Abstract
The epidemiology of Staphylococcus aureus in the community in Ghana was never investigated prior to this study. The aims of the study were: i) to assess prevalence of nasal S. aureus carriage in Ghanaian people living in an urban and a rural area, and ii) to identify phenotypic and genotypic traits of strains isolated from the two communities. Nasal swabs were collected from healthy individuals living in an urban community situated in the suburb of the capital city, Accra (n = 353) and in a rural community situated in the Dangme-West district (n = 234). The overall prevalence of nasal carriage was 21% with a significantly higher prevalence in the urban (28%) than in the rural community (11%) (p<0.0001). The levels of antimicrobial resistance were generally low (<5%) except for penicillin (91%) and tetracycline (25%). The only two (0.3%) MRSA carriers were individuals living in the urban area and had been exposed to hospitals within the last 12 months prior to sampling. Resistance to tetracycline (p = 0.0009) and presence of Panton-Valentine leukocidin (PVL) gene (p = 0.02) were significantly higher among isolates from the rural community compared to isolates from the urban community. Eleven MLST clonal complexes (CC) were detected based on spa typing of the 124 S. aureus isolates from the two communities: CC8 (n = 36), CC152 (n = 21), CC45 (n = 21), CC15 (n = 18), CC121 (n = 6), CC97 (n = 6), CC30 (n = 5), CC5 (n = 5), CC508 (n = 4), CC9 (n = 1), and CC707 (n = 1). CC8 and CC45 were less frequent in the rural area than in the urban area (p = 0.02). These results reveal remarkable differences regarding carriage prevalence, tetracycline resistance, PVL content and clonal distribution of S. aureus in the two study populations. Future research may be required to establish whether such differences in nasal S. aureus carriage are linked to socio-economic differences between urban and rural communities in this African country.
Introduction
Staphylococcus aureus is carried by 20–30% of the human population, defined as persistent carriers, whereas the remaining part of the population does not carry or is only transiently colonized by this opportunistic pathogen [1]. Colonization of the anterior nares is a recognized risk factor for subsequent S. aureus infection, although carriers generally have a better prognosis [2]. Risk factors for colonization include young age, male sex, underlying comorbidities, hospitalization and exposure to livestock [2]–[5].
Data on S. aureus nasal carriage in the community are largely based on developed countries [6]–[13] and reports from sub-Saharan African countries are very limited [14]–[17]. High frequencies (>55%) of strains carrying Panton-Valentine leukocidin (PVL), a toxin associated with community-acquired methicillin-resistant S. aureus (CA-MRSA) [18], [19], have been reported in Mali [14] Gabon [16], [17] and Nigeria [20], [21], suggesting that a common CA-MRSA clone associated with PVL (sequence type ST152) could have evolved from a methicillin-susceptible variant of this clone originating from the African continent [14], [16].
We recently reported a significant difference in nasal carriage prevalence between inpatients (14%) and staff (23%) at the largest hospital in Ghana [22]. This and a subsequent study on clinical S. aureus isolates [23] showed high frequency of PVL-positive isolates (23–60%) with predominance of t355 (CC152) and t084 (CC15) in Ghana. The epidemiology of S. aureus among healthy people in the Ghanaian community, however, remains unknown.
The aims of this study were: i) to assess prevalence of nasal S. aureus carriage in Ghanaian people living in an urban and a rural area, and ii) to identify phenotypic and genotypic differences between strains isolated from the two communities. For this purpose, isolates obtained from the two communities were compared with respect to antimicrobial susceptibility, PVL gene content and genetic background.
Materials and Methods
Ethical Approval
Ethical clearance was obtained from the University of Ghana Medical School Ethical and Protocol Review Board (reference no. MS-Et/M.8 - P.4.4/2010–11). The consent document was signed or thumb printed by participants or guardians (on behalf of children) and a witness. The consent request was interpreted in the local dialect by the researcher to participants or guardians who could not comprehend the English language. The Ethical and Protocol Review Board approved the consent documents and procedures.
Study Design, Area and Population
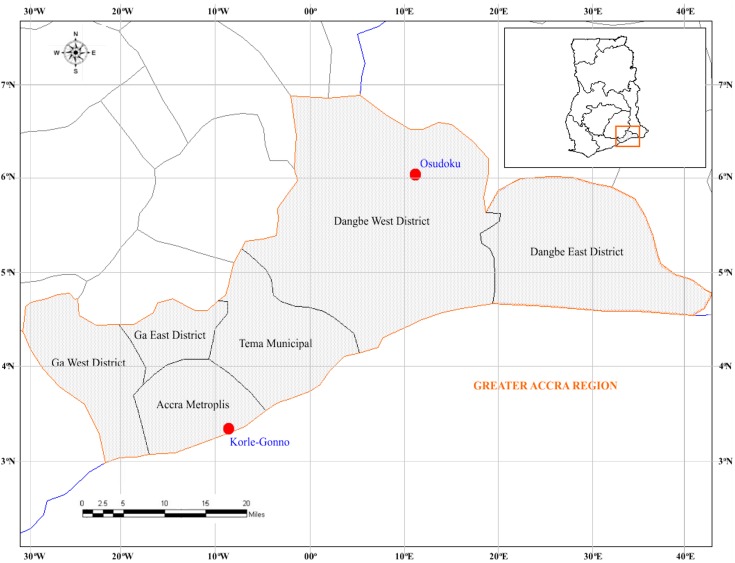
A cross-sectional-type study was conducted between May 2011 and April 2012 at two communities located in Southern Ghana: Korle Gonno (urban) and Osudoku (rural); approximately 102.5 kilometres (63.7 miles) apart. Korle Gonno is a densely populated and overcrowded suburb of Accra Metropolis District with an approximate population of 60,000 inhabitants. Korle gonno is primarily, a fishing community but has a market and beach resorts which attracts clients from various parts of Ghana. This urban community has easy access to pharmacies and to the largest teaching hospital in Ghana, which serve the majority of the population in Ghana. Osudoku is a rural area situated in the Dangme-West district with a low population size of 18,972 inhabitants. Agriculture, animal husbandry and hunting are the prevalent economic activities. Access to healthcare facilities is limited in this remote area. The two communities are located in the Greater Accra region of Ghana (Figure 1).
