Abstract
Objective
To evaluate previous research to determine if exercise can improve preexisting hyperkyphosis by decreasing the angle of thoracic kyphosis in adults aged ≥45 years.
Data Sources
PubMed, Embase, and the Cumulative Index to Nursing and Allied Health Literature databases were searched for studies related to posture, exercise, and age ≥45 years. Online conference proceedings of the American Society for Bone and Mineral Research, American Physical Therapy Association, and Gerontological Society of America were also searched.
Study Selection
Two independent reviewers screened the titles and abstracts and selected studies that tested the effect of exercise on measures of kyphosis, or forward head posture, in individuals with hyperkyphosis at baseline (defined as angle of kyphosis ≥40°). Reviews, letters, notes, and non-English language studies were excluded.
Data Extraction
A pilot-tested abstraction form was used by each reviewer to extract data from each study regarding details of exercise intervention, participant characteristics, safety, adherence, and results. The Cochrane Collaboration’s tool for assessing risk of bias was used to assess methodologic quality. Discrepancies on the abstraction forms between the 2 reviewers were resolved by a third reviewer. A formal meta-analysis was not performed.
Data Synthesis
Thirteen studies were abstracted and included in the review; of these, 8 studies saw improvements in ≥1 measure of posture. The main sources of bias were related to blinding participants and incomplete outcome data. The adherence reported across studies suggests that exercise is an acceptable intervention for individuals with age-related hyperkyphosis.
Conclusions
The scarcity and quality of available data did not permit a pooled estimate of the effect of exercise on hyperkyphotic posture; however, the positive effects observed in high-quality studies suggest some benefit and support the need for an adequately designed randomized controlled trial examining the effect of exercise on hyperkyphosis.
Keywords: Aged, Exercise, Kyphosis, Rehabilitation
Age-related hyperkyphosis, an excessive anterior concavity of the thoracic spine, is estimated to affect 20% to 40% of older adults.1,2 Hyperkyphosis can impair pulmonary function3 and activities of daily living performance,2,4 reduce quality of life,2 and predict mortality independent of underlying spinal osteoporosis.1 Women with hyperkyphosis have slower gait, impaired balance, and increased body sway, all of which can increase their risk for falls.5,6 Individuals with hyperkyphosis may or may not present with underlying spinal osteoporosis and vertebral compression fractures (VCFs).7-9 Although not all individuals with age-related hyperkyphosis have preexisting VCFs,8,9 excessive thoracic kyphosis can increase the biomechanical stress on the spine,10,11 increasing the risk of developing VCFs.9,12 The etiology of hyperkyphotic posture is complex because many factors can contribute to degenerative changes of the spine with age. Vertebral body wedging, routinely poor posture, decreased spinal extension mobility, dehydration of the intervertebral disks, and reduced back extensor muscle strength (BES)1,13,14 are other commonly cited potential causes of age-related hyperkyphosis.
Despite significant findings regarding its adverse effects on measures of health and quality of life, hyperkyphosis is only beginning to be recognized as a major health concern by clinicians,15 and there is no standard protocol for treating hyperkyphosis.16 Treatment modalities are currently in use, including surgery, bracing, and physiotherapy.17-20 Surgery, such as balloon kyphoplasty or vertebroplasty, has been recommended for some people with acute, painful VCF, and it can reduce associated kyphosis.21,22 However, surgery is not indicated for everyone with age-related hyperkyphosis, and there are risks, such as subsequent VCF, associated with kyphoplasty.23 Spinal orthoses have been used to reduce kyphosis; however, they have only been tested in women with underlying spinal osteoporosis.19,20 In contrast to the aforementioned treatment options, exercise allows individuals with hyperkyphosis to take an active role in their own health care and, if performed safely and correctly, is known to provide other health benefits.24 Specifically, exercises that aim to increase BES and spinal flexibility may decrease hyperkyphosis and, if combined with postural training, may enable older adults to maintain a more upright posture. Our aim was to conduct a systematic review to evaluate current research and determine if exercise can improve posture by decreasing the angle of kyphosis in adults aged ≥45 with preexisting hyperkyphosis.
Methods
Search strategy
PubMed, Embase, and the Cumulative Index to Nursing and Allied Health Literature databases were searched by 2 reviewers for articles published from the first year of coverage for each database until 2012. To identify relevant studies, the databases were searched for author keywords and subject headings related to the concepts of exercise, posture, and age ≥45. For example, the Medical Subject Headings searched in PubMed included: kyphosis, exercise, weight lifting, exercise therapy, exercise movement techniques, aged, physical fitness, and middle aged. The titles and abstracts were searched in PubMed using the [tiab] option after the author keywords: exercise, yoga, Pilates, exercise therapy, exercise movement techniques, physical activity, posture, hyperkyphosis, spinal curvature, skeletal alignment, elderly, older adults, seniors, and middle aged (see appendix 1 for complete database search strategy). The online conference proceedings of the annual meetings of the American Society for Bone and Mineral Research, American Physical Therapy Association, and the Gerontological Society of America were screened for relevant titles and abstracts. The American Physical Therapy Association’s proceedings of their combined sections meetings were also screened for relevant abstracts. The literature search was last performed October 15, 2012.
Inclusion criteria
Table 1 shows the inclusion and exclusion criteria applied during the screening process. Age and baseline hyperkyphosis criteria were used to limit our search to studies that tested the effect of exercise on existing age-related hyperkyphosis. The inclusion of individuals as young as age 45 was an attempt to capture studies of postmenopausal women and middle-aged adults affected by osteoporosis because this is a potential cause of hyperkyphosis. If the mean baseline angle of kyphosis for each study group was not given, or if a minimum angle of kyphosis was not an inclusion criterion for the study, it was included on the basis of participants being described as having flexed posture at baseline. Studies were also included if a subgroup analysis that included only those with hyperkyphosis was done as part of the study or if the baseline mean angle of kyphosis of at least 1 of the groups was ≥40°, a commonly used threshold to define hyperkyphosis.25,26 All types of exercise interventions were included as long as the participants performed at least part of the exercises independently in order to distinguish active exercise from passive mobilization aided by a physical therapist. Measures of kyphosis or forward head posture, a commonly used indicator of kyphosis, were allowed.
Table 1.
