Abstract
Objective
Medical-surgical re-hospitalizations within a month after discharge among patients with diabetes result in tremendous costs to the US healthcare system. This study aims to examine if comorbid serious mental illness (SMI) diagnoses (bipolar disorder, schizophrenia, or other psychotic disorders) among patients with diabetes are independently associated with medical-surgical re-hospitalization within a month of discharge after an initial hospitalization.
Methods
This cohort study of all community hospitals in Washington State evaluated data from 82,060 adults discharged in the state of Washington with any ICD-9 CM diagnosis indicating diabetes mellitus between 2010 and 2011. Data on medical-surgical hospitalizations were obtained from the Washington State Comprehensive Hospital Abstract Reporting System. Comorbid SMI diagnoses were identified based on ICD-9 CM diagnosis codes indicating bipolar disorder, schizophrenia or other psychotic disorders. Logistic regression analyses identified factors independently associated with re-hospitalization within a month of discharge. Cox Proportional Hazard analyses estimated time to re-hospitalization for the entire study period.
Results
After adjusting for demographics, medical comorbidity, and characteristics of the index hospitalization, comorbid SMI diagnosis was independently associated with increased odds of re-hospitalization within one month among patients with diabetes who had a medical-surgical hospitalization (Odds Ratio: 1.24, 95% Confidence Interval: 1.07, 1.44). This increased risk of re-hospitalization persisted throughout the study period (up to 24 months).
Conclusions
Comorbid SMI in patients with diabetes is independently associated with greater risk of early medical-surgical re-hospitalization. Future research is needed to define and specify targets for interventions at points of care transition for this vulnerable patient population.
Keywords: Serious Mental Illness, Re-Hospitalization, Diabetes
Background
Diabetes imposes a tremendous economic burden on the US healthcare system: 10% of healthcare dollars are spent on direct costs related to diabetes. The total estimated cost of diabetes was $174 billion in 2007, and the Centers for Disease Control and Prevention project that spending on diabetes care will reach $192 billion in 2020 (1, 2). About half of diabetes-related health care costs are due to potentially preventable complications (3). In the US, hospital admissions for long-term complications such as cardiovascular disease, stroke, and renal failure comprise the majority of diabetes-related expenditures. Patients with diabetes are also at increased risk for medical conditions that can lead to unplanned re-hospitalization, such as community-acquired pneumonia (4, 5).
Among Medicare beneficiaries, re-hospitalization within 30 days of discharge occurs in almost 20% of patients, costing the healthcare system an estimated $17.4 billion in 2004 (6). Up to one-fifth of unplanned re-hospitalizations may be preventable (7), so even a small reduction might reduce costs. Indeed, a key part of the comprehensive strategy of the Centers for Medicare and Medicaid Services to reduce costs is a focus on reducing 30-day hospital re-hospitalizations for heart failure, acute myocardial infarction, and pneumonia (8, 9). Unplanned re-hospitalizations may be a marker of poorer quality of inpatient care or ineffective hospital-to-home transitions (10-13). But not all re-hospitalizations reflect poor quality of inpatient care, especially among complex patients with multiple chronic conditions (14-17). Among patients with diabetes, increased re-hospitalization rates have been associated with demographic factors (older age, non-white race/ ethnicity, and rural residence), ineffective transition to outpatient care (e.g., no outpatient follow-up within 30-days of discharge) (18, 19), and a broad range of social factors, including lack of social support (20-21). However, there have been few studies examining the impact of psychiatric disorders on risk of medical-surgical re-hospitalization.
Among patients with diabetes, those with comorbid serious mental illness (SMI) (such as bipolar disorder, schizophrenia or other psychotic disorders) have higher rates of diabetes complications (22), higher rates of hospitalizations for an ambulatory care-sensitive condition (23), more diabetes-related hospitalizations (24), and increased diabetes-specific mortality (22, 23). Both health-risk behaviors (e.g., smoking, poor diet, and sedentary lifestyle) and pharmacotherapy for psychiatric illness contribute to these poor outcomes, as treatment with second generation antipsychotic medications has been associated with poorer glycemic control among patients with diabetes (25-26). Among Medicaid enrollees with diabetes, those with a psychiatric illness receive poorer quality of outpatient diabetes care, including less intensive pharmacotherapy for diabetes and other cardiovascular risk factors (27, 28). Patients with SMI also appear to under-utilize primary care (29), increasing their risk of potentially preventable medical hospitalizations. Furthermore, these patients may also be at heightened risk of in-hospital adverse events such as nosocomial infections and postoperative complications (30).
Prior research has shown that hospitalized patients with comorbid major depressive or bipolar disorder are at increased risk of subsequent medical hospitalization over a 5-year period (31). Depression has also been associated with increased odds of unplanned re-hospitalization within 30 days among patients 65 years and older (32). But only one study has evaluated comorbid SMI diagnoses as risk factors for medical-surgical re-hospitalization within 30 days among patients with diabetes. This study found no increased risk associated with the presence of these diagnoses (33), but did suggest an association among patients older than 45 which failed to reach statistical significance. This study was done at a single site and may have lacked statistical power since 30-day re-hospitalization is a relatively rare outcome.
The current study had two aims. First, we evaluated the independent association of SMI diagnoses with risk of medical-surgical re-hospitalization among patients with diabetes. We hypothesized that the presence of a SMI diagnosis would be associated with re-hospitalization within one month of discharge from the index hospitalization as well as with elevated risk for re-hospitalization during the entire study period (up to 24 months of follow-up). Second, we sought to identify patient-level characteristics and index hospitalization-related factors that were associated with greater risk of re-hospitalization among these patients.
