Abstract
Background Globally, adults aged 65 years or older will increase from 516 million in 2009 to an estimated 1.53 billion in 2050. Due to substance use at earlier ages that may continue into later life, and ageing-related changes in medical conditions, older substance users are at risk for substance-related consequences.
Methods MEDLINE and PsychInfo databases were searched using keywords: alcohol use disorder, drug use disorder, drug misuse, substance use disorder, prescription drug abuse, and substance abuse. Using the related-articles link, additional articles were screened for inclusion. This review focused on original studies published between 2005 and 2013 to reflect recent trends in substance use disorders. Studies on psychiatric comorbidity were also reviewed to inform treatment needs for older adults with a substance use disorder.
Results Among community non-institutionalized adults aged 50+ years, about 60% used alcohol, 3% used illicit drugs and 1–2% used nonmedical prescription drugs in the past year. Among adults aged 50+, about 5% of men and 1.4% of women had a past-year alcohol use disorder. Among alcohol users, about one in 14 users aged 50–64 had a past-year alcohol use disorder vs one in 30 elder users aged 65+. Among drug users aged 50+, approximately 10–12% had a drug use disorder. Similar to depressive and anxiety disorders, substance use disorders were among the common psychiatric disorders among older adults. Older drug users in methadone maintenance treatment exhibited multiple psychiatric or medical conditions. There have been increases in treatment admissions for illicit and prescription drug problems in the United States.
Conclusions Substance use in late life requires surveillance and research, including tracking substance use in the racial/ethnic populations and developing effective care models to address comorbid medical and mental health problems.
Keywords: Epidemiology, substance use disorders, older adults, comorbidity
Introduction
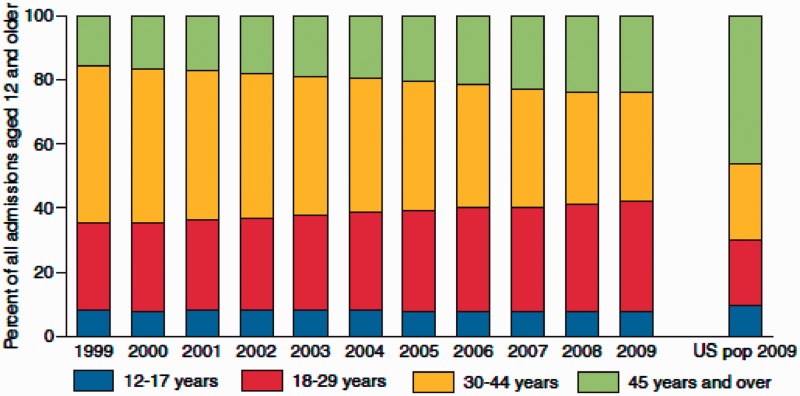
Globally, adults aged 65 years or older will increase from 516 million in 2009 to an estimated 1.53 billion in 2050.1 Improved health and longevity have contributed to a steadily rising number of the ageing population.2 Americans use more psychoactive substances than individuals in other countries.3 In the USA, adults aged 45–64 years, persons born in the post-World War II period and older adults aged 65+ years are the fastest growing age groups. Between 2000 and 2010, they increased by 31.5% (from 22.0% to 26.4% of the US population) and 15.1% (from 12.4% to 13.5% of the US population), respectively, compared with an increase of 9.7% for the total US population.4 Conservative estimates from national surveys of non-institutionalized adults show that the number of Americans aged 50+ years with a substance use disorder (SUD; alcohol or drug use disorders) will double from 2.8 million (annual average) in 2002–06 to 5.7 million in 2020.5 The increase in the number of people with a SUD will occur in all sex and racial/ethnic groups because of combined effects of the growing number of older adults and of persons with a SUD.5 Substance abuse can affect almost all major organs,6 and SUD is a relapsing condition.7 Adults aged 18–64 years (63% of the US population) who comprise the vast majority of problematic substance users—continue to age and are expected to place an increasing burden on health care systems over time.5,8,9 Data from the Treatment Episode Data Set (TEDS), which collects national-level admissions to substance abuse treatment facilities that receive public funds, demonstrate an escalating demand for health services for SUDs among middle-aged and older adults (Figure 1).10
Figure 1.
Age at admission for substance abuse treatments: Treatment Episode Data Set (TEDS) 1999–2009; U.S. population 2009. Source: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Service Adminstration, Treatment Episode Data Set (TEDS). Data received through 11 March 2010. U.S. Bureau of the Census. Annual State Resident Population Estimates for 6 Race Groups by Age, Sex, and Hispanic Origin: 1 April 2000 to 1 July 2009 (SC-EST2009-ALLDATA6, released June, 2010)
Older adults are uniquely at risk for substance-related consequences. Ageing-related physiological changes can enhance one’s sensitivity to adverse effects of substance use. Substances of abuse act by altering neurotransmission in the brain; ageing-related changes to the brain, drug metabolism and pharmacokinetics may interact and intensify older substance users’ risk for developing neurotoxicity and severe medical consequences.11,12 Ageing-related decline in health status also increases older adults’ likelihood of taking medications for either medical or psychological conditions and they may also self-medicate with non-prescription substances. For instance, approximately one in four older adults used psychoactive medications with abuse potential.12 Medication use could interact with substance use and cause adverse effects. Substance use may trigger or intensify medical conditions, such as diabetes and cardiovascular disease,6,13 Use of psychoactive medications also can lead to nonmedical use or even dependence.12,14
Here, we review the extent of SUD (abuse of or dependence on alcohol or drugs) and comorbid psychiatric conditions among adults aged 50+ years to gauge the problems and identify venues for research and intervention. Adults aged 50–64 years, approximately the baby-boom population, are included in this review, because they use more alcohol and illicit/nonmedical drugs than adults 65+ years of age, represent a large proportion of the population and place increasing demands for SUD treatment as they continue to age.4,5
Methods
We combined keywords for SUD (alcohol use disorder, alcohol abuse, alcohol dependence, drug use disorder, drug abuse, drug dependence, drug misuse, substance use disorder, prescription drug abuse, substance abuse) with older adults or geriatric population and searched the PubMed and PsychInfo database. We reviewed abstracts of more than 200 citations, used related citations links to identify additional articles from journal databases and examined the bibliographies of articles that we reviewed. We found that study data were often collected many years earlier than dates on which results were published. To reflect recent trends in substance use, we focused on studies published 2005 onwards. Articles that met the inclusion criteria are summarized in Table 1 (peer-reviewed articles in English language and original studies). We included relevant findings from additional studies to augment the description of the extent of SUDs. To inform treatment needs for older adults with a SUD, we also reviewed original, peer-reviewed studies of psychiatric comorbidity among older adults.
Table 1.
