Abstract
Background
The unmet needs of cancer survivors in rural, remote, and aboriginal communities are largely unexplored. We explored potential differences between rural survivors (rss) in 4 general population (gp) and 4 First Nations (fn) communities.
Methods
We approached 4 gp and 4 fn rs communities to participate in a mixed-methods project. Participants completed the Hospital Anxiety and Depression Scale (hads) and the Survivor Unmet Needs Survey (suns) and provided demographic information. Each question on the suns can be scored from 0 to 4, with 0 representing “no unmet need” and 4 representing “very high unmet need.” A directed approach to content analysis of focus group and interview data was used to triangulate the hads and suns results.
Results
We prospectively accrued 23 fn rss and 56 gp rss for this study. More fn rss had borderline or abnormal anxiety (5% vs. 21%, p = 0.02). Compared with gp rss, fn rss had higher unmet needs scores in all categories: Information (2.29 vs. 0.8, p < 0.001), Work and Financial (1.66 vs. 0.5, p < 0.001), Access and Continuity of Health Care (1.83 vs. 0.44, p < 0.001), Coping and Sharing (2.22 vs. 0.62, p < 0.001), and Emotional (2.12 vs. 0.63, p < 0.001). The qualitative findings provided examples and insight into the unmet needs experienced by rss.
Conclusions
First Nations rss had significantly higher anxiety and unmet needs compared with their gp rs counterparts. In addition, different qualitative themes were identified in the groups. Our findings support the development of tailored approaches to survivorship for these populations.
Keywords: Survivorship, aboriginal, First Nations, rural, remote, unmet needs
1. INTRODUCTION
Globally, cancer survivors are estimated to number 25 million, a population that continues to increase as survival rates for many cancers continue to improve 1,2. Despite the estimated 20% of Canadian cancer survivors residing in rural areas 3, nearly all cancer survivorship research has focused on people and programs in urban areas 4. A large body of literature demonstrates that individuals living in rural areas have unique challenges in accessing health care, and it is therefore anticipated that cancer survivors living in rural locations also face unique challenges 5–7.
The primary objective of our prospective community-based research is to identify the unmet needs of rural survivors (rss) in northern British Columbia, including psychosocial health needs as advocated by reports from the U.S. Institute of Medicine 8,9. At more than 600,000 km2, northern British Columbia is roughly the size of France—although more sparsely populated, with approximately 300,000 residents. Northern British Columbia also has the highest First Nations (fn)a population in the province, consisting of 54 rural and remote communities that are accessible mainly by unpaved logging roads or air. A long history of colonization, residential school experiences, and reported incidences of culturally inappropriate care have resulted in this population not accessing the health care system early in the disease trajectory 11,12. For those reasons, our research was inclusive of both a general (gp) and a fn population. Our ultimate goal is to develop cancer survivorship programs and care plans 13 for the people of northern British Columbia, and we therefore deliberately sought opinions both from fn and from s to establish whether unique approaches should be taken for these different communities.
2. METHODS
The research team deployed a mixed-methods approach to appropriately triangulate results. The Research Ethics boards of the University of British Columbia, the BC Cancer Agency, and the Northern Health Authority approved the study.
2.1. Participants
To accommodate community-level dynamics and to remain culturally appropriate, different methods were used to recruit gp rss and fn rss, as described next.
2.1.1. GP Survivors
The gp rss were recruited from 4 small rural communities dispersed throughout northern British Columbia (Table i). None of the gp rs communities were considered remote, and in fact, all had access to chemotherapy services within the community. The rss were eligible if they were 19 years of age or older, had completed active anticancer treatment within the past 0–60 months, and were not receiving follow-up care from a tertiary cancer centre. Participants were recruited using passive methods including posters, flyers, and the snowball method.
TABLE I.