Methods
Study Design
Data on hospitalizations were obtained from the Washington State Comprehensive Hospital Abstract Reporting System (CHARS) (31). The CHARS database contains abstracts on de-identified patients hospitalized in community hospitals in Washington State. The CHARS database contains abstracts on patients hospitalized in all civilian hospitals in the state; federal (Veterans Affairs and Military) hospitals and state psychiatric hospitals are excluded. A revisit file provided by the Washington State Department of Health allowed hospitalizations to be linked to de-identified patients. Since patients in the study were de-identified, the study was considered exempt from review by the Washington State University IRB.
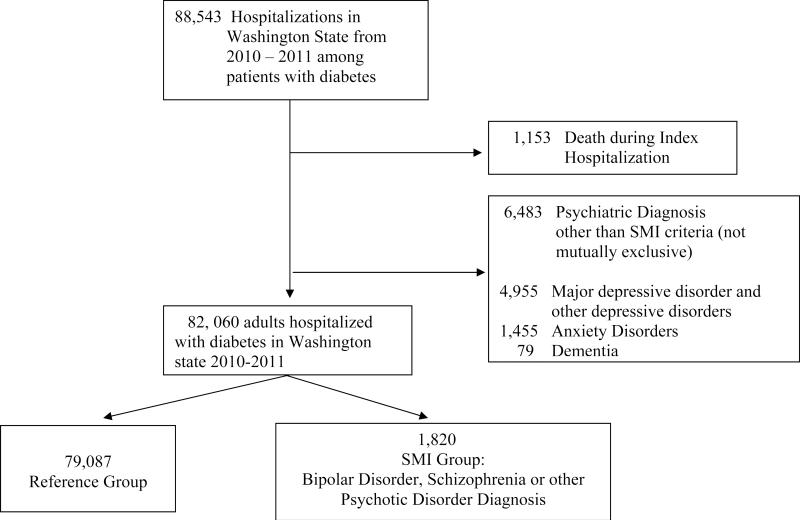
This observational cohort study was comprised of 82,060 adults ≥ 18 years of age in Washington state who had a medical-surgical hospitalization between 2010 and 2011 with any discharge diagnosis indicating diabetes mellitus (International Classification of Disease – 9th Edition (ICD9-CM) diagnosis 250). Index hospitalizations ending in death and hospital transfers were excluded so that only patients discharged to home, long-term care, or hospice were included. Hospitalizations for prenatal care (ICD9-CM primary diagnosis 760-779), labor and delivery or maternity care (ICD9-CM primary diagnosis 630-679), and those for a primary diagnosis of a psychiatric disorder (ICD9-CM primary diagnosis 290-319) were excluded. An additional 6,483 patients were excluded based on the presence of any diagnosis indicating major depressive disorder (ICD9-CM diagnosis 296.2 or 296.3), other depressive disorders (ICD9-CM diagnosis 311), anxiety disorders (ICD9-CM diagnosis 300.4), or dementia (ICD9-CM diagnosis 290). Patients were followed for 1-24 months after their index hospitalization for longitudinal analyses.
Variable Definitions
Serious mental illness
Patients with comorbid SMI diagnoses were identified based on diagnosis codes indicating bipolar disorder (ICD9-CM 296. [0,1,4,5,6,7,8]), schizophrenia (ICD9-CM 295), and the psychotic disorders delusional disorder (ICD9-CM 297) and non-organic psychoses (ICD0-CM 298), consistent with definitions from previous literature (34, 35). The reference cohort was defined as all other patients in the study.
Demographic characteristics were drawn from the index hospitalization
Primary health insurance payer of record on the index hospitalization was used to classify patients as Medicare, Medicaid, Commercial/Health Maintenance Organization and Self-pay. Primary and secondary health insurance payer on the index hospitalization was used to classify patients as dual-enrolled Medicare and Medicaid.
Co-morbidity
Medical comorbidity was determined from a comprehensive set of 24 variables drawn from the index hospitalization and any hospitalizations within 12 months prior to the index hospitalization using the Elixhauser method (36), each coded as present or absent and entered into statistical models as independent variables. Elixhauser definitions have been associated with increased inpatient costs, length of stay and in-hospital mortality (36). The presence of a substance disorder diagnosis was determined from ICD9-CM diagnoses (291, 292, 303, 304) from the index hospitalization records.
Previous hospitalizations
In order to control for varying entry points in the course of disease, we obtained a count of medical-surgical hospitalizations during the 12 months prior to the index hospitalization.
Hospitalization characteristics
Admission to the hospital through the Emergency Department (ED) and primary diagnosis for both index hospitalization and re-hospitalizations were recorded.
Statistical Analyses
The primary outcome of the study was pre-specified as subsequent re-hospitalization within the first month following index hospitalization discharge. Additional outcomes of interest were subsequent re-hospitalization during the duration of the study (up to 24 months) and the elapsed time from index hospitalization to re-hospitalization. For descriptive analyses, patients with comorbid SMI diagnoses were compared to patients without these diagnoses.
