Abstract
The alignment of a lower limb prosthesis affects the way load is transferred to the residual limb through the socket, and this load is critically important for the comfort and function of the prosthesis. Both magnitude and duration of the moment are important factors that may affect the residual limb health. Moment impulse is a well-accepted measurement that incorporates both factors via moment–time integrals. The aim of this study was to investigate the effect of alignment changes on the socket reaction moment impulse in transtibial prostheses. Ten amputees with transtibial prostheses participated in this study. The socket reaction moment impulse was measured at a self-selected walking speed using a Smart Pyramid™ in 25 alignment conditions, including a nominal alignment (clinically aligned by a prosthetist), as well as angle malalignments of 2°, 4° and 6° (abduction, adduction, extension and flexion) and translation malalignments of 5 mm, 10 mm and 15 mm (lateral, medial, anterior and posterior). The socket reaction moment impulse of the nominal alignment was compared for each condition. The relationship between the alignment and the socket reaction moment impulse was clearly observed in the coronal angle, coronal translation and sagittal translation alignment changes. However, this relationship was not evident in the sagittal angle alignment changes. The results of this study suggested that the socket reaction moment impulse could potentially serve as a valuable parameter to assist the alignment tuning process for transtibial prostheses. Further study is needed to investigate the influence of the socket reaction moment impulse on the residual limb health.
Keywords: Amputation, Direct measurement, Gait, Knee adduction moment impulse, Osteoarthritis
1. Introduction
Residual limb management, gait rehabilitation, and selection of appropriate prosthetic components as well as their alignment are important for successful lower-limb prosthetic fit. Poor prosthetic fit and alignment may lead to skin trauma of the residual limb, such as abrasions, blisters or calluses due to increased frictions and pressures at socket–residual limb interface as well as adaptive changes to gait that could result in long-term orthopedic conditions (Mak et al., 2001; Silver-Thorn et al., 1996). Because alignment affects the way load is transferred to the residual limb from the ground through the prosthetic socket, appropriately tuning the prosthetic alignment has a significant role in minimizing these risks, but it is a challenging procedure for both prosthetists and amputees (Boone et al., 2012; Zahedi et al., 1986).
The alignment of transtibial prostheses represents two actions performed by the prosthetists: the measurement and adjustment of the spatial position of the socket relative to the foot. The process of alignment takes into account both static balance and dynamic function in an iterative process of improvement. The prosthetic alignment is tuned to maintain balance achieved by counteracting the tendency of the socket to rotate around the residual limb (Fernie, 1981). In bench alignment of the transtibial prosthesis, the center of posterior brim of the socket is generally positioned 1.3 cm lateral to the center of the heel of the foot (Berger and Fishman, 1997). This bench alignment tends to create an external varus moment that results in decreased compression over the head of fibula and the superficial passage of the peroneal nerve. This moment also helps amputees to maintain trunk stability without unnecessary lateral bending during stance on the prosthetic leg.
Prosthetic socket–residual limb interface load is critically important for the comfort and function of the prosthesis and the socket–residual limb interface pressures have been studied extensively (Beil et al., 2002; Dou et al., 2006; Sanders et al., 2005; Yeung et al., 2013). Since direction and magnitude of load transmission to the residual limb is influenced by the alignment, clinicians need to understand the relationship among the load, alignment and prosthetic fit. Load on the residual limb while walking can be measured directly by attaching a kinetic sensor on the prosthesis (Boone et al., 2013; Frossard et al., 2003; Kobayashi et al., 2013a; Neumann et al., 2013; Sanders et al., 1997; Schwarze et al., 2013) or indirectly using a motion capture system with force plates (Dumas et al., 2009; Frossard et al., 2011; Stephenson and Seedhom, 2002). Direct measurement allows quantification of the load on the residual limb across multiple gait cycles outside of a gait laboratory and is generally expected to be more feasible for in-clinic use.
Joint angular or moment impulse is a measurement that incorporates both the magnitude of moment and its duration time (moment–time integrals). Knee adduction (varus) angular or moment impulse has been commonly used as a parameter to assess gait in patients with knee osteoarthritis (Fantini Pagani et al., 2010; Hinman et al., 2012; Kean et al., 2013; Kito et al., 2010; Thorp et al., 2006). It has been used to study the effect of an orthotic intervention in this patient group. A significant reduction in the knee adduction moment impulse was reported with the use of a lateral wedge shoe insole or a knee orthosis in patients with knee osteoarthritis (Fantini Pagani et al., 2010; Hinman et al., 2012; Jones et al., 2013).
Alignment of the knee joint in the coronal plane has been shown to affect the knee adduction moment impulse. Comparison of the effect of the alignment (4° and 8°) in a valgus knee orthosis revealed 25% and 36% reductions in the knee adduction moment impulse, respectively (Fantini Pagani et al., 2010). Surgical realignment (valgus osteotomy) in the coronal plane of the knee in patients with knee osteoarthritis also induced a significant decrease in the knee adduction moment impulse (Leitch et al., 2013). The knee adduction moment impulse could also distinguish the severity of malalignment in patients with knee osteoarthritis (Kean et al., 2012). Both magnitude and duration of the moment are anticipated to be important factors that affect skin and joint conditions of the residual limb and consequently gait deviations and pathology. Therefore, the moment impulse may also serve as a valuable measurement parameter to investigate the effect of prosthetic alignment on the residual limb while walking.
Socket reaction moments are moments acting about the geometric center of the socket and transferred through the prosthesis at the distal end of the socket while walking and represent how a residual limb inside the socket is loaded (Kobayashi et al., 2012). Prosthetic alignment changes have a systematic effect on the socket reaction moments in amputees with transtibial prostheses (Boone et al., 2013; Kobayashi et al., 2014; Kobayashi et al., 2013b) and amputees with transfemoral or knee-disarticulation prostheses (Kobayashi et al., 2013a). Therefore, the prosthetic alignment changes should also have a similar effect on the socket reaction moment impulse (socket reaction moment–time integrals). Understanding the effect of prosthetic alignment on the residual limb through the socket reaction moment impulse may potentially provide additional information for evidence-based management and help guide the care of the amputees. The aim of this study was to investigate the in-plane effects of alignment changes on the socket reaction moment impulse (i.e. effects of alignment changes on the socket reaction moment impulse in the same plane) in transtibial prostheses. It was hypothesized that alignment changes have significant in-plane effects on the socket reaction moment impulse.
