Abstract
Background: Since the introduction of specified diagnostic criteria for mental disorders in the 1970s, there has been a rapid expansion in the number of large-scale mental health surveys providing population estimates of the combined prevalence of common mental disorders (most commonly involving mood, anxiety and substance use disorders). In this study we undertake a systematic review and meta-analysis of this literature.
Methods: We applied an optimized search strategy across the Medline, PsycINFO, EMBASE and PubMed databases, supplemented by hand searching to identify relevant surveys. We identified 174 surveys across 63 countries providing period prevalence estimates (155 surveys) and lifetime prevalence estimates (85 surveys). Random effects meta-analysis was undertaken on logit-transformed prevalence rates to calculate pooled prevalence estimates, stratified according to methodological and substantive groupings.
Results: Pooling across all studies, approximately 1 in 5 respondents (17.6%, 95% confidence interval:16.3–18.9%) were identified as meeting criteria for a common mental disorder during the 12-months preceding assessment; 29.2% (25.9–32.6%) of respondents were identified as having experienced a common mental disorder at some time during their lifetimes. A consistent gender effect in the prevalence of common mental disorder was evident; women having higher rates of mood (7.3%:4.0%) and anxiety (8.7%:4.3%) disorders during the previous 12 months and men having higher rates of substance use disorders (2.0%:7.5%), with a similar pattern for lifetime prevalence. There was also evidence of consistent regional variation in the prevalence of common mental disorder. Countries within North and South East Asia in particular displayed consistently lower one-year and lifetime prevalence estimates than other regions. One-year prevalence rates were also low among Sub-Saharan-Africa, whereas English speaking counties returned the highest lifetime prevalence estimates.
Conclusions: Despite a substantial degree of inter-survey heterogeneity in the meta-analysis, the findings confirm that common mental disorders are highly prevalent globally, affecting people across all regions of the world. This research provides an important resource for modelling population needs based on global regional estimates of mental disorder. The reasons for regional variation in mental disorder require further investigation.
Keywords: Common mental disorders, mood disorders, anxiety disorders, substance use disorders, systematic review, meta-analysis
Key Messages.
Results from a review of 174 surveys across 26 high income countries and 37 low and middle income counties identified substantial inter-survey heterogeneity in the prevalence of common mental disorder.
Findings pooled across all studies indicate that on average one in five adults (17.6%) experienced a common mental disorder within the past 12 months and 29.2% across their lifetime.
Across both high income and low and middle income countries, females were more likely to experience a mood or anxiety disorder, and males were more likely to experience an alcohol or other substance use disorder.
Countries of North and South East Asia in particular returned lower prevalence estimates than other regions of the world.
Understanding the sources of variability in the global prevalence of common mental disorder remains a substantial ongoing challenge for the field of psychiatric epidemiology.
Introduction
The introduction of operationalized diagnostic criteria for mental disorders in the late 1970s1,2 and their subsequent incorporation into the DSM nomenclature3 represented a seminal development for the field of psychiatric epidemiology. Mental health researchers were able to undertake multi-diagnostic assessments to provide estimates of discrete mental disorders as well as the combined prevalence of mental disorders across clinical domains such as mood, anxiety, substance use disorders or for common mental disorder more broadly.4,5 Over the 34-year period since the publication of DSM-III,3 a large body of psychiatric epidemiological research has accumulated with studies undertaken across multiple countries.
The first of this modern wave of international psychiatric epidemiological work applied two-step methodologies, commencing with population screening followed by clinical assessments of probable cases and non-cases, primarily using the Present State Exam (PSE) CATEGO system, the firstly widely adopted approach to assessing the population prevalence of common mental disorder.6 Developments in the field since then have largely proceeded in parallel with the design and conduct of sequential national mental health surveys undertaken in the USA. Of pivotal importance was the Epidemiologic Catchment Area (ECA) study undertaken in the early 1980s in the immediate aftermath of the release of DSM-III, which assessed 16 mental disorders across five US catchment sites, including persons from institutional settings.7 Although aspects of this study have been criticized,8–10 the ECA demonstrated the feasibility of applying lay-administered diagnostic interviews in a single-step survey, a method replicated in other countries.11–16 The National Comorbidity Survey9 undertaken during the early 1990s introduced a number of innovations: it utilized the WHO Composite International Diagnostic Interview (CIDI);17 limited the range of disorders assessed to the broad clinical domains of mood, anxiety and substance use disorders; introduced nationally representative multi-stage probabilistic sampling frames; and initiated the WHO International Consortium of Psychiatric Epidemiology (ICPE) with similar surveys applying the CIDI18 undertaken in other settings.19,20 More recently the National Comorbidity Survey-Replication Study21,22 established the prototype for the World Mental Health Survey Initiative23,24 (WMHS) which has coordinated mental health surveys across 28 countries. TheWMHS has introduced further rigour into the procedure by: implementing standard procedures and concurrent multi-country clinical reappraisal studies to validate diagnoses; including disorder-specific severity indicators; adding a standardized set of measures of risk and protective factors; and including a range of externalizing disorders that had not been assessed in previous surveys.25
The recent approach to psychiatric epidemiological research has been to provide prevalence estimates of discrete and combined aggregations of mental disorders. The earlier generation of studies, most notably those involving the PSE CATEGO generation of studies and the ECA studies using the Diagnostic Interview Schedule, attempted to combine high and low prevalence disorders including the psychotic disorders. Subsequent studies recognized the inherent difficulties of applying a single methodology to both groupings,8 instead limiting the use of household surveys to a focus on the high-prevalence mental disorders, hereafter referred to as common mental disorders.
An important advance in the field of psychiatric epidemiology, a process given impetus by the 2010 global burden of disease project (GBD), has been the application of quantitative approaches designed to integrate findings across multiple independent psychiatric epidemiological studies. The current revision of the GBD resulted in a series of comprehensive systematic reviews and meta-analyses, each analysing the prevalence of anxiety disorders26 and major depressive disorder,27 the former including 87 studies from 44 countries and the latter 116 studies from 53 countries. These developments build on previous narrative reviews4,5,28–30 of psychiatric epidemiology as well as some regional quantitative reviews most notably within Europe.31–33 A key component of psychiatric epidemiology over this period has been the practice of reporting the combined prevalence of common mental disorder, for the most part, combined across the domains of mood, anxiety and substance use disorders. Although there will inevitably be differences in the sets of discrete mental disorders used to estimate common mental disorder prevalence, the high level of comorbidity between mental disorders,34,35 evidence that common latent constructs underlie most discrete mental disorders,34–37 and a growing evidence base for the effectiveness of transdiagnostic interventions38 support the potential value of applying meta-analytic procedures to integrate the findings emerging from this body of epidemiological investigation.
With the exception of reviews undertaken by Wittchen and colleagues for studies undertaken in Europe,31,32 there has been no dedicated review of the body of psychiatric epidemiological research that reports the combined prevalence of common mental disorders. The present study aims to address this critical gap in the field by undertaking the first comprehensive review and meta-analysis of psychiatric epidemiological population surveys published over the period 1980–2013. We focus on the set of psychiatric epidemiological studies that have applied structured diagnostic measures to provide an estimate of common mental disorder prevalence among adult populations and where available, the prevalence of the constituent domains of mood, anxiety and substance use disorders. The review will examine studies reporting point and period as well as lifetime prevalence estimates. This expands on the approach adopted by the global burden of disease studies which focused only on point or period prevalence.
Methods
We followed the guidelines for conducting and reporting meta-analyses of observational studies in epidemiology (MOOSE)39 and the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA).40 The review was additionally informed by the findings of Brugha and colleagues’41 review of the methodology and reporting of meta-analyses of observational studies in psychiatric epidemiology.
Study inclusion criteria
Included were studies published between 1980 and 2013 (inclusive) that applied census or probabilistic epidemiological procedures to obtain a national or regional general population sample. The review was limited to studies reporting on samples in which the majority of respondents (>50%) were between 16 and 65 years of age. The decision to include only surveys undertaken with a general adult population reflects a recognition of the specialist nature of child-adolescent and older age populations, and the need for separate targeted reviews of common mental disorders among these age groups,42,43 an approach supported by most previous reviews.4,5,28–30,33 The current review was further limited to those studies with a sample size of 450 or more. This ensures that included surveys had sufficient statistical power to provide stable estimates of the general population, a criterion consistent with a number of previous reviews.44,45 We accepted gender-specific samples and age-cohort studies, where the age of the cohort at the time of the survey was within the 16–65 year age range. For inclusion, studies had to:
report current (1-week, 1-month), period (6- or 12-months) or lifetime estimates of common mental disorder prevalence;
apply a structured psychiatric diagnostic interview either to a whole population or as part of a two-step survey methodology;
- identify one or more of the relevant common mental disorders as defined under international diagnostic criteria (DSM-III, DSM-III-R, DSM-IV, ICD-8, ICD-9, ICD-10) where there were at least two of:
- major depressive disorder including major depressive episode or an aggregate of mood disorders (including bipolar disorder);
- the aggregate of at least two common anxiety disorders (generalized anxiety disorder, panic disorder-agoraphobia, social phobia, obsessive compulsive disorder, posttraumatic stress disorder, acute stress disorder, anxiety disorder not otherwise specified);
- alcohol use disorders (harmful use/dependence) or alcohol and other substance-use disorders (cannabis, sedative-hypnotic, stimulant-amphetamine, opioid; harmful use/dependence);
In cases where prospective data were reported, point or period prevalence estimates were taken for the first report after 1980 and lifetime prevalence estimates were taken from the most recent reported estimate. We did not include regional prevalence estimates such as those reported in the European Study of the Epidemiology of Mental Disorders (ESEMeD),48 but rather extracted individual country-level estimates. We excluded studies that only sampled targeted groups (e.g. racial or ethnic sub-groups, military or patient populations), that applied convenience or linkage sampling techniques or that included a majority of respondents under 16 years of age or older than 65 years of age.
