Abstract
Keloids of the helical rim are disfiguring. A cosmetically acceptable reconstruction is difficult especially in moderate to large sized lesions because the helical rim is a 3-dimensional structure with curved and thin cartilage. We report our experience in the management of moderate (4-10 cm) and large (>10 cm) helical rim keloids in five patients. Six helical rim keloids were reconstructed. There were four moderate (4-10 cm) and two large (>10 cm) helical rim keloids. Four were on the right helix and two on the left helix. One patient had bilateral helical rim keloids. The follow-up period ranged from 6 months to 4 years. No secondary surgical revision was required to improve the contour of the reconstructed helical rim. The aesthetic results were satisfactory in all the patients.
KEYWORDS: Helical rim keloids, intramarginal excision, split thickness skin graft, triamcinolone acetonide
INTRODUCTION
Keloids are unique to humans and result from excessive production of fibrous tissue during the healing of wounds. They can occur anywhere on the skin. Anatomical regions most commonly involved are the shoulders, neck, anterior chest, upper arms and the face.[1,2] Keloids of the helical rim are disfiguring and a cosmetically acceptable reconstruction is difficult especially in moderate to large sized lesions because the helical rim is a 3-dimensional structure with curved and thin cartilage.[3] We report our experience in the management of moderate (4-10 cm) and large (>10 cm) helical rim keloids in five patients.
CASE REPORT
Surgical technique
The procedure was carried out using general anaesthesia in all the patients. The periphery of the keloid was infiltrated with a local anaesthetic (0.5% lidocaine with 1:200,000 epinephrine). This facilitates dissection in a bloodless surgical field. An intralesional excision was done leaving a thin rim of keloid. This is a full thickness excision until healthy tissue is visualised with preservation of perichondrium. A split thickness skin graft was harvested with an electric dermatome from the thigh and applied over the defect after achieving haemostasis. The edges of the skin graft and the rim of keloid are meticulously sutured with 4-0 nylon and a bolus dressing is applied. Dressings were removed on the fourth postoperative day to inspect the graft. Sutures are removed after 1 week and compressive dressings with saline-moistened gauze are changed every 2 days for 2 weeks. Forty milligrams of triamcinolone was injected into the residual rim of keloid at 2 weeks post-operation. The injection is repeated at fortnightly intervals for a total of six injections. All patients were reviewed at 1 month from the time of the last steroid injection and followed up for at least 3 years.
RESULTS
Six helical rim keloids were reconstructed in five patients during the study period from December 2010 to January 2012. There were three males and two females. The average age was 24 years with a range of 16-37 years. The aetiology of the helical rim keloid was cosmetic ear piercing for additional ear ring openings in the two female patients. One of the male patients had a history of trauma and it was spontaneous in the other two male patients. The average length of the keloids was 11 cm with a range of 4-18 cm. There were four moderate (4-10 cm) and two large (>10 cm) helical rim keloids. Four were on the right helix and two on the left helix. One patient had bilateral helical rim keloids. Two patients had received repeated intralesional steroid injections, and one patient had received repeated injections plus surgical excisions at another hospital. The donor site was the thigh in all the patients. All the grafts survived. The follow-up period ranged from 6 months to 4 years. There was evidence of keloid recurrence in two patients and marginal elevation of the graft due to graft bed contraction in one patient. These resolved with intralesional injection of steroids. No secondary surgical revision was required to improve the contour of the reconstructed helical rim. All the patients complained about pruritus at the donor site in the third post-operative week. These symptoms disappeared in the sixth post-operative week. In three of the patients, erythema of the donor site was also observed and these disappeared by the sixth post-operative week. Keloid formation at the donor site was not seen in any of the patients at 4 years follow-up. The aesthetic results were satisfactory [Figure 1a and b].
Figure 1.