Community characteristics
| Characteristic |
Community
|
|
|---|---|---|
| General population | First Nations | |
| Population | ||
| Mean | 7,899 | 2,312 |
| Range | 4,064–11,320 | 170–5,800 |
| Distance (km) to | ||
| Nearest chemotherapy facilitya | ||
| Mean | –b | 254 |
| Range | 73–470 | |
| Regional oncology clinic (Prince George)a,c | ||
| Mean | 362 | 490 |
| Range | 98–573 | 355–695 |
| Tertiary cancer centre (Vancouver or Edmonton)a,c | ||
| Mean | 994 | 1270 |
| Range | 591–1355 | 1135–1475 |
Several First Nations communities cannot travel by road to regional or tertiary centres at various times of the year.
Present in all 4 communities.
At the time of the study, a full-service tertiary cancer centre was under construction in Prince George.
2.1.2. FN Survivors
The fn rss were recruited from 4 northern regions that had expressed interest in participating in the project and that had a pre-existing relationship with members of the research team. All fn communities were more remote than the gp rs communities, demonstrated by a lack of access to chemotherapy within the community (Table i), and in fact, several did not have full-time access to a physician. The fn communities selected for inclusion represent a number of language groups with various geographic challenges in accessing supportive care services.
As is culturally appropriate in northern British Columbia, meetings were first held with chief and council. Based on their recommendations, meetings were then held with either elders or community members at large. Community-based research assistants invited fn rss to participate based on the inclusion criteria already indicated.
2.2. Materials and Procedures—All Communities
Participants were mailed a study package before qualitative data were collected. The package contained a letter of introduction to the study, the consent form, the Survivor Unmet Needs Survey (suns), and the Hospital Anxiety and Depression Scale (hads). Arrangements were then made for participants to take part in a focus group or an individual interview.
Interview and focus group questions were semi-structured and focused on medical review, medical surveillance, adjustment and coping strategies, healthy living guidelines, information needs, and resource availability and needs. All interviews and focus groups were digitally recorded and transcribed verbatim. The 7 focus groups and 10 individual interviews with 56 gp rss and 23 fn rss were scheduled depending on the preferences of the individuals and communities. All interviews with fn rss were conducted in person; 8 interviews with gp rss were conducted by telephone to accommodate individual schedules and needs.
2.3. Measures
Most of the gp rss (96%) and fn rss (91%) who were interviewed or took part in focus groups also completed and returned the hads and suns questionnaires. The hads is a validated and reliable 14-item scale, divided into 2 subscales: Anxiety and Depression 14,15. The suns is a validated 89-item survey, divided into 5 subscales: Information, Financial Concerns, Access and Continuity of Care, Relationships, and Emotional Health. Scores for each suns question ranges from 0 (“no unmet need”) to 4 (“very high unmet need”) 16,17. Both instruments are self-report questionnaires.
2.4. Analysis
Quantitative analyses, including descriptive statistics, used the Statistical Package for the Social Sciences (version 14.0: SPSS, Chicago, IL, U.S.A.). The 5 suns subscales were used to guide the qualitative directed-content analysis. The Relationships and Emotional Health subscales were combined in the qualitative analysis, a choice that is supported by the high correlation between those subscales in the original development of the suns 16. A directed approach to content analysis is appropriate when earlier research can guide the analysis and discussion of findings 18. The qualitative data were coded using the NVivo 10 software program (QSR International, Doncaster, Australia) and were grouped according to the suns subscales. Within each subscale, important concepts, ideas, events, and experiences common and unique to the gp and fn rss were identified and compared. Qualitative findings that provided insight into and illustrated the unique experiences and needs of the study participants were then summarized according to the quantitative findings as a means of data triangulation 19.