Search strategy
We implemented an empirical approach to conducting an optimized search strategy for identifying psychiatric epidemiological papers of common mental disorder.49 In the first step we identified 152 references deemed to be critical papers of interest for this field of research that included milestone papers and key review articles. This set of papers was used to generate and iteratively improve search strategies in order to maximize their sensitivity and specificity for identifying relevant articles across four separate databases: MEDLINE, PsycINFO, EMBASE and PubMed. All search strategies achieved sensitivity ranging between 85% (EMBASE) and 90% (MEDLINE) against the initial set of articles. The search strategy was developed in MEDLINE, and iterative changes were made to enable optimal searching in the other databases, for example using the textword (.tw) search field in EMBASE instead of the multi-purpose (.mp) field as described below. We drew on existing optimized search strategies to identify mental health content in the general medical abstracting databases.50 Common mental disorders were searched for using a combination of exp mental disorders AND mental disorders/ep or anxiety disorders/ep or depressive disorders/ep or prevalence.mp. To identify studies reporting the results of epidemiological studies we commenced with broad search terms such as ‘epidemiology’ but were unable to obtain adequate sensitivity and specificity estimates. We identified a two-pronged search strategy combined with this initial search to increase the specificity of searches without losing sensitivity. This was achieved by using one of two search strings to narrow the above search outcomes:
specific searches for the diagnostic instruments included in the study: (‘schedule for affective disorders and schizophrenia’ or ‘Composite International Diagnostic Interview*’ or ‘CIDI’ or ‘Diagnostic Interview Schedule*’ or ‘Clinical Interview Schedule’ or ‘MINI’ or ‘Bradford Somatic Inventory’ or ‘pse’ or ‘Present State Examination’ or ‘Schedule for Clinical Assessment in Neuropsychiatry*’ or ‘SCAN’ or ‘self-reporting questionnaire’ or ‘Social Problem Index’ or ‘WMH’ or ‘cross-national’).mp.; or,
a search for ‘DSM’, which was found to be a common index term for many papers not identified in the first search strategy: (‘diagnostic and statistical manual of mental disorders’ or ‘DSM’).mp. was also included to provide a more sensitive but much less specific index.
The initial search of the four databases was undertaken 3 February 2011 and then updated for publications on 2 March 2013 and 2 January 2014. The full search strings are provided in eTable 5 (available as Supplementary data at IJE online).
All article abstracts obtained in the searches were screened by one of the authors (C.M. or Z.S. or J.J.) in an initial process to remove those ineligible for inclusion. The researchers achieved 100% concordance in determining eligible studies using a sample of 800 papers prior to commencement of screening the full sample. Articles that remained as possible candidates for inclusion in the study were then obtained in full-text form and again assessed by the same researchers for inclusion. Non-English language articles identified from the systematic review were included in the review, where possible, with targeted translation of key sections to enable accurate data extraction. We also included technical reports or monographs that provided unique data.
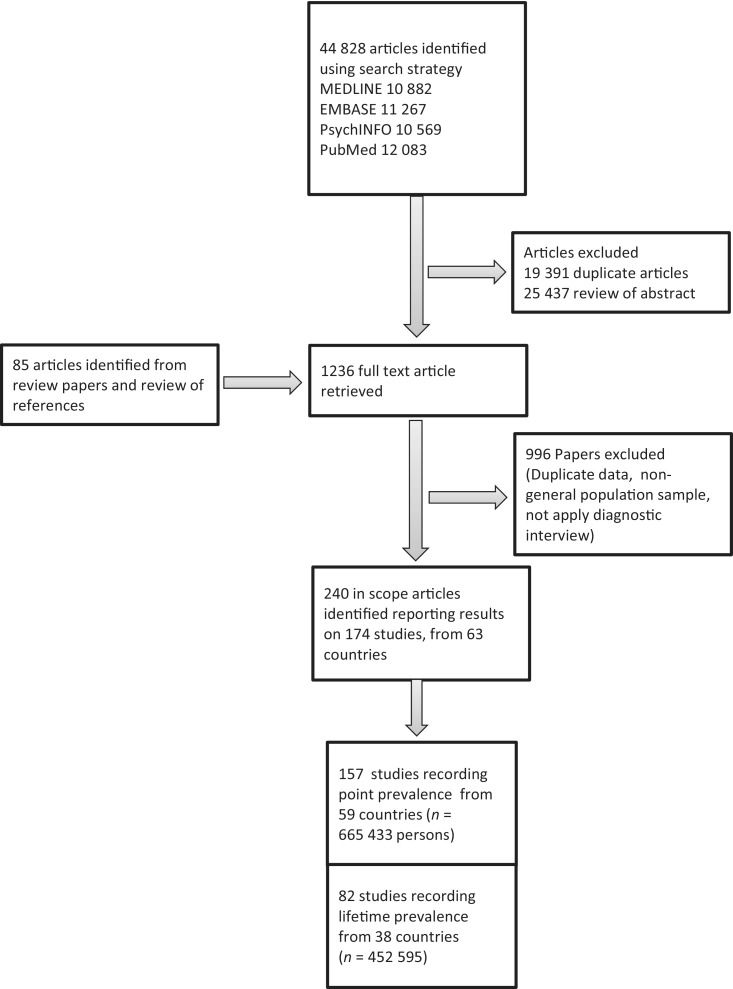
Figure 1 shows the number of articles obtained from the various databases using the search strategy. A total of 25 437 non-duplicate articles were obtained from the search strategy. This search strategy was supplemented by review of existing literature reviews and the reference lists of relevant papers. After a review of abstracts, 1236 full-text article were retrieved for more detailed investigation. Full-text review identified 240 in-scope articles reporting epidemiological data on the prevalence of common mental disorder from 174 studies; eTable 6 (available as Supplementary data at IJE online) provides details of the included surveys; and eTable 7 (available as Supplementary data at IJE online) provides bibliographical references for all articles.
Figure 1.
Flowchart of systematic review procedure for identifying population surveys reporting the aggregate prevalence of mental disorder.
We further examined the sensitivity of the search terms against the final set of articles use to extract data for the current review. Of the 240 papers used, 212 were indexed in EMBASE, 206 in PubMed, 195 in MEDLINE and 181 in PsycINFO. Of the indexed articles, the search terms identified 74% of articles in EMBASE, 80.5% in PubMed, 87% in MEDLINE and 87% in PsycINFO, with the remainder of studies identified through review of reference lists of included papers and key review articles in the field.4,5,19,26–33,51–53
Case ascertainment
For each survey, data were extracted for the aggregated prevalence of common mental disorder as well as the clinical sub-domains of mood, anxiety and substance use disorders where provided by authors. The estimates for the combined prevalence of common mental disorder for each study were based on those reported within each of the reviewed articles. In cases where multiple estimates of common mental disorder were provided by the authors involving different combinations of mental disorder, we extracted the estimate that did not include specific phobia, tobacco dependence (which was not included in any of the estimates extracted), personality disorder, adjustment disorder or neurological disorders such as epilepsy (only relevant to a number of mental health surveys undertaken during the 1970s and early 1980s). The decision to preference estimates of common mental disorder omitting these disorders is based on the low rate of inclusion of these disorders in the majority of surveys reviewed, and also the possible impact of some of the disorders, such as tobacco dependence and specific phobia, which have a high population prevalence that may affect overall prevalence estimates.
In extracting prevalence estimates for the clinical domains of mood disorders and substance use disorders, we preferentially extracted an estimate that included a combination of all mood disorders assessed within a study or all substance use disorders assessed within a study. In studies that did not provide a combined prevalence estimate across multiple mood or multiple substance use disorders, and consistent with the inclusion criteria, we used the prevalence of major depressive disorder as a proxy measure for mood disorders and the prevalence of alcohol abuse and/or alcohol dependence as a proxy measure of substance use disorders. This reflects that these disorders account for the majority of cases within the respective clinic domains. With respect to clinical estimates of the prevalence of anxiety disorders, a study had to report the combined prevalence of at least two anxiety disorders in order for an estimate to be extracted from the survey.