We used binary logistic regression models to estimate Odds Ratios (ORs) and 95% Confidence Intervals (95%CIs) for the potential association of comorbid SMI diagnoses and re-hospitalization in the next month. First, we tested the association of comorbid SMI diagnoses with re-hospitalization in the next month without adjustment. We then sequentially adjusted for potentially confounding variables in the following sequence: 1) index hospitalization substance disorder diagnosis; 2) age, gender, payer, number of hospitalizations in the 12 months prior to baseline, index hospitalization admission through the ED and length of stay; 3) medical co-morbidity (Elixhauser method), and 4) index hospitalization primary diagnoses. We fitted an additional logistic regression model testing the presence of effect modification between comorbid SMI and substance abuse diagnoses with respect to re-hospitalization within a month following the index medical-surgical hospitalization.
For analyses of time from index hospitalization to re-hospitalization, we used sequentially adjusted Cox Proportional-Hazard regression models to estimate Hazard Ratios (HRs) and 95%CIs.
A p-value <0.05 was required to define statistical significance for all analyses. SPSS Version 18.0 (IBM; Chicago, Ill) was used for all statistical analyses.
Results
Of the 82,060 adults with diabetes in Washington State who had a medical-surgical hospitalization between 2010 and 2011, 1,820 (2.2%) patients had a co-morbid SMI diagnosis, including, 29% with a diagnosis of schizophrenia (n= 531); 60% with diagnosis of bipolar disorder (n = 1090) and 11% with a diagnosis of another psychotic disorder (n = 203). Four patients had diagnoses of both schizophrenia and another psychotic disorder. Table 1 describes the demographic and clinical characteristics of the patients at the index hospitalizations, and shows differences between patients with diagnoses of SMI and the reference group. Hospitalized patients with diabetes and comorbid SMI diagnosis were younger (mean age: 55.8, standard deviation [SD]: 14.4) than patients without any SMI diagnosis (mean age: 65.4, SD: 14.8). The percentage of patients with Type 1 diabetes was higher among patients with a comorbid SMI diagnosis than among the reference group (5.4% compared to 4.3%). More patients with diabetes and a SMI diagnosis had a substance use disorder diagnosis and some form of public insurance. A greater proportion of patients with a SMI diagnosis had ≥ 1 hospitalization in the preceding 12 months (16.6% compared to 11.6%).
Table 1.
Characteristics of Patients with Diabetes Mellitus Discharged from Washington State Hospitals 2010-2011.
| Reference (n=79,087) | SMI1 (n=1,820) | ||||
|---|---|---|---|---|---|
| Demographic Characteristics | Values | n | % | n | % |
| Gender | Male | 40,364 | 51.0 | 722 | 39.7 |
| Female | 38,723 | 49.0 | 1,098 | 60.3 | |
| Race2 | White | 23,802 | 86.1 | 495 | 84.0 |
| Black or African American | 1,311 | 4.7 | 54 | 9.2 | |
| American Indian or Alaska Native | 511 | 1.8 | 9 | 1.5 | |
| Asian | 1,911 | 4.3 | 14 | 2.4 | |
| Native Hawaiian/Pacific Islander | 840 | 3.0 | 17 | 2.9 | |
| Primary payer | Medicare | 33,774 | 42.7 | 494 | 27.1 |
| Medicaid | 5,813 | 7.3 | 453 | 24.9 | |
| Commercial/HMO | 28,831 | 36.5 | 411 | 22.6 | |
| Self-pay/Charitable Care | 4,116 | 5.2 | 50 | 2.7 | |
| Dual Medicare/Medicaid | 6,552 | 8.3 | 412 | 22.6 |
| Mean | SD | Mean | SD | ||
|---|---|---|---|---|---|
| Age (years) | 65.4 | 14.8 | 55.8 | 14.4 |
| Comorbidity | n | % | n | % | |
|---|---|---|---|---|---|
| Heart Failure | 7,172 | 9.1 | 90 | 4.9 | |
| Renal Failure | 12,216 | 15.4 | 153 | 8.4 | |
| Diabetes Complicated | 14,473 | 18.3 | 246 | 13.5 | |
| Hypertension Complicated | 10,712 | 13.5 | 138 | 7.6 | |
| Peripheral Vascular | 4,104 | 5.2 | 38 | 2.1 | |
| Substance Use Disorder | 8,620 | 10.9 | 407 | 22.4 | |
| 1+ Previous 12 Month Hospitalizations | 9,146 | 11.6 | 305 | 16.8 |
| Characteristics of Index hospitalization | ICD9-CM | n | % | n | % |
|---|---|---|---|---|---|
| Primary Diagnosis | |||||
| Diabetes | 250 | 5,412 | 6.8 | 203 | 11.2 |
| Diabetes – Ketoacidosis | 250.1 | 1,945 | 2.5 | 78 | 4.3 |
| Diabetes – Hypoglycemia | 250.8 | 1,295 | 1.6 | 33 | 1.8 |
| Diabetes – Hyperosmolar and Neurologic | 250.2; 250.3; 250.6 | 998 | 1.3 | 45 | 2.5 |
| Diabetes – Uncomplicated | 250.0 | 537 | 0.7 | 40 | 2.2 |
| Ischemic Heart Disease | 410-414 | 5,770 | 7.3 | 55 | 3.0 |
| Cardiac Arrhythmias | 427 | 2,400 | 3.0 | 28 | 1.5 |
| Stroke | 430-438 | 3,625 | 4.6 | 45 | 2.5 |
| COPD | 490-496 | 2,052 | 2.6 | 94 | 5.2 |
| Sepsis | 038 | 2,761 | 3.5 | 51 | 2.8 |
| Pneumonia | 480-486 | 2,747 | 3.5 | 72 | 4.0 |
| Congestive Heart Failure | 428 | 2,894 | 3.7 | 20 | 1.1 |
| Acute Kidney Injury | 584 | 1,700 | 2.1 | 36 | 2.0 |
| Poisoning | 960-979 | 351 | 0.4 | 55 | 3.0 |
| Procedural Complications | 996-999 | 2,189 | 2.8 | 33 | 1.8 |
| Injury | 800-959 | 3,574 | 4.5 | 76 | 4.2 |
| Admission Through ED | 14,628 | 18.5 | 427 | 23.5 |
(N=80,907)
SMI cohort includes patients with Diabetes Mellitus and co-occurring diagnosis for bipolar and psychoses disorders.