Inclusion and exclusion criteria
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Study is an RCT, clinical trial (any phase), nonrandomized intervention trial |
Study is a letter, note, review article, or brief report |
| ≥1 of the outcomes is a measure of kyphosis or forward head posture |
Non-English language |
| Participants are individuals aged ≥45 years with hyperkyphosis at baseline; defined by objective measure or clinical diagnosis |
Study examines effect of exercise on posture in specific subgroup (eg, stroke survivors) |
| Intervention involves exercise and/or physical therapy with an independent exercise component |
Data collection and synthesis
Two independent reviewers (S.B., W.B.K.) screened the titles and abstracts of the search results and reviewed the full texts selected for inclusion in the review. A pilot-tested abstraction form was used for each full-text paper; each reviewer recorded details of each study, including study setting, inclusion/exclusion criteria, participant characteristics at baseline, details of the exercise interventions, outcome measures, adherence, adverse events, statistical analyses performed, and results. The abstraction form also included the Cochrane Collaboration’s tool for assessing risk of bias, which was used to determine the quality of each study. This assessment evaluates the methodologic quality of key domains of randomized controlled trials (RCTs), such as blinding, random sequence generation, and selective outcome reporting.27 After the abstraction forms were completed, they were compared and any discrepancies that could not be resolved through discussion by the 2 reviewers (S.B., W.B.K.) were resolved by a third, unbiased reviewer. This review was written in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses. Details of the study samples and exercise interventions are summarized in tables 2, 3, and 4. Mean within-group changes or the between-group difference in means postintervention are reported for the group(s) of each study, as applicable. A formal meta-analysis was planned; however, it was not performed because of heterogeneity among the selected RCTs in regard to the types of interventions, outcome measures, duration of intervention, and missing values in some publications that would have been required for a meta-analysis.
Table 2.
Participant characteristics
| Study | Analyzed/ Recruited (n) |
Females (%) | Main Inclusion Criteria | Main Exclusion Criteria | Outcome Measures | Included Individuals With VCF |
|---|---|---|---|---|---|---|
| Abreu et al36 | 20/20 | 100 | Older adult women with osteoporosis |
None stated | Flexicurve angle (deg) | Unclear |
| Bautmans et al35 | 48/48 | 100 | Postmenopausal women receiving 3-monthly intravenous pamidronate |
CITE, rheumatoid arthritis, Paget disease, ankylosing spondylitis |
Handheld inclinometer (deg) | Not if acute VCF |
| Benedetti et al33 | 28/34 | 64.7 | Age ≥65y, flexed posture | CITE, disabling blindness or deafness, secondary osteoporosis |
Occiput-to-wall distance (cm) | No |
| Bennell et al32 | 20/20 | 80 | Age >50y, diagnosis of osteoporosis |
CITE, steroid use, radiating back pain, treatment for low back pain |
Digital inclinometer (deg) | Not if acute VCF |
| Bergström et al37 | 28/36 | 100 | Postmenopausal women on bisphosphonate medication for ≥4mo |
Exercising at or above the level of the program, CITE |
Kyphometer (deg) | Not if acute VCF |
| Greendale et al38 | 14/21 | 100 | Age ≥60y, hyperkyphosis ≥40° at baseline, physician clearance |
Angina, uncontrolled lung disease, inability to pass safety test |
Distance from tragus-to-wall, kyphometer (deg) |
Yes |
| Greendale et al30 | 118/118 | 81.4 | Age ≥60y, hyperkyphosis ≥40° at baseline |
CITE, use of assistive device, inability to see or hear adequately |
Flexicurve index, flexicurve angle (deg), kyphometer (deg) |
Yes |
| Itoi and Sinaki29 | 60/60 | 100 | Nonsmoking, healthy, postmenopausal women |
Diseases or special diet affecting bone metabolism or muscle strength |
Cobb angle (deg) | Unclear |
| Katzman et al13 | 21/25 | 100 | Age ≥65y, kyphosis ≥50°, approval to participate by physician |
Inability to pass safety test, inability to decrease usual kyphosis by ≥5° |
Kyphometer (deg); distance from occiput-to-wall (cm) |
Not if acute VCF |
| Kuo et al39 | 34/34 | 70.6 | Age ≥60y, no previous Pilates experience |
History of movement dysfunction, pain or pathologies of legs or spine, exercise participation in last 6mo |
Thoracic spine angle from photometric technique (deg) |
Unclear |
| Renno et al40 | 14/26 | 100.0 | Age ≥65y, white, nonsmoking, sedentary, osteoporosis for ≥5y |
CITE | Angle of kyphosis from photometric technique (deg) |
No |
| Schuerman34 | 50/60 | 100.0 | Age ≥50y, osteoporosis, healthy | Inability to pass safety test, CITE, obvious leg length discrepancy, limb fracture, visual field loss |
Inclinometer (deg) | Yes |
Abbreviation: CITE, contraindications to exercise.
Table 3.
Interventions and results of RCTs
| Study | Intervention | Equipment Used |
Volume of Supervision |
Frequency* and Duration† |
Volume‡ or Intensity§ | Results |
|---|---|---|---|---|---|---|
| Abreu et al36 |
|
Not stated | Not stated | 2d/wk for 12wk | Not stated | |
| Bautmans et al35 |
|
Dumbbells | Continual | Exercises every day, physiotherapy 3d/wk for 2wk and then decreased thereafter for 10wk |
3 sets of 10–15 reps |
|
| Benedetti et al33 |
|
Table, chair, stick |
Not stated | 2d/wk for 12wk | 8–10 reps |
|
| Bennell et al32 |
|
Dumbbells | Continual | Exercise 3d/wk for strength and trunk control, every day for posture and range of motion, 1 physiotherapy session per week for 10wk |
Not stated |
|
| Greendale et al30 |
|
Table, chair, stick |
Continual | 3d/wk for 24wk | Not stated |
|
| Itoi and Sinaki29 |
|
Weighted backpack |
Intermittent | 5d/wk for 2y | 10 reps with weight of 30% of maximum isometric BES to a maximum of 22.68 kg |
|
| Schuerman34 |
|
None | Intermittent | Every day for 12wk | Tailored to individual |
|
Abbreviations: CI, confidence interval.
Frequency refers to number of days per week.
Duration refers to total length of the intervention.
Volume refers to number of repetitions (reps).
Intensity refers to % of 1-repetition maximum or intensity as stated in the study (eg, moderate).
Standard error/standard deviation not published.
Table 4.