Figure 1. Map showing the location of the two communities in Ghana.
Sample Collection and Isolation of S. aureus
Apparently healthy persons were enrolled based on their consent to participate in the study. Nasal samples were taken by rotating sterile cotton swabs in both anterior nares. Using a standardised questionnaire, information regarding the following demographic data and risk factors were obtained from each participant: age, sex, exposure to hospitals (i.e. visit as an outpatient or hospitalization) and self-reported antimicrobial therapy within the last 12 months, self-reported diseases such as eczema or diabetes and presence of a healthcare worker in household.
Pre-enrichment of nasal swabs was performed in 5 mL Muller Hinton broth supplemented with 6.5% NaCl, (Oxoid, Ltd., Basingstokes, UK) within 24 hrs after sampling and incubated at 37°C for 24 hrs and plated on 5% sheep blood agar (Oxoid, Ltd., Basingstokes, UK). S. aureus isolates were identified phenotypically by colony morphology, haemolysis, catalase test, Gram staining and confirmed by tube coagulase, slidex staphplus test (bioMérieux, Marcy l′Etoil, France) and PCR identification of the spa gene [24].
Antimicrobial Susceptibility Testing
Susceptibility testing of 11 antimicrobial agents was done according to EUCAST guidelines (www.eucast.org) as described elsewhere [22]. MRSA isolated were tested for glycopeptide resistance as previously described [25]. Multidrug resistance (MDR) was defined as resistance to three or more distinct antimicrobial classes [26].
Molecular Characterization
Detection of spa, mecA and pvl genes was performed according to standard methods [24], [27]. For all isolates, spa types and MLST CCs were assigned using BioNumerics V6.5 (Applied Maths, Sint-Martens-Latem Belgium) with the spa (http://www.spaserver.ridom.de) plug in. Multi-Locus Sequence Typing (MLST) [28] and Staphylococcal cassette chromosome mec (SCCmec) typing by multiplex PCR assays 1 and 2 [29] were done limited to MRSA isolates.
Statistical Analysis
Data were analyzed using the glm-function in R version 2.15.2 (R Development Core Team, 2012). Possible associations of S. aureus nasal carriage with age, sex and the other four risk factors investigated by the questionnaire (exposure to hospital environment, self-reported antimicrobial therapy, self-reported disease, and health worker in household) were assessed by logistic regression analysis. The confounding effects were assessed for each factor through assessment of the effect of the parameter estimates by offering the factors individually and assessing the effect from this. Furthermore, two-way interactions were assessed. For analytical purposes, community-associated (CA) S. aureus was defined as isolates from participants without previous exposure to the hospital environment, whereas community-onset (CO) S. aureus referred to isolates from participants with a history of hospital exposure within the last 12 months [30]. Model fit was assessed using the Pearson Χ2-statistics to judge unexplained extra-binomial variation. Relative risks of significant parameters were subsequently estimated. The two-sample z-test was used to compare the proportion of strains resistant to the different antimicrobials in the two areas. Furthermore, the association of genotypes (spa type, CC-groups, PVL-positivity) to sex and source (community) were determined using the Fisher exact test. Only the four most prevalent genotypes with more than 10 observations were included in this analysis.
Results
Study Population and S. aureus Carriage
A total of 587 nasal swabs were obtained from the two study areas: 353 (60%) from Korle Gonno (urban) and 234 (40%) from Osudoku (rural). Demographic characteristics of the two study populations are shown in Table 1. The participants included 370 (63%) females and 217 (37%) males, with an overall mean age of 32 years (age range: 1–115 years). Among the 587 study participants, 216 (36.8%) indicated exposure to the hospital environment within the last 12 months (Table 1). Forty-one (7%) reported recent usage of antimicrobial agents, including penicillin (n = 34, 6%); ciprofloxacin (n = 5, 0.9%) and tetracycline (n = 2, 0.3%).