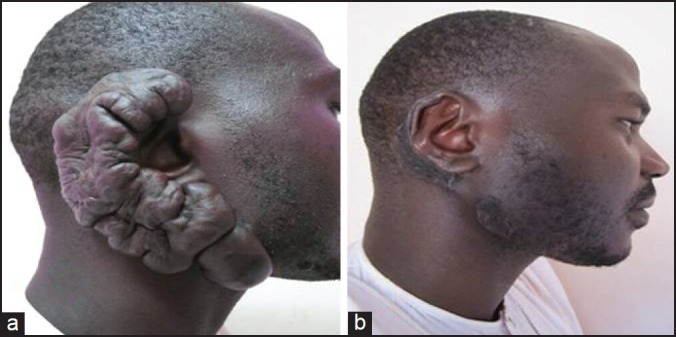
(a) Helical rim keloid before treatment (b) Helical rim keloid after treatment
DISCUSSION
Keloids are a common and difficult problem to treat. The influence of ethnicity on keloid scarring is significant as they tend to occur in darker skinned individuals.[4] Keloid formation has been ascribed to altered growth factor regulation, aberrant collagen turnover, immune dysfunction and genetics. No single unifying hypothesis adequately explains the aetiopathogenesis of keloids.[4] This is due in part, to the lack of a reliable in vivo experimental model, because keloid formation is a unique phenomenon that occurs in humans.[5,6] Helical rim keloids can result from a variety of causes involving deep dermal injury, with the most common being ear piercings, post-elective surgery, acne, trauma or burns.[3] Increasing tension placed upon the lesion in certain sites and orientations, and the presence of infection and foreign bodies, may augment the risk of keloid formation. Keloid can develop at any age, but tends to be most prevalent in individuals aged between 10 and 30 years.[7] In this study, the incidence is approximately equal for male and female, and the patients were in the same age range as described in most reports. The onset was following trauma in four patients. These dense, fibrous growths are benign, but it can cause symptoms such as pain, tenderness and pruritus in addition to the psychosocial implications caused by aesthetic concerns.[7,8,9]
The surgical excision of keloids alone has consistently shown poor results, with recurrence rates of 40-100%. Simple excision is believed to stimulate additional collagen synthesis, resulting in a more rapid growth and often a larger keloid.[2] Surgery has been found to be most effective when combined with steroid, irradiation or pressure therapy.[2] Intralesional excision has been credited with improved outcome and fewer recurrences. The residual rim of the keloid splints the wound and relieves tension, thus decreasing the stimulus for collagen synthesis.[1]
The closure of the defect, following the excision of moderate and large sized keloids of the ear or other body sites using skin grafts has been described as satisfactory.[3] Split-thickness skin grafts may, however, produce suboptimal cosmetic results due to its thinness and shrinking, although it shows excellent graft take. Full-thickness skin grafting may produce an excellent cosmetic outcome when the donor skin has a similar colour, but is generally considered too unreliable over the poorly vascularised perichondrial bed. The lack of an adequate vascular supply on a narrow helical defect with exposed cartilage may result in failure of full-thickness skin grafts.[3] In this study, the size of the lesions precluded the use of full thickness skin grafts. The reported recurrence rate after skin grafting has ranged from 0% to 9% and is the lowest among all of the surgical techniques used; 12.5% after keloid core excision and the use of a rind flap, 44% after local excision and 50% after the use of a keloid fillet flap.[3]
Donor site morbidity, including keloid formation at the donor site, is a significant concern following any grafting procedure in patients with keloids. Keloids arise from skin trauma and must be removed through skin trauma. Therein lies the challenge of reconstruction, where recurrence would seem inevitable.[10] All the patients were counselled about the risk of keloid formation at the donor site. The proximal thigh was selected as the donor site in all the patients. In this study, none of the patients developed keloids at the donor site. This is similar to the findings reported by Saha et al.[11] in a series of 15 patients who had excision of ear lobule keloids and split-thickness skin grafting of the defect. There was minimal donor site morbidity at 3 years follow-up. Burm[3] also reported a satisfactory outcome following the use of full thickness skin graft in the reconstruction of helical keloids in seven patients. A fine linear scar without hypertrophy was present at all the donor sites.