We followed the WHO burden of disease group by integrating point and period prevalence estimates.27 In the current analysis we have given primacy to 12-month period prevalence over point prevalence when more than one index was provided. Twelve-month period prevalence has emerged as the most commonly reported time period over recent years32 and arguably provides an estimate across a more meaningful clinical period than 1-week or 1-month point prevalence. Where point and period prevalence estimates were available, both were extracted from papers, but 12-month period prevalence estimates were used in data analysis. We also extracted data on the type and number of individual mental disorders assessed that formed each of the combined estimates of common mental disorders, mood disorders, anxiety disorders and substance use disorders. Where possible, prevalence rates were extracted separately for males and females as well as for the combined prevalence across genders. In cases where only odds ratios were available to indicate the magnitude of gender differences we applied a variation of the formula to generate odds ratios in order to recover cell marginal probabilities and prevalence estimates.54
Other data extraction
Additional information extracted included: the sample size; the recruitment design, response rate; the diagnostic time frame; the diagnostic instrument used; the year(s) of data collection; the age range of respondents; the diagnostic nomenclature applied (DSM-III, DSM-III-R, DSM-IV, ICD-10); and the country of the survey. We also identified whether studies were undertaken using the methodologies associated with each of the major generation of studies, namely: the early CATEGO and PSE studies primarily undertaken during the late 1970s and early 1980s; the ECA generation of studies applying the Diagnostic Interview Schedule; the ICPE set of studies based on the Composite International Diagnostic Interview (CIDI 1.0 and 2.0); or the WHO WMHS group of studies. Another clear set of studies have followed on from the PSE in the use of the Clinical Interview Schedule-Revised (CIS-R) and the Schedule for Clinical Assessment in Neuropsychiatry (SCAN) represented by the 1992, 2000 and 2007 UK surveys46,55,56 but also undertaken across multiple other settings. Surveys not following the methodologies developed as part of these broad approaches or generations of surveys were listed as ‘other’. Countries were grouped into World Bank income groupings. Low and Middle Income Countries (LMIC) were further classified according to the broad World Bank regional groupings.57 For High Income Countries an additional classification was applied that distinguished English language HICs from HICs in Europe, and HICs in Asia, groupings that covered the majority of HIC countries identified in the current review.
Data analysis
Meta-analytic techniques for the analysis of observational studies39 enables the quantitative integration of data across multiple studies in order to derive pooled prevalence estimates stratified across key variables such as differing diagnostic nomenclature, year range of data ascertainment, the number of disorders assessed and the geographical region of the population survey. Data analysis was carried out in SAS (SAS V9.3; 2002–2010 by SAS Institute, Cary, NC, USA) and STATA software (version 12, STATA Corporation, College Station, TX, USA) using user defined metan, metafunnel and metabias procedures. The prevalence rate of disorders was converted from percentage to logit. The Delta method was applied to compute within-study variance, variance, namely, var(logit) = 1/case + 1/non_case,58 with all pooled meta-analysis estimates weighted for the statistical precision (sample size) of the included prevalence estimates.
Meta-analysis was carried out using the metan procedure in STATA. Analyses for the prevalence of common mental disorder were stratified by study characteristics including the mid-year of data ascertainment, the diagnostic nomenclature used, the generation of psychiatric epidemiology that informed the survey methodology, the recruitment design (two-step or one-step survey), the number of mental disorders assessed and World Bank income and regional groupings. Meta-analytic models were also calculated for prevalence rates extracted for males and females and for mood, anxiety and substance use disorders. Only a single prevalence estimate for each study was included within each meta-analytic model.
The random effect regression logits and 95% CIs were back transformed and expressed as absolute prevalence estimates (not relative to the reference group) and presented in tables with forest plots. Prevalence logits were bivariate normal for the combined prevalence of mental disorders and for clinical domains of mood, anxiety and substance use disorders. We refer to the random effects estimate as the pooled prevalence estimate representing the weighted average of the prevalence estimates within the meta-analysis.59 Pooled prevalence estimates have only been reported for variable strata with four or more surveys. The level of statistical heterogeneity is reported using the I2 statistic [(Q statistic—d.f. /Q statistic) x 100%] as a measure of the percentage of variability in the pooled prevalence estimate due to inter-study heterogeneity (τ2).60 Funnel plots of the prevalence logit, plotted against the standard error, were assessed for asymmetry to assess for evidence of publication bias. Begg's rank correlation test and Egger's asymmetry test were also conducted to provide a formal assessment of publication bias across studies.61,62 We applied sensitivity analyses to examine the effect of the removal of studies identified as points of undue influence (defined as +/− 2 standard deviations in logit prevalence rates; constituting 4.4% of data points) on the pooled estimates provided from all meta-analytic models. The complete results of the sensitivity analyses are provided within the online supplementary material (available as Supplementary data at IJE online).
Results
Figure 1 presents the results of the systematic review. In all, 174 studies met inclusion criteria, providing prevalence data for common mental disorders for a total sample of 829 673 persons from 63 countries, including 106 surveys within 26 HIC settings and 68 surveys within 37 LMIC settings. In addition, 114 surveys provide data on the aggregated prevalence of common mental disorders among females (n = 513 341) and 110 among males (509 456). In the majority of surveys (79%), the estimate of common mental disorder extracted included a combination of disorders across the mood, anxiety and substance use disorder spectrum, with a limited number of surveys not assessing, or not including, substance use disorders in the final estimate of common mental disorder (n = 37, 21%).
In addition to estimates of the prevalence of common mental disorder, 166 surveys also provided estimates for the prevalence of mood disorders (n = 855 562), 134 surveys for the combined prevalence of anxiety disorders (n = 723 097), and 120 surveys estimates on the prevalence of substance use disorders (n = 742 916).
Across the 34-year study period reviewed, there was an increase in the number of studies undertaken on an annual basis, with the majority of studies (60%) undertaken over the period 1995 to 2009. This increase has also reflected a steady increase in the diversity of countries, increasing from 22 countries during the 1980s and 34 countries in the 1990s to 37 countries in the 2000s, with LMIC representation increasing from 6 during the 1980s to 19 countries during the 2000s.
The median sample size across all studies was 2314 (IQR = 1040–5035) with an average median increase in sample size of 543 (261–923, 95% CI quantile regression) across each time period listed in Tables 1 and 2.The response rate was reported for 129 surveys with a median of 77.1% (IQR 70.6–87.5%), a minimum of 45.9% and a maximum of 99.5%. There was no evidence of change in response rates across time.
Table 1.
Random effects meta-analysis pooled 12-month period prevalence estimates and forest plots for common mental disorders stratified by methodological and substantive variables
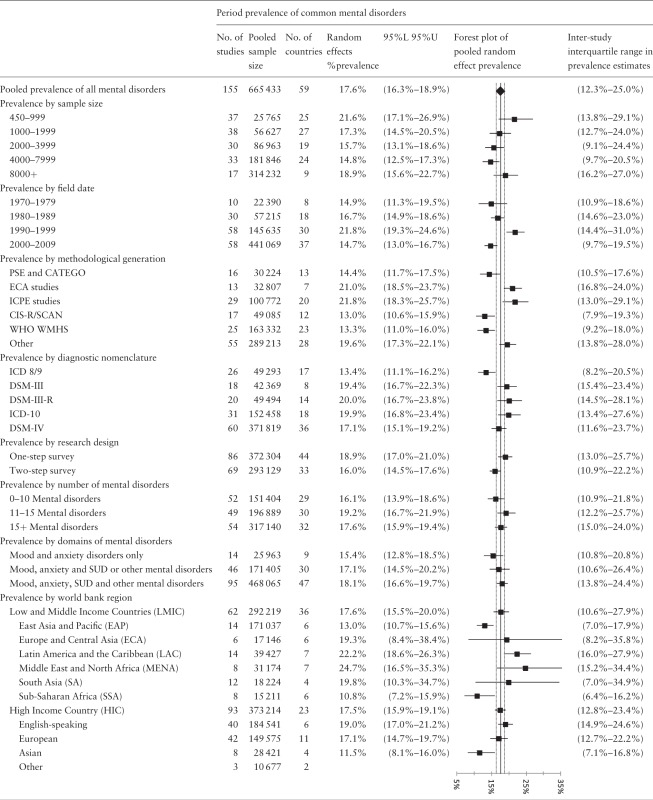 |
95%L = 95% confidence interval lower range estimate; 95%U = 95% confidence interval upper range estimate.
NB: Pooled prevalence estimates have only been reported for strata in which there are 4 or more studies providing prevalence data.