Table 1. Demographic characteristics of the study participants from the rural community in Osudoku (OS) and the urban community in Korle-gonno (KG), Ghana, 2011–2012.
| Characteristic | Category | OS (N = 234) | KG (N = 353) | Total (N = 587) | p-value |
| n (%) | n (%) | n (%) | |||
| Age (mean/sd) | 34.5 (23.2) | 29.7 (20.6) | 31.6 (21.8) | 0.0085 | |
| Sex | Female | 140 (59.8) | 230 (65.2) | 370 (63.0) | |
| Male | 94 (40.2) | 123 (34.8) | 217 (37.0) | 0.2218 | |
| EH | No | 132 (56.4) | 239 (67.7) | 371 (63.2) | |
| Yes | 102 (43.6) | 114 (32.3) | 216 (36.8) | 0.0071 | |
| SRD | No | 192 (82.1) | 338 (95.8) | 530 (90.3) | |
| Yes | 42 (17.9) | 15 (4.2) | 57 (9.7) | <0.0001 | |
| SRAT | No | 209 (89.3) | 337 (95.5) | 546 (93.0) | |
| Yes | 25 (10.7) | 16 (4.5) | 41 (7.0) | 0.0069 | |
| HWHH | No | 227 (97.0) | 284 (80.5) | 511 (87.1) | |
| Yes | 7 (3.0) | 69 (19.5) | 76 (12.9) | <0.0001 |
sd, standard deviation; EH: exposure to hospitals; SRD: Self-reported disease; SRAT: self-reported antimicrobial therapy; HWHH: healthcare worker in household.
S. aureus was identified in 21% (124/587) of the nasal swabs cultured. Among the 124 carriers, 98 (79%) resided in the urban area and 26 (21%) in the rural area. (Table 2). The nasal carriage prevalence was significantly higher at Korle Gonno (urban) (98/353; 28%) compared to Osudoku (rural) (26/234; 11%) (p<0.0001), resulting in a 2.5 (95% CI: 1.7–3.7) higher risk of being a carrier in the urban area. No confounding effects were detected. The proportions of carriers in the age groups 0–9, 10–19, 20–29, 30–39, 40–49, 50–59, 60–69 and >70 years were 19%, 29%, 19%, 17%, 20%, 20%, 19% and 18%, respectively. No statistical differences in nasal carriage of S. aureus and MRSA were detected relating to age, sex, exposure to hospitals, self reported disease, self reported antimicrobial therapy and health worker in household.
Table 2. Characteristics of S. aureus non-carriers and carriers in the two Ghanaian communities, 2011–2012.
| Characteristic | Category | Non-carriers (N = 463) | Carriers (N = 124) | Total (N = 587) | p-value |
| n (%) | n (%) | n (%) | |||
| Age (mean/sd) | 32.1 (22.1) | 29.8 (20.3) | 31.6 (21.8) | 0.2812 | |
| Sex | Female | 290 (62.6) | 80 (64.5) | 370 (63.0) | |
| Male | 173 (37.4) | 44 (35.5) | 217 (37.0) | 0.7790 | |
| Community | OS | 208 (44.9) | 26 (21.0) | 234 (39.9) | |
| KG | 255 (55.1) | 98 (79.0) | 353 (60.1) | <0.0001 | |
| EH | No | 285 (61.6) | 86 (69.4) | 371 (63.2) | |
| Yes | 178 (38.4) | 38 (30.6) | 216 (36.8) | 0.1350 | |
| SRD | No | 414 (89.4) | 116 (93.5) | 530 (90.3) | |
| Yes | 49 (10.6) | 8 (6.5) | 57 (9.7) | 0.2266 | |
| SRAT | No | 430 (92.9) | 116 (93.5) | 546 (93.0) | |
| Yes | 33 (7.1) | 8 (6.5) | 41 (7.0) | 0.9491 | |
| HWHH | No | 405 (87.5) | 106 (85.5) | 511 (87.1) | |
| Yes | 58 (12.5) | 18 (14.5) | 76 (12.9) | 0.6633 |
OS: Osudoku (rural); KG: Korle-gonno (urban); EH: exposure to hospitals; SRD: self-reported disease; SRAT: self-reported antimicrobial therapy; HWHH: healthcare worker in household.
Prevalence of Antimicrobial Resistance
Among the 124 S. aureus isolates, 113 (91%) were resistant to penicillin and 31 (25%) to tetracycline. Resistance to erythromycin, fusidic acid, norfloxacin and cefoxitin was below 5% (Table 3). The level of resistance to tetracycline was significantly higher in Osudoku (50%) compared to Korle Gonno (18%) (p = 0.0009), whereas there were no detectable differences for the remaining antimicrobials. All isolates were susceptible to clindamycin, trimethoprim-sulphamethoxazole, gentamicin, rifampicin, mupirocin, and linezolid. Seven (6%) isolates were MDR, with penicillin-tetracycline-norfloxacin (n = 5) being the predominant resistance profile.
Table 3. Percentage antimicrobial resistance in S. aureus isolated from nasal carriers in two Ghanaian communities, 2011–2012.
| Antimicrobial Agent | OS (N = 26) | KG (N = 98) | Total (N = 124) |
| n (%) | n (%) | n (%) | |
| Penicillin | 23 (88.4) | 90 (91.8) | 113 (91.0) |
| Tetracycline | 13 (50.0) | 18 (18.4) | 31 (25.0) |
| Fucidic acid | 1 (3.8) | 2 (2.0) | 3 (2.4) |
| Cefoxitin | 0 (0.0) | 2 (2.0) | 2 (1.6) |
| Erythromycin | 1 (3.8) | 1 (1.0) | 2 (1.6) |
| Norfloxacin | 0 | 6 (6.1) | 6 (4.8) |
OS: Osudoku (rural), KG: Korle Gonno (urban). No resistance was detected in both areas for Trimethoprim Sufamethozaxole, Clindamycin, Gentamicin, Rifampicin Mupirocin and Linezolid.