Interventions and results of pre-post design studies
| Study | Intervention | Equipment Used | Volume of Supervision |
Frequency and Duration | Volume or Intensity | Results (Mean ± SD/SE, P) |
|---|---|---|---|---|---|---|
| Bergström et al31 |
|
Resistance band | Continual | 2d/wk for 16wk | Tailored to individual |
|
| Greendale et al38 |
|
Yoga mats | Continual | 2d/wk for 12wk | Not stated |
|
| Katzman et al13 |
|
Resistance band, foam rollers, stretch straps, and dumbbells |
Not stated | 2d/wk, postural correction every day for 12wk |
Moderate to high |
|
| Kuo et al39 |
|
Weights, resistance band, mats, wobble board, fitball, foam rollers |
Continual | 2d/wk for 10wk | Tailored to individual |
|
| Pawlowsky et al28 | NA, follow-up study | None | NA | NA | NA |
|
| Renno et al40 |
|
Weighted backpack | Not stated | 3d/wk for 8wk | Trunk extension 10 reps with weight of 30% of 1-repetition maximum |
|
Abbreviations: CI, confidence interval;Duration, total length of the intervention;Frequency, number of days per week;Intensity, percentage of 1 repetition maximum or intensity as stated in the study (eg, moderate); lat, latissimus dorsi;NA, not applicable;reps, repetitions;Volume, number of repetitions.
SE/SD not published.
Results
Study selection process
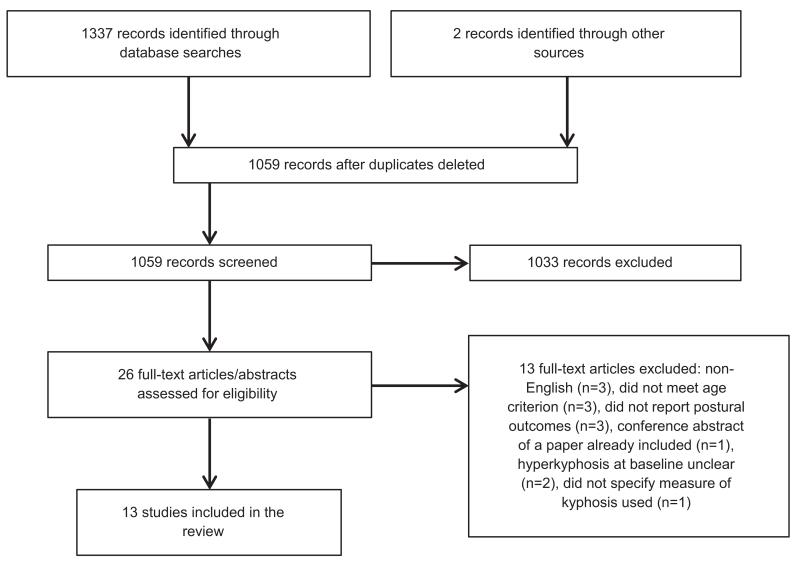
Our database search yielded 1377 titles, and 2 potentially relevant titles were retrieved from other sources (fig 1). Twelve studies were fully abstracted and included in this review. One additional study was identified, but it was a follow-up of participants in an already included study to determine whether participants maintained improvements from the prior intervention at 1 year28; only the results section of the follow-up study is described here. Seven studies were randomized, parallel group designs,29-35 and the remaining studies were characterized as nonrandomized intervention trials (eg, pilot studies). One RCT was a published abstract that provided limited information about the study in terms of study design and statistical analysis; however, it was still included based on meeting the selection criteria.36 Although 1 study did not meet the prespecified criterion for hyperkyphosis at baseline, it was included based on a mean baseline occiput-to-wall distance of >5cm in both the intervention and control groups. The 2010 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada37 state that an occiput-to-wall distance >5cm indicates kyphosis and vertebral fractures. Overall, there were 33 discrepancies found between the abstraction forms completed by the 2 independent reviewers; most were resolved via discussion, and 2 of these discrepancies had to be resolved by a third, unbiased reviewer.
Fig 1.
Flow diagram depicting results of the study selection process.
Studies included
Of the 13 articles selected for inclusion, 8 reported significant improvements in ≥1 measure of kyphosis or forward head posture (see tables 3 and 4).13,28-30,33,35,38,39 One additional study did not perform a formal statistical analysis but reported a 5% improvement in the mean angle of kyphosis from baseline to post-intervention.40 All studies had ≥1 issue with methodologic quality that may have introduced biases and affected the interpretation of their results (table 5).
Table 5.
Results of assessing risk of bias
| Study | Study Design | Random Sequence Generation |
Allocation Concealment |
Blinding of Participants and Personnel |
Blinding of Outcome Assessment |
Incomplete Outcome Data |
Selective Reporting |
Other Sources of Bias |
|---|---|---|---|---|---|---|---|---|
| Abreu et al36 | RCT | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Bautmans et al35 | RCT | Low | Low | High | Low | Low | Low | Unclear |
| Benedetti et al33 | RCT | Unclear | Unclear | Low | Unclear | High | Low | Unclear |
| Bennell et al33 | RCT | Low | Low | High | Low | Low | Low | Unclear |
| Bergstrom et al37 | Pre-post | Low | High | High | High | High | High | Unclear |
| Green dale et al38 | Pre-post | High | High | High | High | Low | Low | Unclear |
| Green dale et al30 | RCT | Low | Low | High | Low | High | Low | Unclear |
| Itoi and Sinaki29 | RCT | Unclear | Unclear | High | Low | Low | Low | High |
| Katzman et al13 | Pre-post | High | High | High | High | High | Low | Unclear |
| Kuo et al39 | RCT | High | High | High | High | Low | Low | Unclear |
| Pawlowsky et al28 | Pre-post | High | High | High | High | Low | Low | Unclear |
| Renno et al40 | Pre-post | High | High | High | High | High | Low | Unclear |
| Schuerman34 | RCT | High | Low | High | Unclear | High | Low | Unclear |
Randomized controlled trials
Seven studies stated that they were RCTs, and 4 of these reported significant improvements in measures of kyphosis within the intervention groups or significant between-group differences. Given the heterogeneity of the interventions and varied durations of the 7 RCTs, it did not seem appropriate to pool their results for the purposes of a meta-analysis (see table 3). Only 4 of the 7 included RCTs reported between-group results. Of these 4 RCTs that reported between-group results, 2 of them reported significant differences between the intervention and control groups in favor of exercise.29,30 One of these 2 studies used 10 repetitions of prone trunk extension with a weighted backpack 5 days per week for 2 years,29 and the other study’s intervention consisted of a group yoga class 3 days per week for 24 weeks. The yoga intervention RCT was a high-quality study based on ratings of low risk of bias in many domains except for blinding of participants, which is difficult in an exercise RCT, and incomplete outcome data because a true intention-to-treat analysis had not been done.30 The weighted backpack intervention also received a rating of low risk of bias in several domains, with the exception of participant blinding and other sources of bias because a post hoc analysis had been performed in which participants were stratified by baseline angle of kyphosis and BES.29
Of the 3 RCTs that reported within-group results, 2 reported significant improvements in the intervention groups after the exercise programs.33,35 These studies primarily used strengthening exercises to improve kyphosis, and 1 incorporated physical therapy in addition to exercise.35 Both interventions were performed for 12 weeks; 1 study had participants exercise 2 days per week,33 whereas the study of exercise and physical therapy instructed participants to exercise every day.35 The quality of these studies varied; the study of exercise and physical therapy was mainly rated low risk of bias, with the exception of participant blinding, which was high risk,35 and the remaining study was given a mix of low and unclear risk of bias in most domains, except for incomplete outcome data, which were not accounted for in the study.33
Pre-post design studies
Five of the included studies were pre-post intervention designs, and 1 was a follow-up study; of these 6 studies, 4 reported statistically significant within-group improvements in measures of kyphosis13,28,39 and 1 did not perform a formal statistical analysis but stated that a 5% improvement in the angle of kyphosis was observed after the intervention.40 All of these studies received a rating of high risk of bias in ≥5 domains on the Cochrane Collaboration’s tool, mainly because of a lack of a control group. The studies that reported significant improvements varied in terms of the type of intervention, from yoga to multicomponent exercise programs and Pilates. The duration of the interventions ranged from 8 to 12 weeks, with exercises typically performed 2 to 3 days per week.