3. RESULTS
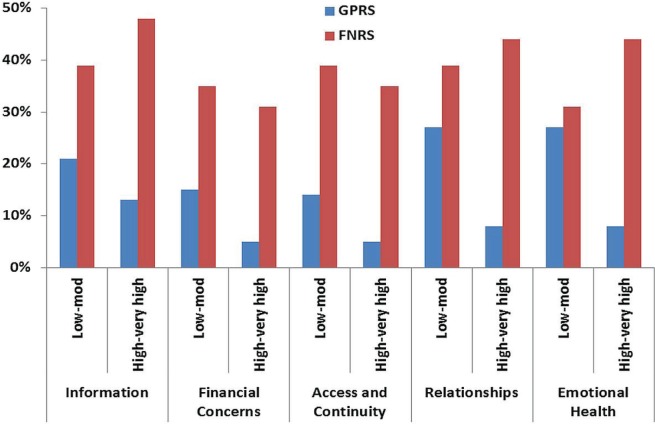
Table i presents the characteristics of the 8 participating communities, and Table ii presents participant characteristics. In all domains of the suns, higher unmet needs were reported by fn rss than by their gp rs counterparts (Table iii, Figure 1).
TABLE II.
Participant characteristics and scores on the Hospital Anxiety and Depression Scale (hads)
| Characteristic |
Rural survivor group
|
p Value | ||
|---|---|---|---|---|
| General population | First Nations | |||
| Participants (n) | 56 | 23 | ||
| Sex [n (%) women] | 49 (88) | 14 (61) | 0.01 | |
| Age (years) | ||||
| Mean | 59 | 55 | 0.30 | |
| Range | 33–83 | 21–81 | ||
| Most recent cancer diagnosis [n (%)] | ||||
| Breast cancer | 39 (70) | 8 (35) | 0.16 | |
| Colorectal cancer | 3 (5) | 5 (22) | ||
| Lymphoma | 3 (5) | 3 (13) | ||
| Gynecologic cancer | 7 (13) | 5 (22) | ||
| Other | 4 (7) | 2 (9) | ||
| hads score [n (%)] | ||||
| Anxiety | Normal | 43 (80) | 10 (48) | 0.02 |
| Borderline | 7 (13) | 6 (29) | ||
| Abnormal | 4 (8) | 5 (24) | ||
| Depression | Normal | 50 (93) | 19 (91) | 0.42 |
| Borderline | 2 (4) | 2 (10) | ||
| Abnormal | 2 (4) | 0 | ||
TABLE III.
Mean score on the Survivors Unmet Needs Survey (suns), by category
| suns domain of unmet need |
Rural survivor group
|
p Value | |
|---|---|---|---|
| General population | First Nations | ||
| Information | 0.80 | 2.29 | <0.001 |
| Financial concerns | 0.50 | 1.66 | <0.001 |
| Access and continuity of care | 0.44 | 1.83 | <0.001 |
| Relationships | 0.62 | 2.22 | <0.001 |
| Emotional health | 0.63 | 2.12 | <0.001 |
FIGURE 1.
Unmet needs results for rural survivors, by category. gp rs = general population rural survivors; fn rs = First Nations rural survivors.
Qualitatively, rss described unmet needs in all 5 suns subscales (Table iii). Several unmet needs were common to both gp and fn rss. However, both populations had some unique unmet needs.
3.1. Informational Unmet Needs
The gp and fn rss had similar difficulties accessing medical and supportive care information after treatment:
The information wasn’t helpful. I couldn’t find what I was looking for. I couldn’t find if [it] was it a side effect. For me, it was horrendous.
However, fn rss encountered additional barriers to accessing desired information, related to obtaining and comprehending information, as highlighted by these quotes:
Lack of the access to the Internet is frustrating.
And some of our people up here may not be able to read [the] information [given]. I would say [because] of the education.
The fn rss also emphasized their need for information to share with family members, not only so that family could understood the challenges facing survivors, but also to help the family members cope with their own anxieties. Survivors considered this information to be lacking, as evidenced in this quote:
[I] need information for the children in the family. Like, my mother needed the information just as much as I did, and my daughter, I know, needed the information, but it has to be at her level.
3.2. Financial Unmet Needs
The gp and fn rss reported similar unmet financial needs on the suns, although qualitatively, they described different financial concerns. Compared with fn rss, gp rss more commonly described financial constraints related to loss of employment. Both groups described frustrations with the cost of travel:
They call you back for a follow-up appointment in Vancouver, and it costs you a lot of money to fly down, stay overnight, and come back. We were so broke. I had to scrape up the money for gas. It’s a four-day trip, and I can’t, I don’t have the money.