Race indicated on subset of records. Rates based on cases in which race was indicated.
IQR=Inter Quartile Range (25th-75th Percentile).
A greater proportion of patients with a SMI diagnosis were admitted through the ED for the index medical hospitalization; and primary diagnosis for the index hospitalization also differed between the groups. Among patients in the reference group, 6.8% of the index hospitalizations were for a primary diagnosis of diabetes, which is consistent with 2008 national data rate of 6.7% (37). Among the patients in this study with SMI diagnoses, however, a greater proportion of index hospitalizations (11.2%, Table 1) were for diabetes or diabetes-related complications, particularly diabetic ketoacidosis).
Of all re-hospitalizations over the study period, 10,613 occurred within a month of the index hospitalization. Patients with a comorbid SMI diagnosis had higher rates of re-hospitalization within the first month of discharge after the index hospitalization (15.4% compared to 13.1%), and also during the entire study period (42.7% compared to 37.9%). In logistic regression analyses, the presence of a comorbid SMI diagnosis was associated with an increased odds of re-hospitalization within a month of discharge from the index hospitalization (OR: 1.22, 95%CI: 1.07, 1.38). After adjusting for demographics, insurance type, comorbid substance use disorder diagnosis, number of hospitalizations in the year pre-baseline, index admission through the ED, and index admission length of stay, a significant association remained between a SMI diagnosis and re-hospitalization within the next month (OR: 1.17, 95%CI: 1.01, 1.36). This association remained significant after adjusting for comorbidities using the Elixhauser method (OR: 1.22, 95%CI: 1.05, 1.42). In the fully adjusted logistic regression model, a SMI diagnosis was independently associated with medical-surgical re-hospitalization within the next month (OR: 1.24, 95%CI: 1.07, 1.44) (Table 2 and supplemental table 1). In subgroup analyses to evaluate the impact of each SMI diagnosis on 30-day re-hospitalization, all diagnoses were significantly associated with increased odds of re-hospitalization in unadjusted models. Bipolar disorder and other psychoses remained significant in the fully adjusted models. The presence of a substance use disorder diagnosis was also associated with re-hospitalization within the next month in the final logistic regression model (OR: 1.10, 95%CI: 1.03, 1.18), but there was no evidence of effect modification between comorbid SMI and substance use disorder diagnoses with respect to re-hospitalization within one month (Table 2). Older age, public insurance, medical hospitalization in the 12 months prior to the index hospitalization, and admission through the ED and length of stay of the index hospitalization were also independently associated with increased odds of re-hospitalization in the final fully-adjusted model (supplemental table 1).
Table 2.
Re-hospitalization among Patients Hospitalized with Diabetes Mellitus in Washington State Hospitals 2010-2011. (N=80,907)
| Cohort | Re- Hospitalization (next month) |
|||||
|---|---|---|---|---|---|---|
| N | n | % | OR1 | 95%CI | p | |
| SMI2 | 1,820 | 281 | 15.4 | 1.24 | 1.07-1.44 | 0.006 |
| Reference | 79,087 | 10,332 | 13.1 | |||
| Numbers at Risk | ||||||
| SMI | 1,820 | 1,053 | 599 | 274 | 48 | |
| Reference | 79,087 | 46,291 | 27,832 | 13,170 | 2,344 | |
OR=Fully Adjusted odds ratio computed by binary logistic regression for risk of re-hospitalization within the next month controlling for substance use disorder, interaction of substance use disorder and cohort, age, sex, race, payer, index admission through ED and length of stay, count of hospitalizations in the previous 12 months, Elixhauser medical comorbidities, and primary diagnosis for index hospitalization.
SMI cohort includes patients with Diabetes Mellitus and diagnosis of bipolar disorder, schizophrenia or other psychotic disorders.