2. Method
2.1. Subjects
Ten individuals with transtibial prostheses (50 ± 11 years old; 4 females/6 males) participated from the community (Table 1). The mean height of the participants was 1.74 ± 0.08 m, while the mean mass was 84 ± 18 kg. All subjects used energy storage and return feet for their prostheses. The cause of amputation was trauma in 9 subjects and peripheral vascular disease in 1 subject. This study was approved by an institutional review board governing the institution, and informed consent was obtained from each subject.
Table 1.
Demographic information of the subjects with transtibial amputation.
| Subject | AGE (year-old) | Gender | Amputated side | Height (m) | Mass (kg) | Time since amputation (years) | Residual limb length (m) | Prosthetic foot |
|---|---|---|---|---|---|---|---|---|
| A | 46 | M | L | 1.85 | 85 | 6 | 0.18 | Multiflex foot |
| B | 53 | M | L | 1.85 | 93 | 9 | 0.13 | Flex walk |
| C | 70 | M | L | 1.78 | 83 | 48 | 0.16 | Seattle light foot |
| D | 50 | F | R | 1.64 | 63 | 18 | 0.13 | Seattle voyager foot |
| E | 64 | F | R | 1.75 | 64 | 32 | 0.13 | Seattle carbon light |
| F | 45 | M | R | 1.83 | 101 | 20 | 0.14 | Cadence HP |
| G | 35 | M | L | 1.73 | 75 | 15 | 0.13 | Seattle catalyst foot |
| H | 49 | F | L | 1.65 | 112 | 9 | 0.14 | Century 22 adjustable heel height foot |
| I | 35 | F | L | 1.63 | 62 | 12 | 0.16 | Renegade low profile |
| J | 51 | M | R | 1.73 | 98 | 1 | 0.20 | Seattle light foot |
| Mean (SD) | 50 (11) | – | – | 1.74 (0.08) | 84 (18) | 17 (14) | 0.15 (0.02) | – |
Abbreviations: F: female, M: male, L: left, R: right, SD: standard deviation.
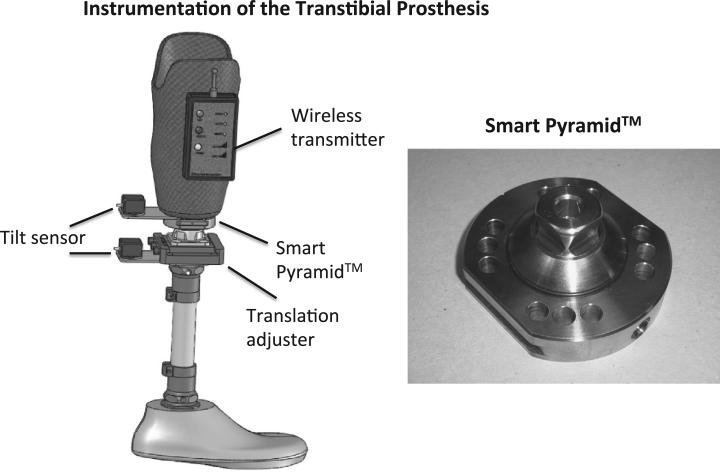
2.2. Apparatus
A Smart Pyramid™ (currently known as Europa™) (Height: 3.22 cm; Mass: 0.14 kg) (Orthocare Innovations, Mountlake Terrace, WA, USA) was used to quantify the socket reaction moment impulse (Kobayashi et al., 2014) (Fig. 1). The Smart Pyramid is an instrumented prosthetic pyramid adapter that is attached at the base of the socket. It can measure the socket reaction moments in the sagittal and coronal plane. The Smart Pyramid collects data at the sampling frequency of 100 Hz and sends them wirelessly to a computer using Bluetooth for further analysis. The moment measured by the Smart Pyramid was highly linear with coefficients of determination of R2 = 0.998 for the sagittal moment and R2 = 0.996 for the coronal moment. The sagittal moment measured by the Smart Pyramid revealed a root mean square error of 2.08% and coronal moments at 2.80% (Kobayashi et al., 2013a). A biaxial MEMS tilt sensor (CXT-02, Crossbow Technologies, San Jose, Germany) was used to adjust angle alignment changes, while a millimeter scale on a translation adjuster (10A40/A, F.G. Streifeneder KG, Emmering, Germany) (Boone et al., 2013) was used to adjust translation alignment changes (Fig. 1).
Fig. 1.
Instrumentation of the transtibial prosthesis and Smart Pyramid™.
2.3. Protocol
The Smart Pyramid was attached to the base of the socket of each participant's prosthesis that was used in daily life. Fitting of the socket was checked prior to the study to make sure the fit was appropriate. The orientation of the pyramid in the transverse plane was established so that it was aligned with the line of progression, and this accounted for the typical external foot progression angle. The alignment of the prosthesis was adjusted until it was satisfactory to both the investigator prosthetist and the amputee. This alignment was considered as a nominal alignment. From this nominal alignment, the alignment of the prosthesis was randomly changed by 2°, 4° and 6° (abduction, adduction, extension and flexion) in angles and 5 mm, 10 mm and 15 mm (lateral, medial, anterior and posterior) in translations in a random order. The alignment changes are described as a spatial relationship of the moving foot relative to the nominal alignment with the socket fixed in space. Twenty-five alignment (1 nominally-aligned and 24 malaligned) conditions were tested in this study. During the data collection, participants were advised to walk down a 10-meter path at a self-selected walking speed immediately after the alignment was adjusted according to a current clinical alignment adjustment procedure.