The gp rss also more commonly described expenses as a barrier to accessing supportive care services such as counselling, rehabilitation, and breast prostheses:
And then there’s special bras, there’s the prosthesis, and then there’s the travel. But, we are in the north, and so I kind of accept that we can’t have everything up here.
The fn rs did not attribute finances as a barrier to supportive care services; rather, they described the challenge of working through multiple levels of bureaucracy to access financial support. They also portrayed their reliance on their community for financial support as problematic at times because of discrepancies or disagreements between survivors and band members, as evidenced in these quotes:
[The] band hasn’t really helped me. They did for the weekend once, when I first came here. [Chief’s name] said okay to that, but never paid nothing into my health. They’ve never helped me moneywise.
We got our own room because [the band] health wouldn’t cover it because they said I should wait until the [community oncology clinic] was available to take me in. I just went to Prince George anyways and covered the cost myself.
3.3. Access and Continuity of Care Unmet Needs
Both populations described difficulty in access to and continuity of medical and supportive care, often related to the need to travel great distances in treacherous weather conditions. Multiple gp rss highlighted a discrepancy between services that were promised and those that actually existed. They perceived that their follow-up care was managed by their family physician in isolation, and they would prefer a team approach:
All the little brochures that I got, it always talked about this team of people that would be helping me. And there was nobody except my family doctor. In the cancer brochures it says, I think, there’s about four or five people it says that would help.
The gp and fn rss also described a similar disconnect between specialist and follow-up care provided closer to home, as exemplified by one gp rs:
I think there is kind of a disconnect between the actual care of specialists. And then when you come home, and you’re a lot of miles away from the doctor who gave you, or the specialist that gave you, treatment.
The fn rss expressed additional concerns about the quality of their follow-up care:
I would like to have known what doctors are good with cancer patients. Like, the general doctors, I’m finding frustrating. I’m just not comfortable going with my regular doctor now because of some of the things that happened when I was going through this.
Furthermore, accessing even basic medical and supportive care, such as a family physician or home care, was problematic for several fn rss:
The barriers would be the doctors. They’re not here when I need them. And I know there was a week we had without doctors, period. And that was—I thought—was important because I needed the refill of my medication.
And sometimes they [nurses] would show up, or else they would show up too late and then they couldn’t give me the needle. So it got to the point where I just couldn’t rely on them, and I just had to start doing it myself.
3.4. Relationships and Emotional Unmet Needs
Remote video psychosocial support is available for rss in northern British Columbia through the Northern Health Authority, operated out of Prince George. However, many rss in both gp and fn communities were unaware of this service, and identified psychosocial support as an unmet need:
There were no services, there’s no support group, there’s no counselling for people. Health care providers and support staff stated that they didn’t have training for [providing emotional support] ... or [for helping] people that are dealing with these types of emotions that illness causes. — gp rs
Th gp rss who were aware of remote counselling services would have preferred access to in-person counselling. Compared with the gp rss, fewer fn rss described opportunities for connecting with other survivors. They also highlighted a significant unmet need for peer and professional support for family members:
Counsellors available for you, your family, and your children.... Honestly I don’t think my mom ever really chatted with anyone yet.
4. DISCUSSION
This community-based research project identified many categories of unmet needs for survivors living in rural communities in northern British Columbia. As anticipated, access to specialists and to survivor services were common unmet needs reported by gp and fn rss alike. However, multiple differences in unmet needs were evident for rss from gp and fn communities, suggesting that unique approaches to survivorship care for these populations are warranted. In addition, fn rss reported significantly higher levels of unmet need in all categories collected, indicating that this population is most in need of improvement in survivorship care.