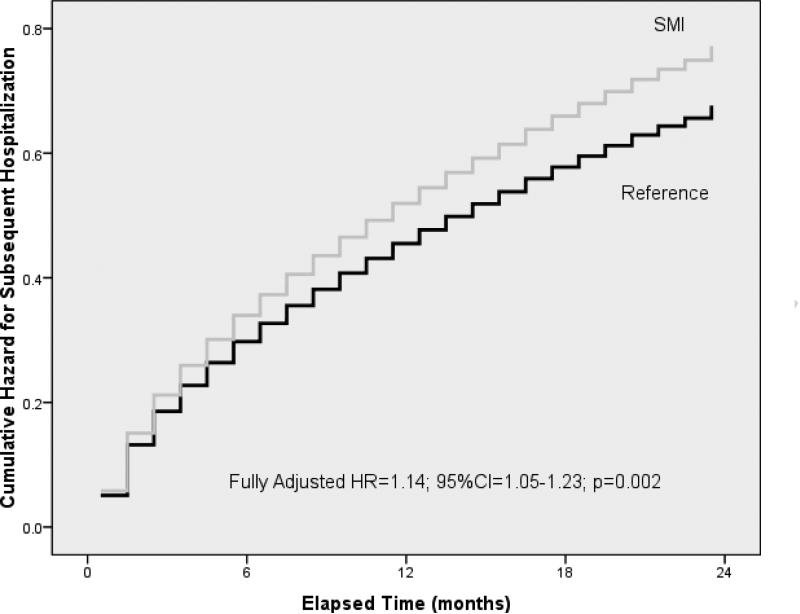
We next evaluated the association between SMI diagnosis and increased risk of re-hospitalization throughout the entire study period. In unadjusted analyses, patients with a comorbid SMI diagnosis had a 15% greater risk of re-hospitalization for medical-surgical illnesses during the 24-month study period (HR: 1.15, 95%CI: 1.07, 1.24). In the fully adjusted proportional-hazards model (Figure 2, supplemental table 2), a comorbid SMI diagnosis was independently associated with a 14% greater risk of re-hospitalization for medical-surgical illnesses (HR: 1.14, 95%CI: 1.05, 1.23) (Supplemental Table 2). As in the analyses of the odds of re-hospitalization within a month after discharge, there was also an independent association between a substance use disorder diagnosis and risk of re-hospitalization (HR: 1.08, 95%CI: 1.04, 1.12)—but no evidence of effect modification between SMI and substance use disorder diagnoses and risk of re-hospitalization during the study period.
Figure 2.
Time to Re-Hospitalization using Cox Proportional Hazard Analysis for Patients with Diabetes Mellitus Discharged from Washington State Hospitals 2010-2011. (N=80,907)
Fully-adjusted model controlling for substance use disorder, interaction of substance use disorder and cohort, age, sex, race, payer, index admission through ED and length of stay, count of hospitalizations in the previous 12 months, Elixhauser medical comorbidities, and primary diagnosis for index hospitalization.
Table 3 displays the most common primary diagnoses for re-hospitalizations occurring within one month of the index hospitalization. Among patients with comorbid diabetes and SMI diagnoses, diabetes itself was the most common primary diagnosis leading to early re-hospitalization. In contrast, complications related to procedures during the index hospitalization were the most common primary diagnoses leading to early re-hospitalization among patients without SMI diagnoses.
Table 3.
Primary Diagnosis for Re-hospitalization within the Next Month after Discharge from Index Hospitalization in Washington State 2010-2011.
| Reference Cohort (10,332 Hospitalizations) | SMI Cohort (281 Hospitalizations) | ||||||
|---|---|---|---|---|---|---|---|
| Primary Diagnosis | ICD9-CM | n | % | Primary Diagnosis | ICD9-CM | n | % |
| Procedural Complications | 996-999 | 859 | 8.3 | Diabetes Mellitus | 250 | 22 | 7.8 |
| Heart Failure | 428 | 638 | 6.2 | Procedural Complications | 996-999 | 21 | 7.5 |
| Ischemic Heart Disease | 410-414 | 586 | 5.7 | Sepsis | 038 | 20 | 7.1 |
| Diabetes Mellitus | 250 | 514 | 5.0 | Acute Kidney Failure | 584 | 13 | 4.6 |
| Sepsis | 038 | 505 | 4.9 | Chronic Pulmonary Disorders | 490-496 | 11 | 3.9 |
| SMI Cohort | 0.21 | 0.08 | 1.24 | 1.07-1.44 | 0.006 |
| Cohort*Substance Abuse | 0.06 | 0.16 | 1.07 | 0.78-1.46 | 0.70 |
| Substance Abuse | 0.10 | 0.04 | 1.10 | 10.3-1.18 | 0.008 |
| Age | 0.01 | 0.001 | 1.01 | 1.01-1.01 | <0.001 |
| Gender Female | −0.03 | 0.02 | 0.97 | 0.93-1.01 | 0.15 |
| Race Caucasian1 | −0.09 | 0.03 | 0.91 | 0.87-0.96 | <0.001 |
| Race African American1 | −0.04 | 0.09 | 0.97 | 0.82-1.14 | 0.68 |
| Race American Indian1 | −0.06 | 0.14 | 0.94 | 0.71-1.25 | 0.68 |
| Race Asian1 | −0.44 | 0.11 | 0.64 | 0.52-0.79 | <0.001 |
| Race Pacific Islander1 | 0.27 | 0.10 | 1.31 | 1.08-1.58 | 0.005 |
| Race Mixed and Other1 | 0.12 | 0.77 | 1.13 | 0.25-5.05 | 0.88 |
| Medicare and Medicaid | 0.18 | 0.02 | 1.19 | 1.34-1.25 | <0.001 |
| Previous 12 Month Hospitalization | 0.24 | 0.01 | 2.27 | 1.24-1.30 | <0.001 |
| Admission through ED | 0.08 | 0.03 | 1.08 | 1.02-1.15 | 0.005 |
| Length of Stay | 0.04 | 0.003 | 1.04 | 1.04-1.05 | <0.001 |
| Comorbid Aids | −0.19 | 0.41 | 0.83 | 0.37-1.85 | 0.65 |
| Comorbid Anemia Deficiency | 0.09 | 0.03 | 1.10 | 1.03-1.17 | 0.002 |
| Comorbid Rheumatoid Arthritis | 0.16 | 0.07 | 1.17 | 1.02-1.34 | 0.03 |
| Comorbid Blood Loss Anemia | 0.18 | 0.09 | 1.20 | 1.00-1.43 | 0.05 |
| Comorbid Congestive Heart Failure | 0.24 | 0.03 | 1.27 | 1.18-1.35 | <0.001 |
Discussion
In this prospective cohort study of adult patients with diabetes who had a medical-surgical hospitalization in Washington State between 2010 and 2011, the presence of a co-morbid SMI diagnosis was independently associated with increased odds of medical re-hospitalization within one month. This group had an increased odds of early re-hospitalization despite being, on average, younger than those patients without SMI diagnoses; and the increased odds of re-hospitalization persisted even after adjustment for demographic factors, medical comorbidity, and co-occurring substance use disorder diagnoses. There was an increased prevalence of substance use disorder diagnoses among those patients with SMI diagnoses compared to patients in the reference group—and substance use disorder diagnoses were independently associated with risk of re-hospitalization. Consistent with previous studies examining risk factors for medical-surgical re-hospitalization in general, we found that older age and index hospitalization length of stay were independently associated with this outcome among patients with diabetes (32, 38). We also found that admission through the ED for the index hospitalization was associated with greater odds of early medical-surgical re-hospitalization, which may reflect the acuity of the medical illness leading to the index hospitalization—or the ineffective use of primary care by persons with SMI (27).