Table 2.
Random effects meta-analysis pooled lifetime prevalence estimates and forest plots for common mental disorders stratified by methodological and substantive variables
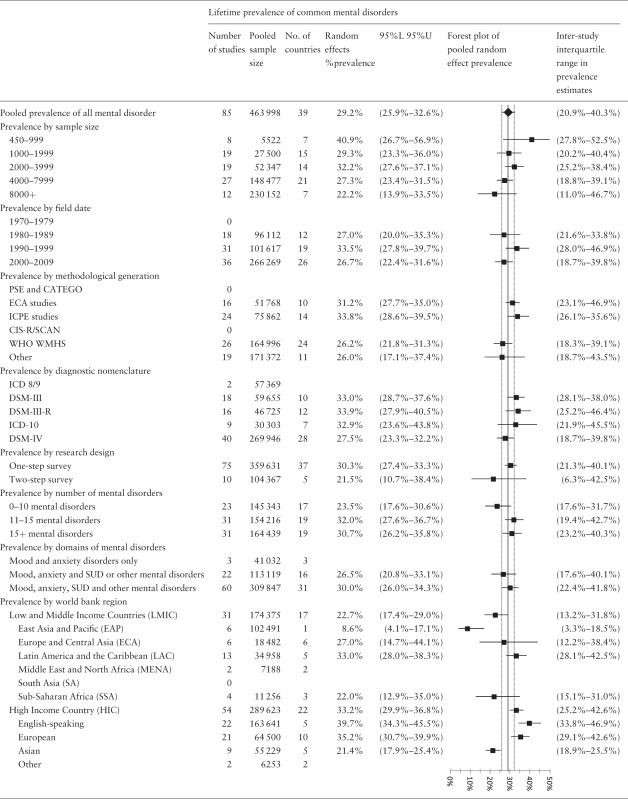 |
95%L = 95% confidence interval lower range estimate; 95%U = 95% confidence interval upper range estimate.
NB: Pooled prevalence estimates have only been reported for strata in which there are 4 or more studies providing prevalence data.
Global prevalence of common mental disorder
Tables 1 and 2 present the random effects prevalence estimates for period and lifetime mental disorders, respectively. Period prevalence of common mental disorder was available from 155 surveys with a pooled prevalence estimate of 17.6% (95% CI, 16.3–18.9%) across 59 countries. The pooled lifetime prevalence of common mental disorders across 85 surveys was 29.2% (95% CI, 25.9–32.6%). There was a trend for surveys utilizing smaller sample sizes (>1000) to return higher period and lifetime prevalence estimates of common mental disorder than those recruiting larger samples; however, overlapping confidence intervals preclude clear interpretation of this finding.
Surveys undertaken during the 1990s returned a higher pooled prevalence estimate than surveys undertaken during the other decades reviewed, particularly considering period prevalence. These results were slightly attenuated following sensitivity analysis (see eTable 1 and eTable2, available as Supplementary data at IJE online) which removed points of undue influence (+/−2 standard deviations in logit prevalence rates), but the pooled period prevalence for the 1990s remained higher than the surveys within the 2000s. The groupings of studies into the five broad generations of psychiatric epidemiological approaches co-varied with study field date (chi square = 160.2, df = 20, P < .0001). The majority of PSE CATEGO studies were carried out within the 1970s and 1980s; ECA studies during the 1980s; ICPE during the 1990s; CIS-R/SCAN studies during the 1990s and 2000s; and WMHS studies during the 2000s; with the uncategorized studies spread evenly across all time periods. The pooled period prevalence estimates for the ECA and ICPE studies were higher than those recorded by the earlier generation of PSE CATEGO studies as well as the more recent CIS-R/SCAN and WMHS sets of studies. Again this was attenuated following sensitivity analysis, with a number of ICPE-influenced studies identified with extreme values removed.
There was a trend for studies using two-step methodologies, applying screening instruments followed by detailed clinical case ascertainment, to return lower prevalence rates than single-step surveys that applied diagnostic interviewing to a whole sample with both period and lifetime prevalence rates. The expectation that there would be a linear increase in prevalence of common mental disorder with the greater number of mental disorders assessed in the survey was not born out. It is important to note that there was an interaction between the number of mental disorders assessed and the method applied. For example the average number of diagnoses assessed by surveys using a single-step model was 12.9 compared with 16.4 for two-step surveys (F = 9.64, df 1172, P = 0.002) which may account for this pattern.
Examination of prevalence estimates by regional groupings identified some key differences. In regard to the income level of the country, there was no difference in the pooled period prevalence of common mental disorders across the 92 surveys undertaken in HIC and the 62 surveys in LMIC settings. For lifetime prevalence, the 54 surveys undertaken in HIC countries returned a pooled prevalence estimate of 32.2% (29.9–36.8%) compared with 22.7%(17.4–29.0%) across the 31 surveys undertaken in LMICs. After sensitivity analysis excluded surveys with potential undue influence, the LMIC pooled lifetime prevalence estimate (25.0%; 21.0–29.5%) shifted closer to that recorded in HIC settings but remained lower as indicated by non-overlapping confidence intervals (see eTable 2, available as Supplementary data at IJE online).
Surveys undertaken in the East Asia and Pacific LMIC region displayed lower period and lifetime common mental disorder prevalence than other regions. A similar pattern was also evident for HIC countries, with countries primarily within North and South East Asia returning lower pooled prevalence estimates than other regions. With regard to period prevalence, countries within sub-Saharan Africa were identified with lower pooled prevalence estimates but this emerged only as a trend when considering lifetime prevalence estimates, most likely due to the low number of surveys included. With regard to lifetime prevalence, HIC English-speaking countries returned the highest lifetime prevalence estimates. Removal of potential points of undue influence attenuated the pattern but there still emerged evidence of lower rates in East Asia and Pacific LMIC and for North and South East Asian HIC settings as well as lifetime estimates for HIC English-speaking countries.
There was substantial inter-survey heterogeneity across period (Q = 29096, df = 154, I2 = 99.5%) and lifetime prevalence estimates (Q = 45119, df = 84, I2 = 99.8%), a pattern that was also evident across all of the strata collated in Table 1 (I2 = range 90.2–99.8%). The magnitude of variability is clear when considering the range of common mental disorder recorded, from 3.1% in Tanzania using the CIS-R63 to 77.7% in a rural region of Udmurt Republic on the basis of CIDI 2.1 assessments.64,65 After removing surveys +/−2 standard deviation units, the range was still substantial (4.7–46.1%, see eTable 3 available as Supplementary data at IJE online). Lifetime prevalence was recorded for 85 surveys with a pooled estimate of 29.1% (25.9–32.5%) across 39 countries ranging from 2.9%52,66 to 81.8%64,65 (8.2–61.4% after sensitivity analysis).
Figure e1.1a and e1.2b (available as Supplementary data at IJE online) present funnel plots for period and lifetime prevalence logits by the logit standard error. The Begg’s adjusted rank correlation test61 for funnel plot asymmetry (period z = −1.51, P = 0.13; lifetime z = −1.02, P = 0.31) was not significant. Evidence of a linear association between prevalence and standard error was indicated by Eggar’s weighted regression67 (period t = −2.77, P = 0.006; lifetime t = −2.17, P = 0.033) with the regression line displayed on the funnel plots. These findings remained after sensitivity analysis in which points of undue influence were removed (see efigure 1.2a and 2.2b, available as Supplementary data at IJE online) indicating a general tendency for studies reporting lower prevalence estimates to have larger standard errors.
Global prevalence of common mental disorder by clinical sub-domain and gender
Table 3 presents data from surveys that provided disaggregated prevalence estimates for males and females and for the broad clinical domains of mood, anxiety and substance use disorders. The pooled period prevalence of mood disorder across 148 surveys was 5.4% (4.9–6.0%) with a pooled lifetime prevalence of 9.6% (8.5–10.7%) across 83 surveys. For anxiety disorders, the pooled period prevalence was 6.7% (6.0–7.6%) from 122 surveys with a lifetime prevalence of 12.9% (11.3–14.7%) from 70 surveys. Substance use disorders showed a pooled period prevalence of 3.8% (3.4–4.3%) from 104 surveys and a lifetime prevalence estimated at 3.4% which shifts to 10.7% (9.2–12.4%) from 74 surveys once points of undue influence have been removed (see eTable 3, available as Supplementary data at IJE online).
Table 3.