Only two isolates (1.6%; 2/124) were resistant to cefoxitin and confirmed to be MRSA by mecA PCR. Both MRSA isolates were susceptible to all non-beta lactam antimicrobials tested and originated from participants from Korle Gonno with a history of exposure to hospital environment within the last 12 months: a 60 years old male who declared to have taken antihypertensive drugs and a 27 years old female who reported usage of penicillin and other drugs she could not identify.
Genetic Diversity of S. aureus Isolates
The most prevalent among the 46 spa types found were t355, (CC152, 15%), t084 (CC15, 11%), t10519 (CC8, 10%), and t008 (CC8, 9%). Thirty-one singletons, including 10 new spa types (t10832, t10834, t10835, t10839 to t10845) were found among the isolates. Based on spa typing the following CCs were identified among the isolates: CC8 (n = 36), CC152 (n = 21), CC45 (n = 21), CC15 (n = 18), CC121 (n = 6), CC97 (n = 6), CC30 (n = 5), CC5 (n = 5), CC508 (n = 4), CC9 (n = 1), and CC707 (n = 1). Distributions of the most frequent spa types (t355, t084, t10519 and t008) and CCs (CC8, CC152, CC45, CC15 and CC121) differed significantly (p = 0.04 and p = 0.014, respectively) between Osudoku and Korle-gonno, and were not influenced by age and sex.
Thirty-four (27%) isolates were PVL-positive (Table 4), the majority of which belonged to CC152 (n = 15), CC15 (n = 7), CC30 (n = 3), CC121 (n = 3) and CC5 (n = 2). Among the four most frequent spa types, PVL was associated to t355 (CC152) (38%) and t084 (CC15) (15%) (p<0.01), while it was not detected in t008 (CC8) and t10519 (CC8). There was a two times increased risk of carrying a PVL-positive S. aureus in Osudoku (12/26, 46%) compared to Korle Gonno (22/98, 22%) (p = 0.03, 95% CI: 1.2–3.7). The two MRSA isolates were PVL-negative, displayed the same spa type (t5132) associated to ST508, and carried SCCmec type V.
Table 4. Distribution of spa types and PVL within each Staphylococcus aureus clonal complex (CC) detected in Osudoku (rural) and Korle Gonno (urban) communities in Ghana, 2011–2012.
| CC | Distribution of spa types | PVL frequency (N = 34) | |
| Osudoku (N = 26) | Korle Gonno (N = 98) | ||
| CC5 | Not detected | t10839(1), t311(3), t071(1) | 2/5 |
| CC8 | t1476(3), t10519(1) | t008(11), t1476(5), t10519(12), t10842(1) 10844(1), t197(1), t304(1) | 0/36 |
| CC9 | Not detected | t2700(1) | 0/1 |
| CC15 | t084(5) | t7568(1), t084(9), t346(1), t10843(1), t10845(1) | 7/18 |
| CC30 | t3194(1), t021(1) | t021(2), t363(1) | 3/5 |
| CC97 | t359(4) | t359(1) | 2/5 |
| Not detected | t044(1) | 0/1 | |
| CC45 | t861(1) | t2771(3), t5602(3), t6038(2), t1996(1) t065(1), t10834(1), t10840(1),t10841(1), t1510(1) t3986(1), t861(2), t939(1), t2784(1) t8453(1) | 1/21 |
| CC121 | t159(1), t2304(1) | t091(2), t4499(1), t645(1) | 3/6 |
| CC152 | t454(1), t355(6), t10835(1) | t454 (1), t355(12) | 15/21 |
| CC508 | Not detected | t5132(2), t10832(1) t6694 (1) | 0/4 |
| CC707 | Not detected | t1458(1) | 1/1 |
CC152 occurred more frequently among CA isolates than among CO isolates (p = 0.01), whereas CC8 was more common among CO isolates (p = 0.04) No other significant differences were observed in the occurrence of CCs among CA and CO isolates (Table 5).
Table 5. Distribution of spa types among community-onset (CO) and community-associated (CA) S. aureus isolates from the two Ghanian communities, 2011–2012.