Subgroup analyses suggested that this finding was most robust among those patients with a diagnosis of bipolar disorder, as a diagnosis of schizophrenia was no longer significant in the final fully adjusted models. This finding may be explained by imprecision in the diagnostic coding of psychiatric disorders among medical-surgical inpatients. Alternatively, given the significantly increased odds of re-hospitalization among patients with a schizophrenia diagnosis in the unadjusted model, covariates which were included in the adjusted model (e.g., substance use disorders medical co-morbidity, or insurance status) may have had a greater impact on re-hospitalization in this subgroup.
Among patients with diabetes and comorbid SMI diagnoses, the most common primary diagnosis for both index hospitalization and re-hospitalization within a month of discharge was diabetes itself. By comparison, rates of admission for a diagnosis of diabetes among patients in the reference group were consistent with national data on admission diagnoses among patients with diabetes (37), suggesting that poorly-controlled diabetes may be driving excess hospitalizations among patients with a comorbid SMI diagnosis. This interpretation is further supported by the observed higher rates of hospitalization for diagnoses of ketoacidosis, hyperosmolar states, and neurologic complications among patients with SMI diagnoses. A previous study found no association between SMI diagnosis and risk of medical re-hospitalization among patients with diabetes (33), but suggested an association among patients older than 45 years (not statistically significant). The larger sample size and number of hospitals in the current study may help to explain differences in our findings. Moreover, the exclusion of patients with a depression diagnosis from the SMI cohort in the current study may highlight a unique vulnerability among patients with bipolar disorder or psychotic disorders.
Patients with SMI hospitalized for medical illnesses may face unique challenges at key healthcare transition points (e.g., from the hospital back to primary care) due to poorer overall quality of care as well as psychiatric symptoms and impaired cognition. Previous work has identified that break downs in care at such key transition points due to both patient and system-level factors may increase the risk of early re-hospitalizations (39). Furthermore, patients with SMI may be at heightened risk of social vulnerabilities which may increase the risk of early re-hospitalization, such as homelessness, poor health literacy and poverty (21). But interventions that have been shown to prevent early re-hospitalizations (13, 40) have not been studied in patients with SMI and comorbid medical illnesses. As this study suggests, subgroups of patients with diabetes and comorbid SMI (those dual-enrolled with Medicaid/Medicare and those with comorbid substance use disorder diagnoses) may be at particular risk of early re-hospitalization, and require specific intervention.
Our study has several potential limitations. The use of administrative data to identify patients with SMI diagnoses may have resulted in the misclassification of patients with SMI disorders and their inclusion in the reference group. But the prevalence rate for bipolar disorder in this sample (1.3%) is comparable to lifetime prevalence estimates in the US population of 1-3% (41), as is the rate of schizophrenia (0.8% in the sample compared to population rates of 0.3-0.8%) (42). Also, the use of administrative data did not allow for us to capture and adjust for poor health behaviors that may mediate the greater risk of early medical-surgical hospitalization such as smoking, sedentary lifestyle and poor diet in patients with SMI. Furthermore, while we were able to rigorously evaluate the burden of medical comorbidity using the Elixhauser method, we were unable to adjust for diabetes severity, as laboratory data was not available. Second, while we found a robust independent effect of comorbid SMI, we cannot attribute this increased risk to the psychiatric disorders per se. Our inability to access pharmacy data still leaves open the question of the extent to which this increased risk of re-hospitalization is due to treatment with specific second generation antipsychotic medications, as there appears to be heterogeneity across these medications with respect to the risk of diabetic ketoacidosis (43). Additionally, no information about the utilization of outpatient (primary care) services is included; thus, it is possible that decreased access to outpatient medical care significantly contributes to the increased risk of medical re-hospitalization among patients with SMI.
In conclusion, we found that a comorbid SMI diagnosis in patients with diabetes was independently associated with greater odds of early medical-surgical re-hospitalization, possibly indicating poor quality of medical care for these patients with diabetes who have comorbid SMI. Alternatively, our findings may be further evidence that patients with SMI interact with healthcare system differently and have unique barriers to adherence with medical care and follow-up. Improving the coordination or integration of outpatient medical and psychiatric care for these complex patients may decrease risk of early re-hospitalizations. Future research is needed to develop interventions addressing the unique challenges that patients with SMI face surrounding key care transition points to both reduce healthcare costs and prevent potential morbidity and mortality.