Peer-reviewed studies of substance use disorders
| Authors | Year/ Country | Design | Data source | Sample/ Age in year | Substance | Selected findings |
|---|---|---|---|---|---|---|
| Huang et al.24 | 2006/USA | Cross-sectional | 2000–2001 NESARC | n = 43093; ≥18 years | Drugs | Lifetime nonmedical prescription drug disorder by age groups: 18–29 years, 30–44, 45–64, 65+, respectively:
|
| Kohn et al.19 | 2008/Chile | Cross-sectional | 1992–1999 CPPS | n = 352; ≥65 years | Alcohol, Drugs |
|
| Préville et al.28 | 2008/Canada | Cross-sectional | 2005–2006 ESA | n = 2798; ≥65 years | Benzodia-zepine | Past-year prevalence: benzodiazepine dependence, 2.3%, mood disorder, 7.4%; anxiety disorder, 5.6% |
| Blazer & Wu20 | 2009/USA | Cross-sectional | 2005–2006 NSDUH | n = 10953; ≥50 years | Alcohol, Drugs |
|
| Han et al.5 | 2009/USA | Cross-sectional | 2002–2006 NSDUH | n = 25525; ≥50 years | Alcohol, Drugs | Model-based estimations for alcohol/drug disorder among adults aged 50+: 3.4% in 2002–2006 vs 4.9% in 2020 |
| Sacco et al.31 | 2009/USA | Cross-sectional | 2000–2001 NESARC | n = 4646; ≥60 years | Alcohol |
|
| Gum et al.17 | 2009/USA | Cross-sectional | 2001–2003 NCS-R | n = 1461; ≥65 years | Alcohol, Drugs |
|
| Voyer et al.14 | 2009/Canada | Cross-sectional | 2005–2006 ESA | n = 2785; ≥65 years | Benzodia-zepine |
|
| Blazer & Wu22 | 2011/USA | Cross-sectional | 2005–2007 NSDUH | n = 16304; ≥50 years | Alcohol, Drugs |
|
| Lin et al.18 | 2011/USA | Cross-sectional | 2000–2001 NESARC | n = 8205; ≥65 years | Alcohol, Drugs |
|
| Chou et al.15 | 2011/USA | Longitu-dinal | 2000–2001 & 2004–2005 NESARC | n = 8012; ≥60 years | Alcohol, Drugs | Incidence of disorder within 3 years: alcohol, 1.4%; drug, 0.3%; major depression, 3.3%; generalized anxiety disorder, 1.6% |
| Verges et al.16 | 2012/USA | Longitu-dinal | 2000–2001 & 2004–2005 NESARC | n = 43 093 at wave1; n = 34 653 at wave2 | Alcohol | Alcohol dependence at wave 2 (as shown in figures):
|
CPPS, Chile Psychiatric Prevalence Study; ESA, Enquête sur la Santé des Aînés or Quebec Survey on the Health of Seniors; NCS-R, National Comorbidity Survey-Replication; NESARC, National Epidemiologic Survey on Alcohol and Related Conditions; NSDUH, National Survey on Drug Use and Health.
Results
Substance use disorders
There is a lack of large-scale studies that specifically gauge SUDs and treatment needs in the ageing population (Table 1). Most studies examined the subsamples of older adults from national samples of survey studies, including the National Comorbidity Study-Replication (NCS-R), National Survey on Drug Use and Health (NSDUH) and the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Few studies examined incidence rates of SUDs using the longitudinal data from the NESARC.15,16
Alcohol use disorders
Using data from older adults aged 65+ years in the 2001–03 NCS-R (n = 1461), Gum et al. (2009)17 found that 4.1% of older adults aged 65–75 (8.1%, men; 1.0%, women) and 1.6% of adults aged 75+ (2.1%, men; 1.3%, women) reported a lifetime history of alcohol use disorder. Lin et al. (2011)18 analysed data from 8205 older adults aged 65+ in the 2000–01 NESARC; lifetime and past-year prevalences of alcohol use disorders were found to be 16.1% and 1.5%, respectively. Ages 65–74 (vs 75+ years), male sex, being White (vs being Asian/Pacific Islander) and being divorced/widowed were associated with elevated odds of having a lifetime alcohol use disorder; ages 65–74 (vs 75+ years) and male sex were associated with elevated odds of having a past-year alcohol use disorder.18 This is one of the first studies reporting rates of past-year alcohol use disorders in a national sample of older adults, but the number of older adults with a past-year alcohol use disorder (n = 109) limits analyses of correlates and frequency of recent alcohol use. Based on the data from the Chile Psychiatric Prevalence Study (CPPS) conducted between 1992 and 1999, Kohn et al. (2008)19 found that alcohol/drug use disorders (5.3%), like mood (3.7%) and anxiety disorders (4.4%), were the most prevalent past-year psychiatric disorders among 352 older adults aged 65+ years. Although the small sample size excluded analyses of correlates of SUD, Kohn et al. (2008)19 reported that none of these older adults used treatments for a SUD in the past 6 months. These studies demonstrate that a sufficiently large sample of older adults is needed to better estimate the extent of recent or active substance use and SUDs.
By pooling the data from two independent national surveys of the NSDUH in 2005–06, Blazer and Wu (2009)20 examined the frequency of alcohol use and alcohol disorders among 10 953 adults aged 50+ years. Overall, 60% of adults aged 50+ used alcohol in the past year; factors associated with elevated odds of past-year alcohol use included ages 50–64 (vs ages 65+), male sex, being White or Hispanic (vs being Black), college education, being employed, high family income and residence in metropolitan areas. Among past-year alcohol users aged 50+, 61.9% reported using alcohol on 30+ days in the past year (mean 103.5 days/year) and 5.0% had an alcohol use disorder in the past year. This analysis of a large sample shows frequent alcohol use among adults aged 50+.
Based on the American Geriatric Society’s clinical guidelines for defining low-risk and at-risk alcohol use, Blazer and Wu (2009)21 investigated the magnitude and correlates of low-risk use (no more than 1 drink on a usual drinking day within the past 30 days), at-risk use (2 or more drinks on a usual drinking day within the past 30 days) and binge drinking (5 or more drinks on the same occasion on at least 1 day within the past 30 days). The findings revealed prevalent rates of current at-risk and binge alcohol use among adults aged 50+ in both men (16.7% and 19.6%, respectively) and women (10.9% and 6.3%, respectively). Among men, ages 50–64 (vs ages 65+), being Hispanic (vs being Black), being employed, being separated/divorced/widowed, high family income, college education, past-year tobacco use and past-year illicit drug use were associated with elevated odds of binge drinking. Among women, ages 50–64 (vs ages 65+), being separated/divorced/widowed, college education, being employed, past-year tobacco use, past-year illicit drug use and past-year nonmedical prescription drug use were associated with elevated odds of binge drinking.21 The large sample helped identify unexpected but prevalent at-risk and binge alcohol use among older men (27.5%) and women (11.4%) aged 65+, demonstrating that an exclusive use of alcohol use disorders in a study can overlook a large number of older problematic alcohol users who may benefit from early intervention.