Study participants
Men were not included in most studies, and none of the studies had participants as young as 45 years of age, the threshold chosen for inclusion in this review. Three studies did not specify an age criterion for inclusion but stated that participants had to be post-menopausal, suggesting that they were >45 years,29,31,35 whereas another study described participants as elderly women.36 The presence of osteoporosis and/or vertebral fractures at baseline varied among studies, and it is not clear whether the presence or absence of vertebral fracture was an effect modifier. Furthermore, 1 study performed a stratified analysis by the presence/absence of vertebral fractures and found no differences between the stratified and the pooled analyses.38 Sample sizes were small, and many studies either did not explicitly state that they performed a power calculation29,32,33,35,36,38,39 or reported that they were underpowered.13,31,34,40
The main exclusion criteria across studies were safety or disability (cognitive or physical) criteria30,33,35,38 and contraindications to exercise or diagnoses that may affect exercise participation, such as pulmonary disease, cardiac conditions, and neurologic diagnoses.13,30-34,38-40 Surprisingly, only 3 studies accounted for the exercise habits of participants at baseline.
Outcome measures
The outcome measures varied across studies. Three studies used >1 measure of posture,13,30,38 whereas the other 10 used only 1 (see table 2). Some studies used reliable, previously validated measures of kyphosis,41 such as the Debrunner kyphometer, flexicurve, and Cobb angle obtained from a radiograph. A few studies measured forward head posture or determined the distance between occiput to wall or tragus to wall; however, the validity of these measures compared with the criterion standard Cobb angle has not been determined. Three studies used an inclinometer to measure kyphosis32-35; all 3 studies reported intraclass correlation coefficients of ≥.73 for their respective measures, suggesting that the inclinometer was a reliable measure.
Interestingly, a few studies used a photometric technique to measure kyphosis.33,39,40 The photometric technique involves placing cutaneous markers on the superior and inferior borders of the thoracic spine and recording a photograph or video of each participant wearing these markers. The angle of kyphosis was calculated based on lines projected from the markers. One of these studies reported an intraclass correlation coefficient of .85 to .92 for marker placement from a pilot study,39 1 study did not report the reliability of its measure,33 and the last study cited an intra- and interobserver coefficient r2=.998 from a validation study of their technique.40
In most studies it was stated that kyphosis measurements were acquired when participants were standing. However, many studies did not report whether measurements were acquired during usual or best posture stance. Two studies only reported best posture,31,34 and 2 reported usual and best posture.13,28
Interventions
Exercises aimed at increasing BES were common to all of the interventions, and a few studies also included abdominal strengthening exercises (see tables 3 and 4).33,36,38,39,42 Two studies incorporated postural education into the interventions.13,39 Several exercise programs were at least an hour in length.30,31,33,38-40 Some studies specified who provided the exercise program; generally, it was physiotherapists13,31,32,35 or certified instructors.30,39 In most cases, the comparator groups in the RCTs were not prescribed any type of intervention.29,31,32,35,36 In 1 study, the control group performed a nonspecific exercise program for older adults,33 and in another study, they attended a monthly lunch and learn session that aimed to provide a social environment similar to that of the yoga intervention.30 Participants acted as their own controls in the Pilates-based exercise study; measurements were taken twice prior to the intervention, which served as the control period, and then twice after the intervention to determine if the effects of exercise persisted after a 4-week follow-up period.39
Assessing risk of bias
In general, there was a high risk of bias across all studies, most often related to blinding and incomplete outcome data. The non-randomized trials were rated as high risk of bias because they failed to use random sequence generation, allocation concealment, and blinding in their study design. Selective reporting did not appear to be an issue in any study; however, most studies were not registered, and their study protocol was not available to confirm whether selective reporting had occurred. Although 5 studies blinded outcome assessors to the allocation status of participants,29,30,32,33,35 it is almost impossible to blind the participants in an exercise trial, except when the control group is also performing exercise.33 In addition, 6 studies did not perform a true intention-to-treat (ITT) analysis,13,30,31,33,34,40 and 1 study introduced bias by performing a post hoc analysis.29 Finally, 3 studies stated that they enrolled relatively motivated or healthy individuals,13,29,30 suggesting that nonresponse bias may have been introduced.