Random effects meta-analysis pooled prevalence estimates and forest plots for mental disorders, mood, anxiety and substance use disorder by gender
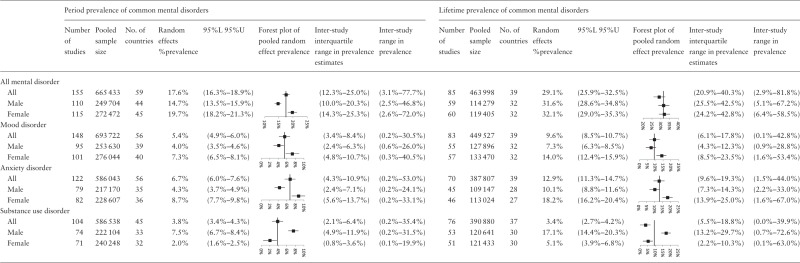 |
95%L = 95% confidence interval lower range estimate; 95%U = 95% confidence interval upper range estimate.
Females had a higher aggregated period prevalence estimate of common mental disorder (19.8%; 18.3–21.3%) than males (15.2%, 14.1–16.3%), but that finding was not replicated in the pooled lifetime prevalence estimates of common mental disorder (females 32.1%, 29.0–35.3%; males 31.6%, 28.6–34.8%). A consistent pattern of results however emerged for gender when examining the three clinical sub-domains. Women had higher period and lifetime prevalence rates for mood (period 7.3%, 6.5–8.1%; lifetime 14.0%, 12.4–15.9%) and anxiety disorders (period 8.7%, 7.6–9.8%; lifetime 18.2%, 16.2–20.4%) compared with men (mood period, 4.0%, 3.5–4.6%; mood lifetime 7.3%, 6.3–8.5%; anxiety period 4.3%, 3.7–4.9%; anxiety lifetime 10.1%, 8.8–11.6%). In contrast, men had higher pooled prevalence rates for substance disorders (period 7.5%, 6.7–8.4%; lifetime 17.1%, 14.4–20.3%) compared with women (period 2.0%, 1.6–2.5%; lifetime 5.0%, 3.9–8%). Results of additional meta-analyses stratified by broad World Bank country income classifications indicated that HIC and LMIC displayed the same pattern of gender differences, with women having higher pooled prevalence rates for mood and anxiety disorders and men higher prevalence rates for substance use disorders (see online Table e4, available as Supplementary data at IJE online).
Discussion
The past three decades have witnessed a burgeoning in the field of psychiatric epidemiology, with the current review identifying 174 population surveys providing aggregated estimates for the prevalence of common mental disorder across a combined population of 829 673 respondents with surveys undertaken in 63 countries including 106 surveys in 26 HIC and 68 surveys in 37 LMIC.
Before considering the key findings of the meta-analysis, it is important to note the following limitations. The meta-analysis identified substantial inter-survey heterogeneity across all random effect models reported. Period and lifetime prevalence estimates of common mental disorder displayed substantial variability even after removal of points of undue influence (period prevalence, 4.7–46.1%; lifetime prevalence 8.2–61.4%). Comparable levels of heterogeneity have been identified in other recent reviews of psychiatric epidemiological findings.26,27,41,53,68 The presence of heterogeneity can adversely affect the stability and interpretability of the pooled prevalence estimates derived. In the current study, although I2 was above 90% in all models, it is important to note that the statistic is particularly sensitive to study precision and the total number of studies included, factors that are generally present in psychiatric epidemiological reviews. As a consequence, several authorities have raised questions about the merit of reporting such heterogeneity indices in meta-analytic studies of observational studies where the number of studies and sample sizes tend to be large.69,70 Notwithstanding this, a key issue is whether the level of heterogeneity observed precludes the possibility of deriving meaningful pooled summary statistics. In the current analysis, the sub-group analysis, while identifying sources of variability, also returned pooled prevalence estimates for common mental disorder that fell within a relatively narrow range of 5–10 percentage points across the categories of the variables examined in Tables 1 and 2. Thus whereas there was substantial variability at the individual study level, there was much less variability at the pooled prevalence estimate level. This is also in part reflected by consideration of the interquartile ranges in the current study, which ranged from 12.3% to 24.3% for period prevalence and 27.6% to 33.2% for lifetime prevalence, indicating that the majority of studies had estimates close to the pooled results reported. It should be noted that the interquartile range estimates of common mental disorder derived from the current review of 174 studies is of a similar range to that recorded by the World Mental Health Survey Initiative (12-month 9.8–19.1%; lifetime 18.1–36.1%) where common survey and research design approaches were used.71 As an additional measure to assess the stability of the estimates provided, we undertook sensitivity analysis of the key results by removing potential points of undue influence associated with study heterogeneity, which with the exception of one or two analyses had little effect on the results reported. Collectively these considerations, in concert with the consistency of the findings reported, provide support for the interpretability of the estimates provided.
In order to derive an aggregate estimate of period prevalence we integrated estimates of point, 1-week, 6-month and 12-month period prevalence26,27 but gave primacy to 12-month prevalence estimates where available. 12-month prevalence estimates are widely reported within the field of psychiatric epidemiology, and is the standard period prevalence estimate reported within key publications associated with the ICPE and WMHS generation of studies. It could be argued that shorter periods may provide a more valid measure by avoiding possible recall bias with evidence that more conservative estimates of 12-month and lifetime prevalence are produced through cross-sectional as opposed to prospective research designs.72,73 As with previous research,26 we did not find a substantial difference between point and period prevalence in sub-group analysis and hence have retained a focus on 12 month prevalence.
An important limitation that has not been able to be addressed from the current study is that the prevalence rates extracted from studies are derived from samples with potentially differing underlying population age structures particularly between HIC and LMIC, a factor that may introduce variation in common mental disorder prevalence.26,74,75 Studies were only selected for inclusion if they provided a combined estimate of common mental disorder across at least two of the major domains of mood, anxiety or substance use disorders with 79% of studies based on a combination of all three. Notwithstanding this, studies displayed a wide range of mental disorders assessed, with 75% of surveys including additional mental disorders in the estimate of common mental disorder. There was no evidence of a linear association between the number of mental disorders and the prevalence rate recorded, suggesting that high levels of comorbidity among mental disorders51,74 may constrain any increase in the overall prevalence estimates obtained by including larger numbers of diagnostic categories. That inference is supported by the finding that two-step survey designs, which on average assessed five more mental disorders than single-step approaches, did not yield higher aggregated prevalence estimates of common mental disorder. There was also evidence of moderate bias, with inspection of the funnel plots and Eggar’s weighted regression indicating that prevalence estimates co-varied with the standard error of point estimates, with lower prevalence estimates returned by studies with higher standard errors. This effect was primarily attributable to the inclusion of studies with sample sizes under 1000, which returned higher prevalence estimates of common mental disorder than surveys with larger sample sizes, a finding that has been noted in previous psychiatric epidemiological reviews.53
A key challenge and potential source of bias relates to the implementation of appropriate search strategies to identify relevant studies. This use of untested and ineffective search strategies has been identified as a major threat to valid systematic reviews and meta-analysis, that is not adequately addressed in many studies.41,76 In addressing this potential bias we adopted an iterative empirical approach to the development and refinement of search terms in order to identify relevant articles, with the search strategy achieving an initial 85–90% sensitivity across the four abstracting databases used.49 Re-examination of the search terms against the final set of studies meeting fully inclusion criteria demonstrated that the search strategy retained a high sensitivity (74–87%) across the four abstracting databases, providing strong support for the iterative search strategies developed.49 The search strategy was supplemented with a review of reference lists of included studies and previous reviews. Despite these procedures it is possible that relevant surveys were omitted from the current review. In particular we did not undertake individual country reviews to identify government or other unpublished reports that may not have been indexed or cited in the studies reviewed.
We have not assessed the extent to which the surveys undertaken, particularly within LMIC settings, were adapted to cultural context and environment. A large body of research has documented the importance of transcultural variations in idioms of mental health distress across contexts. A number of recent studies provide evidence to indicate that the uncritical use of standard psychiatric diagnostic instruments in some cultural settings may lead to either under-or over-enumeration of mental disorders.77,78 This is an ongoing challenge that faces the field of psychiatric epidemiology. There remains substantial concern about the meaning equivalence of assessments across different cultural contexts.79–81 Finally, the current review does not include surveys undertaken primarily with children and adolescents or older adults. As such, the results should be interpreted as only being relevant to the general adult population.
The current review provides the largest contemporary review of the field of psychiatric epidemiology of common mental disorders. To be included, all surveys had to meet criteria for methodological rigor including the use of census or representative sampling frames, the identification of mental disorder using structured or semi-structured diagnostic interviews and a minimum sample size of 450 to ensure stability of the estimates provided. A particular strength of the current review was the capacity to examine meta-analytic results in parallel across studies reporting period and lifetime prevalence rates. Even though there was overlap, the two final datasets were distinctive so that the parallel analyses provide a form of cross-validation of the findings reported.