Subsequently, Blazer and Wu (2011)22 examined patterns of subthreshold and threshold alcohol use disorders among 16 304 adults aged 50+ years. The study documented new national estimates of past-year DSM-IV alcohol dependence (≥3 dependence symptoms), abuse (≥1 abuse symptoms), subthreshold dependence (1–2 dependence symptoms plus no abuse symptoms) and use without DSM-IV symptoms among adults aged 50–64 (1.9%, 2.3%, 7.0% and 44.7%, respectively) and older adults aged 65+ (0.6%, 0.9%, 5.2% and 36.4%, respectively). The results unveil the extent of subthreshold alcohol disorders. At least 6.3% of adults aged 50+ in the community exhibited some alcohol dependence symptoms (including men and adults with college education), but they may not be identified because of not having engaged in activities that may lead to legal, job-related or relationship consequences (DSM-IV defined abuse). Of note, many adults aged 50+ with alcohol dependence, abuse or subthreshold dependence were frequent alcohol users (mean numbers of alcohol-using days/year: 215, 204 and 171 days, respectively) and engaged in binge drinking in the past month (70.3%, 61.6% and 48.2%, respectively). The frequency of binge drinking is especially of concern. The coming new DSM5 combines dependence and abuse as a disorder and requires presence of ≥2 abuse/dependence symptoms for having a SUD.23 The DSM5 will include some subthreshold alcohol users in the threshold group; however, it also excludes alcohol users with one abuse symptom only from the threshold group. Research will be needed to evaluate how DSM5 influences prevalence estimates of SUDs among older adults.
With the large sample of alcohol users available, it became possible to examine conditional prevalences of alcohol use disorders (probability of having a disorder-given use) to identify subgroups with elevated odds of having SUDs. Blazer and Wu (2011)22 reported conditional prevalences of alcohol use disorders (7.4%) and subthreshold dependence (12.5%) among 5548 past-year alcohol users aged 50–64 as well as conditional prevalences of alcohol use disorders (3.4%) and subthreshold dependence (12.1%) among 3478 past-year alcohol users aged 65+.22 Conditional prevalences of SUDs identify potential risk groups of SUDs to supplement the limitation of prevalence rates in the total sample. Adjusted logistic regression analyses of past-year alcohol users showed that ages 50–64, male sex, being Black, being separated/divorced/widowed, low family income, major depression, current nicotine dependence, past-year illicit drug use, past-year nonmedical prescription drug use and early onset of alcohol use (<18 years) were associated with elevated odds of having an alcohol use disorder. In addition, male sex, being Black, being Hispanic, low family income, nicotine dependence, nonmedical prescription drug use and early onset of alcohol use were associated with elevated odds of having subthreshold alcohol dependence in the past year.
Taken together, alcohol use is common among adults aged 50+, but alcohol use problems or disorders are likely to affect subsets of alcohol users who are male, separated/divorced/widowed, low-income or depressed, as well as alcohol users who also use or abuse other psychoactive substances.
Drug use disorders
Compared with alcohol, relatively few studies examine illicit or nonmedical drug use problems in a representative sample of older adults.9 Huang et al. (2006)24 reported lifetime prevalences of nonmedical drug use for four age groups, 18–29, 30–44, 45–64 and 65+ years in the 2000–01 NESARC, including sedatives (4.7%, 5.1%, 4.3% and 1.1%, respectively), tranquillizers (4.7%, 4.2%, 3.3% and 0.7%, respectively), opioids (7.4%, 5.7%,3.9% and 1.1%, respectively) and amphetamines (4.4%, 6.8%, 4.9% and 0.4%, respectively). Moor et al. (2009)25 specifically examined adults aged 65+ (n = 8205) in the 2000–01 NESARC; 3.5% of the sample reported any lifetime use of illicit or nonmedical drugs and 1.1% reported any past-year use of illicit or nonmedical drugs. In addition, only 0.6% of adults aged 65+ had a lifetime drug use disorder (cannabis, 0.21%; opioids, 0.16%; tranquillizers, 0.13%; amphetamine, 0.11%; sedatives, 0.07%), and 0.2% had a past-year drug use disorder.18 The very low rate of drug use in the national sample of non-institutionalized older adults may explain the scarcity of drug abuse research in the geriatric population. It also shows the need for a particularly large sample size of the general population to produce reliable drug use estimates.
Blazer and Wu (2009)20 examined recent use of illicit drugs among 10 953 non-institutionalized adults aged 50+ from the 2005–06 NSDUH. Of all drugs examined, marijuana use exhibited the highest prevalence of use in the past year (3.9% among adults aged 50–64; 0.7% among adults aged 65+). Rates of past-year illicit use of other drugs among adults aged 50+ were low: cocaine (0.4%), inhalants (0.1%), hallucinogens (0.1%), methamphetamine (0.1%) and and heroin (0.05%). Consistent with drug use in younger adults, marijuana is the most common illicit drug used by older adults. Although the number of older illicit drug users identified from surveys of the general population was small, many older drug users reported drug use regularly, suggesting a high liability to experiencing a drug use disorder. For example, 49% of marijuana users and 57% of cocaine users used the drug on 30+ days in the past year (mean number of drug-using days/year: marijuana, 81 days; cocaine, 101 days). Conditional rates of SUDs reveal that drug users are more likely to experience a SUD than are alcohol users: close to 12% of past-year drug users aged 50+ had a drug use disorder, whereas about 5% of past-year alcohol users aged 50+ had an alcohol use disorder.20
Similarly, few studies specifically examine recent nonmedical prescription drug use and disorders among older adults. Results from 10 953 adults aged 50+ showed that nonmedical use of prescription opioids (e.g. Darvocet, Vicodin, Percocet, hydrocodone) had a higher past-year prevalence (1.4%) than nonmedical use of other prescription drugs (tranquillizers, 0.5%; stimulants, 0.2%; sedatives, 0.1%).26 Like alcohol use, nonmedical opioid use was more common among adults aged 50–64 (vs adults aged 65+), men and marijuana users. Of all nonmedical prescription opioid users, one-fifth (21%) reported onset of first nonmedical use at age 50+, and the majority started nonmedical prescription opioid use between aged 18 and 39 years (51.0%). Overall, 9.4% of past-year nonmedical opioid users met criteria for having a prescription opioid abuse (1.7%) or dependence (7.6%) disorder in the past year.26 Therefore, use of one substance increases the likelihood of using another substance, and the majority (81%) of older adults with a prescription opioid use disorder exhibited dependence symptoms. Although marijuana use was more prevalent than opioid use in the general population, treatment admission data (TEDS) found opioids the most frequently reported primary illicit drugs by treatment-seeking adults 50+,27 suggesting more severe drug problems among opioid users than marijuana users. This is in line with a low conditional rate of marijuana use disorders (4.5%).20
In Canada, Préville and colleagues (2008) conducted a cross-sectional survey in 2005–06 to determine the extent of psychiatric disorders among adults aged 65 years in Quebec (n = 2798).28 DSM-IV benzodiazepine dependence was the only SUD reported in their study. Past-year prevalence of benzodiazepine dependence (2.3%) was lower than prevalences of anxiety (5.6) or mood disorder (7.4%). Overall, 12.7% had any of these disorders; ages 65–74 years (vs ages 75+ years) and female sex were associated with increased odds of having any disorder.28 The study team also characterized benzodiazepine dependence.14 Of the 707 current medical benzodiazepine users aged 65+ identified by the survey, 9.5% met criteria for having past-year benzodiazepine dependence. Female sex, mild cognitive impairment, depression, panic disorder and suicidal ideation were associated with benzodiazepine dependence.14 This high conditional rate of benzodiazepine dependence may be related partly to the sample’s unique characteristics. For instance, benzodiazepine users were ‘medical users’ of benzodiazepines, and they might have used this medication for a long time as shown in the associations between benzodiazepine dependence and mental health conditions (depression, panic disorder) and a high rate of mood or anxiety disorder (31.3%) among benzodiazepine-dependent adults. Although the study does not include data about patterns of benzodiazepine use and other substance use problems, results suggest the need to examine prescription drug use problems among older medical users of psychoactive medications, including benzodiazepines and opioids.