| CC | Total no of isolates, N = 124 | CO isolates | N = 38 | CA isolates | N = 86 |
| n (%) | n (%) | n (%) | |||
| CC5 | 5 (4.0) | t071(1), t10839(1), t311(2) | 4 (10.5) | t311(1) | 1 (1.2) |
| CC8 | 36 (29.0) | t008(4), t10519(5), t10842(1), t1476(3), t304(1) | 14 (36.8) | t008(7), t10519(8), t10844(1), t1476(5), t197(1) | 22 (25.6) |
| CC9 | 1 (0.8) | t2700(1) | 1 (2.6) | - | 0 (0.0) |
| CC15 | 18 (14.5) | t084(3), t10843(1), t10845(1) t7568(1) | 6 (15.8) | t084(11), t346(1) | 12 (13.9) |
| CC30 | 5 (4.0) | t021(2) | 2 (5.2) | t021(1), t3194(1), t363(1) | 3 (3.5) |
| CC45 | 21 (16.9) | t10841(1), t6038(1), | 2 (5.2) | t065(1),t10834(1), t10840(1), t1510(1), t1996(1), t2771(3), t2784(1), t3986(1),t5602(3), t6038(1), t8453(1), t861(3), t939(1) | 19 (22.1) |
| CC97 | 6 (4.8) | t359(1), t044(1) | 2(5.2) | t359(4) | 4 (4.7) |
| CC121 | 6 (4.8) | t4499(1) | 1 (2.6) | t091(2), t159(1), t2304(1), t645(1) | 5 (5.8) |
| CC152 | 21 (16.9) | t10835(1), t454(2) | 4 (10.5) | t355(17) | 17 (19.7) |
| CC508 | 4 (3.2) | t5132(2) | 2 (5.4) | t10832(1), t6694(1) | 2 (2.3) |
| CC707 | 1 (0.8) | - | 0 (0.0) | t1458(1) | 1 (1.2) |
Discussion
We investigated the prevalence of nasal S. aureus carriage among healthy individuals in two communities representing urban and rural areas in Ghana. The overall prevalence of 21% is within the range (14–33%) of those previously reported in other African countries such as Nigeria [15], [31] and Gabon [16], [17]. Based on these data, the frequencies of S. aureus in African communities seems to resemble those obtained in communities of developed countries [6], [10], [12], even though carriage has been hypothesized to vary between different races [6], [32]. Interestingly, the frequency of nasal carriage among people from the urban community was significantly higher than among people from the rural community. This is apparently in contrast with recent study in Gabon, where S. aureus carriage was higher (37%) in subjects from rural areas than in subjects from semi-urban areas (21%) [17]. The different S. aureus carriage prevalence observed between urban and rural dwellers might be linked to specific socio-economic differences between the two communities. For example, inhabitants in the urban area live in overcrowded settlements compared to those in the rural area.
The prevalence of antimicrobial resistance was generally low with the only exception of penicillin resistance, which is widespread in human isolates of S. aureus worldwide [15], [32], [33]. One exception to this general rule is provided by a remote community of Pigmies in Gabon, where high susceptibility to penicillin (>60%) has recently been reported, probably as a consequence of a limited usage of antimicrobial agents in this population [16] . The significantly higher frequency of tetracycline resistance observed in this study in the rural community compared to the urban community could be correlated to veterinary use of tetracycline since this antibiotic is commonly used in livestock farming in Ghana [34], [35]. However, none of the S. aureus lineages found in this rural community is known to be livestock-associated. Possible associations with the use of tetracycline in this community could not be determined since regional data on antimicrobial consumption are not available. Antimicrobial usage might be higher than indicated by our questionnaire study considering the high rate of self-medication [36] and widespread usage of antimicrobial agents in Ghana and most African countries [37]–[39].
Carriage of MRSA (2/578) in the Ghanaian community was low (0.3%) and exclusively associated to urban participants recently exposed to hospitals. This is in line with the low prevalence (0.9%) of MRSA nasal carriage previously reported among inpatients and staff at the hospital in Ghana [22] and the lack of MRSA detection by previous studies conducted on remote communities in Africa [16]. High prevalence (27.5%) of presumptive MRSA was reported in a community study in Nigeria, a neighboring country [15]. It should however be noted that presumptive MRSA detected in the Nigerian study were not confirmed genotypically by PCR detection of mecA.
Both MRSA isolates detected in the urban community belonged to a rare spa type (t5132) associated to ST508. The two MRSA-positive individuals lived in the urban area. As they shared isolates with the same uncommon spa type, it cannot be excluded that the two cases were epidemiologically related. ST508 is a single locus variant of the Berlin epidemic clone ST45 [40]. Interestingly, ST508 was isolated among methicillin-susceptible isolates in the previous study on hospital carriage in Ghana [22], among clinical and community isolates in Gabon [17], [41] and Nigeria [20], [42], indicating that a reservoir of ST508 exists in these parts of Africa. The ST508 MRSA isolates shared the SCCmecV element often associated with CA-MRSA isolates [43], [44] but lacked PVL [43]. Two out of six MRSA isolated in the previous hospital carriage study in Ghana also harbored SCCmec V, whereas the remaining four isolates contained SCCmec types I or IV [22].
The population structure of S. aureus isolated from the two communities in Ghana was heterogeneous. Specific spa types such as t355 and t084 were frequent in this study as well as in the previous studies conducted among nasal carriers at the hospital in Korle Gonno (Korle Bu Teaching Hospital) [22] and clinical isolates from Ghanaian health care institutions [23], indicating that these lineages (CC152 and CC15, respectively) are widespread in Ghana. The predominant distribution of CC152 and CC15 in this study resembles what has been found in a nasal carrier study in Mali [14] and Gabon [41]. Some of the most common CCs (CC152, CC15 and CC8) and spa types (t355, t084 and t008) were commonly isolated from nasal carriers in the previous hospital study [22]. Within CC8, t10519 was relatively common in this study, especially in the urban community of Korle Gonno (12%), but was not detected in the local hospital [22], suggesting that this spa type is mainly restricted to the local community and has limited ability to spread inside the hospital. On the contrary, CC1 and CC88, which were detected among the nasal carriers in the hospital study in Ghana [22], were not detected in the community, indicating that these lineages may be associated with hospital environments in Ghana.