The key results of the analysis are that common mental disorders, often showing comorbid patterns, are highly prevalent, affecting substantial sections of all the populations surveyed. Close to one in five respondents (17.6%;16.3–18.9%) met criteria for a common mental disorder during the previous 12 months and 29.2% (25.9–32.6%) met lifetime prevalence. Anxiety disorders had the highest 12-month prevalence rates, affecting 1 in 15 persons annually (6.7%; 6.1–7.9%), with mood disorders affecting 1 in 20 persons (5.4%;4.9–6.0%) and substance use disorders approximately 1 in 25 persons (3.8%; 3.3–4.2%). Lifetime estimates were 12.9% (11.3–14.7%) for anxiety disorders, 9.6% (8.5–10.7%) for mood disorders and 10.7% (9.2–12.5%) for substance use disorders after removing points of undue influence.
Our findings concur broadly with the estimates of depression and anxiety disorder prevalence produced by the Global Burden of Disease 2010 review. Baxter and colleagues,26 applying a similar definition of two or more anxiety disorders, calculated a meta-regression adjusted global estimate of anxiety disorder of 7.6% (4.8–10%) from 87 surveys, which is remarkably similar to the estimate of 7.1% provided herein based on 113 surveys. Within the mood disorder spectrum, Ferrari and colleagues27 undertook a more targeted systematic review and meta-regression analysis of 116 surveys, reporting an adjusted estimate of 4.7% (4.4–5.0%) for the prevalence of major depressive disorder across 53 countries, a rate similar to the 5% estimated by Paykel and colleagues33 based on the body of psychiatric epidemiological research in Western Europe. Another major source of global information on the prevalence of mood disorder comes from the results of the 2002–03 WHO World Health Survey.82,83 In addition to other physical disorders, the World Health Survey assessed the prevalence of major depressive disorder using the lay-administered WMHS CIDI in a survey population of 187 496 respondents using nationally representative sampling across 53 participating countries. Results for major depressive disorder aggregated according to World Bank country income groupings ranged from 7.1% in high income countries to 6.0% in low income countries. Taken together, the results of other published reviews appear to converge with the findings for the anxiety and mood disorders recorded here.
At the level of common mental disorder, the 17.6% recorded herein for common mental disorder appears to represent a more conservative prevalence estimate than those derived by Wittchen and colleagues31,32 in relation to psychiatric epidemiological research within Europe. Their initial 2005 review reported 12-month prevalence of common mental disorder among adult populations from 27 epidemiological studies reporting. This was updated to include more recent epidemiological data in 2011. In both the original and the updated reviews, the authors examined the prevalence of 13 mental disorders to identify a combined 12-month prevalence of 27%. The discrepancy may reflect a number of factors. The review methodology applied by Wittchen et al. involved the use of median prevalence estimates across existing studies for each mental disorder, in combination with expert panels, in contrast to the meta-analytic method applied in the current review. The findings were also adjusted for older population age structures in Europe. In addition, the estimate provided by Wittchen and colleagues included specific phobia (6.4%) and somatoform disorders (4.9%), both of which were identified as highly prevalent.
One of the strongest findings from the current meta-analysis was a robust gender effect across the clinical sub-domains of mental disorder that was evident for both period and lifetime prevalence estimates. Females had higher prevalence rates of mood (7.3:4.0%) and anxiety disorders (8.7:4.3%) with males returning higher prevalence estimates of substance use disorders (2.0:7.5%). Examination of gender effects stratified by HIC and LMIC settings confirmed the global consistency of the findings. Moreover the gender ratios identified also consistent with global burden of disease reviews26,27 and the World Health Survey depression study,84 as well as earlier reviews that have focused on common mental disorders31,32,84 and individually on anxiety disorders,28 depression30,33,83 and substance use disorders.29
The meta-analysis identified substantive regional differences in the prevalence of common mental disorder. LMIC countries in East Asia and the Pacific grouping and within HIC Asia were found to have significantly lower period and lifetime prevalence estimates than the pooled average. The tendency for epidemiological surveys to identify low prevalence rates of common mental disorder within North and South East Asia has been noted in a number of previous studies.77,78,85 An increasing body of evidence is growing to support these observations. The recent burden of disease reviews for anxiety disorders and for major depressive disorder both identified comparatively lower rates of disorder within the North and South East Asia region.26,27 Similarly the results of the WHO World Health Survey depression study83 identified the lowest prevalence estimates for major depression in Vietnam, China, Malaysia, Laos and the Philippines. The convergence of findings between the current review and the results of the World Health Survey is of particular note as the data sources are independent. Investigation of the source of the lower prevalence estimates in this key region must now be seen as a matter of priority within the field. We have previously demonstrated that the use of the CIDI in Vietnam was associated with an under-enumeration of mental disorders in comparison with a culturally adapted case-finding instrument.78 Also results from the metropolitan China site of the WMHS suggest that under-enumeration may have occurred as a result of the predominance of affective, as opposed to somatic symptom screening items in the psychiatric instruments based on the DSM-IV diagnostic criteria.77,86 Nevertheless, the possibility that the lower population risk for common mental disorder in parts of Asia may be associated with key cultural or other protective factors cannot be discounted.
Other regional differences emerged primarily in relation to 12-month period prevalence rates, including reduced rates of common mental disorder among LMIC countries of sub-Saharan Africa. The stability of these results remains in question, with sensitivity analysis reducing the magnitude of the differences observed. Nevertheless, similar findings were identified for sub-Saharan Africa in the global burden of disease reviews.26,27 With regard to lifetime prevalence, English-speaking HIC countries were found to record a higher prevalence, at 39.7%, than other HIC and LMIC settings. The possibility that this may be attributable to age differences between surveys cannot be dismissed, with English speaking samples possibly including persons of greater age who had passed through a longer period of risk, particularly in comparison with surveys undertaken within LMIC.
The results of the current review do not provide a clear picture about the nature of changes in the prevalence of common mental disorder across time despite some evidence that prevalence rates varied as a function of the decade in which the surveys were undertaken. In particular, surveys undertaken during the 1990s returned higher pooled prevalence estimates than those undertaken during the 2000s and also during the 1970s. The result may in part reflect different approaches to psychiatric epidemiology during these eras, with both ECA and ICPE surveys returning higher estimates of common mental disorder.20,24 In terms of diagnostic nomenclature, the early generation of surveys applying ICD-8 and ICD-9 appeared to return the lowest estimates, but not substantially different from rates returned using DSM-IV, whereas DSM-III, DSM-III-R and ICD-10 all had a trend to return higher prevalence estimates.
At an international policy level, the results of the current review provide independent support for the findings of the global burden of disease study87,88 that mental and behavioural disorders represent a major contributor to health burden globally.51 The results provide the first comprehensive estimates of the combined prevalence of common mental disorders that may be of particular use for planning services and policy responses compared with estimates derived from multiple discrete mental disorders.51,89 The high prevalence of common mental disorders across HIC and LMIC settings, combined with evidence that the common mental disorders have a life-onset that is earlier than other comparable chronic conditions,71 highlights the importance of mental and behavioural disorders as a contributor to population health burden.51 Whereas there are contested views regarding the most appropriate response to the management of common mental disorders,90,91 substantial evidence indicates the majority of people with mental disorder do not receive specialized services and that global resources allocated to the management of mental disorders is substantially lower than for other chronic health conditions.92–94
Conclusion
Results of the systematic review and meta-analysis indicated that approximately one in five persons experienced a common mental disorder within a 12-month period across 155 general population surveys undertaken in 59 countries. The aggregate lifetime prevalence of common mental disorder was estimated at 29.2% from 85 surveys undertaken across 39 countries. Despite substantial inter-survey heterogeneity, results identified a robust gender effect with women experiencing higher prevalence rates of mood and anxiety disorders and men displaying a higher rate of substance use disorders across HIC and LMIC settings. There was evidence of regional variation in the prevalence of common mental disorder, with countries of North and South East Asia in particular returning lower prevalence estimates than countries in other regional groupings.
Supplementary Data
Supplementary data are available at IJE online.
Funding
This study has been supported by NHMRC Program Grant No. 568970. V.P. is supported by Wellcome Trust Senior Research Fellowship in Clinical Science.
Supplementary Material
Acknowledgments
The research team would like to thank the support of Mrs Gordana Sobacic who provided administrative support in the management of the data for this analysis and manuscript.
Conflict of interest: ZS; TC; DS. were authors on one of the studies included in the review (see e-reference 191, available as Supplementary data at IJE online). Data extraction for that study was undertaken by an independent author (C.I.). V.P. was an invited editor for the special series on mental health for IJE but was not involved in the review or editorial decision making for the current paper. There was no other conflict of interest related to this work. The lead author has checked references for accuracy and completeness and confirms that this material has not been published previously in a substantially similar form.