Adherence and safety
Methods for reporting adherence varied across studies, and adherence was relatively high when it was reported. Three studies did not report any quantification of adherence29,34,36; 2 studies reported a mean adherence of 80%,38 1 reported a mean adherence of 97.5%,39 and 1 reported a median adherence of 95% (inter-quartile range, 78%–100%).32 Two studies reported adherence in a way that emphasized adherence in those that completed the exercises (eg, 88% attended at least 80% of the sessions33 or average attendance of those who attended ≥75% of the sessions was 95%40). Three studies simply stated raw numbers: 28 women attended ≥90% of sessions,31 21 of 36 individuals attended 100% of sessions,13 and 15 of 21 individuals who completed the study attended ≥50% of the physiotherapy sessions.35 In addition, the participants of 2 studies expressed that the intervention was an overall positive experience for them.35,39
Generally, the interventions appear to be safe, although 7 studies did not mention adverse events,13,29,33,36,38-40 and 1 study stated that no adverse events occurred during the intervention.38 Commonly reported adverse effects of the interventions in studies that did report them were the following: shoulder pain/discomfort, soreness, irritation caused by physio tape, and back pain.30,32,34,35 Only 1 study reported serious adverse events, namely myocardial infarction and cardiac arrhythmia; however, it is unclear whether this was related to the intervention.34
Discussion
Our systematic review of the literature suggests that the available evidence regarding the effects of exercise on age-related hyperkyphosis is scarce and largely of low quality and that a few trials report some benefit of exercise or multimodal interventions that include exercise, a finding that is consistent with previous narrative reviews.14,15 The results of 2 RCTs reporting between-group results suggest that targeted spinal extension muscle exercises and yoga may reduce kyphosis among older adults with hyperkyphosis. Exercise adherence was generally good in studies that reported it, suggesting that exercise is an acceptable treatment option for people with age-related hyperkyphosis. The 2 RCTs that demonstrated significant between-group differences post-intervention ranged from 24 weeks to 2 years in duration and that exercise was performed on ≥3 days per week. Despite the improvements reported in some of the pre-post studies, it is difficult to make recommendations based on them because they were not the best quality and sample sizes were generally small. Most of the studies included in this review did not state the intensity of their interventions, making it difficult to provide guidelines for the level of exercise intensity that could improve hyperkyphosis. It is not possible to distinguish the effects of exercise in studies of multimodal interventions. However, most of the interventions to date have been led by physical therapists or trained instructors; therefore, it is reasonable to conclude that a physical therapist or instructor-led intervention including exercise may result in improved posture, but these findings may not be generalizable to other exercise types or settings.
It has been hypothesized that improvements in posture can be achieved with improved BES or other factors related to hyperkyphosis, such as spinal extension mobility, improved postural awareness, or fewer incident VCFs compared with controls. All of the exercise interventions identified in this review focused, in part, on reducing hyperkyphosis by increasing BES. None of the RCTs reviewed measured the effects of the intervention on BES; therefore, it is unclear whether participants had weak BES at baseline or if the intervention had an effect on BES. It is still not known whether BES is a strong determinant of posture. A previous study of older adults with osteoporosis reported an association between BES and hyperkyphosis when the study population was stratified according to strong, moderate, or weak BES, but not when the data were pooled.43 In this study, only those categorized as having weak back extensors had significantly higher mean angles of kyphosis compared with the moderate and strong group means.43 Recently, a study of women with and without osteoporosis reported that the degree of thoracic kyphosis was negatively correlated with BES.44 In contrast, 1 of the studies in this review reported a significant improvement in BES without a corresponding improvement in posture,31 whereas another study reported that posture improved with exercise only among participants with weak BES and kyphosis of at least ≥34° at baseline.29 Variation across studies may be because of different techniques used to measure BES or differences in the sample populations. Future exercise trials could consider measuring baseline and change in BES to evaluate if it is a potential mechanism for any observed changes in hyperkyphotic posture. The fact that the interventions in all of the selected studies included exercises aimed at improving BES suggests that there is some consensus among researchers in the field that this is an important component to target. However, back extensor endurance has been measured in selected studies here and in studies of women with vertebral fracture,32,45 and it may be more relevant for maintaining upright posture.
Poor study design and reporting across many trials of exercise for the treatment of hyperkyphosis weaken the conclusions that can be derived and the generalizability of the work to date. The inconclusive findings in many studies may have been the result of small sample sizes or that few studies accounted for the exercise levels of participants at baseline. RCTs should state their power to detect a meaningful difference and perform an appropriate sample size calculation, as per Consolidated Standards of Reporting Trials guidelines.46 However, given that there is no consensus regarding a clinically meaningful change in kyphosis, these power calculations may be difficult. The 2 high-quality RCTs that incorporated physical therapy into their interventions observed a statistically significant improvement in kyphosis within the intervention group of >3°.32,35 The yoga intervention RCT noted a significant between-group difference in the flexicurve angle (but not the kyphometer angle) of 1.75° at follow-up.30 Many studies did not perform a true ITT analysis and likely overestimated the effect of their interventions. Conversely, above average activity levels at baseline might limit the potential efficacy of the interventions or create variability that would obscure the ability to observe between group differences. However, most studies saw improvements in other physical function outcomes,13,30-35,38,40 suggesting that there was room for improvement. Finally, the external validity of the trials to date may be limited; few studies included men, and many excluded individuals with vertebral fractures and were single-center trials. Although hyperkyphosis may progress more quickly in women than in men,25 there is no firm evidence that the prevalence of age-related hyperkyphosis is higher in women than in men.8,14,47 Individuals with vertebral fracture were often excluded for the purposes of safety; however, many individuals with hyperkyphosis present with underlying vertebral body wedging and VCFs.48 Similarly, excluding individuals with disability, comorbid conditions, or cognitive impairment may be relevant in a research setting but does not necessarily apply to an older adult population in a clinical setting where individuals with these coexisting conditions must be cared for. Finally, most studies recruited from a single clinic or outpatient department. Although recruiting from a single center may have the advantages of being convenient and less costly, the results of community-based or multicenter studies are generally more applicable to the external population.49
There are a number of methods for assessing posture and no clear consensus on which should be used in clinical trials; however, it has been suggested that the flexicurve may be favored because it is easy to use and will not introduce large errors when there are deformities, such as scoliosis, present in the ends of the spine, where the Cobb and kyphometer angle measurements are based.41 There were divergent results within studies that used multiple measures of posture in that they reported improvements in some, but not all, postural outcomes. Most trials did not use the criterion standard Cobb angle obtained from radiographs, avoiding unnecessary exposure to radiographs. Three of the measures used (flexicurve index, flexicurve angle, Debrunner kyphometer angle) have been validated against the Cobb angle measure with Pearson r values equal to .69, .69, and .62, respectively.41 The same validation study calculated a conversion factor to convert any of the 3 measures to the Cobb angle measure without having to take a radiograph,41 which may be useful in future studies. A few studies used photometric techniques and inclinometers and explanations regarding standardization of measurements were lacking. Although the inclinometer and photometric techniques used appeared reliable based on reported intraclass correlation coefficients, they have not been validated against the Cobb angle. Additionally, these techniques may not be relevant in a clinical setting where practitioners are likely to favor measurements that are less expensive and simpler to obtain, such as the flexicurve angle/index or occiput-to-wall distance. It is important to standardize the measurements of kyphosis because the degree of kyphosis can vary while standing in the usual or best posture. Moreover, a significant improvement in best posture may indicate improved spinal extension mobility, whereas an improvement in usual posture may indicate a decrease in the angle of kyphosis because of underlying musculoskeletal improvements.
