study. This laser has a wave length of 595 nm with a variable pulse duration (0.45-40 ms) and the spot sizes of 10 mm, 7 mm, 5 mm and 3 × 10 mm oval.
In our study, 85.6% of patients showed some improvement after a minimum of eight sessions. Twenty percent of patients responded well to treatment with the percentage of improvement of >80%. We observed that the percentage of improvement was directly proportional to the number of treatments, with patients requiring at least six to eight sessions for 41-60% improvement in adults and 61-80% improvement in children. Our experience suggests that early treatment of PWS during childhood leads to the best response. 90% of children showed grade 2 improvement as compared to 60% in adults. Among children, four patients had near total clearance. The favourable responses could be due to thinner skin in infants, smaller and more superficial vessels and smaller affected surface area. However, other authors have not observed the same results.[7] Poorest response was seen in adult patients with thick non-blanching lesion with a coppery red colour. Other studies have also found out this fact.[8] Another factor which decides the clearance is the location of the lesion. We observed that the forehead, lateral aspect of cheeks, chin and anterior aspect of neck responded faster than other parts of the face and body. Ninety percent of patients with forehead lesions showed grade 3 response after six to eight sessions. The most recalcitrant area was the upper lip probably due to the presence of abundant pilosebaceous units. Adamic et al. have observed similar findings.[9] The poor prognostic factors observed in our study were late presentation, non-blanching thick PWS, coppery red colour and centro-facial lesions.
The side effects were mostly transient and included erythema, oedema and crusting of the treated skin. All patients had one or two of these skin changes soon after the treatment. Thirty percent of patients developed hyperpigmentation either patchy or diffuse after 10-15 days. Shorter pulse duration and higher fluence on a dark-skinned individual have the potential to induce post-inflammatory hyperpigmentation as the competing chromophore is melanin. Sharma and Khandpur also observed this complication in 25% of their patients treated with PDL.[6] Scarring and textural changes occurs rarely and is due to inadequate cooling, higher fluences and stacking of pulses. Two of our patients who developed scars showed a poor response to treatment and they were given stacking pulses. Some of the authors have observed redarkening of the treated area after a few years. It could be due to neovascularisation.[10,11] In our study, no patient has shown re-darkening till date.
Some of the PWS are resistant to treatment with PDL. Inspite of multiple sessions with adequate settings 10% of patients are likely not to respond to treatment as shown by previous studies.[12,13] In our study, 15% of adults did not respond to PDL treatment even after six sessions. So we need to combine other vascular lasers like long pulsed or frequency doubled Nd-Yag laser, PDT, topical rapamycin and angiogenic compounds for a better outcome.
CONCLUSION
Pulsed dye laser offers good cosmetic improvement in PWS in Indian patients with a very good safety profile. Multiple sessions are required to achieve a satisfactory improvement and earlier treatment leads to faster and better outcome.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Alper JG, Holmes LB. The incidence and significance of birthmarks in a cohort of 4,641 newborns. Pediatr Dermatol. 1983;1:58–66. doi: 10.1111/j.1525-1470.1983.tb01093.x. [DOI] [PubMed] [Google Scholar]
- 2.Nanda A, Kaur S, Bhakoo ON, Dhall K. Survey of cutaneous lesions in Indian newborns. Paediatr Dermatol. 1989;6:39–42. doi: 10.1111/j.1525-1470.1989.tb00265.x. [DOI] [PubMed] [Google Scholar]
- 3.Tan OT, Morrison P, Kurban AK. 585 nm for the treatment of port-wine stains. Plast Reconstr Surg. 1990;86:1112–7. doi: 10.1097/00006534-199012000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Loo WJ, Lanignan SW. Recent advances in laser therapy for the treatment of cutaneous vascular disorders. Lasers Med Sci. 2002;17:9–12. doi: 10.1007/s10103-002-8260-y. [DOI] [PubMed] [Google Scholar]
- 5.Dover JS, Arndt KA. New approaches to the treatment of vascular lesions. Lasers Surg Med. 2000;26:158–63. doi: 10.1002/(sici)1096-9101(2000)26:2<158::aid-lsm6>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 6.Sharma VK, Khandpur S. Efficacy of PDL in facial port-wine stains in Indian patients. Dermatol Surg. 2007;3:560–6. doi: 10.1111/j.1524-4725.2007.33114.x. [DOI] [PubMed] [Google Scholar]
- 7.van der Horst CM, Koster PH, de Borgie CA, Bossuyt PM, van Gemert MJ. Efficacy of the timing of treatment of port-wine stains with flash lamp pumped pulsed dye laser. N Engl J Med. 1998;338:1028–33. doi: 10.1056/NEJM199804093381504. [DOI] [PubMed] [Google Scholar]
- 8.Laube S, Taibjee S, Lanigan SW. Treatment of resistant port-wine stains with the V beam pulsed dye laser. Lasers Surg Med. 2003;33:282–7. doi: 10.1002/lsm.10234. [DOI] [PubMed] [Google Scholar]
- 9.Adamic M, Troilius A, Adatto M, Drosner M, Dahmane R. Vascular lasers and IPLS: Guidelines for care from the European Society for Laser Dermatology. J Cosmet Laser Ther. 2007;9:113–24. doi: 10.1080/14764170701280693. [DOI] [PubMed] [Google Scholar]
- 10.Huikeshoven M, Koster PH, de Borgie LA, Beek JF, van Gemert MJ, van der Horst CM. Redarkening of port-wine stains 10 years after pulsed dye laser treatment. N Eng J Med. 2007;356:1235–40. doi: 10.1056/NEJMoa064329. [DOI] [PubMed] [Google Scholar]
- 11.Ho WS, Chan HH, Ying SY, Chan PC. Laser treatment of congenital facial port-wine stains: Long term efficacy and complications in Chinese patients. Lasers Surg Med. 2002;30:44–7. doi: 10.1002/lsm.10003. [DOI] [PubMed] [Google Scholar]
- 12.Lanigan SW. Port-wine stains unresponsive to pulsed dye laser: Explanations and solutions. Br J Dermatol. 1998;139:173–7. doi: 10.1046/j.1365-2133.1998.02351.x. [DOI] [PubMed] [Google Scholar]
- 13.Katagampola GA, Lanigan SW. Five years’ experience of treating portwine stains with the flash lamp- pumped pulsed dye laser. Br J Dermatol. 1997;137:750–4. [PubMed] [Google Scholar]