2.4. Data analysis
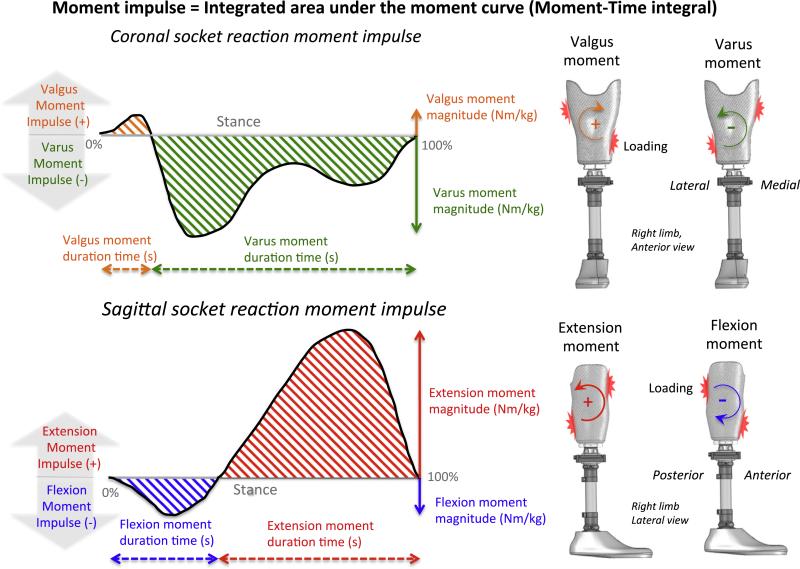
The socket reaction moment impulse (Nm·s/kg) was calculated by integrating the area under the socket reaction moment curve (normalized to body mass) during stance according to the method used to calculate the joint moment impulse in previous studies (Jones et al., 2013; Kito et al., 2010) (Fig. 2). Stance duration time was also used to ensure that gait speed was not affected by alignment changes. The socket reaction moment impulse was calculated using data from 3 steps in the middle of each walking trial. The flexion (extension) socket reaction moment impulse was calculated by integrating the area under the normalized flexion (extension) socket reaction moment across the stance duration time of the flexion (extension) socket reaction moment in the sagittal plane. The flexion socket reaction moment impulse occurs while distal anterior and proximal posterior aspects of the residual limb are generally loaded, while the extension socket reaction moment impulse occurs while proximal anterior and distal posterior aspects of the residual limb are generally loaded (Fig. 2). The varus (valgus) socket reaction moment impulse was calculated by integrating the area under the normalized varus (valgus) socket reaction moment across the stance duration time of the varus (valgus) socket reaction moment in the coronal plane. The varus socket reaction moment impulse occurs while proximal medial and distal lateral aspects of the residual limb are generally loaded, while the valgus moment impulse occurs while proximal lateral and distal medial aspects of the residual limb are generally loaded (Fig. 2). An extension socket reaction moment impulse in the sagittal plane and a valgus socket reaction moment impulse in the coronal plane were defined as positive.
Fig. 2.
Description of socket reaction moment impulse. For the coronal socket reaction moment impulse, the valgus socket reaction moment impulse (valgus moment impulse) is presented in orange, while the varus socket reaction moment impulse (varus moment impulse) is presented in green. For the sagittal socket reaction moment impulse, the extension socket reaction moment impulse (extension moment impulse) is presented in red, while the flexion socket reaction moment impulse (flexion moment impulse) is presented in blue. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
2.5. Statistical analysis
The effect of the alignment changes on the socket reaction moment impulse and the stance duration time were statistically analyzed. The socket reaction moment impulse and stance duration time of the nominally aligned condition was compared to each of the malaligned conditions using a 2-tailed paired t-test with Stata/IC 11.1 (STATA Corp, College Station, USA). No statistical comparisons were made between malaligned conditions. Means, standard deviations and 95% confidence intervals of the socket reaction moment impulse and stance duration time were calculated. Statistical significance was set at an α = 0.05, and P-values were adjusted for multiple comparisons using the Tukey–Ciminera–Heyse procedure (Sankoh et al., 1997; Tukey et al., 1985).
3. Results
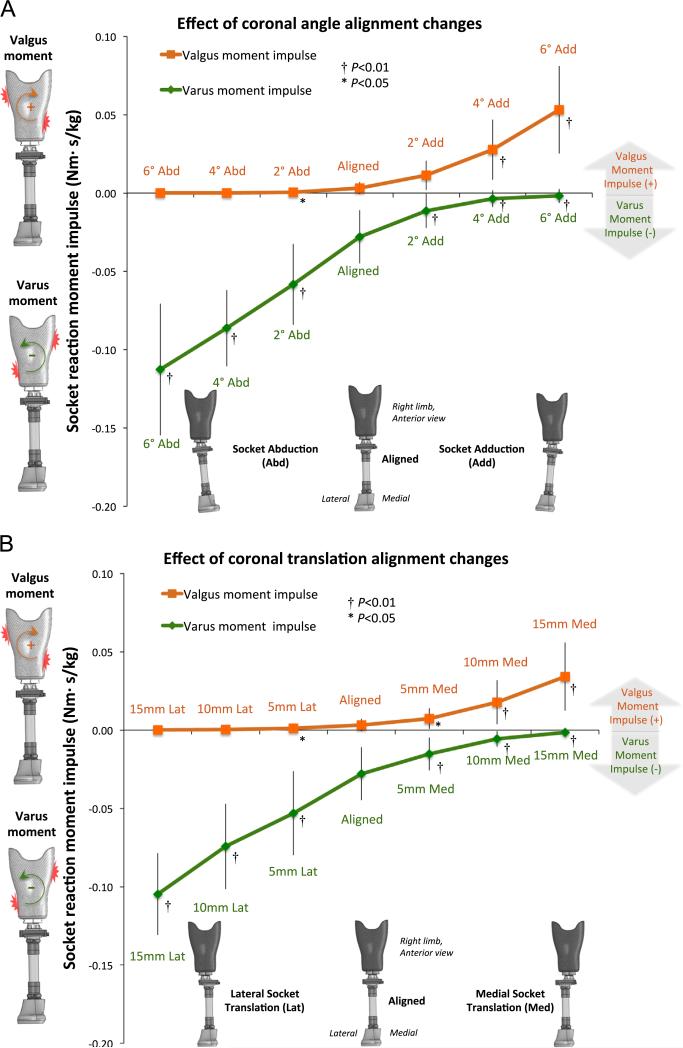
3.1. Effect of coronal alignment changes on the coronal socket reaction moment impulse
Both angle and translation alignment changes induced significant differences at all malaligned conditions for the varus socket reaction moment impulse and at some malaligned conditions for the valgus socket reaction moment impulse in comparison to the nominally aligned condition (Table 2; Fig. 3).
Table 2.