Incidence rates of SUDs
The NESRAC appears to be the only known national survey that uses longitudinal designs (with two waves of data collection in 2000–01 and 2004–05) to permit analysis of new cases (incidence) of SUDs in a representative sample of older adults. Chou et al. (2011)15 examined incidence rates of SUDs and other mental disorders among 8012 adults aged 60+ in the NESARC. Over a period of 3 years, 1.0% of adults aged 60+ developed alcohol abuse, 0.4% developed alcohol dependence and 0.3% developed drug abuse or dependence, which was slightly lower than incidence rates of major depression (3.3%) and generalized anxiety disorder (1.6%). Men had higher incidence rates of alcohol abuse (2.3% vs 0.3%) and dependence (0.7% vs 0.2%) than women.15 Verges et al. (2012)16 also determined incidence of alcohol dependence in the NESRAC. Of adults aged 53+ with alcohol dependence at wave 1, data in figures suggested that about 35–45% still had alcohol dependence at the 3-year follow-up (persistence), and that approximately 2–6% aged 53+ with a prior-to-past-year alcohol dependence at wave 1 survey reported alcohol dependence at the 3-year follow-up (recurrence).
In summary, few older adults identified from the national survey of non-institutionalized populations develop new onsets of alcohol or drug use disorders. However, among older adults with an existing alcohol disorder, a high proportion appears to have persistent alcohol problems. Alcohol problems also relapse in later life. Hence, given the prevalent rate of active alcohol use in the middle-aged and older population,21 longitudinal research is needed to identify new cases of at-risk or binge alcohol use to better inform screening and prevention efforts.
Psychiatric comorbidity
There is a scarcity of data sources available that permit detailed analyses of psychiatric comorbidities with SUDs among older adults (Table 2). The NESARC appears to be the only data set with a comparatively large national sample and comprehensive assessments of psychiatric comorbidities. One of the NESARC studies reports incidence rates of comorbidities.15 In other survey studies, depression is often the single focus of the comorbid psychiatric condition. Data from clinical samples are included to provide additional information on comorbidities for treatment-seeking older substance abusers.
Table 2.
Peer-reviewed studies of comorbidities
| Authors | Year/ Country | Design | Data source | Sample/ Age in year | Substance | Selected findings |
|---|---|---|---|---|---|---|
| Lofwall et al.33 | 2005/USA | Cross-sectional | Year not available | n = 41; 50–66 years | Opioid-dependent patients |
|
| n = 26; 25-34 years | ||||||
| Merrick et al.29 | 2008/USA | Cross-sectional | 2003 MCBS | n = 12413; ≥65 years | Alcohol |
|
| Préville et al.28 | 2008/Canada | Cross-sectional | 2005–2006 ESA | n = 2798; ≥65 years | Benzodia-zepine | Among persons with past-year benzodiazepine dependence (n = 64), 31.3% had 1-year mood or anxiety disorders |
| Rosen et al.34 | 2008/USA | Cross-sectional | Year not available | n = 140; ≥50 years | Opioid-dependent patients | Past-year prevalence: major depression, 32.9%; generalized anxiety disorder, 29.7%; PTSD, 27.8%; mood or anxiety disorder, 47.1%, arthritis, 54.3%; hepatitis C, 49.3%; hypertension, 44.9%; heart condition, 17.9%; lung disease, 22.1%; cirrhosis, 14.3%; diabetes, 11.4% |
| Sacco et al.31 | 2009/USA | Cross-sectional | 2000–2001 NESARC | n = 4646; ≥60 years | Alcohol |
|
| Blazer & Wu20 | 2009/USA | Cross-sectional | 2005–2006 NSDUH | n = 10953; ≥50 years | Alcohol, Drugs | Major depression was associated with marijuana use and with cocaine use |
| Voyer et al.14 | 2009/Canada | Cross-sectional | 2005–2006 ESA | n = 2785; ≥65 years | Benzodia-zepine | Mild cognitive impairment, major depression, anxiety disorder and suicidal ideation were associated with increased odds of benzodiazepine dependence |
| Woo & Chen35 | 2010/USA | Cross-sectional | 2006–2007 | n = 90; ≥65 years | Drugs |
|
| Pietrzak et al.32 | 2011/USA | Cross-sectional | 2004–2005 NESARC | n = 9,463; ≥60 years | Drugs | PTSD was associated with lifetime mood, anxiety, drug use and borderline and narcissistic personality disorders |
| Choi & Dinitto30 | 2011/USA | Cross-sectional | 2005–2006 NSHAP | n = 2924; ≥57 years | Alcohol | The number of depressive symptoms was positively associated with binge/heavy alcohol use in men only |
| Chou et al.15 | 2011/USA | Longitu-dinal | 2000–2001 & 2004–2005 NESARC | n = 8012; ≥60 years | Alcohol, Drugs |
|
| Cicero et al.36 | 2012/USA | Cross-sectional | 2008–2010 | n = 2573; ≥18 years | Opioid-dependent patients | Opioid-dependent patients ages 45+ (n = 476) were more likely than younger opioid-dependent patients ages 18-44 years to have an anxiety/depressive disorder or alcohol dependence, and to report moderate-to-severe pain |
ESA, Enquête sur la Santé des Aînés or Quebec Survey on the Health of Seniors; MCBS, Access to Care file of the Medicare Current Beneficiary Survey; NESARC, National Epidemiologic Survey on Alcohol and Related Conditions; NSDUH, National Survey on Drug Use and Health; NSHAP, National Social Life, Health, and Aging Project; PTSD, post-traumatic stress disorder.
Comorbidity in surveys of the general population
Merrick et al. (2008)29 analysed data from the 2003 Access to Care file of the Medicare Current Beneficiary Survey, which included 12 413 continuously enrolled Medicare adults aged 65+. Overall, 9% of Medicare beneficiaries reported unhealthy drinking (>30 drinks/month, ≥4 drink/day) and depressive symptoms were positively associated with unhealthy drinking among drinkers. Depressive symptoms were the only mental health condition examined by the study. Choi and Dinitto (2011)30 analysed the data from the 2005–06 National Social Life, Health, and Ageing Project (NSHAP) to examine the association between depressive symptoms and binge/heavy drinking among 2924 adults aged 57+. Binge/heavy drinking (4+ drinks in men; 3+ drinks in women, per drinking day), as opposed to no drinking, was positively associated with depressive symptoms in older men, but not in older women. A lower level of drinking (<4 drinks in men; <3 drinks in women, per drinking day), as opposed to no drinking, was not associated with depressive symptoms in either gender.30 Using pooled samples from independent national surveys (NSDUH), Blazer and Wu (2009)20 found that past-year major depressive episode was associated with elevated odds of past-year marijuana use and of cocaine use among 10953 adults aged 50+. Similarly, major depressive episode was the only mental disorder assessed by the study. These results suggest that older adults who engage in binge/heavy alcohol use or illicit drug use have elevated odds of experiencing depressive symptoms.