Supplementary Material
Figure 1.
Study Flow Diagram
Acknowledgements
The research reported here was supported by grants K23 MH077824 and KL2 TR000421from the National Institutes of Health, and grants from the National Center for Research Resources (5P20RR016474-12) and the National Institute of General Medical Sciences (8 P20 GM103432-12) from the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure
None of the authors has a conflict of interest to disclose.
References
- 1.Centers for Disease Control and Prevention . National Diabetes Fact Sheet. National Center for Chronic Disease Prevention and Health Promotion; Division of Diabetes Translation; 2007. [Google Scholar]
- 2.American Diabetes Association Economic costs of diabetes in the U.S. In 2007. Diabetes Care. 2008;31(3):596–615. doi: 10.2337/dc08-9017. [DOI] [PubMed] [Google Scholar]
- 3.Herman WH, Eastman RC. The effects of treatment on the direct costs of diabetes. Diabetes Care. 1998;21(Suppl 3):C19–24. doi: 10.2337/diacare.21.3.c19. [DOI] [PubMed] [Google Scholar]
- 4.Ehrlich SF, Quesenberry CP, Jr., Van Den Eeden SK, Shan J, Ferrara A. Patients diagnosed with diabetes are at increased risk for asthma, chronic obstructive pulmonary disease, pulmonary fibrosis, and pneumonia but not lung cancer. Diabetes Care. 2010;33(1):55–60. doi: 10.2337/dc09-0880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kornum JB, Thomsen RW, Riis A, Lervang HH, Schonheyder HC, Sorensen HT. Diabetes, glycemic control, and risk of hospitalization with pneumonia: a population-based case-control study. Diabetes Care. 2008;31(8):1541–5. doi: 10.2337/dc08-0138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for- service program. N Engl J Med. 2009;360(14):1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 7.Kim H, Ross JS, Melkus GD, Zhao Z, Boockvar K. Scheduled and unscheduled hospital readmissions among patients with diabetes. Am J Manag Care. 2010;16(10):760–7. [PMC free article] [PubMed] [Google Scholar]
- 8.Kocher RP, Adashi EY. Hospital readmissions and the Affordable Care Act: paying for coordinated quality care. JAMA. 2011;306(16):1794–5. doi: 10.1001/jama.2011.1561. [DOI] [PubMed] [Google Scholar]
- 9.National Quality Forum . National Voluntary Consensus Standards for Hospital Care 2007: Performance measures - A consensus report. National Quality Forum; Washington, DC: 2008. [Google Scholar]
- 10.Ashton CM, Kuykendall DH, Johnson ML, Wray NP, Wu L. The association between the quality of inpatient care and early readmission. Ann Intern Med. 1995;122(6):415–21. doi: 10.7326/0003-4819-122-6-199503150-00003. [DOI] [PubMed] [Google Scholar]
- 11.Halfon P, Eggli Y, Pretre-Rohrbach I, Meylan D, Marazzi A, Burnand B. Validation of the potentially avoidable hospital readmission rate as a routine indicator of the quality of hospital care. Med Care. 2006;44(11):972–81. doi: 10.1097/01.mlr.0000228002.43688.c2. [DOI] [PubMed] [Google Scholar]
- 12.Balaban RB, Weissman JS, Samuel PA, Woolhandler S. Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study. J Gen Intern Med. 2008;23(8):1228–33. doi: 10.1007/s11606-008-0618-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822–8. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 14.Vaduganathan M, Bonow RO, Gheorghiade M. Thirty-day readmissions: the clock is ticking. JAMA. 2013;309(4):345–6. doi: 10.1001/jama.2012.205110. [DOI] [PubMed] [Google Scholar]
- 15.Hasan O, Meltzer DO, Shaykevich SA, Bell CM, Kaboli PJ, Auerbach AD, et al. Hospital readmission in general medicine patients: a prediction model. J Gen Intern Med. 2010;25(3):211–9. doi: 10.1007/s11606-009-1196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kossovsky MP, Sarasin FP, Perneger TV, Chopard P, Sigaud P, Gaspoz J. Unplanned readmissions of patients with congestive heart failure: do they reflect in-hospital quality of care or patient characteristics? Am J Med. 2000;109(5):386–90. doi: 10.1016/s0002-9343(00)00489-7. [DOI] [PubMed] [Google Scholar]
- 17.Louis Simonet M, Kossovsky MP, Chopard P, Sigaud P, Perneger TV, Gaspoz JM. A predictive score to identify hospitalized patients' risk of discharge to a post-acute care facility. BMC Health Serv Res. 2008;8:154. doi: 10.1186/1472-6963-8-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jiang HX, Majumdar SR, Dick DA, Moreau M, Raso J, Otto DD, et al. Development and initial validation of a risk score for predicting in-hospital and 1-year mortality in patients with hip fractures. J Bone Miner Res. 2005;20(3):494–500. doi: 10.1359/JBMR.041133. [DOI] [PubMed] [Google Scholar]
- 19.Bennett KJ, Probst JC, Vyavaharkar M, Glover S. Missing the handoff: post-hospitalization follow- up care among rural Medicare beneficiaries with diabetes. Rural Remote Health. 2012;12:2097. [PubMed] [Google Scholar]
- 20.Garrison GM, Mansukhani MP, Bohn B. Predictors of thirty-day readmission among hospitalized family medicine patients. J Am Board Fam Med. 2013;26(1):71–7. doi: 10.3122/jabfm.2013.01.120107. [DOI] [PubMed] [Google Scholar]