Effect of sagittal and coronal alignment changes on socket reaction moment impulse.
| Alignment changes | Valgus moment impulse (Nm·s/kg) |
Varus moment impulse (Nm·s/kg) |
||
|---|---|---|---|---|
| Mean (SD) | 95% CI | Mean (SD) | 95% CI | |
| Coronal Angle | ||||
| 6° Abd | 0.0001 (0.0002) | –0.0001, 0.0002 | –0.1126 (0.0421)† | –0.1427, –0.0825 |
| 4° Abd | 0.0001 (0.0002) | –0.0001, 0.0002 | –0.0863 (0.0243)† | –0.1037, –0.0689 |
| 2° Abd | 0.0006 (0.0010)* | –0.0002, 0.0013 | –0.0583 (0.0258)† | –0.0768, –0.0398 |
| Aligned | 0.0032 (0.0039) | 0.0005, 0.0060 | –0.0279 (0.0169) | –0.0400, –0.0159 |
| 2° Add | 0.0113 (0.0093) | 0.0046, 0.0180 | –0.0114 (0.0109)† | –0.0192, –0.0036 |
| 4° Add | 0.0277 (0.0191)† | 0.0140, 0.0414 | –0.0036 (0.0054)† | –0.0075, 0.0002 |
| 6° Add | 0.0532 (0.0279)† | 0.0332, 0.0732 | –0.0018 (0.0044)† | –0.0050, 0.0013 |
| Coronal Translation | ||||
| 15 mm Lat | 0.0001 (0.0002) | –0.0001, 0.0002 | –0.1047 (0.0262)† | –0.1235, –0.0860 |
| 10 mm Lat | 0.0003 (0.0006) | –0.0001, 0.0007 | –0.0743 (0.0273)† | –0.0938, –0.0547 |
| 5 mm Lat | 0.0012 (0.0021)* | –0.0003, 0.0027 | –0.0532 (0.0268)† | –0.0720, –0.0340 |
| Aligned | 0.0032 (0.0039) | 0.0005, 0.0060 | –0.0279 (0.0169) | –0.0400, –0.0159 |
| 5 mm Med | 0.0073 (0.0066)* | 0.0026, 0.0120 | –0.0153 (0.0105)† | –0.0228, –0.0078 |
| 10 mm Med | 0.0179 (0.0141)† | 0.0078, 0.0279 | –0.0057 (0.0050)† | –0.0093, –0.0020 |
| 15 mm Med | 0.0341 (0.0218)† | 0.0185, 0.0497 | –0.0015 (0.0022)† | –0.0031, 0.0000 |
| Alignment changes | Extension moment impulse (Nm·s/kg) |
Flexion moment impulse (Nm·s/kg) |
||
|---|---|---|---|---|
| Mean (SD) | 95% CI | Mean (SD) | 95% CI | |
| Sagittal Angle | ||||
| 6°Ext | 0.1620 (0.0449) | 0.1298, 0.1941 | –0.0079 (0.0067) | –0.0126, –0.0031 |
| 4°Ext | 0.1652 (0.0490) | 0.1302, 0.2002 | –0.0092 (0.0088) | –0.0155, –0.0030 |
| 2° Ext | 0.1620 (0.0476) | 0.1279, 0.1960 | –0.0091 (0.0085) | –0.0152, –0.0030 |
| Aligned | 0.1658 (0.0512) | 0.1292, 0.2024 | –0.0090 (0.0108) | –0.0167, –0.0013 |
| 2° Flex | 0.1704 (0.0553) | 0.1309, 0.2100 | –0.0066 (0.0077) | –0.0121, –0.0011 |
| 4° Flex | 0.1734 (0.0621) | 0.1289, 0.2178 | –0.0070 (0.0101) | –0.0143, 0.0002 |
| 6° Flex | 0.1824 (0.0745) | 0.1291, 0.2356 | –0.0074 (0.0148) | –0.0180, –0.0032 |
| Sagittal Translation | ||||
| 15 mm Ant | 0.1168 (0.0374)† | 0.0900, 0.1435 | –0.0179 (0.0152)† | –0.0288, –0.0069 |
| 10 mm Ant | 0.1328 (0.0405)† | 0.1038, 0.1618 | –0.0145 (0.0130)† | –0.0239, –0.0052 |
| 5 mm Ant | 0.1473 (0.0411)* | 0.1180, 0.1767 | –0.0109 (0.0098) | –0.0179, –0.0039 |
| Aligned | 0.1658 (0.0512) | 0.1292, 0.2024 | –0.0090 (0.0108) | –0.0167, –0.0013 |
| 5 mm Post | 0.1864 (0.0595)† | 0.1438, 0.2290 | –0.0068 (0.0088) | –0.0131, –0.0047 |
| 10 mm Post | 0.2033 (0.0728)† | 0.1513, 0.2554 | –0.0054 (0.0080)* | –0.0111, 0.0003 |
| 15 mm Post | 0.2368 (0.0788)† | 0.1805, 0.2932 | –0.0039 (0.0068)* | –0.0088, 0.0010 |
Abbreviations: 95% CI, 95% confidence interval; Abd, abduction; Add, adduction; Ant, anterior; Ext, extension; Flex, flexion; Lat, lateral; Med, medial; Post, posterior; SD, standard deviation.
Indicates a significant difference at P < 0.05 from the nominally aligned condition.
Indicates a significant difference at P < 0.01 from the nominally aligned condition.
Fig. 3.