Three studies used the NESARC data to explore psychiatric comorbidity among older adults. Sacco et al. (2009)31 analysed the subsample of 4646 current alcohol users aged 60+ in the 2000–01 NESARC. Based on the pattern of alcohol use (>7 drinks/week, heavy use) and alcohol abuse and dependence symptoms, three groups of alcohol users were identified: low-risk (89.2%), moderate-risk (9.7%) and high-risk (1.2%) groups. Compared with the low-risk and moderate-risk groups, the high-risk group had higher prevalences of major depression (24.9%, 3.2% and 3.2%, respectively), anxiety disorder (8.8%, 1.4% and 2.3%, respectively), and antisocial personality disorder (5.9%, 0.9% and 1.2%, respectively). On the other hand, Pietrzak et al. (2012)32 reported the extent of comorbidities by posttraumatic stress disorder status among 9463 adults aged 60+ in the wave 2 NESARC. About 10% of the sample reported a history of full (4.5%) or partial (5.5%) post-traumatic stress disorder. A high proportion of adults aged 60+ with a full (19.9%), partial (25.2%) or no (22.2%) post-traumatic stress disorder had a history of alcohol use disorders; a small proportion of adults aged 60+ with a full (4.3%), partial (3.5%) or no (1.7%) post-traumatic stress disorder had a history of drug use disorders. However, past-year data are not available to inform the extent of recent or active comorbidities.
Chou et al. (2011)15 analysed the longitudinal NESARC data to determine the incidence (new occurrences) of psychiatric disorders by SUD status. Among adults aged 60+ with an alcohol use disorder, about 4% and 2% developed a new major depressive disorder and a new generalized anxiety disorder, respectively, over a span of 3 years.15 Among adults aged 60+ with a drug use disorder, 6.7% developed a new major depressive disorder within 3 years, but the number of older adults with a drug use disorder was too small to generate reliable estimates for comorbid disorders.15
Taken together, psychiatric disorders, mainly major depression, appear to affect predominantly non-institutionalized older adults with a SUD (mainly alcohol use disorder), and a very small proportion of psychiatric disorders in late adulthood are new-onset cases. The available data suggest that a single survey of non-institutionalized adults may not generate a sufficiently large sample of older adults with a drug use disorder to produce reliable estimates for comorbidities.
Comorbidity in clinical samples
There are few studies of comorbidities among treatment-seeking older drug users. Lofwall et al. (2005)33 documented prevalent rates of lifetime psychiatric disorders among 41 methadone maintenance patients aged 50–66 years: major depression, 34.1%; alcohol use disorder, 75.6%; cocaine use disorder, 73.2%; opioid use disorder, 100%; cannabis use disorder, 41.5%; and sedative use disorder, 36.6%. Rosen et al. (2008)34 examined 140 methadone maintenance patients aged 50+ years and found a high rate (57%) of past-year mental and medical conditions (major depression, 32.9%; posttraumatic stress disorder, 27.8%; generalized anxiety disorder, 29.7%; arthritis, 54.3%; hypertension, 44.9%; hepatitis C, 49.3%; heart condition, 17.9%; lung disease, 22.1%; cirrhosis, 14.3%; diabetes, 11.4%). Rosen et al. (2008)34 also reported important sex and racial/ethnic differences in comorbidity. Women had higher prevalences than men of major depression (43.8% vs 27.2%), agoraphobia (20.8% vs 9.8%), and panic disorder (22.9% vs 12.0%), whereas men had higher prevalences than women of hypertension (52.2% vs 29.2%) and diabetes (16.3% vs 2.1%). Compared with African Americans, Whites showed higher prevalences of major depression (40.3% vs 26.0%), generalized anxiety disorder (37.3% vs 21.9%) and chronic lung disease (31.3% vs 13.7%), but lower prevalences than whites of hypertension (29.9% vs 57.5%) and diabetes (4.5% vs 17.8%). These data suggest that older drug users in methadone maintenance treatment are likely to have multiple SUDs and to be affected by additional psychiatric disorders and/or chronic medical illnesses.
Results from a study of 104 patients aged 65+ who accessed emergency care for psychiatric conditions in a hospital also suggest prevalent drug use among adults with a psychiatric diagnosis.35 The vast majority (93%) of the studied patients had a documented psychiatric diagnosis (psychosis, depression, substance use disorder), and more than one in four elderly patients (27%) showed positive urine toxicology on drug use at intake (i.e. barbiturate, benzodiazepine, cocaine, opiate, phencyclidine and amphetamine).35 A more recent study of treatment-seeking opioid-dependent adults further suggests that older drug abusers might be particularly affected by psychiatric and medical comorbidities. Cicero et al. (2012)36 found that treatment-seeking opioid-dependent patients aged 45+ (n = 476) had higher odds of having a comorbid disorder (anxiety, depressive, alcohol use disorders) and reporting moderate-to-severe pain than younger opioid-dependent patients aged 18–44 (n = 2097).
In summary, although findings from treatment-seeking adults are limited in their generalizability (a small sample size, selection bias), they demonstrate that older drug users in methadone maintenance treatment and older patients with a psychiatric condition constitute subsets severely affected by comorbid psychiatric or medical problems.
Discussion
Among community non-institutionalized adults aged 50+ years, around 60% used alcohol, 3% used illicit drugs (mainly marijuana) and 1–2% used nonmedical prescription drugs in the past year. Substance use and related disorders were comparatively prevalent among middle-aged adults, men and those who were separated/divorced/widowed or self-reported depression. Among adults aged 50+, approximately 5% of men vs 1.4% of women had an alcohol use disorder in the past year.22
Among alcohol users, about one in 14 (7.4%) users aged 50–64 had an alcohol use disorder in the past year compared with one in 30 (3.4%) older users aged 65+.22 Adults aged 50–64 were about four times (4%) more likely than elders aged 65+ (0.7%) to use marijuana in the past year; likewise, 4% of men and 1.4% of women aged 50+ used marijuana in the past year. Less than 1% of adults aged 50+ in the national survey had a drug use disorder in the past year; however, among drug users aged 50+, approximately 10–12% had a drug use disorder in the past year. Overall, alcohol is the primary abused substance in the mid and later life, and nonmedical prescription drug use (opioids, benzodiazepines) are emerging problems.37–39
Compared with other frequently reported psychiatric disorders (depression, anxiety disorders), SUDs can be considered among the most common psychiatric disorders affecting the older population. Although this review focuses on alcohol and drug use disorders, about 4% of older adults aged 65+ are estimated to have nicotine dependence in the past year.18,40 In NESARC, 5.6% of adults aged 45–64 and 2.7% of adults aged 65+ had a past-year major depressive disorder,41 and corresponding prevalences for generalized anxiety disorders were 2.1% and 1.0%, respectively.42 Additionally, among adults aged 55+, 1.2% had a past-year panic disorder,43 and 1.8% had past-year social anxiety disorder.44 Thus, SUDs may be more common than some specific anxiety disorders. However, SUDs affect more older men than older women, whereas mood and anxiety disorders are more common among older women than older men.45 Available studies, however, are too limited in their sample size to elucidate detailed sex differences in comorbid SUD with psychiatric disorders. Nonetheless, having one disorder increases the odds of having another disorder, suggesting a particularly high level of treatment needs among older adults.9,45 Therefore, all persons presenting substance use problems should be assessed for additional mental health conditions to inform treatment plans and management.