Noteworthy, t044, a widely disseminated spa type associated with MRSA ST80 in Middle East [45] and Europe [46], was isolated from an urban participant as MSSA. Further characterization by whole genome sequencing (data not shown) showed that this strain belonged to another lineage (ST669, CC97) not related to CC80. This phenomenon has been described for other spa types. For example, t037 has been associated with both CC8 (ST239) and CC30, probably as a result of chromosomal recombination within the variable region of spa [47], [48]. Thus, although good correlation between spa types and MLST CCs has been previously reported [48], the fact that MSSA isolates were only characterized by spa typing may be regarded as a limitation of the study, since this approach may not lead to accurate clonal identification at the ST and CC levels. However, this is a minor limitation as it does not influence the genotypic and phenotypic differences observed between the two communities.
The high frequency (27%) of PVL-positive isolates was anticipated as a similar trend was seen among nasal isolates from the Korle Bu hospital [22], clinical isolates from health care institution in Ghana [23] and in other African studies [14], [16], [20], [42]. The higher prevalence of PVL-positive isolates in the rural community mirrors the finding in a remote (rural) Gabonese community compared to urban populations [16] and is likely to reflect differences in the distribution of genetic lineages between the two communities.
To the best of our knowledge, this is the first study investigating carriage prevalence, antimicrobial resistance and clonal distribution of S. aureus in the Ghanaian community. The study reveals marked differences between an urban and a rural area with respect to carriage rate, tetracycline resistance, PVL content and clonal distribution. Even though the distribution of S. aureus clones differed significantly between the two communities, the difference was small and may not necessarily be biologically relevant. Further studies may be required to establish the socio-economic factors that may be responsible for the geographical differences observed between these two Ghanaian communities.
Acknowledgments
The chiefs and community members of the study areas are thanked for their support to the study. We are grateful to Stephen Osei-Wusu, Lone Ryste Kildevang Hansen, Julie Hindsberg Nielsen and David Kweku Egyir for their excellent technical assistance.
Funding Statement
This study was supported by Antibiotic Drug use, Monitoring and Evaluation of Resistance (ADMER), a project funded by the Danish International Development Agency (DANIDA). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Van Belkum A, Verkaik NJ, de Vogel CP, Boelens HA, Verveer J, et al. (2009) Reclassification of Staphylococcus aureus nasal carriage types. J Infect Dis 199: 1820–1826. [DOI] [PubMed] [Google Scholar]
- 2. Wertheim HFL, Melles DC, Vos MC, van Leeuwen W, van Belkum A, et al. (2005) The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect Dis 5: 751–762. [DOI] [PubMed] [Google Scholar]
- 3.Von Eiff C, Becker K, Machka K, Stammer H, Peters G, et al. (2001) Nasal Carriage as a Source of Staphylococcus aureus Bacteremia. N Engl J Med; 344, 11–16. [DOI] [PubMed]
- 4. Gorwitz RJ, Kruszon-Moran D, McAllister SK, McQuillan G, McDougal LK, et al. (2008) Changes in the prevalence of nasal colonization with Staphylococcus aureus in the United States, 2001–2004. J Infect Dis 197: 1226–1234. [DOI] [PubMed] [Google Scholar]
- 5. Aubry-Damon H, Grenet K, Sall-Ndiaye P, Che D, Cordeiro E, et al. (2004) Antimicrobial resistance in commensal flora of pig farmers. Emerg Infect Dis 10: 873–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Munckhof WJ, Nimmo GR, Schooneveldt JM, Schlebusch S, Stephens AJ, et al. (2009) Nasal carriage of Staphylococcus aureus, including community-associated methicillin-resistant strains, in Queensland adults. Clin Microbiol Infect 15: 149–155. [DOI] [PubMed] [Google Scholar]
- 7. Nakamura MM, Rohling KL, Shashaty M, Lu H, Tang YW, et al. (2002) Prevalence of methicillin-resistant Staphylococcus aureus nasal carriage in the community pediatric population. Pediatr Infect Dis J 21: 917–922. [DOI] [PubMed] [Google Scholar]
- 8. Rolo J, Miragaia M, Turlej-Rogacka A, Empel J, Bouchami O, et al. (2012) High genetic diversity among community-associated Staphylococcus aureus in Europe: results from a multicenter study. PLoS One 7: e34768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Scerri J, Monecke S, Borg MA (2013) Prevalence and characteristics of community carriage of methicillin-resistant Staphylococcus aureus in Malta. J Epidemiol Glob Health 3: 165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Skråmm I, Moen AEF, Bukholm G (2011) Nasal carriage of Staphylococcus aureus: frequency and molecular diversity in a randomly sampled Norwegian community population. APMIS 119: 522–528. [DOI] [PubMed] [Google Scholar]