Study limitations
The limitations of this review must be acknowledged. Studies that examined whether exercise can prevent the development of hyperkyphosis were excluded because the purpose of this review was specifically to determine if exercise could improve preexisting hyperkyphosis. The inclusion of studies that described participants as having flexed posture may not have accurately captured those with hyperkyphosis because we do not know the baseline mean angle of kyphosis of participants in these studies, thus limiting the conclusions that can be made based on these studies. The inclusion of only English language articles may have introduced bias. Three studies may have met the inclusion criteria based on screening their English abstracts.50-52 The heterogeneity across the studies and lack of available data do not allow for a meta-analysis to be done at this time.
Conclusions
Our ability to provide definitive conclusions about the effects of exercise on hyperkyphotic posture was limited by the quality of and heterogeneity in the study designs and reporting in the trials to date. A small number of RCTs suggest that exercise overseen by a physical therapist or trained instructor may result in a modest improvement in posture and that a common feature of the exercise was an emphasis on improved BES. However, there were studies that showed no effect; therefore, the findings should be confirmed in a high-quality RCT. Choosing a validated, precise, and clinically relevant outcome measure, specifying a criterion for hyperkyphosis at baseline, including participants who are male, and measuring BES are considerations for future trials.
Acknowledgments
We thank Jackie Stapleton for her assistance with the development of the literature search strategy.
Supported by the National Institute on Aging (grant no. RO1 AG041921); the Office of Research in Women’s Health and the National Institute of Arthritis and Musculoskeletal and Skin Diseases (grant no. P50 AR063043); the Ontario Ministry of Research and Innovation; and the Canadian Institutes of Health Research.
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit on the authors or on any organization with which the authors are associated.
List of abbreviations
- BES
back extensor muscle strength
- ITT
intention-to-treat analysis
- RCT
randomized controlled trial
- VCF
vertebral compression fracture
Appendix 1 Database Search Strategies and Results as of October 2012
PubMed Search
#1 “exercise” [mesh] OR “exercise” [tiab] OR “yoga” [tiab] OR “pilates” [tiab] OR “exercise therapy” [tiab] OR “physical activity” [tiab] OR “exercise movement techniques” [tiab] OR “resistance training” [tiab] OR “weight lifting” [mesh] OR “exercise therapy” [mesh] OR “exercise movement techniques” [mesh] OR “physical fitness” [MeSH]
#2 “posture” [tiab] OR “spinal curvature” [tiab] OR “hyperkyphosis” [tiab] OR “kyphosis” [tiab] OR “skeletal alignment” [tiab] OR “kyphosis” [mesh]
#3 “elderly” [tiab] OR “older adults” [tiab] OR “seniors” [tiab] OR “older people” [tiab] OR “middle aged” [tiab] OR “aged” [mesh] OR “middle aged” [mesh]
Final Search: #1 AND #2 AND #3
Yield: 579 hits
Cumulative Index to Nursing and Allied Health Literature Search
#1 MH (“exercise” OR “therapeutic exercise”) OR TX (“exercise” OR “pilates” OR “yoga” OR “physical activity” OR “exercise movement techniques” OR “resistance training”)
#2 TX “posture” OR “spinal curvature” OR “hyperkyphosis” OR “kyphosis” OR “skeletal alignment”
#3 MH (“aged” OR “middle age” OR “frail elderly”) OR TX (“elderly” OR “older adults” OR “in old age”)
Final Search: S1 AND S2 AND S3
Yield: 367 hits
Embase Search
#1 kyphosis/di, dm, pc, rh, th [Diagnosis, Disease Management, Prevention, Rehabilitation, Therapy]
#2 posture.tw
#3 spinal curvature.tw
#4 skeletal alignment.tw
#5 hyperkyphosis.tw
#6 1 or 2 or 3 or 4 or 5
#7 exercise/ or aerobic exercise/ or anaerobic exercise/ or aquatic exercise/ or arm exercise/ or breathing exercise/ or dynamic exercise/ or endurance training/ or isokinetic exercise/ or muscle exercise/ or pilates/ or plyometrics/ or resistance training/ or static exercise/
#8 exercise therapy.tw
#9 physical activity/ or cycling/ or jogging/ or jumping/ or lifting effort/ or running/ or stretching/ or swimming/ or walking/ or weight bearing/ or weight lifting/
#10 yoga/th [Therapy]
#11 7 or 8 or 9 or 10
#12 aged/
#13 older adults.tw
#14 middle aged/
#15 seniors.tw
#16 12 or 13 or 14 or 15
Final Search: #6 and #11 and #16
Yield: 391
Total number of titles from databases before duplicates deleted: 1337
Total number of titles from databases after duplicates deleted: 1058
Footnotes
Presented to the Toronto Rehabilitation Institute, November 23, 2012, Toronto, ON, Canada.