The few available studies suggest that older adults with a SUD are under-served. None of the older adults with a SUD in a Chilean survey used any SUD service in the past 6 months.19 In a study of methadone maintenance patients aged 55–68 years, who were characterized by exhibiting a history of substance abuse and numerous medical and psychiatric complaints, only 7% of the patients had regular contact with a primary care physician.46 The scarcity of research on understanding treatment need and service use reveals the need for research to better characterize substance use patterns to inform early use of preventive services and intervention. Age-related decline in health coupled with an increase in medication use indicate older adults’ elevated risk of developing adverse effects from substance misuse. Hence, early identification of at-risk older adults is needed to inform prevention, and use of SUDs for estimating treatment needs can miss a large size of problematic substance users. For instance, by focusing on the patterns of alcohol use, research reveals high prevalences of at-risk and binge drinking in a national sample of adults aged 50–64 (42% men, 22% women) and elders aged 65+ (28% men, 11% women).21 Collectively, there are increasing demands for SUD-related care as the size of the geriatric population continues to rise, and many of them also require mental health care (e.g. for depression). Substance abuse treatment data suggest that only a small proportion of older substance abusers were referred to treatment by general healthcare providers.47 Integrating routine substance use screening, brief intervention and referral to treatment into the mainstream primary care are needed to improve timely detection of substance use problems and early intervention, and to reduce escalation of addiction and use of costly health care.48,49
The constraint of survey data to generate an adequate number of older adults with a SUD to clarify comorbidities also suggests the utility of research on adults in addiction or mental health settings to help elucidate coexisting psychiatric conditions for different sex and racial/ethnic groups. The available data from clinical samples show that older drug users seeking treatment exhibit a pervasive pattern of psychiatric and medical comorbidities; however, the sample size precludes finer-grained analyses of comorbidity.33,34 Future research could consider use of multisite designs to improve the sample size and diversity of study participants’ demographic and clinical profiles. Longitudinal studies will be needed to understand incidences of new and recurrent episodes of SUDs and their temporal associations with comorbidities.50 The prevalent rate of subthreshold alcohol dependence (12%) in the national sample of both middle-aged and elderly alcohol users22 indicates the need to investigate subthreshold users’ likelihood and risk factors of developing a SUD. Similarly, middle-aged drug users warrant research to identify factors promoting continued use or escalating to a SUD. Suspected risk might include personal or family history of substance abuse, changes in life events (retirement, loss of family members or bereavements) and mental or medical conditions (depression, anxiety, pain related conditions).14,15,33,34,51,52 Substance use has been reported to cope with mental and medical conditions (e.g. pain), and older adults with mental/medical conditions are likely to receive and use prescribed psychoactive medications (opioids, benzodiazepines) that may further increase the chance of nonmedical use or addiction.14,51,53
Further, treatment encounters data from admissions to emergency departments (ED) of non-Federal hospitals (Drug Abuse Warning Network) and substance abuse treatment facilities that received public funding (TEDS) indicate an increased trend in drug-related admissions among older adults. Between 2004 and 2009, ED visits involving pharmacological use or misuse (e.g. opioid pain relievers) among adults aged 50+ increased by 159% (from 115 798 to 300 082 ED visits).39 TEDS data showed that admissions for primary drug misuse among adults aged 55+ increased by 106% for men and 119% for women between 1995 and 2002.54 Among elders aged 65+, admissions for primary opioid misuse increased from 6.6% in 1996 to 10.5% in 2005.55 Additionally, between 1998 and 2008, there were increases in the number of first-time admissions for primary misuse of marijuana, cocaine and heroin among adults aged 55+, whereas there were few changes in the younger group (ages 30–54).56 Recent TEDS findings further confirmed that substance abuse treatment admissions among adults aged 50+ increased from 6.6% in 1992 to 12.7% in 2009.57 Specifically, admissions for combined alcohol/drug misuse rose from 12.4% to 42.0%, whereas admissions for alcohol problems only decreased from 87.6% in 1992 to 58.0% in 2009. Thus, treatment encounter data point to an emerging trend in illicit/nonmedical drug use problems in the ageing population.
There are methodological challenges in studying substance use problems. Variations in definition of drinking problems complicate comparisons in findings across studies. Estimates from surveys of non-institutionalized populations may underestimate prevalences of substance use and SUDs due to bias associated with self-reports (underreporting, forgetfulness) and an exclusion of institutionalized (psychiatric patients, incarcerated adults) and homeless individuals from the survey sampling. Additionally, SUD estimates are influenced by survival bias, as substance users who died prematurely from substance-related consequences (accidents, HIV/AIDS, hepatitis, suicides) are not captured by surveys.7,58 This bias may be related to drug use (heroin/opioids, cocaine, amphetamines).7,59 All these factors may contribute to low rates of drug use estimates among older adults in surveys. As noted from treatment encounters data, multiple data sources are needed to better gauge substance use problems.
In conclusion, at-risk and binge alcohol use is common in mid and later life. Illicit and prescription drug misuse is an emerging drug problem. There have been increases in substance abuse treatment admissions among adults aged 50+. Substance use in late life requires ongoing surveillance as large numbers of baby boomers enter the geriatric population. There is a clear need to increase research efforts, including tracking substance use and SUDs in the growing racial/ethnic populations and developing effective substance abuse care models to address the wide range of their medical and mental health problems.
Funding
This work was supported by research grants from the U.S. National Institute on Drug Abuse of the National Institutes of Health (R21DA027503, R33DA027503, R01DA019623, and R01DA019901 to L-T.W.; HSN271200522071C to D.G.B.) and support from Duke University School of Medicine. The opinions expressed in this paper are solely those of the authors, not of any sponsoring agency. Both authors take responsibility for the content of the paper.
Conflict of interest: None declared.
KEY MESSAGES.
At-risk and binge drinking is common among adults aged 50 years or older.
Illicit and nonmedical drug use, especially prescription medications (opioids), is an emerging problem given that the 50–64 age cohort is carrying a much heavier burden of these problems than the 65+ cohort.
A limited number of longitudinal studies suggest new onset of substance use and mental disorders in later life.
Cross-sectional studies of treatment-seeking adults show that older drug users have multiple psychiatric and medical problems.