We hypothesize that the more profound remoteness of the fn communities (compared with the gp communities) might in part explain the differences found. For example, the presence of a general practitioner with experience in caring for cancer patients and giving chemotherapy probably improves the coordination of cancer survivorship in the gp communities, where those physicians would serve as a reference for the family physicians of the patients. The hiring of such physicians into the small fn communities is unlikely, but perhaps future work could focus on connecting those physicians (or oncologists) to other health care providers in fn communities, potentially through the use of video technology or novel electronic communication (such as electronic medical record messaging). It is possible that fn rss had higher anxiety as a result of not having access to a physician experienced with cancer care and follow-up in their community, but our study was not able to assess that possibility directly. The remoteness of the fn communities might explain some of the differences, but we also anticipate that a lack of cultural awareness on the part of health care practitioners might also explain some of the unique unmet needs described by the fn survivors. We therefore believe that some important steps specific to fn rss should be pursued, including competency training in indigenous cultures (for example, http://www.culturalcompetency.ca), care plans that are culturally appropriate (for example, through discussion of fn diets and natural health care practices), and navigation programs run by individuals familiar with the challenges faced by particular communities.
Research on rss in the Canadian context with which to compare the present study has been limited. In 2006, an Ontario group of researchers conducted focus groups with breast cancer survivors in “rural” Canadian locations, identifying difficulty accessing health care information, support, and services as the main concerns 4. However, it is important to note that these women self-identified as “rural” residents (though half lived within 1 hour of a surgical centre), suggesting that the study findings represented the concerns of women living in a more urban context than was the norm in the current study 4. To the best of our knowledge, other Canadian rs research is limited to piloting support programs for survivors living in rural locations20,21. We are not aware of any Canadian research on the survivorship experience of fn or other aboriginal peoples, although important work in rural palliative care has been conducted in Canada 22.
The current findings are consistent with research from Australia, where rural, remote, and indigenous populations have difficulties with health care access (encompassing availability, geography, affordability, accommodation, timeliness, acceptability, and culturally appropriate care) that are similar to those experienced by gp and fn Canadian populations living in rural and remote locations 23. Several research teams have demonstrated that Australian patients on active treatment have difficulties accessing care and finding support, and have high levels of unmet needs, especially in the psychological domain 24–26. As did rss in the present study, Australian rss described gaps in care upon return to their home communities, difficulty with accessing tertiary follow-up and support services, and perceptions of a lack in coordination between specialists and rural primary care providers 27–29.
Our study should be interpreted in the context of its strengths and limitations. Despite the strong community buy-in for this research project, the small populations of the 8 communities meant that the sample size was relatively small, limiting analysis and interpretation. In addition, the study design is susceptible to selection bias, in which patients with particular traits might be overrepresented. Also, the differences in demographics between the fn and gp communities (Table i) make it difficult to draw conclusions about the differences between the communities. Ancestral background should certainly not be interpreted as causal of any differences found or described between the communities. However, the purposeful inclusion of rural, remote, and fn communities, although limited by the small sample, brings a rich qualitative insight into the experiences of northern British Columbian survivors.
5. FURTHER STEPS
Our analysis has led to the development, for both gp and fn rss, of unique survivorship care plans that are currently being evaluated in the same 8 communities. In addition, an aboriginal cancer care strategy has been developed through a partnership between Northern Health and the BC Cancer Agency. Furthermore, an aboriginal care coordinator has been hired at the BC Cancer Agency Centre for the North. We therefore anticipate that the unmet needs identified in the current study are less problematic since those changes were implemented, but future research is aimed at assessing the changes. Future research is also focused on improving the communication and sharing of care between oncologists and family physicians, partially through novel electronic methods.
6. CONCLUSIONS
Cancer survivors living in rural communities of northern British Columbia have unique unmet needs. The gp and fn survivors all expressed a need for the health care system to provide tailored survivorship care suited to their rural situation, and for improvements in communication and coordination between specialists and primary care providers. However, there were differences in the challenges and needs described by the two groups of survivors, suggesting that distinct approaches to the communities are warranted. The fn survivors had consistently higher unmet needs in all categories assessed, suggesting that this population is most in need of improvements in cancer survivorship care.
7. ACKNOWLEDGMENTS
This study was funded by the Public Health Agency of Canada and the Northern Health Authority. FH holds a Research Trainee – Post-Doctoral Fellowship Award from the Michael Smith Foundation for Health Research.