- 21.Calvillo-King L, Arnold D, Eubank KJ, Lo M, Yunyongying P, Stieglitz H, Halm EA. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J Gen Intern Med. 2013;28(2):269–282. doi: 10.1007/s11606-012-2235-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mai Q, Holman CD, Sanfilippo FM, Emery JD, Preen DB. Mental illness related disparities in diabetes prevalence, quality of care and outcomes: a population-based longitudinal study. BMC Med. 2011;9:118. doi: 10.1186/1741-7015-9-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Druss BG, Zhao L, Cummings JR, Shim RS, Rust GS, Marcus SC. Mental comorbidity and quality of diabetes care under medicaid: A 50-state analysis. Med Care. 2012;50(5):428–33. doi: 10.1097/MLR.0b013e318245a528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Becker T, Hux J. Risk of acute complications of diabetes among people with schizophrenia in Ontario, Canada. Diabetes Care. 2011;34(2):398–402. doi: 10.2337/dc10-1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Newcomer JW. Second-generation (atypical) antipsychotics and metabolic effects: a comprehensive literature review. CNS Drugs. 2005;19(1):1–93. doi: 10.2165/00023210-200519001-00001. [DOI] [PubMed] [Google Scholar]
- 26.Lipscombe LL, Levesque L, Gruneir A, Fischer HD, Juurlink DN, Gill SS, et al. Antipsychotic drugs and hyperglycemia in older patients with diabetes. Arch Intern Med. 2009;169(14):1282–9. doi: 10.1001/archinternmed.2009.207. [DOI] [PubMed] [Google Scholar]
- 27.Kreyenbuhl J, Dickerson FB, Medoff DR, Brown CH, Goldberg RW, Fang L, et al. Extent and management of cardiovascular risk factors in patients with type 2 diabetes and serious mental illness. J Nerv Ment Dis. 2006;194(6):404–10. doi: 10.1097/01.nmd.0000221177.51089.7d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Himelhoch S, Leith J, Goldberg R, Kreyenbuhl J, Medoff D, Dixon L. Care and management of cardiovascular risk factors among individuals with schizophrenia and type 2 diabetes who smoke. Gen Hosp Psychiatry. 2009;31(1):30–2. doi: 10.1016/j.genhosppsych.2008.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chwastiak LA, Rosenheck RA, Kazis LE. Utilization of primary care by veterans with psychiatric illness in the National Department of Veterans Affairs Health Care System. J Gen Intern Med. 2008;23(11):1835–40. doi: 10.1007/s11606-008-0786-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Daumit GL, Pronovost PJ, Anthony CB, Guallar E, Steinwachs DM, Ford DE. Adverse events during medical and surgical hospitalizations for persons with schizophrenia. Arch Gen Psychiatry. 2006;63:267–272. doi: 10.1001/archpsyc.63.3.267. [DOI] [PubMed] [Google Scholar]
- 31.Daratha KB, Barbosa-Leiker C, M HB, Short R, Layton ME, McPherson S, et al. Co-occurring mood disorders among hospitalized patients and risk for subsequent medical hospitalization. Gen Hosp Psychiatry. 2012;34(5):500–5. doi: 10.1016/j.genhosppsych.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 32.Marcantonio ER, McKean S, Goldfinger M, Kleefield S, Yurkofsky M, Brennan TA. Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan. Am J Med. 1999;107(1):13–7. doi: 10.1016/s0002-9343(99)00159-x. [DOI] [PubMed] [Google Scholar]
- 33.Albrecht JS, Hirshon JM, Goldberg R, Langenberg P, Day HR, Morgan DJ, et al. Serious mental illness and acute hospital readmission in diabetic patients. Am J Med Qual. 2012;27(6):503–8. doi: 10.1177/1062860612436576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand SL, Manderscheid RW, Walters EE, Zaslavsky AM. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 35.Parks J, Svedsen D, Singer P, Foti ME, editors. Morbidity and Mortality in Persons with Serious Mental Illness. National Association of State Mental Health Program Directors Council; Alexandria VA: 2006. [Google Scholar]
- 36.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 37.Agency for Healthcare Research and Quality . Healthcare Cost and Utilization Project, Nationwide Inpatient Sample. Center for Delivery Organization and Markets; 2008. [Google Scholar]
- 38.Krumholz HM, Parent EM, Tu N, et al. Readmission after hospitalization for congestive heart failure. Arch Intern Med. 1997;157:99–104. [PubMed] [Google Scholar]
- 39.Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004;141:S33–S36. doi: 10.7326/0003-4819-141-7-200410050-00009. [DOI] [PubMed] [Google Scholar]
- 40.Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. 1999;281:613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 41.Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2007;64(5):543–52. doi: 10.1001/archpsyc.64.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Saha S, Chant D, Welham J, McGrath J. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005;2(5):e141. doi: 10.1371/journal.pmed.0020141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ramaswamy K, Kozma CM, Nasrallah H. Risk of diabetic ketoacidosis after exposure to risperidone or olanzapine. Drug Saf. 2007;30(7):589–99. doi: 10.2165/00002018-200730070-00004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.