Socket reaction moment impulse (Nm·s/kg) in the coronal plane in response to (A) coronal angle alignment changes and (B) coronal translation alignment changes. The means and standard deviations at each alignment condition are presented in orange for the valgus socket reaction moment impulse (valgus moment impulse) and in green for the varus socket reaction moment impulse (varus moment impulse). An asterisk (*) indicates a significant difference at P < 0.05 from the nominally aligned condition, while a cross (†) indicates a significant difference at P < 0.01 from the nominally aligned condition. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
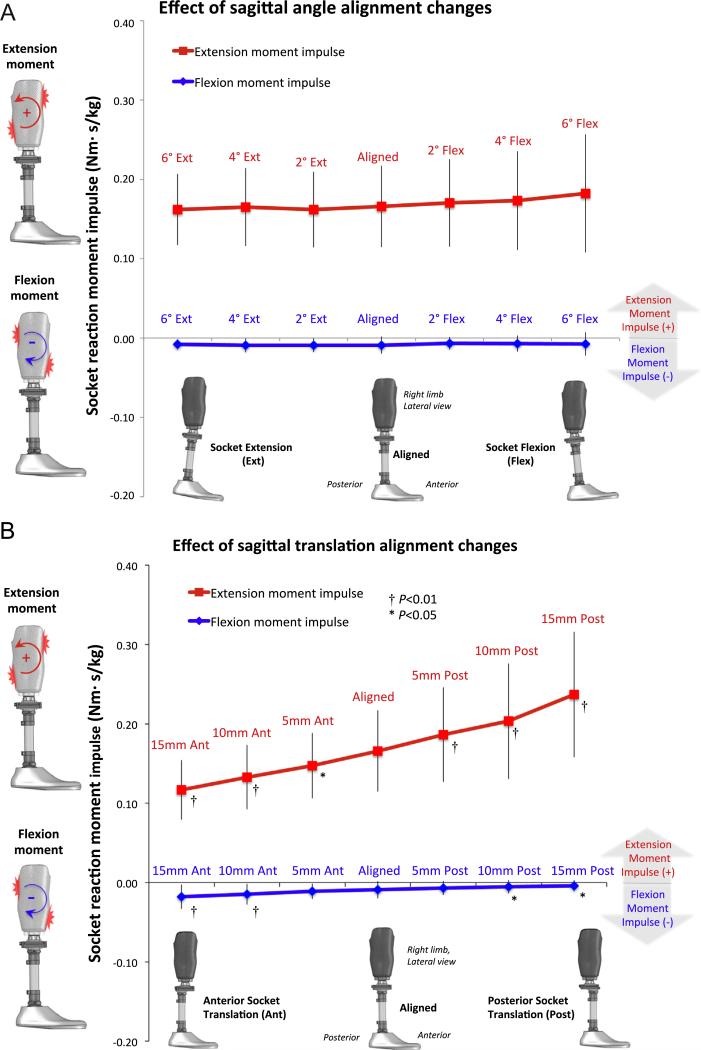
3.2. Effect of sagittal alignment changes on the sagittal socket reaction moment impulse
Sagittal angle alignment changes did not induce any significant differences at all malaligned conditions for the extension and flexion socket reaction moment impulse compared to the nominally aligned condition. However, translation alignment changes induced significant differences at all malaligned conditions for the extension socket reaction moment impulse and at some malaligned conditions for the flexion socket reaction moment impulse in comparison to the nominally aligned condition (Table 2; Fig. 4).
Fig. 4.
Socket reaction moment impulse (Nm·s/kg) in the sagittal plane in response to (A) sagittal angle alignment changes and (B) sagittal translation alignment changes. The means and standard deviations at each alignment condition are presented in red for the extension socket reaction moment impulse (extension moment impulse) and in blue for the flexion socket reaction moment impulse (flexion moment impulse). An asterisk (*) indicates a significant difference at P < 0.05 from the nominally aligned condition, while a cross (†) indicates a significant difference at P < 0.01 from the nominally aligned condition. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
3.3. Effect of sagittal and coronal alignment changes on the stance duration time
No significant differences were found between the nominally aligned and malaligned conditions for all comparisons (Table 3).
Table 3.
Effect of sagittal and coronal alignment changes on stance duration time.
| Alignment changes | Stance duration time (s) |
Alignment changes | Stance duration time (s) |
||
|---|---|---|---|---|---|
| Mean (SD) | 95% CI | Mean (SD) | 95% CI | ||
| Coronal Angle | Sagittal Angle | ||||
| 6° Abd | 0.71 (0.09) | 0.65, 0.78 | 6°Ext | 0.71 (0.10) | 0.64, 0.78 |
| 4° Abd | 0.72 (0.11) | 0.64, 0.79 | 4°Ext | 0.72 (0.10) | 0.64, 0.79 |
| 2° Abd | 0.70 (0.10) | 0.63, 0.78 | 2° Ext | 0.71 (0.11) | 0.63, 0.79 |
| Aligned | 0.72 (0.11) | 0.65, 0.80 | Aligned | 0.72 (0.11) | 0.65, 0.80 |
| 2° Add | 0.72 (0.10) | 0.64, 0.79 | 2° Ext | 0.71 (0.11) | 0.63, 0.79 |
| 4° Add | 0.71 (0.09) | 0.64, 0.77 | 4° Flex | 0.72 (0.12) | 0.63, 0.81 |
| 6° Add | 0.72 (0.10) | 0.65, 0.79 | 6° Flex | 0.72 (0.11) | 0.64, 0.79 |
| Coronal Translation | Sagittal Translation | ||||
| 15 mm Lat | 0.73 (0.11) | 0.65, 0.81 | 15 mm Ant | 0.72 (0.11) | 0.64, 0.79 |
| 10 mm Lat | 0.71 (0.09) | 0.64, 0.77 | 10 mm Ant | 0.72 (0.13) | 0.63, 0.82 |
| 5 mm Lat | 0.72 (0.11) | 0.64, 0.80 | 5 mm Ant | 0.72 (0.10) | 0.65, 0.79 |
| Aligned | 0.72 (0.11) | 0.65, 0.80 | Aligned | 0.72 (0.11) | 0.65, 0.80 |
| 5 mm Med | 0.72 (0.11) | 0.64, 0.80 | 5 mm Post | 0.71 (0.10) | 0.63, 0.79 |
| 10 mm Med | 0.72 (0.12) | 0.64, 0.80 | 10 mm Post | 0.70 (0.10) | 0.63, 0.78 |
| 15 mm Med | 0.72 (0.11) | 0.65, 0.80 | 15 mm Post | 0.71 (0.11) | 0.64, 0.79 |
Abbreviations: 95% CI, 95% confidence interval; Abd, abduction; Add, adduction; Ant, anterior; Ext, extension; Flex, flexion; Lat, lateral; Med, medial; Post, posterior; SD, standard deviation.
4. Discussion
This study demonstrated the relationship between the transtibial prosthetic alignment and the socket reaction moment impulse. Quantifying the effect of alignment changes on the impulse in lower-limb prostheses is a novel idea that may advance evidence-based practice in prosthetic alignment. While an amputee is walking, the residual limb is cyclically exposed to the socket reaction moment impulse. Because the socket reaction moment impulse accounts for both the magnitude and duration of load, it may provide additional biomechanical information to investigate the socket-residual limb interface (Mak et al., 2001). Further study on the relationships among the alignment, socket reaction moment impulse, pressure, stress and residual limb skin or tissue conditions are warranted to explore more comprehensive care and management of the residual limb in amputees through better prosthetic alignment.