Excision of the lesion followed by injection of triamcinolone is one the most successful combination regimen in the management of keloids. Cure rates exceeding 80% have been consistently reported using this regimen.[1] Intralesional steroids act by suppressing the inflammatory response, diminishing collagen synthesis, decreasing mucinous ground substance production and inhibiting collagenase inhibitors that prevent the degradation of collagen. The adverse effects of steroids include atrophy of the skin, hypopigmentation, telangiectasia and cushingoid effects from systemic absorption.[2]
The technique described in this report is similar in principle to other surgical approaches that combine surgical excision with post-operative steroid injections.[2,9] However, some differences need to be emphasised. The excision of the helical rim keloid is intralesional and not extralesional. It deliberately aims to leave a thin rim of keloid. While success with surgical techniques that combine the injection of steroid immediately after excision of keloid have been reported, it has also been our observation that this causes delayed wound healing. In the technique described in this report, the injection of steroid was delayed until the time of suture removal. This avoids any interference with initial wound healing.[2]
CONCLUSION
Our study demonstrates that intralesional excision, split thickness skin graft and intralesional triamcinolone are suitable in treating helical rim keloids with a good contour and colour match. The outcome in our patients’ has been satisfactory and encouraging.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Al-Attar A, Mess S, Thomassen JM, Kauffman CL, Davison SP. Keloid pathogenesis and treatment. Plast Reconstr Surg. 2006;117:286–300. doi: 10.1097/01.prs.0000195073.73580.46. [DOI] [PubMed] [Google Scholar]
- 2.Donkor P. Head and neck keloid: Treatment by core excision and delayed intralesional injection of steroid. J Oral Maxillofac Surg. 2007;65:1292–6. doi: 10.1016/j.joms.2006.10.049. [DOI] [PubMed] [Google Scholar]
- 3.Burm JS, Hansen JE. Full-thickness skin grafting with marginal deepithelialization of the defect for reconstruction of helical rim keloids. Ann Plast Surg. 2010;65:193–6. doi: 10.1097/SAP.0b013e3181ba99f2. [DOI] [PubMed] [Google Scholar]
- 4.Davison SP, Dayan JH, Clemens MW, Sonni S, Wang A, Crane A. Efficacy of intralesional 5-fluorouracil and triamcinolone in the treatment of keloids. Aesthet Surg J. 2009;29:40–6. doi: 10.1016/j.asj.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 5.Lee Y, Minn KW, Baek RM, Hong JJ. A new surgical treatment of keloid: Keloid core excision. Ann Plast Surg. 2001;46:135–40. doi: 10.1097/00000637-200102000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Kelly AP. Update on the management of keloids. Semin Cutan Med Surg. 2009;28:71–6. doi: 10.1016/j.sder.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 7.Ud-Din S, Bayat A. Strategic management of keloid disease in ethnic skina: Structured approach supported by the emerging literature. Br J Dermatol. 2013;169:71–81. doi: 10.1111/bjd.12588. [DOI] [PubMed] [Google Scholar]
- 8.Juckett G, Hartman-Adams H. Management of keloids and hypertrophic scars. Am Fam Physician. 2009;80:253–60. [PubMed] [Google Scholar]
- 9.Brown NA, Ortega FR. The role of full-thickness skin grafting and steroid injection in the treatment of auricular keloids. Ann Plast Surg. 2010;64:637–8. doi: 10.1097/SAP.0b013e3181dba8aa. [DOI] [PubMed] [Google Scholar]
- 10.Rosen DJ, Patel MK, Freeman K, Weiss PR. A primary protocol for the management of ear keloids: Results of excision combined with intraoperative and postoperative steroid injections. Plast Reconstr Surg. 2007;120:1395–400. doi: 10.1097/01.prs.0000279373.25099.2a. [DOI] [PubMed] [Google Scholar]
- 11.Saha SS, Kumar V, Khazanchi RK, Aggarwal A, Garg S. Primary skin grafting in ear lobule keloid. Plast Reconstr Surg. 2004;114:1204–7. doi: 10.1097/01.prs.0000135889.48745.e4. [DOI] [PubMed] [Google Scholar]