Additional research is needed to characterize patterns of substance use problems and comorbidities in racial/ethnic populations
References
- 1.US Census Bureau. 2012. International Data Base, 2009. http://www.census.gov/population/international/data/worldpop/tool_population.php (25 December 2012, date last accessed) [Google Scholar]
- 2.Kinsella K, He W. An Ageing World: 2008. Washington, DC: U.S. Government Printing Office; 2009. U.S. Census Bureau, International Population Reports, P95/09-1. [Google Scholar]
- 3.Degenhardt L, Dierker L, Chiu WT, et al. Evaluating the drug use ‘gateway’ theory using cross-national data: consistency and associations of the order of initiation of drug use among participants in the WHO World Mental Health Surveys. Drug Alcohol Depend. 2010;108:84–97. doi: 10.1016/j.drugalcdep.2009.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.US Census Bureau. Age and Sex Composition: 2010. Washington, DC: US Department of Commerce Economics and Statistics Administration; 2011. [Google Scholar]
- 5.Han B, Gfroerer JC, Colliver JD, Penne MA. Substance use disorder among older adults in the United States in 2020. Addiction. 2009;104:88–96. doi: 10.1111/j.1360-0443.2008.02411.x. [DOI] [PubMed] [Google Scholar]
- 6.Brick J, editor. Handbook of the Medical Consequences of Alcohol and Drug Abuse. New York: Haworth Press; 2004. [Google Scholar]
- 7.Wu LT, Woody GE, Yang C, Mannelli P, Blazer DG. Differences in onset and abuse/dependence episodes between prescription opioids and heroin: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Subst Abuse Rehabil. 2011;2:77–88. doi: 10.2147/SAR.S18969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Substance Abuse and Mental Health Services Administration. Results From the 2011 National Survey on Drug Use and Health: Summary of National Findings. NSDUH Series H-44, HHS Publication No. (SMA) 12-4713. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2012. [Google Scholar]
- 9.Wu LT, Blazer DG. Illicit and nonmedical drug use among older adults: a review. J Ageing Health. 2011;23:481–504. doi: 10.1177/0898264310386224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Substance Abuse and Mental Health Services Administration, Office of Applied Studies. Treatment Episode Data Set (TEDS), 1999-2009. DASIS Series: S-56, HHS Publication No. SMA 11-4646. Rockville, MD; Substance Abuse and Mental Health Services Administration, 2011. [Google Scholar]
- 11.Dowling GJ, Weiss SR, Condon TP. Drugs of abuse and the ageing brain. Neuropsychopharmacology. 2008;33:209–18. doi: 10.1038/sj.npp.1301412. [DOI] [PubMed] [Google Scholar]
- 12.Simoni-Wastila L, Yang HK. Psychoactive drug abuse in older adults. Am J Geriatr Pharmacother. 2006;4:380–94. doi: 10.1016/j.amjopharm.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 13.Ghitza UE, Wu LT, Tai B. Integrating substance abuse care with community diabetes care: implications for research and clinical practice. Subst Abuse Rehabil. 2013;4:3–10. doi: 10.2147/SAR.S39982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Voyer P, Preville M, Roussel ME, Berbiche D, Beland SG. Factors associated with benzodiazepine dependence among community-dwelling seniors. J Community Health Nurs. 2009;26:101–13. doi: 10.1080/07370010903034375. [DOI] [PubMed] [Google Scholar]
- 15.Chou KL, Mackenzie CS, Liang K, Sareen J. Three-year incidence and predictors of first-onset of DSM-IV mood, anxiety, and substance use disorders in older adults: results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2011;72:144–55. doi: 10.4088/JCP.09m05618gry. [DOI] [PubMed] [Google Scholar]
- 16.Vergés A, Jackson KM, Bucholz KK, et al. Deconstructing the age-prevalence curve of alcohol dependence: why ‘maturing out’ is only a small piece of the puzzle. J Abnorm Psychol. 2012;121:511–23. doi: 10.1037/a0026027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gum AM, King-Kallimanis B, Kohn R. Prevalence of mood, anxiety, and substance-abuse disorders for older Americans in the national comorbidity survey-replication. Am J Geriatr Psychiatry. 2009;17:769–81. doi: 10.1097/JGP.0b013e3181ad4f5a. [DOI] [PubMed] [Google Scholar]
- 18.Lin JC, Karno MP, Grella CE, et al. Alcohol, tobacco, and nonmedical drug use disorders in U.S. Adults aged 65 years and older: data from the 2001-2002 National Epidemiologic Survey of Alcohol and Related Conditions. Am J Geriatr Psychiatry. 2011;19:292–99. doi: 10.1097/JGP.0b013e3181e898b4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kohn R, Vicente B, Saldivia S, Rioseco P, Torres S. Psychiatric epidemiology of the elderly population in Chile. Am J Geriatr Psychiatry. 2008;16:1020–28. doi: 10.1097/JGP.0b013e31818a0e1c. [DOI] [PubMed] [Google Scholar]
- 20.Blazer DG, Wu LT. The epidemiology of substance use and disorders among middle aged and elderly community adults: national survey on drug use and health. Am J Geriatr Psychiatry. 2009;17:237–45. doi: 10.1097/JGP.0b013e318190b8ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blazer DG, Wu LT. The epidemiology of at-risk and binge drinking among middle-aged and elderly community adults: National Survey on Drug Use and Health. Am J Psychiatry. 2009;166:1162–99. doi: 10.1176/appi.ajp.2009.09010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blazer DG, Wu LT. The epidemiology of alcohol use disorders and subthreshold dependence in a middle-aged and elderly community sample. Am J Geriatr Psychiatry. 2011;19:685–94. doi: 10.1097/JGP.0b013e3182006a96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hasin DS. Combining abuse and dependence in DSM-5. J Stud Alcohol Drugs. 2012;73:702–04. doi: 10.15288/jsad.2012.73.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huang B, Dawson DA, Stinson FS, et al. Prevalence, correlates, and comorbidity of nonmedical prescription drug use and drug use disorders in the United States: Results of the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006;67:1062–73. doi: 10.4088/jcp.v67n0708. [DOI] [PubMed] [Google Scholar]
- 25.Moore AA, Karno MP, Grella CE, et al. Alcohol, tobacco, and nonmedical drug use in older U.S. Adults: data from the 2001/02 national epidemiologic survey of alcohol and related conditions. J Am Geriatr Soc. 2009;57:2275–81. doi: 10.1111/j.1532-5415.2009.02554.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blazer DG, Wu LT. Nonprescription use of pain relievers by middle-aged and elderly community-living adults: National Survey on Drug Use and Health. J Am Geriatr Soc. 2009;57:1252–57. doi: 10.1111/j.1532-5415.2009.02306.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Substance Abuse and Mental Health Services Administration, Office of Applied Studies. The DASIS Report: Older Adults in Substance Abuse Treatment: 2005. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2007. [Google Scholar]
- 28.Préville M, Boyer R, Grenier S, et al. Scientific Committee of the ESA Study. The epidemiology of psychiatric disorders in Quebec's older adult population. Can J Psychiatry. 2008;53:822–32. doi: 10.1177/070674370805301208. [DOI] [PubMed] [Google Scholar]