References
- 1.Kado DM, Huang MH, Karlamangla AS, Barrett-Connor E, Greendale GA. Hyperkyphotic posture predicts mortality in older community-dwelling men and women: a prospective study. J Am Geriatr Soc. 2004;52:1662–7. doi: 10.1111/j.1532-5415.2004.52458.x. [DOI] [PubMed] [Google Scholar]
- 2.Takahashi T, Ishida K, Hirose D, et al. Trunk deformity is associated with a reduction in outdoor activities of daily living and life satisfaction in community-dwelling older people. Osteoporosis Int. 2005;16:273–9. doi: 10.1007/s00198-004-1669-3. [DOI] [PubMed] [Google Scholar]
- 3.Teramoto S, Suzuki M, Matsuse T, et al. [Influence of kyphosis on the age-related decline in pulmonary function] [Japanese] Nihon Ronen Igakkai Zasshi. 1998;35:23–7. doi: 10.3143/geriatrics.35.23. [DOI] [PubMed] [Google Scholar]
- 4.Ryan SD, Fried LP. The impact of kyphosis on daily functioning. J Am Geriatr Soc. 1997;45:1479–86. doi: 10.1111/j.1532-5415.1997.tb03199.x. [DOI] [PubMed] [Google Scholar]
- 5.Kado DM, Huang MH, Nguyen CB, Barrett-Connor E, Greendale GA. Hyperkyphotic posture and risk of injurious falls in older persons: the Rancho Bernardo Study. J Gerontol A Biol Sci Med Sci. 2007;62:652–7. doi: 10.1093/gerona/62.6.652. [DOI] [PubMed] [Google Scholar]
- 6.Sinaki M, Brey RH, Hughes CA, Larson DR, Kaufman KR. Balance disorder and increased risk of falls in osteoporosis and kyphosis: significance of kyphotic posture and muscle strength. Osteoporosis Int. 2005;16:1004–10. doi: 10.1007/s00198-004-1791-2. [DOI] [PubMed] [Google Scholar]
- 7.Lyles KW, Gold DT, Shipp KM, Pieper CF, Martinez S, Mulhausen PL. Association of osteoporotic vertebral compression fractures with impaired functional status. Am J Med. 1993;94:595–601. doi: 10.1016/0002-9343(93)90210-g. [DOI] [PubMed] [Google Scholar]
- 8.Schneider DL, Von Mühlen DG, Barrett-Connor E, Sartoris DJ. Kyphosis does not equal vertebral fractures: the Rancho Bernardo Study. J Rheumatol. 2004;31:747–52. [PubMed] [Google Scholar]
- 9.Bartynski WS, Heller MT, Grahovac SZ, Rothfus WE, Kurs-Lasky M. Severe thoracic kyphosis in the older patient in the absence of vertebral fracture: association of extreme curve with age. Am J Neuroradiol. 2005;26:2077–85. [PMC free article] [PubMed] [Google Scholar]
- 10.Briggs AM, Van Dieën JH, Wrigley TV, et al. Thoracic kyphosis affects spinal loads and trunk muscle force. Phys Ther. 2007;87:595–607. doi: 10.2522/ptj.20060119. [DOI] [PubMed] [Google Scholar]
- 11.Bruno AG, Anderson DE, D’Agostino J, Bouxsein ML. The effect of thoracic kyphosis and sagittal plane alignment on vertebral compressive loading. J Bone Miner Res. 2012;27:2144–51. doi: 10.1002/jbmr.1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang MH, Barrett-Connor E, Greendale GA, Kado DM. Hyperkyphotic posture and risk of future osteoporotic fractures: the Rancho Bernardo Study. J Bone Miner Res. 2006;21:419–23. doi: 10.1359/JBMR.051201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katzman WB, Sellmeyer DE, Stewart AL, Wanek L, Hamel KA. Changes in flexed posture, musculoskeletal impairments, and physical performance after group exercise in community-dwelling older women. Arch Phys Med Rehabil. 2007;88:192–9. doi: 10.1016/j.apmr.2006.10.033. [DOI] [PubMed] [Google Scholar]
- 14.Katzman WB, Wanek L, Shepherd JA, Sellmeyer DE. Age-related hyperkyphosis: its causes, consequences, and management. J Orthop Sports Phys Ther. 2010;40:352–60. doi: 10.2519/jospt.2010.3099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kado DM. The rehabilitation of hyperkyphotic posture in the elderly. Eur J Phys Rehabil Med. 2009;45:583–93. [PubMed] [Google Scholar]
- 16.Lewiecki EM. Kyphosis and vertebral fractures: what do we know now? Aging Health. 2009;5:483–7. [Google Scholar]
- 17.Perriman DM, Scarvell JM, Hughes AR, Lueck CJ, Dear KB, Smith PN. Thoracic hyperkyphosis: a survey of Australian physiotherapists. Physiother Res Int. 2012;17:167–78. doi: 10.1002/pri.529. [DOI] [PubMed] [Google Scholar]
- 18.Greig AM, Bennell KL, Briggs AM, Hodges PW. Postural taping decreases thoracic kyphosis but does not influence trunk muscle electromyographic activity or balance in women with osteoporosis. Man Ther. 2008;13:249–57. doi: 10.1016/j.math.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 19.Pfeifer M, Kohlwey L, Begerow B, Minne HW. Effects of two newly developed spinal orthoses on trunk muscle strength, posture, and quality-of-life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil. 2011;90:805–15. doi: 10.1097/PHM.0b013e31821f6df3. [DOI] [PubMed] [Google Scholar]
- 20.Vogt L, Hübscher M, Brettmann K, Banzer W, Fink M. Postural correction by osteoporosis orthosis (osteo-med): a randomized, placebo-controlled trial. Prosthet Orthot Int. 2008;32:103–10. doi: 10.1080/03093640701838265. [DOI] [PubMed] [Google Scholar]
- 21.Teng MM, Wei CJ, Wei LC, et al. Kyphosis correction and height restoration effects of percutaneous vertebroplasty. AJNR Am J Neuroradiol. 2003;24:1893–900. [PMC free article] [PubMed] [Google Scholar]
- 22.Theodorou DJ, Theodorou SJ, Duncan TD, Garfin SR, Wong WH. Percutaneous balloon kyphoplasty for the correction of spinal deformity in painful vertebral body compression fractures. Clin Imaging. 2002;26:1–5. doi: 10.1016/s0899-7071(01)00350-3. [DOI] [PubMed] [Google Scholar]
- 23.Kim YY, Rhyu KW. Recompression of vertebral body after balloon kyphoplasty for osteoporotic vertebral compression fracture. Eur Spine J. 2010;19:1907–12. doi: 10.1007/s00586-010-1479-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bergland A, Thorsen H, Kåresen R. Effect of exercise on mobility, balance, and health-related quality of life in osteoporotic women with a history of vertebral fracture: a randomized, controlled trial. Osteoporosis Int. 2011;22:1863–71. doi: 10.1007/s00198-010-1435-7. [DOI] [PubMed] [Google Scholar]
- 25.Fon GJ, Pitt MJ, Thies AC., Jr. Thoracic kyphosis: range in normal subjects. Am J Roentgenol. 1980;134:979–83. doi: 10.2214/ajr.134.5.979. [DOI] [PubMed] [Google Scholar]
- 26.Voutsinas SA, MacEwen GD. Sagittal profiles of the spine. Clin Orthop Relat Res. 1986;(210):235–42. [PubMed] [Google Scholar]