The relationship between the alignment and the socket reaction moment impulse was clearly observed in the coronal angle, coronal translation and sagittal translation alignment changes (Fig. 3A and B, Fig. 4B). However, this relationship was not evident in the sagittal angle alignment changes (Fig. 4A). No significant differences were found in the socket reaction moment impulse at all malaligned conditions in comparison to the nominally aligned condition when sagittal angle alignment changes were induced. This is an interesting finding, suggesting the potential difference in the effect of sagittal angle and translation alignment changes. This difference appears to be attributable to the differences in their effects on the magnitude of the socket reaction moment because no significant difference was observed in the stance duration time among the alignment conditions (Table 3).
An earlier study demonstrated that the effect of increased socket extension is (1) decreased flexion moment at early stance, (2) increased extension moment at mid-stance, and (3) decreased peak extension moment at late stance; while the effect of increased socket flexion is (1) increased flexion moment at early stance, (2) decreased extension moment at mid-stance, and (3) increased extension moment at late stance (Kobayashi et al., 2014). As a result, the net area under the socket reaction moment curve did not change significantly by the angle alignment changes. The study also demonstrated that the effect of increased socket anterior translation is (1) increased flexion moment at early stance, (2) decreased extension moment at mid-stance, and (3) decreased peak extension moment at late stance, while the effect of increased socket posterior translation is (1) decreased flexion moment at early stance, (2) increased extension moment at mid-stance, and (3) increased peak extension moment at late stance (Kobayashi et al., 2014). As a result, the area under the socket reaction moment curve systematically increased as the socket was translated more posteriorly. Sagittal angle and translation alignment changes therefore have a different effect on the socket reaction moment impulse based solely on the relative difference on the resultant socket reaction moment.
Under the nominally aligned condition, the mean valgus socket reaction moment impulse was 0.0032 (0.0039) Nm·s/kg and the mean varus socket reaction moment impulse was –0.0279 (0.0169) Nm·s/kg in the coronal plane, while the mean extension socket reaction moment impulse was 0.1658 (0.0512) Nm·s/kg and the mean flexion socket reaction moment impulse was –0.0090 (0.0108) Nm·s/kg in the sagittal plane (Table 2). It should be noted that the nominal alignment was determined based on the agreement between the prosthetist and the participant. The nominal alignment might not be a true optimal alignment. In the coronal plane, the socket is generally positioned slightly lateral to the foot in bench alignment for mid-stance stability (Berger and Fishman, 1997). This would bias the coronal socket reaction moment impulse toward varus. With 4° of socket adduction or 10 mm of medial translation of the socket, the valgus socket reaction moment impulse became more dominant, suggesting potential instability during mid-stance. In the sagittal plane, translation malalignments induced a linear change in the extension socket reaction moment impulse (Fig. 4B). This means that the extension socket reaction moment impulse is smaller at 15 mm of anterior malalignment condition than when nominally aligned. It is anticipated that a certain amount of extension socket reaction moment impulse is needed for gait stability and propulsion. Zero socket reaction moment impulse is only possible with no movement. Therefore, the goal of alignment tuning is not simply to minimize the socket reaction moment impulse, but rather to normalize it for amputees gait. Although the acceptable amount of the socket reaction moment impulse or its range is not known at this stage, this study suggested that an appropriate range might exist for effective gait with a prosthesis. A future study should investigate this in order to utilize the socket reaction moment impulse data to drive the alignment tuning process.
The moment impulse is influenced by the magnitude of moment and the stance duration time. The stance duration time did not show any statistical differences among the alignment conditions in this study. Therefore, the differences in the impulse primarily attribute to the magnitude of moment at each alignment condition. It was suggested that the moment impulse is sensitive to gait speed because it affects the stance duration time (Robbins and Maly, 2009). Generally, walking at slower gait speed results in increases in the moment impulse because it increases the stance duration despite the fact that it generally reduces the moment magnitude (Robbins and Maly, 2009; Thorp et al., 2006). However, a recent study showed that both fast and slow walking resulted in increases in the moment impulse in healthy adults (van den Noort et al., 2013). The knee moment impulse of the residual and intact limb were compared in transtibial amputees (Fey and Neptune, 2012). The internal knee flexion moment impulse in the sagittal plane and external knee rotation moment impulse in the transverse plane of the intact knee were generally larger across gait speeds in the amputees. Gait speed was not measured in this study, but no significant differences were found in stance time across alignment conditions. Therefore, it was most likely that the socket reaction moment impulse was not affected by gait speed changes due to alignment changes. Although individual analysis of the effect of alignment changes on the socket reaction moment impulse was not performed, the socket reaction moment impulse may also be influenced by the individual's length of experience using a prosthesis to walk, and the type of prosthetic feet. Finally, a total of 25 alignment conditions were tested in this study. Each participant was allowed to rest during data collection, but there might have been effects of fatigue on their gait.
This study focused on in-plane effects of the alignment changes on the socket reaction moment impulse. However, a preceeding study suggested that sagittal alignment changes could potentially affect coronal socket reaction moments in transtibial prostheses (Kobayashi et al., 2012). The alignment was changed only in the sagittal and coronal planes. Findings of the studies that investigated the effect of the foot alignment in the transverse plane on the moment impulse in healthy adults are contradictory. One study showed that the toe-out gait pattern significantly reduced the knee adduction moment impulse (Caldwell et al., 2013), while the other study revealed that the toe-in gait pattern significantly reduced it (van den Noort et al., 2013). In prostheses, toe-in and toe-out are expected to affect both the sagittal and coronal socket reaction moments as they change the length of the moment lever arm in both planes. It is our intention to investigate the effect of transverse plane alignment changes on the socket reaction moment impulse in a future study.
The immediate effects of alignment changes on the socket reaction moment impulse were investigated in this study. Amputees do not appear especially sensitive to alignment errors in the short term (Boone et al., 2012), but the adverse effects of malalignment on residual limb health most likely occur in the long term. Amputees may accommodate the malalignment through gait compensations or by reducing their daily activity level. Either strategy can reduce the residual limb discomfort, one by reducing the magnitude of the moment impulse the other by reducing the number of times this impulse is applied by reducing locomotion. Long-term residual limb health might be estimated by multiplying the socket reaction moment impulse by the number of steps each day. This approach has been suggested in the etiology of knee osteoarthritis (Maly et al., 2013). Monitoring load on the residual limb and amputees activity in the community would be valuable to evaluate the efficacy and impact of the prosthetic components and their alignment in their daily life.