References
- 1.Spitzer RL, Endicott J, Robins E. Research diagnostic criteria: rationale and reliabitity. Arch Gen Psychiatry 1978;35:773–82 [DOI] [PubMed] [Google Scholar]
- 2.Wing JK, Cooper JE, Sartorious N. The Measurement and Classiflcation of Psychiatric Symptoms. London: Cambridge University Press, 1974 [Google Scholar]
- 3.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd edn Washington, DC: American Psychiatric Association Press, 1980 [Google Scholar]
- 4.Dohrenwend B, Dohrenwend BS. Perspectives on the past and future of psychiatric epidemiology: The 1981 Rema Lapouse lecture. Am J Public Health 1982;72:1271–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dohrenwend BP. A psychosocial perspective on the past and future of psychiatric epidemiology. Am J Epidemiol 1998;147:222–31 [DOI] [PubMed] [Google Scholar]
- 6.Wing IK, Cooper JE, Sartorious N. The Description and Classification of Psychitrric Symptoms: an Instruction Manual for the PSE and Catego System. London: Cambridge University Press, 1974 [Google Scholar]
- 7.Bourdon KH, Rae DS, Locke BZ, Narrow WE, Regier DA. Estimating the prevalence of mental disorders in U.S. adults from the Epidemiologic Catchment Area Survey. Public Health Rep 1992;107:663–68 [PMC free article] [PubMed] [Google Scholar]
- 8.Regier DA, Kaelber CT, Rae DS, et al. Limitations of diagnostic criteria and assessment instruments for mental disorders: Implications for research and policy. Arch Gen Psychiatry 1998;55:109–15 [DOI] [PubMed] [Google Scholar]
- 9.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: Results from the National Comorbidity Survey. Arch Gen Psychiatry 1994;51:8–19 [DOI] [PubMed] [Google Scholar]
- 10.Parker G. Are the lifetime prevalence estimates in the ECA study accurate? Psychol Med 1987;17:275–82 [DOI] [PubMed] [Google Scholar]
- 11.Bland RC, Newman SC, Orn H. Period prevalence of psychiatric disorders in Edmonton. Acta Psychiatr Scand Suppl 1988;338:33–42 [DOI] [PubMed] [Google Scholar]
- 12.Bland RC, Orn H, Newman SC. Lifetime prevalence of psychiatric disorders in Edmonton. Acta Psychiatr Scand Suppl 1988;338:24–32 [DOI] [PubMed] [Google Scholar]
- 13.Oakley-Browne MA, Joyce PR, Wells JE, Bushnell JA, Hornblow AR. Christchurch Psychiatric Epidemiology Study, Part II: Six month and other period prevalences of specific psychiatric disorders. Aust N Z J Psychiatry 1989;23:327–40 [DOI] [PubMed] [Google Scholar]
- 14.Wells JE, Bushnell JA, Hornblow AR, Joyce PR, Oakley-Browne MA. Christchurch Psychiatric Epidemiology Study, Part I: Methodology and lifetime prevalence for specific psychiatric disorders. Aust N Z J Psychiatry 1989;23:315–26 [DOI] [PubMed] [Google Scholar]
- 15.Canino GJ, Bird HR, Shrout PE, et al. The prevalence of specific psychiatric disorders in Puerto Rico. Arch Gen Psychiatry 1987;44:727–35 [DOI] [PubMed] [Google Scholar]
- 16.Hwu HG, Yeh EK, Chang LY. Prevalence of psychiatric disorders in Taiwan defined by the Chinese Diagnostic Interview Schedule. Acta Psychiatr Scand 1989;79:136–47 [DOI] [PubMed] [Google Scholar]
- 17.Robins LN, Wing J, Wittchen HU, Helzer JE. The Composite International Diagnostic Interview: an epidemiologic instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch Gen Psychiatry 1988;45:1069–77 [DOI] [PubMed] [Google Scholar]
- 18.Andrews G, Henderson S, Hall W. Prevalence, comorbidity, disability and service utilisation: Overview of the Australian National Mental Health Survey. Br J Psychiatry 2001;178:145–53 [DOI] [PubMed] [Google Scholar]
- 19.Weissman MM, Bland R, Canino G, et al. Cross-national epidemiology of major depression and bipolar disorder. JAMA 1996;276:293–99 [PubMed] [Google Scholar]
- 20.WHO International Consortium in Psychiatric Epidemiology. Cross-national comparisons of the prevalences and correlates of mental disorders. Bull World Health Organ 2000;78:413–26 [PMC free article] [PubMed] [Google Scholar]
- 21.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE, Merikangas KR. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005;62:617–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005;62:93–602 [DOI] [PubMed] [Google Scholar]
- 23.Demyttenaere K, Bruffaerts R, Posada-Villa J, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA 2004;291:2581–90 [DOI] [PubMed] [Google Scholar]
- 24.Kessler RC, Angermeyer M, Anthony JC, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization's World Mental Health Survey Initiative. World Psychiatry 2007;6:168–76 [PMC free article] [PubMed] [Google Scholar]
- 25.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int JMethods Psychiatr Res 2004;13:93–121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baxter AJ, Scott KM, Vos T, Whiteford HA. Global prevalence of anxiety disorders: A systematic review and meta-regression. Psychol Med 2013;43:897–910 [DOI] [PubMed] [Google Scholar]
- 27.Ferrari AJ, Somerville AJ, Baxter AJ, et al. Global variation in the prevalence and incidence of major depressive disorder: A systematic review of the epidemiological literature. Psychol Med 2013;43:471–81 [DOI] [PubMed] [Google Scholar]
- 28.Somers JM, Goldner EM, Waraich P, Hsu L. Prevalence and incidence of anxiety disorders: a systematic review of the literature. Can J Psychiatry 2006;51:100–13 [DOI] [PubMed] [Google Scholar]
- 29.Somers JM, Goldner EM, Waraich P, Hsu L. Prevalence studies of substance-related disorders: a systematic review of the literature. Can J Psychiatry 2004;49:373–84 [DOI] [PubMed] [Google Scholar]
- 30.Waraich P, Goldner EM, Somers JM, Hsu L. Prevalence and incidence studies of mood disorders: a systematic review of the literature. Can J Psychiatry 2004;49:124–38 [DOI] [PubMed] [Google Scholar]
- 31.Wittchen HU, Jacobi F. Size and burden of mental disorders in Europe – a critical review and appraisal of 27 studies. Eur Neuropsychopharmacology 2005; 15:357-76 [DOI] [PubMed] [Google Scholar]
- 32.Wittchen HU, Jacobi F, Rehm J, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. European Neuropsychopharmacol 2011;21:655–79 [DOI] [PubMed] [Google Scholar]
- 33.Paykel ES, Brugha T, Fryers T. Size and burden of depressive disorders in Europe. Eur Neuropsychopharmacol 2005;15:411–23 [DOI] [PubMed] [Google Scholar]
- 34.Kessler RC, Ormel J, Petukhova M, et al. Development of lifetime comorbidity in the World Health Organization world mental health surveys. Arch Gen Psychiatry 2011;68:90–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Conway CC, Hammen C, Brennan PA. Expanding stress generation theory: test of a transdiagnostic model. J Abnorm Psychol 2012;121:754–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kessler RC, Petukhova M, Zaslavsky AM. The role of latent internalizing and externalizing predispositions in accounting for the development of comorbidity among common mental disorders. Curr Opin Psychiatry 2011;24:307–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kingerlee R. Conceptualizing men: a transdiagnostic model of male distress. Psychol Psychother 2012;85:83–99 [DOI] [PubMed] [Google Scholar]
- 38.Craske MG. Transdiagnostic treatment for anxiety and depression. Depress Anxiety 2012;29:749–53 [DOI] [PubMed] [Google Scholar]
- 39.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008–12 [DOI] [PubMed] [Google Scholar]
- 40.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med 2009;e6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brugha TS, Matthews R, Morgan Z, Hill T, Alonso J, Jones DR. Methodology and reporting of systematic reviews and meta-analyses of observational studies in psychiatric epidemiology: Systematic review. Br J Psychiatry 2012;200:446–53 [DOI] [PubMed] [Google Scholar]
- 42.Luppa M, Sikorski C, Luck T, et al. Age- and gender-specific prevalence of depression in latest-life – systematic review and meta-analysis. J Affect Disord 2012;136:212–21 [DOI] [PubMed] [Google Scholar]
- 43.Kieling C, Rohde LA. Going global: Epidemiology of child and adolescent psychopathology. J Am Acad Child Adolesc Psychiatry 2012;51:1236–37 [DOI] [PubMed] [Google Scholar]
- 44.Saha S, Chant D, McGrath J. Meta-analyses of the incidence and prevalence of schizophrenia: Conceptual and methodological issues. Int J Methods Psychiatr Res 2008;17:55–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Goldner EM, Hsu L, Waraich P, Somers JM. Prevalence and incidence studies of schizophrenic disorders: A systematic review of the literature. Can J Psychiatry 2002;47:833–43 [DOI] [PubMed] [Google Scholar]