- 27.Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pawlowsky SB, Hamel KA, Katzman WB. Stability of kyphosis, strength, and physical performance gains 1 year after a group exercise program in community-dwelling hyperkyphotic older women. Arch Phys Med Rehabil. 2009;90:358–61. doi: 10.1016/j.apmr.2008.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Itoi E, Sinaki M. Effect of back-strengthening exercise on posture in healthy women 49 to 65 years of age. Mayo Clin Proc. 1994;69:1054–9. doi: 10.1016/s0025-6196(12)61372-x. [DOI] [PubMed] [Google Scholar]
- 30.Greendale GA, Huang MH, Karlamangla AS, Seeger L, Crawford S. Yoga decreases kyphosis in senior women and men with adult-onset hyperkyphosis: results of a randomized controlled trial. J Am Geriatr Soc. 2009;57:1569–79. doi: 10.1111/j.1532-5415.2009.02391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bergström I, Bergström K, Kronhed AG, Karlsson S, Brinck J. Back extensor training increases muscle strength in postmenopausal women with osteoporosis, kyphosis and vertebral fractures. Adv Physiother. 2011;13:110–7. [Google Scholar]
- 32.Bennell KL, Matthews B, Greig A, et al. Effects of an exercise and manual therapy program on physical impairments, function and quality-of-life in people with osteoporotic vertebral fracture: a randomised, single-blind controlled pilot trial. BMC Musculoskelet Disord. 2010;11:36. doi: 10.1186/1471-2474-11-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Benedetti MG, Berti L, Presti C, Frizziero A, Giannini S. Effects of an adapted physical activity program in a group of elderly subjects with flexed posture: clinical and instrumental assessment. J Neuroeng Rehabil. 2008;5:32. doi: 10.1186/1743-0003-5-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schuerman S. Relationships between postural exercise and risk factors for falling in individuals with osteoporosis [dissertation] University of Nebraska; Omaha: 1998. [Google Scholar]
- 35.Bautmans I, Van Arken J, Van Mackelenberg M, Mets T. Rehabilitation using manual mobilization for thoracic kyphosis in elderly postmenopausal patients with osteoporosis. J Rehabil Med. 2010;42:129–35. doi: 10.2340/16501977-0486. [DOI] [PubMed] [Google Scholar]
- 36.Abreu DC, Matos MS, Costa GC, Trevisan DC, Reis JG. The effect of physical exercise on thoracic hyperkyphosis in osteoporotic elderly women. Osteoporosis Int. 2012;23(Suppl 2):S120. [abstract] [Google Scholar]
- 37.Papaioannou A, Morin S, Cheung AM, et al. clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ. 2010;2010;182:1864–73. doi: 10.1503/cmaj.100771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Greendale GA, McDivit A, Carpenter A, Seeger L, Huang MH. Yoga for women with hyperkyphosis: results of a pilot study. Am J Public Health. 2002;92:1611–4. doi: 10.2105/ajph.92.10.1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kuo YL, Tully EA, Galea MP. Sagittal spinal posture after pilates-based exercise in healthy older adults. Spine (Phila Pa 1976) 2009;34:1046–51. doi: 10.1097/BRS.0b013e31819c11f8. [DOI] [PubMed] [Google Scholar]
- 40.Renno AC, Granito RN, Driusso P, Costa D, Oishi J. Effects of an exercise program on respiratory function, posture and on quality of life in osteoporotic women: a pilot study. Physiotherapy. 2005;91:113–8. [Google Scholar]
- 41.Greendale GA, Nili NS, Huang MH, Seeger L, Karlamangla AS. The reliability and validity of three non-radiological measures of thoracic kyphosis and their relations to the standing radiological Cobb angle. Osteoporosis Int. 2011;22:1897–905. doi: 10.1007/s00198-010-1422-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Katzman W, Cawthon P, Hicks GE, et al. Association of spinal muscle composition and prevalence of hyperkyphosis in healthy community-dwelling older men and women. J Gerontol A Biol Sci Med Sci. 2011;67:191–5. doi: 10.1093/gerona/glr160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mika A, Fernhall B, Mika P. Association between moderate physical activity, spinal motion and back muscle strength in postmenopausal women with and without osteoporosis. Disabil Rehabil. 2009;31:734–40. doi: 10.1080/09638280802308998. [DOI] [PubMed] [Google Scholar]
- 44.Granito RN, Aveiro MC, Renno AC, Oishi J, Driusso P. Comparison of thoracic kyphosis degree, trunk muscle strength and joint position sense among healthy and osteoporotic elderly women: a cross-sectional preliminary study. Arch Gerontol Geriatr. 2012;54:e199–202. doi: 10.1016/j.archger.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 45.Shipp KM, Gold DT, Pieper CF, Lyles KW. Improving trunk strength and endurance in older women with vertebral fractures [abstract] J Bone Miner Res. 2010;22:S463. [Google Scholar]
- 46.Altman DG, Moher D, Schulz KF. Improving the reporting of randomised trials: the CONSORT statement and beyond. Stat Med. 2012;31:2985–97. doi: 10.1002/sim.5402. [DOI] [PubMed] [Google Scholar]
- 47.Kado DM, Prenovost K, Crandall C. Narrative review: hyperkyphosis in older persons. Ann Intern Med. 2007;147:330–8. doi: 10.7326/0003-4819-147-5-200709040-00008. [DOI] [PubMed] [Google Scholar]
- 48.Puche RC, Morosano M, Masoni A, et al. The natural history of kyphosis in postmenopausal women. Bone. 1995;17:239–46. doi: 10.1016/8756-3282(95)00212-v. [DOI] [PubMed] [Google Scholar]
- 49.Bellomo R, Warrillow SJ, Reade MC. Why we should be wary of single-center trials. Crit Care Med. 2009;37:3114–9. doi: 10.1097/CCM.0b013e3181bc7bd5. [DOI] [PubMed] [Google Scholar]
- 50.Wang R-, Wang Y, Bai J-, et al. Effects of rehabilitation exercise on pulmonary function, thoracic kyphosis and physical activity in old female patients with osteoporosis. Chinese Journal of Clinical Rehabilitation. 2006;10:34–6. [Google Scholar]
- 51.Angin E, Erden Z. Effects of exercise training on pain, spinal mobility, lordosis and kyphosis angle in osteoporosis: a pilot study. Turk Geriatri Dergisi. 2010;13:117–24. [Google Scholar]
- 52.Capponi D, Hlebs S. The impact of physical activity on the severity of spine curvatures and balance disorders in postmenopausal women. Slovenian Nursing Review. 2008;42:77–86. [Google Scholar]