5. Conclusion
This study demonstrated the relationship between the alignment and the socket reaction moment impulse. Although the appropriate range of the socket reaction moment impulse for effective prosthetic gait and care of the residual limb is not currently known, the results of this study suggested that the socket reaction moment impulse could potentially serve as a valuable parameter to assist the alignment tuning process of the transtibial prostheses. Further study is needed to investigate the impact of the socket reaction moment impulse on residual limb health in amputees.
Acknowledgments
This study was supported by the National Center for Medical Rehabilitation Research, National Institutes of Health, Grant numbers R43HD047119 and R44HD047119.
Footnotes
Conflict of interest statement
Authors of the manuscript (Kobayashi T, Orendurff MS, Rosenbaum-Chou TG and Boone DA) are currently employees of the company that manufactures the Smart Pyramid™ (currently known as Europa™) used in this study.
References
- Beil TL, Street GM, Covey SJ. Interface pressures during ambulation using suction and vacuum-assisted prosthetic sockets. J. Rehabil Res. Dev. 2002;39:693–700. [PubMed] [Google Scholar]
- Berger N, Fishman S. Prosthetic Fitting, Alignment and Fabrication, Lower-Limb Prosthetics. Prosthetics-Orthotics Publications; New York: 1997. pp. 97–104. [Google Scholar]
- Boone DA, Kobayashi T, Chou TG, Arabian AK, Coleman KL, Orendurff MS, Zhang M. Perception of socket alignment perturbations in amputees with transtibial prostheses. J. Rehabil Res. Dev. 2012;49:843–854. doi: 10.1682/jrrd.2011.08.0143. [DOI] [PubMed] [Google Scholar]
- Boone DA, Kobayashi T, Chou TG, Arabian AK, Coleman KL, Orendurff MS, Zhang M. Influence of malalignment on socket reaction moments during gait in amputees with transtibial prostheses. Gait Posture. 2013;37:620–626. doi: 10.1016/j.gaitpost.2012.10.002. [DOI] [PubMed] [Google Scholar]
- Caldwell LK, Laubach LL, Barrios JA. Effect of specific gait modifications on medial knee loading, metabolic cost and perception of task difficulty. Clin. Biomech. (Bristol, Avon) 2013;28:649–654. doi: 10.1016/j.clinbiomech.2013.05.012. [DOI] [PubMed] [Google Scholar]
- Dou P, Jia X, Suo S, Wang R, Zhang M. Pressure distribution at the stump/ socket interface in transtibial amputees during walking on stairs, slope and non-flat road. Clin. Biomech. (Bristol, Avon) 2006;21:1067–1073. doi: 10.1016/j.clinbiomech.2006.06.004. [DOI] [PubMed] [Google Scholar]
- Dumas R, Cheze L, Frossard L. Loading applied on prosthetic knee of transfemoral amputee: comparison of inverse dynamics and direct measurements. Gait Posture. 2009;30:560–562. doi: 10.1016/j.gaitpost.2009.07.126. [DOI] [PubMed] [Google Scholar]
- Fantini Pagani CH, Potthast W, Bruggemann GP. The effect of valgus bracing on the knee adduction moment during gait and running in male subjects with varus alignment. Clin. Biomech. (Bristol, Avon) 2010;25:70–76. doi: 10.1016/j.clinbiomech.2009.08.010. [DOI] [PubMed] [Google Scholar]
- Fernie G. Biomechanics of gait and prosthetic alignment. In: Kostuik J, Gillespie R, editors. Amputation Surgery and Rehabilitation: The Toronto Experience. Churchhill Livingstone; New York: 1981. pp. 259–265. [Google Scholar]
- Fey NP, Neptune RR. 3D intersegmental knee loading in below-knee amputees across steady-state walking speeds. Clin. Biomech. (Bristol, Avon) 2012;27:409–414. doi: 10.1016/j.clinbiomech.2011.10.017. [DOI] [PubMed] [Google Scholar]
- Frossard L, Beck J, Dillon M, Chappell M, Evans J. Development and preliminary testing of a device for the direct measurement of forces and moments in the prosthetic limb of transfemoral amputees during activities of daily living. J. Prosthet. Orthot. 2003;15:135–142. [Google Scholar]
- Frossard L, Cheze L, Dumas R. Dynamic input to determine hip joint moments, power and work on the prosthetic limb of transfemoral amputees: ground reaction vs knee reaction. Prosthet. Orthot. Int. 2011;35:140–149. doi: 10.1177/0309364611409002. [DOI] [PubMed] [Google Scholar]
- Hinman RS, Bowles KA, Metcalf BB, Wrigley TV, Bennell KL. Lateral wedge insoles for medial knee osteoarthritis: effects on lower limb frontal plane biomechanics. Clin. Biomech. (Bristol, Avon) 2012;27:27–33. doi: 10.1016/j.clinbiomech.2011.07.010. [DOI] [PubMed] [Google Scholar]
- Jones RK, Nester CJ, Richards JD, Kim WY, Johnson DS, Jari S, Laxton P, Tyson SF. A comparison of the biomechanical effects of valgus knee braces and lateral wedged insoles in patients with knee osteoarthritis. Gait Posture. 2013;37:368–372. doi: 10.1016/j.gaitpost.2012.08.002. [DOI] [PubMed] [Google Scholar]
- Kean CO, Bennell KL, Wrigley TV, Hinman RS. Modified walking shoes for knee osteoarthritis: mechanisms for reductions in the knee adduction moment. J. Biomech. 2013;46:2060–2066. doi: 10.1016/j.jbiomech.2013.05.011. [DOI] [PubMed] [Google Scholar]
- Kean CO, Hinman RS, Bowles KA, Cicuttini F, Davies-Tuck M, Bennell KL. Comparison of peak knee adduction moment and knee adduction moment impulse in distinguishing between severities of knee osteoarthritis. Clin. Biomech. (Bristol, Avon) 2012;27:520–523. doi: 10.1016/j.clinbiomech.2011.12.007. [DOI] [PubMed] [Google Scholar]