- 46.Jenkins R, Lewis G, Bebbington P, et al. The National Psychiatric Morbidity surveys of Great Britain – initial findings from the household survey. Psychol Med 1997;27:775–89 [DOI] [PubMed] [Google Scholar]
- 47.Jenkins R, Meltzer H. The national survey of psychiatric morbidity in Great Britain. Soc Psychiatry Psychiatr Epidemiol 1995;30:1–4 [DOI] [PubMed] [Google Scholar]
- 48.Alonso J, Angermeyer MC, Bernert S, et al. Prevalence of mental disorders in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl 2004;109:21–27 [DOI] [PubMed] [Google Scholar]
- 49.Hausner E, Waffenschmidt S, Kaiser T, Simon M. Routine development of objectively derived search strategies. Syst Rev 2012;1:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wilczynski NL, Haynes RB, Hedges T. Optimal search strategies for identifying mental health content in MEDLINE: an analytic survey. Ann Gen Psychiatry 2006;5:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet 2013;382:1575–86 [DOI] [PubMed] [Google Scholar]
- 52.Guo W-J, Tsang A, Li T, Lee S. Psychiatric epidemiological surveys in China 1960-2010: how real is the increase of mental disorders? Curr Opin Psychiatry 2011;24:324–30 [DOI] [PubMed] [Google Scholar]
- 53.Steel Z, Chey T, Silove D, Marnane C, Bryant RA, Van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. JAMA 2009;302:537–49 [DOI] [PubMed] [Google Scholar]
- 54.Pietrantonj CD. Four-fold table cell frequencies imputation in meta analysis. Stat Med 2006;25:2299–322 [DOI] [PubMed] [Google Scholar]
- 55.Spiers N, Bebbington P, McManus S, Brugha TS, Jenkins R, Meltzer H. Age and birth cohort differences in the prevalence of common mental disorder in England: National psychiatric morbidity surveys 1993-2007. Br J Psychiatry 2011;198:479–84 [DOI] [PubMed] [Google Scholar]
- 56.Weich S, Brugha T, King M, et al. Mental well-being and mental illness: findings from the Adult Psychiatric Morbidity Survey for England 2007. Br J Psychiatry 2011;199:23–28 [DOI] [PubMed] [Google Scholar]
- 57.World Bank. World Bank World Development Indicators. Washington, DC: World Bank, 2012 [Google Scholar]
- 58.van Houwelingen HC, Arends LR, Stijnen T. Advanced methods in meta-analysis: Multivariate approach and meta-regression. Stat Med 2002;21:589–624 [DOI] [PubMed] [Google Scholar]
- 59.Riley RD, Higgins JPT, Deeks JJ. Interpretation of random effects meta-analyses. BMJ 2011;342:964–67 [DOI] [PubMed] [Google Scholar]
- 60.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58 [DOI] [PubMed] [Google Scholar]
- 61.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088–101 [PubMed] [Google Scholar]
- 62.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315 629–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jenkins R, Mbatia J, Singleton N, White B. Common mental disorders and risk factors in urban Tanzania. Int J Environ Res Public Health 2010;7:2543–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pakriev S, Vasar V, Aluoja A, Saarma M, Shlik J. Prevalence of mood disorders in the rural population of Udmurtia. Acta Psychiatr Scand 1998;97:169–74 [DOI] [PubMed] [Google Scholar]
- 65.Pakriev S, Vasar V, Aluoja A, Shlik J. Prevalence of ICD-10 harmful use of alcohol and alcohol dependence among the rural population in Udmurtia. Alcohol Alcohol 1998;33:255–64 [DOI] [PubMed] [Google Scholar]
- 66.Cheung P. Adult psychiatric epidemiology in China in the 80s. Cult Med Psychiatry 1991;15:479–96 [DOI] [PubMed] [Google Scholar]
- 67.Sterne JAC, Gavaghan D, Egger M. Publication and related bias in meta-analysis: Power of statistical tests and prevalence in the literature. J Clin Epidemiol 2000;53:1119–29 [DOI] [PubMed] [Google Scholar]
- 68.Khandaker GM, Kirkbride JB, Jones PB. Epidemiological challenges in systematic reviews. Br J Psychiatry 2012;201:248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Coory MD. Comment on: Heterogeneity in meta-analysis should be expected and appropriately quantified. Int J Epidemiol 2010;39:932. [DOI] [PubMed] [Google Scholar]
- 70.Higgins JPT. Commentary: Heterogeneity in meta-analysis should be expected and appropriately quantified. Int J Epidemiol 2008;37:115860. [DOI] [PubMed] [Google Scholar]
- 71.Kessler RC, Aguilar-Gaxiola S, Alonso J, et al. The global burden of mental disorders: an update from the WHO World Mental Health (WMH) surveys. Epidemiol Psichiatr Soc 2009;18:23–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Moffitt TE, Caspi A, Taylor A, et al. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychol Med 2010;40:899–909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Alegria M, Shrout PE, Torres M, et al. Lessons learned from the clinical reappraisal study of the Composite International Diagnostic Interview with Latinos. Int Psychiat Res 2009;18 84–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kessler RC, Birnbaum HG, Shahly V, et al. Age differences in the prevalence and co-morbidity of DSM-IV major depressive episodes: Results from the WHO world mental health survey initiative. Depress Anxiety 2010;27:351–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Liddell BJ, Chey T, Silove D, Phan TTB, Giao NM, Steel Z. Patterns of risk for anxiety-depression amongst Vietnamese-immigrants: a comparison with source and host populations. BMC Psychiatry 2013;13:329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lerner F, Hamblen JL. Methodology and reporting of systematic reviews and meta-analyses. Br J Psychiatry 2013;202:75–76 [DOI] [PubMed] [Google Scholar]
- 77.Shen YC, Zhang MY, Huang YQ, et al. Twelve-month prevalence, severity, and unmet need for treatment of mental disorders in metropolitan China. Psychol Med 2006;36:257–67 [DOI] [PubMed] [Google Scholar]
- 78.Steel Z, Silove D, Giao NM, et al. International and indigenous diagnoses of mental disorder among Vietnamese living in Vietnam and Australia. Br J Psychiatry 2009;194:326–33 [DOI] [PubMed] [Google Scholar]
- 79.Westermeyer J. Psychiatric epidemiology across cultures: current issues and trends. Transcult Psychiatr Res Rev 1989;26:5–25 [Google Scholar]
- 80.Littlewood R. From categories to contexts: a decade of the ‘new cross-cultural psychiatry’. Br J Psychiatry 1990;156:308–27 [DOI] [PubMed] [Google Scholar]
- 81.Kleinman AM. Depression, somatization and the ‘new cross-cultural psychiatry’. Soc Sci Med 1977;11:3–10 [DOI] [PubMed] [Google Scholar]
- 82.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 2007;370:851–58 [DOI] [PubMed] [Google Scholar]
- 83.Rai D, Zitko P, Jones K, Lynch J, Araya R. Country- and individual-level socioeconomic determinants of depression: Multilevel cross-national comparison. Br J Psychiatry 2013;202:195–203 [DOI] [PubMed] [Google Scholar]
- 84.Seedat S, Scott KM, Angermeyer MC, et al. Cross-national associations between gender and mental disorders in the World Health Organization World Mental Health Surveys. Arch Gen Psychiatry 2009;66:785–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Patten SB. International differences in major depression prevalence: What do they mean? J Clin Epidemiol 2003;56:711–16 [DOI] [PubMed] [Google Scholar]
- 86.Lee S, Tsang A, Zhang M-Y, et al. Lifetime prevalence and inter-cohort variation in DSM-IV disorders in metropolitan China. Psychol Med 2007;37:61–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Murray CJL, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2197–223 [DOI] [PubMed] [Google Scholar]
- 88.Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2163–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Whiteford HA, Ferrari AJ, Baxter AJ, Charlson FJ, Degenhardt L. How did we arrive at burden of disease estimates for mental and illicit drug use disorders in the Global Burden of Disease Study 2010? Curr Opin Psychiatry 2013;26:376–83 [DOI] [PubMed] [Google Scholar]
- 90.Bracken P, Thomas P, Timimi S, et al. Psychiatry beyond the current paradigm. Br J Psychiatry 2012;201:430–34 [DOI] [PubMed] [Google Scholar]
- 91.Summerfield D, Veale D. Proposals for massive expansion of psychological therapies would be counterproductive across society. Br J Psychiatry 2008;192:326–30 [DOI] [PubMed] [Google Scholar]
- 92.Chisholm D, Flisher A, Lund C, et al. Scale up services for mental disorders: a call for action. Lancet 2007;370:1241–52 [DOI] [PubMed] [Google Scholar]
- 93.Prince M, Patel V, Saxena S, et al. No health without mental health. Lancet 2007;370:859–77 [DOI] [PubMed] [Google Scholar]
- 94.Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. Lancet 2007;370:878–89 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.