The principal investigators were RAO and AW. CZ and KT facilitated the gp rs interviews, and PT facilitated the fn rs interviews. FH lead the qualitative analysis, which was performed by FH, KT, DM, and RAO. RAO and FH performed the quantitative analyses. All authors reviewed and provided critical feedback to the manuscript.
Footnotes
It is understood that the aboriginal population in Canada refers to First Nations, Metis, and Inuit. Our study was conducted specifically with First Nations, considered by Statistics Canada to be individuals with membership in a First Nation or Indian Band as outlined within the 198510 amendment to the Indian Act of Canada (Bill C-31) or a person who identifies as being a member of a First Nation, not necessarily indicating a person who is considered a registered or unregistered Status Indian or non-Status Indian.
8. CONFLICT OF INTEREST DISCLOSURES
No financial conflicts of interest were declared by any of the authors.
9. REFERENCES
- 1.Coleman M, Forman D, Bryant H, et al. on behalf of the icbp Module 1 Working Group Cancer survival in Australia, Canada, Denmark, Norway, Sweden, and the UK, 1995–2007 (the International Cancer Benchmarking Partnership): an analysis of population-based cancer registry data. Lancet. 2011;377:127–38. doi: 10.1016/S0140-6736(10)62231-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boyle P, Levin B. World Cancer Report 2008. Lyon, France: International Agency for Research on Cancer; 2008. [Google Scholar]
- 3.Employment and Social Development Canada Home > Well-being Home > Canadians in Context > Geographic Distribution > Canadians in Context – Geographic Distribution [Web page]. [Available at: http://www4.hrsdc.gc.ca/.3ndic.1t.4r@-eng.jsp?iid=34; cited May 21, 2013]
- 4.Gray RE, James P, Manthorne J, Gould J, Fitch MI. A consultation with Canadian rural women with breast cancer. Health Expect. 2004;7:40–50. doi: 10.1046/j.1369-6513.2003.00248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Olson RA, Nichol A, Caron NR, et al. Effect of community population size on breast cancer screening, stage distribution, treatment use and outcomes. Can J Public Health. 2012;103:46–52. doi: 10.1007/BF03404068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ryan–Nicholls KD. Health and sustainability of rural communities. Rural Remote Health. 2004;4:242. [PubMed] [Google Scholar]
- 7.Sibley LM, Weiner JP. An evaluation of access to health care services along the rural–urban continuum in Canada. BMC Health Serv Res. 2011;11:20. doi: 10.1186/1472-6963-11-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hewitt M, Herdman R, Holland J, on behalf of the Institute of Medicine of the National Academies, editors. Meeting Psychosocial Needs of Women with Breast Cancer. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 9.Adler NE, Page AEK, on behalf of the Institute of Medicine of the National Academies, editors. Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. Washington, DC: National Academies Press; 2008. [PubMed] [Google Scholar]
- 10.Statistics Canada Home > Definitions, data sources and methods > Aboriginal peoples survey (APS) [Web page]. [Available at: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3250&lang=en&db=imdb&adm=8&dis=2; cited May 21, 2013]
- 11.Brown HJ, McPherson G, Peterson R, Newman V, Cranmer B. Our land, our language: connecting dispossession and health equity in an indigenous context. Can J Nurs Res. 2012;44:44–63. [PubMed] [Google Scholar]
- 12.Castleden H, Crooks VA, Hanlon N, Schuurman N. Providers’ perceptions of aboriginal palliative care in British Columbia’s rural interior. Health Soc Care Community. 2010;18:483–91. doi: 10.1111/j.1365-2524.2010.00922.x. [DOI] [PubMed] [Google Scholar]