- Kito N, Shinkoda K, Yamasaki T, Kanemura N, Anan M, Okanishi N, Ozawa J, Moriyama H. Contribution of knee adduction moment impulse to pain and disability in Japanese women with medial knee osteoarthritis. Clin. Biomech. (Bristol, Avon) 2010;25:914–919. doi: 10.1016/j.clinbiomech.2010.06.008. [DOI] [PubMed] [Google Scholar]
- Kobayashi T, Arabian AK, Orendurff MS, Chou TG, Boone DA. Effect of alignment changes on socket reaction moments while walking in transtibial prostheses with energy storage and return feet. Clin. Biomech. (Bristol, Avon) 2014;29:47–56. doi: 10.1016/j.clinbiomech.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi T, Orendurff MS, Boone DA. Effect of alignment changes on socket reaction moments during gait in transfemoral and knee-disarticulation prostheses: case series. J. Biomech. 2013a;46:2539–2545. doi: 10.1016/j.jbiomech.2013.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi T, Orendurff MS, Zhang M, Boone DA. Effect of transtibial prosthesis alignment changes on out-of-plane socket reaction moments during walking in amputees. J. Biomech. 2012;45:2603–2609. doi: 10.1016/j.jbiomech.2012.08.014. [DOI] [PubMed] [Google Scholar]
- Kobayashi T, Orendurff MS, Zhang M, Boone DA. Effect of alignment changes on sagittal and coronal socket reaction moment interactions in transtibial prostheses. J. Biomech. 2013b;46:1343–1350. doi: 10.1016/j.jbiomech.2013.01.026. [DOI] [PubMed] [Google Scholar]
- Leitch KM, Birmingham TB, Dunning CE, Giffin JR. Changes in valgus and varus alignment neutralize aberrant frontal plane knee moments in patients with unicompartmental knee osteoarthritis. J. Biomech. 2013;46:1408–1412. doi: 10.1016/j.jbiomech.2013.01.024. [DOI] [PubMed] [Google Scholar]
- Mak AF, Zhang M, Boone DA. State-of-the-art research in lower-limb prosthetic biomechanics-socket interface: a review. J. Rehabil. Res. Dev. 2001;38:161–174. [PubMed] [Google Scholar]
- Maly MR, Robbins SM, Stratford PW, Birmingham TB, Callaghan JP. Cumulative knee adductor load distinguishes between healthy and osteoarthritic knees – a proof of principle study. Gait Posture. 2013;37:397–401. doi: 10.1016/j.gaitpost.2012.08.013. [DOI] [PubMed] [Google Scholar]
- Neumann ES, Brink J, Yalamanchili K, Lee JS. Use of a load cell and force-moment curves to compare transverse plane moment loads on transtibial residual limbs: a preliminary investigation. Prosthet Orthot Int. 2013 doi: 10.1177/0309364613497048. first published on August 6, 2013 as http://dx.doi.org/10.1177/0309364613497048. [DOI] [PubMed]
- Robbins SM, Maly MR. The effect of gait speed on the knee adduction moment depends on waveform summary measures. Gait Posture. 2009;30:543–546. doi: 10.1016/j.gaitpost.2009.08.236. [DOI] [PubMed] [Google Scholar]
- Sanders JE, Miller RA, Berglund DN, Zachariah SG. A modular six-directional force sensor for prosthetic assessment: a technical note. J. Rehabil. Res. Dev. 1997;34:195–202. [PubMed] [Google Scholar]
- Sanders JE, Zachariah SG, Jacobsen AK, Fergason JR. Changes in interface pressures and shear stresses over time on trans-tibial amputee subjects ambulating with prosthetic limbs: comparison of diurnal and six-month differences. J. Biomech. 2005;38:1566–1573. doi: 10.1016/j.jbiomech.2004.08.008. [DOI] [PubMed] [Google Scholar]
- Sankoh AJ, Huque MF, Dubey SD. Some comments on frequently used multiple endpoint adjustment methods in clinical trials. Stat. Med. 1997;16:2529–2542. doi: 10.1002/(sici)1097-0258(19971130)16:22<2529::aid-sim692>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- Schwarze M, Hurschler C, Seehaus F, Oehler S, Welke B. Loads on the prosthesis-socket interface of above-knee amputees during normal gait: validation of a multi-body simulation. J. Biomech. 2013;46:1201–1206. doi: 10.1016/j.jbiomech.2013.02.005. [DOI] [PubMed] [Google Scholar]
- Silver-Thorn MB, Steege JW, Childress DS. A review of prosthetic interface stress investigations. J. Rehabil. Res. Dev. 1996;33:253–266. [PubMed] [Google Scholar]
- Stephenson P, Seedhom BB. Estimation of forces at the interface between an artificial limb and an implant directly fixed into the femur in above-knee amputees. J. Orthop. Sci.: Off. J. Jpn. Orthop. Assoc. 2002;7:292–297. doi: 10.1007/s007760200050. [DOI] [PubMed] [Google Scholar]
- Thorp LE, Sumner DR, Block JA, Moisio KC, Shott S, Wimmer MA. Knee joint loading differs in individuals with mild compared with moderate medial knee osteoarthritis. Arthritis Rheum. 2006;54:3842–3849. doi: 10.1002/art.22247. [DOI] [PubMed] [Google Scholar]
- Tukey JW, Ciminera JL, Heyse JF. Testing the statistical certainty of a response to increasing doses of a drug. Biometrics. 1985;41:295–301. [PubMed] [Google Scholar]
- van den Noort JC, Schaffers I, Snijders J, Harlaar J. The effectiveness of voluntary modifications of gait pattern to reduce the knee adduction moment. Hum. Mov. Sci. 2013;32:412–424. doi: 10.1016/j.humov.2012.02.009. [DOI] [PubMed] [Google Scholar]
- Yeung LF, Leung AK, Zhang M, Lee WC. Effects of long-distance walking on socket-limb interface pressure, tactile sensitivity and subjective perceptions of trans-tibial amputees. Disabil. Rehabil. 2013;35:888–893. doi: 10.3109/09638288.2012.712197. [DOI] [PubMed] [Google Scholar]
- Zahedi MS, Spence WD, Solomonidis SE, Paul JP. Alignment of lower-limb prostheses. J. Rehabil. Res. Dev. 1986;23:2–19. [PubMed] [Google Scholar]