- 11. Zanelli G, Sansoni A, Zanchi A, Cresti S, Pollini S, et al. (2002) Staphylococcus aureus nasal carriage in the community: a survey from central Italy. Epidemiol Infect 129: 417–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kluytmans J, van Belkum A, Verbrugh H (1997) Nasal carriage of Staphylococcus aureus: epidemiology, underlying mechanisms, and associated risks. Clin Microbiol Rev 10: 505–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Charlebois ED, Bangsberg DR, Moss NJ, Moore MR, Moss AR, et al. (2002) Population-based community prevalence of methicillin-resistant Staphylococcus aureus in the urban poor of San Francisco. Clin Infect Dis 34: 425–433. [DOI] [PubMed] [Google Scholar]
- 14. Ruimy R, Maiga A, Armand-Lefevre L, Maiga I, Diallo A, et al. (2008) The carriage population of Staphylococcus aureus from Mali is composed of a combination of pandemic clones and the divergent Panton-Valentine leukocidin-positive genotype ST152. J Bacteriol 190: 3962–3968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Onanuga A, Temedie TC (2011) Nasal carriage of multi-drug resistant Staphylococcus aureus in healthy inhabitants of Amassoma in Niger delta region of Nigeria. Afr Health Sci 11: 176–181. [PMC free article] [PubMed] [Google Scholar]
- 16. Schaumburg F, Köck R, Friedrich AW, Soulanoudjingar S, Ngoa UA, et al. (2011) Population structure of Staphylococcus aureus from remote African Babongo Pygmies. PLoS Negl Trop Dis 5: e1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ateba Ngoa U, Schaumburg F, Adegnika AA, Kösters K, Möller T, et al. (2012) Epidemiology and population structure of Staphylococcus aureus in various population groups from a rural and semi urban area in Gabon, Central Africa. Acta Trop 124: 42–47. [DOI] [PubMed] [Google Scholar]
- 18. David MZ, Daum RS (2010) Community-Associated Methicillin-Resistant Staphylococcus aureus: Epidemiology and Clinical Consequences of an Emerging Epidemic. Clin Microbiol Rev 23: 616–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lina G, Piémont Y, Godail-Gamot F, Bes M, Peter MO, et al. (1999) Involvement of Panton-Valentine leukocidin-producing Staphylococcus aureus in primary skin infections and pneumonia. Clin Infect Dis 29: 1128–1132. [DOI] [PubMed] [Google Scholar]
- 20. Shittu AO, Okon K, Adesida S, Oyedara O, Witte W, et al. (2011) Antibiotic resistance and molecular epidemiology of Staphylococcus aureus in Nigeria. BMC Microbiol 11: 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Okon KO, Basset P, Uba A, Lin J, Oyawoye B, et al. (2009) Cooccurrence of predominant Panton-Valentine leukocidin-positive sequence type (ST) 152 and multidrug-resistant ST 241 Staphylococcus aureus clones in Nigerian hospitals. J Clin Microbiol 47: 3000–3003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Egyir B, Guardabassi L, Nielsen SS, Larsen J, Addo KK, et al. (2013) Prevalence of nasal carriage and diversity of Staphylococcus aureus among inpatients and hospital staff at Korle Bu Teaching Hospital, Ghana. J Glob Antimicrob Resist.1 (4): 189–193. [DOI] [PubMed] [Google Scholar]
- 23. Egyir B, Guardabassi L, Sørum M, Nielsen SS, Kolekang A, et al. (2014) Molecular Epidemiology and Antimicrobial Susceptibility of Clinical Staphylococcus aureus from Healthcare Institutions in Ghana. PLoS One 9: e89716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Harmsen D, Claus H, Witte W, Claus H, Turnwald D, et al. (2003) Typing of Methicillin-Resistant Staphylococcus aureus in a University Hospital Setting by Using Novel Software for spa Repeat Determination and Database Management. J Clin Microbiol 41: 5442–5448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Fitzgibbon MM, Rossney AS, O’Connell B (2007) Investigation of reduced susceptibility to glycopeptides among methicillin-resistant Staphylococcus aureus isolates from patients in Ireland and evaluation of agar screening methods for detection of heterogeneously glycopeptide-intermediate S. aureus . J Clin Microbiol 45: 3263–3269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Magiorakos A, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, et al. (2011) Multidrug resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance Clin Microbiol Infect 2012. 18: 268–281. [DOI] [PubMed] [Google Scholar]
- 27. Larsen AR, Stegger M, Sørum M (2008) spa typing directly from a mecA, spa and pvl multiplex PCR assay–a cost-effective improvement for methicillin-resistant Staphylococcus aureus surveillance. Clin Microbiol Infect 14: 611–614. [DOI] [PubMed] [Google Scholar]
- 28. Enright MC, Day NP, Davies CE, Peacock SJ, Spratt BG (2000) Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus . J Clin Microbiol 38: 1008–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kondo Y, Ito T, Ma XX, Watanabe S, Kreiswirth BN, et al. (2007) Combination of multiplex PCRs for staphylococcal cassette chromosome mec type assignment: rapid identification system for mec, ccr, and major differences in junkyard regions. Antimicrob Agents Chemother 51: 264–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention (2011) Active Bacterial Core Surveillance Report, Emerging Infections Program Network, Methicillin- Resistant Staphylococcus aureus Available: http://www.cdc.gov/abcs/reports-findings/survreports/mrsa11.pdf.