- 29.Merrick EL, Horgan CM, Hodgkin D, et al. Unhealthy drinking patterns in older adults: prevalence and associated characteristics. J Am Geriatr Soc. 2008;56:214–23. doi: 10.1111/j.1532-5415.2007.01539.x. [DOI] [PubMed] [Google Scholar]
- 30.Choi NG, Dinitto DM. Heavy/binge drinking and depressive symptoms in older adults: gender differences. Int J Geriatr Psychiatry. 2011;26:860–68. doi: 10.1002/gps.2616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sacco P, Bucholz KK, Spitznagel EL. Alcohol use among older adults in the National Epidemiologic Survey on Alcohol and Related Conditions: a latent class analysis. J Stud Alcohol Drugs. 2009;70:829–38. doi: 10.15288/jsad.2009.70.829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Psychiatric comorbidity of full and partial posttraumatic stress disorder among older adults in the United States: results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Am J Geriatr Psychiatry. 2012;20:380–90. doi: 10.1097/JGP.0b013e31820d92e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lofwall MR, Brooner RK, Bigelow GE, Kindbom K, Strain EC. Characteristics of older opioid maintenance patients. J Subst Abuse Treat. 2005;28:265–72. doi: 10.1016/j.jsat.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 34.Rosen D, Smith ML, Reynolds CF., III The prevalence of mental and physical health disorders among older methadone patients. Am J Geriatr Psychiatry. 2008;16:488–97. doi: 10.1097/JGP.0b013e31816ff35a. [DOI] [PubMed] [Google Scholar]
- 35.Woo BK, Chen W. Substance misuse among older patients in psychiatric emergency service. Gen Hosp Psychiatry. 2010;32:99–101. doi: 10.1016/j.genhosppsych.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 36.Cicero TJ, Surratt HL, Kurtz S, Ellis MS, Inciardi JA. Patterns of prescription opioid abuse and comorbidity in an ageing treatment population. J Subst Abuse Treat. 2012;42:87–94. doi: 10.1016/j.jsat.2011.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Substance Abuse and Mental Health Services Administration, Office of Applied Studies. Emergency Department Visits Involving Nonmedical Use of Selected Pharmaceuticals. Rockville, MD: Office of Applied Studies, Substance Abuse and Mental Health Services Administration; 2009. [Google Scholar]
- 38.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. The TEDS Report: Substance Abuse Treatment Admissions for Abuse of Benzodiazepines. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2011. [Google Scholar]
- 39.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. The DAWN Report: Drug-Related Emergency Department Visits Involving Pharmaceutical Misuse or Abuse by Older Adults: 2009. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. [Google Scholar]
- 40.Blazer DG, Wu LT. Patterns of tobacco use and tobacco-related psychiatric morbidity and substance use among middle-aged and older adults in the United States. Ageing Ment Health. 2012;16:296–304. doi: 10.1080/13607863.2011.615739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62:1097–106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 42.Grant BF, Hasin DS, Stinson FS, et al. Prevalence, correlates, co-morbidity, and comparative disability of DSM-IV generalized anxiety disorder in the USA: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2005;35:1747–59. doi: 10.1017/S0033291705006069. [DOI] [PubMed] [Google Scholar]
- 43.Chou KL. Panic disorder in older adults: evidence from the national epidemiologic survey on alcohol and related conditions. Int J Geriatr Psychiatry. 2010;25:822–32. doi: 10.1002/gps.2424. [DOI] [PubMed] [Google Scholar]
- 44.Chou KL. Social anxiety disorder in older adults: evidence from the National Epidemiologic Survey on alcohol and related conditions. J Affect Disord. 2009;119:76–83. doi: 10.1016/j.jad.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 45.Byers AL, Yaffe K, Covinsky KE, Friedman MB, Bruce ML. High occurrence of mood and anxiety disorders among older adults: The National Comorbidity Survey Replication. Arch Gen Psychiatry. 2010;67:489–96. doi: 10.1001/archgenpsychiatry.2010.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rajaratnam R, Sivesind D, Todman M, Roane D, Seewald R. The ageing methadone maintenance patient: treatment adjustment, long-term success, and quality of life. J Opioid Manag. 2009;5:27–37. doi: 10.5055/jom.2009.0004. [DOI] [PubMed] [Google Scholar]
- 47.Arndt S, Gunter TD, Acion L. Older admissions to substance abuse treatment in 2001. Am J Geriatr Psychiatry. 2005;13:385–92. doi: 10.1176/appi.ajgp.13.5.385. [DOI] [PubMed] [Google Scholar]
- 48.Pilowsky DJ, Wu LT. Screening for alcohol and drug use disorders among adults in primary care: a review. Subst Abuse Rehabil. 2012;3:25–34. doi: 10.2147/SAR.S30057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tai B, Wu LT, Clark HW. Electronic health records: essential tools in integrating substance abuse treatment with primary care. Subst Abuse Rehabil. 2012;3:1–8. doi: 10.2147/SAR.S22575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Moos RH, Schutte KK, Brennan PL, Moos BS. Late-life and life history predictors of older adults' high-risk alcohol consumption and drinking problems. Drug Alcohol Depend. 2010;108:13–20. doi: 10.1016/j.drugalcdep.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brennan PL, Schutte KK, Moos RH. Pain and use of alcohol to manage pain: prevalence and 3-year outcomes among older problem and non-problem drinkers. Addiction. 2005;100:777–86. doi: 10.1111/j.1360-0443.2005.01074.x. [DOI] [PubMed] [Google Scholar]
- 52.Kuerbis A, Sacco P. The impact of retirement on the drinking patterns of older adults: a review. Addict Behav. 2012;37:587–95. doi: 10.1016/j.addbeh.2012.01.022. [DOI] [PubMed] [Google Scholar]
- 53.Aira M, Hartikainen S, Sulkava R. Drinking alcohol for medicinal purposes by people aged over 75: a community-based interview study. Fam Pract. 2008;25:445–49. doi: 10.1093/fampra/cmn065. [DOI] [PubMed] [Google Scholar]
- 54.Substance Abuse and Mental Health Services Administration, Office of Applied Studies. Older Adults in Substance Abuse Treatment: Update. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2005. [Google Scholar]
- 55.Substance Abuse and Mental Health Services Administration, Office of Applied Studies. The DASIS Report: Adults Aged 65 or Older in Substance Abuse Treatment: 2005. Rockville, MD: Office of Applied Studies, Substance Abuse and Mental Health Services; 2007. [Google Scholar]
- 56.Arndt S, Clayton R, Schultz SK. Trends in substance abuse treatment 1998-2008: increasing older adult first-time admissions for illicit drugs. Am J Geriatr Psychiatry. 2011;19:704–11. doi: 10.1097/JGP.0b013e31820d942b. [DOI] [PubMed] [Google Scholar]
- 57.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. The TEDS Report: Older Adult Admissions Reporting Alcohol as a Substance of Abuse: 1992 and 2009. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2011. [Google Scholar]
- 58.Centers for Disease Control and Prevention (CDC) CDC grand rounds: prescription drug overdoses – a U.S. epidemic. MMWR Morb Mortal Wkly Rep. 2012;61:10–13. [PubMed] [Google Scholar]
- 59.United Nations Office on Drugs and Crime. World Drug Report 2012. Sales No. E.12.XI.1. Vienna: United Nations Office on Drugs and Crime, 2012. [Google Scholar]