- 13.Earle CC. Long term care planning for cancer survivors: a health services research agenda. J Cancer Surviv. 2007;1:64–74. doi: 10.1007/s11764-006-0003-9. [DOI] [PubMed] [Google Scholar]
- 14.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/S0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 15.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 16.Campbell HS, Sanson–Fisher R, Turner D, Hayward L, Wang XS, Taylor–Brown J. Psychometric properties of cancer survivors’ unmet needs survey. Support Care Cancer. 2010;19:221–30. doi: 10.1007/s00520-009-0806-0. [DOI] [PubMed] [Google Scholar]
- 17.Campbell HS, Sanson–Fisher R, Taylor–Brown J, Hayward L, Wang XS, Turner D. The cancer support person’s unmet needs survey: psychometric properties. Cancer. 2009;115:3351–9. doi: 10.1002/cncr.24386. [DOI] [PubMed] [Google Scholar]
- 18.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–88. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 19.Denzin NK, Lincoln YS. Introduction: the discipline and practice of qualitative research. In: Denzin NK, Lincoln YS, editors. The Sage Handbook of Qualitative Research. 3rd ed. Thousand Oaks, CA: Sage Publications; 2005. pp. 1–30. [Google Scholar]
- 20.Stephen J, Rojubally A, Macgregor K, et al. Evaluation of CancerChatCanada: a program of online support for Canadians affected by cancer. Curr Oncol. 2013;20:39–47. doi: 10.3747/co.20.1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vallance JK, Lavallee CM, Culos–Reed NS, Trudeau MG. Physical activity is associated with clinically important differences in health-related quality of life among rural and small-town breast cancer survivors. Support Care Cancer. 2012;20:1079–87. doi: 10.1007/s00520-011-1188-7. [DOI] [PubMed] [Google Scholar]
- 22.Kelly L, Linkewich B, Cromary H, St Pierre–Hansen N, Antone I, Giles C. Palliative care of First Nations people: a qualitative study of bereaved family members. Can Fam Physician. 2009;55:394–395. e7. [Erratum in: Can Fam Physician 2009;55:590] [PMC free article] [PubMed] [Google Scholar]
- 23.Russell DJ, Humphreys JS, Ward B, et al. Helping policymakers address rural health access problems. Aust J Rural Health. 2013;21:61–71. doi: 10.1111/ajr.12023. [DOI] [PubMed] [Google Scholar]
- 24.White KJ, Roydhouse JK, D’Abrew NK, Katris P, O’Connor M, Emery L. Unmet psychological and practical needs of patients with cancer in rural and remote areas of Western Australia. Rural Remote Health. 2011;11:1784. [PubMed] [Google Scholar]
- 25.Clavarino AM, Lowe JB, Carmont SA, Balanda K. The needs of cancer patients and their families from rural and remote areas of Queensland. Aust J Rural Health. 2002;10:188–95. doi: 10.1046/j.1440-1584.2002.00436.x. [DOI] [PubMed] [Google Scholar]
- 26.Wilkes LM, White K, Mohan S, Beale B. Accessing metropolitan cancer care services: practical needs of rural families. J Psychosoc Oncol. 2006;24:85–101. doi: 10.1300/J077v24n02_06. [DOI] [PubMed] [Google Scholar]
- 27.Lawler S, Spathonis K, Masters J, Adams J, Eakin E. Follow-up care after breast cancer treatment: experiences and perceptions of service provision and provider interactions in rural Australian women. Support Care Cancer. 2011;19:1975–82. doi: 10.1007/s00520-010-1041-4. [DOI] [PubMed] [Google Scholar]
- 28.McGrath P, Patterson C, Yates P, Treloar S, Oldenburg B, Loos C. A study of postdiagnosis breast cancer concerns for women living in rural and remote Queensland. Part i: personal concerns. Aust J Rural Health. 1999;7:34–42. doi: 10.1046/j.1440-1584.1999.00214.x. [DOI] [PubMed] [Google Scholar]
- 29.McGrath P, Patterson C, Yates P, Treloar S, Oldenburg B, Loos C. A study of postdiagnosis breast cancer concerns for women living in rural and remote Queensland. Part ii: support issues. Aust J Rural Health. 1999;7:43–52. doi: 10.1046/j.1440-1584.1999.00216.x. [DOI] [PubMed] [Google Scholar]