- 31. Adesida SA, Abioye OA, Bamiro BS, Brai BIC, Smith SI, et al. (2007) Associated risk factors and pulsed field gel electrophoresis of nasal isolates of Staphylococcus aureus from medical students in a tertiary hospital in Lagos, Nigeria. Braz J Infect Dis 11: 63–69. [DOI] [PubMed] [Google Scholar]
- 32. Choi CS, Yin CS, Bakar AA, Sakewi Z, Naing NN, et al. (2006) Nasal carriage of Staphylococcus aureus among healthy adults. J Microbiol Immunol Infect 39: 458–464. [PubMed] [Google Scholar]
- 33. Du J, Chen C, Ding B, Tu J, Qin Z, et al. (2011) Molecular characterization and antimicrobial susceptibility of nasal Staphylococcus aureus isolates from a Chinese medical college campus. PLoS One 6: e27328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Annan-Prah A, Agbemafle E, Asare PT, Akorli SY (2012) Antibiotic use, abuse and their public health implication: The contributory role of management flaws in the poultry industry in two agro-ecological zones in Ghana. J Vet Adv 2(4): 199–208. [Google Scholar]
- 35. Donkor ES, Newman MJ, Yeboah-Manu D (2012) Epidemiological aspects of non-human antibiotic usage and resistance: implications for the control of antibiotic resistance in Ghana. Trop Med Int Health 17: 462–468. [DOI] [PubMed] [Google Scholar]
- 36. Donkor ES, Tetteh-Quarcoo PB, Nartey P, Agyeman IO (2012) Self-medication practices with antibiotics among tertiary level students in Accra, Ghana: a cross-sectional study. Int J Environ Res Public Health 9: 3519–3529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kimang’AN (2012) Review article: A situational analysis of antimicrobial drug resistance in africa: are we losing the battle? Ethiop J Health Sci 22: 2. [PMC free article] [PubMed] [Google Scholar]
- 38. Alabi AS, Frielinghaus L, Kaba H, Kösters K, Huson MAM, et al. (2013) Retrospective analysis of antimicrobial resistance and bacterial spectrum of infection in Gabon, Central Africa. BMC Infect Dis 13: 455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Newman MJ, Frimpong E, Donkor ES, Opintan JA, Asamoah-Adu A (2011) Resistance to antimicrobial drugs in Ghana. Infect Drug Resist 4: 215–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wannet WJB, Spalburg E, Heck MEOC, Pluister GN, Tiemersma E, et al. (2005) Emergence of Virulent Methicillin-Resistant Staphylococcus aureus Strains Carrying Panton-Valentine Leucocidin Genes in The Netherlands. J Clin Microbiol 43: 3341–3345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Schaumburg F, Ngoa UA, Kösters K, Köck R, Adegnika AA, et al. (2011) Virulence factors and genotypes of Staphylococcus aureus from infection and carriage in Gabon. Clin Microbiol Infect 17: 1507–1513. [DOI] [PubMed] [Google Scholar]
- 42. Ghebremedhin B, Olugbosi MO, Raji AM, Layer F, Bakare RA, et al. (2009) Emergence of a Community-Associated Methicillin-Resistant Staphylococcus aureus Strain with a Unique Resistance Profile in Southwest Nigeria. J Clin Microbiol 47: 2975–2980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. David MZ, Boyle-Vavra S, Zychowski DL, Daum RS (2011) Methicillin-susceptible Staphylococcus aureus as a predominantly healthcare-associated pathogen: a possible reversal of roles? PLoS One 6: e18217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Gillet Y, Issartel B, Vanhems P, Fournet J, Lina G, et al. (2002) Mechanisms of disease Association between Staphylococcus aureus strains carrying gene for Panton-Valentine leukocidin and highly lethal necrotising pneumonia in young immunocompetent patients. Lancet 359: 753–759. [DOI] [PubMed] [Google Scholar]
- 45. Tokajian ST, Khalil PA, Jabbour D, Rizk M, Farah MJ, et al. (2010) Molecular characterization of Staphylococcus aureus in Lebanon. Epidemiol Infect 138: 707–712. [DOI] [PubMed] [Google Scholar]
- 46. Deurenberg RH, Stobberingh EE (2009) The molecular evolution of hospital- and community-associated methicillin-resistant Staphylococcus aureus. . Curr Mol Med 9: 100–115. [DOI] [PubMed] [Google Scholar]
- 47. Koreen L, Ramaswamy SV, Graviss EA, Naidich S, Musser JM, et al. (2004) spa Typing Method for Discriminating among Staphylococcus aureus Isolates: Implications for Use of a Single Marker To Detect Genetic Micro- and Macrovariation. J Clin Microbiol 42: 792–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Strommenger B, Kettlitz C, Weniger T, Harmsen D, Friedrich AW, et al. (2006) Assignment of Staphylococcus isolates to groups by spa typing, SmaI macrorestriction analysis, and multilocus sequence typing. J Clin Microbiol 44: 2533–2540. [DOI] [PMC free article] [PubMed] [Google Scholar]