Abstract
Background/Context
A period of non-surgical management is advocated prior to surgical treatment for most patients with lumbar spinal stenosis. Currently, little evidence is available to define optimal non-surgical management. Physical therapy is often used, however its use and effectiveness relative to other non-surgical strategies has not been adequately explored.
Purpose
Describe the utilization of physical therapy and other non-surgical interventions by patients with lumbar spinal stenosis and examine the relationship between physical therapy and long-term prognosis.
Study Design
Secondary analysis of the Spine Patient Outcomes Research Trial (SPORT) combining data from randomized and observational studies.
Setting
13 spine clinics in 11 states in the United States.
Patient Sample
Patients with lumbar spinal stenosis receiving non-surgical management including those who did or did not receive physical therapy within 6 weeks of enrollment.
Outcome Measures
Primary outcome measures included cross-over to surgery, the bodily pain and physical function scales changes from the Survey Short Form 36 (SF-36), and the modified Oswestry Disability Index. Secondary outcome measures were patient satisfaction and the Sciatica Bothersomeness Index.
Methods
Baseline characteristics and rates of cross-over to surgery were compared between patients who did or did not receive physical therapy. Baseline factors predictive of receiving physical therapy were examined with logistic regression. Mixed effects models were used to compare outcomes between groups at 3 and 6 months, and 1 year after enrollment adjusted for baseline severity and patient characteristics.
Results
Physical therapy was used in the first 6 weeks by 90 of 244 patients (37%) and was predicted by the absence of radiating pain and being single instead of married. Physical therapy was associated with a reduced likelihood of cross-over to surgery after 1 year (21% vs 33%, p=0.045), and greater reductions on the SF-36 physical functioning scale after 6 months (mean difference =6.0, 95% CI: 0.2, 11.7) and 1 year (mean difference =6.5, 95% CI: 0.6, 12.4). There were no differences in bodily pain or Oswestry scores across time.
Conclusion
Many patients with lumbar spinal stenosis pursuing conservative management receive physical therapy. Using physical therapy was associated with reduced likelihood of patients receiving surgery within 1 year. Results for other outcomes were mixed with no differences in several measures. Further research is needed to examine the effectiveness of physical therapy relative to other non-surgical management strategies for patients with lumbar spinal stenosis.
INTRODUCTION
Lumbar spinal stenosis is a degenerative condition of the lumbar spine that is a common source of pain and diminished quality of life in those over age 50. The prevalence of lumbar spinal stenosis based on imaging criteria is estimated to be almost 50% in individuals over age 60, although not all cases are symptomatic.1,2 Advances in the sensitivity of diagnostic imaging technology combined with the aging of the population in many countries will likely result in continued growth in the number of patients diagnosed with lumbar spinal stenosis.
Considering the pervasiveness of lumbar spinal stenosis among older adults, there is a surprising lack of clarity and consensus regarding the most effective management strategies. The natural history of lumbar spinal stenosis without interventions is not well-described, however it appears that many affected individuals remain stable or improve over time.3 It is generally agreed that a period of conservative management is an appropriate initial strategy.4,5 Various conservative approaches have been advocated, including watchful waiting, medications, physical therapy and epidural injections,6,7 however there is little evidence to guide the choice of a conservative option.8 Many patients pursuing conservative management for lumbar receive physical therapy.9,10 The value of this approach relative to other options is unclear.
Development of an optimal conservative management strategy for patients with lumbar spinal stenosis is hindered by several factors. There is little descriptive research available to characterize the conservative options currently being used by patients across the United States. Physical therapy is frequently advocated as an important aspect of conservative management.11–14 Little is currently known about the degree of utilization of physical therapy or patient-related factors associated with the use of physical therapy. Finally, the relationship between the use of conservative options, including physical therapy, and prognosis with conservative management has been largely unexamined. Exploring how various conservative treatment choices relate to prognosis may provide insights into strategies worthy of further research.
The Spine Patient Outcomes Research Trial (SPORT), a multi-center study conducted at 13 sites across the United States, provides an opportunity to examine the approaches to conservative management chosen by patients with lumbar spinal stenosis and to evaluate the relationship between these choices and prognosis. The SPORT design included both a randomized and a concurrent observational cohort of patients with lumbar spinal stenosis that used identical inclusion criteria and assessment procedures.15 The combined results of the two cohorts showed significantly more improvement in patients treated surgically, though some patients who were either randomized to, or chose, conservative management experienced improvement and were satisfied with their care.16,17 Patients in the conservative arms of the SPORT study were treated using “usual care” defined as providing recommendations for active physical therapy, education or counseling with home exercise instruction, and/or non-steroidal anti-inflammatory medication (NSAIDs);16 however, no standardized protocol was used. The ultimate choice of conservative options was therefore at the discretion of the physician and patient, with the specific treatments used by patients systematically tracked.15
The goal of this study was to perform a secondary analysis of patients with lumbar spinal stenosis who were in the conservative arms of SPORT in order to describe the utilization of physical therapy by patients with lumbar spinal stenosis, and examine the relationship to long-term prognosis. Specifically, the purposes of this study were to: 1) evaluate the utilization of physical therapy as an initial conservative management strategy; 2) explore the factors associated with receiving physical therapy for initial conservative management; and 3) examine the relationship between receiving physical therapy as an initial conservative management strategy and long-term (1-year) outcomes.
MATERIALS and METHODS
Subjects
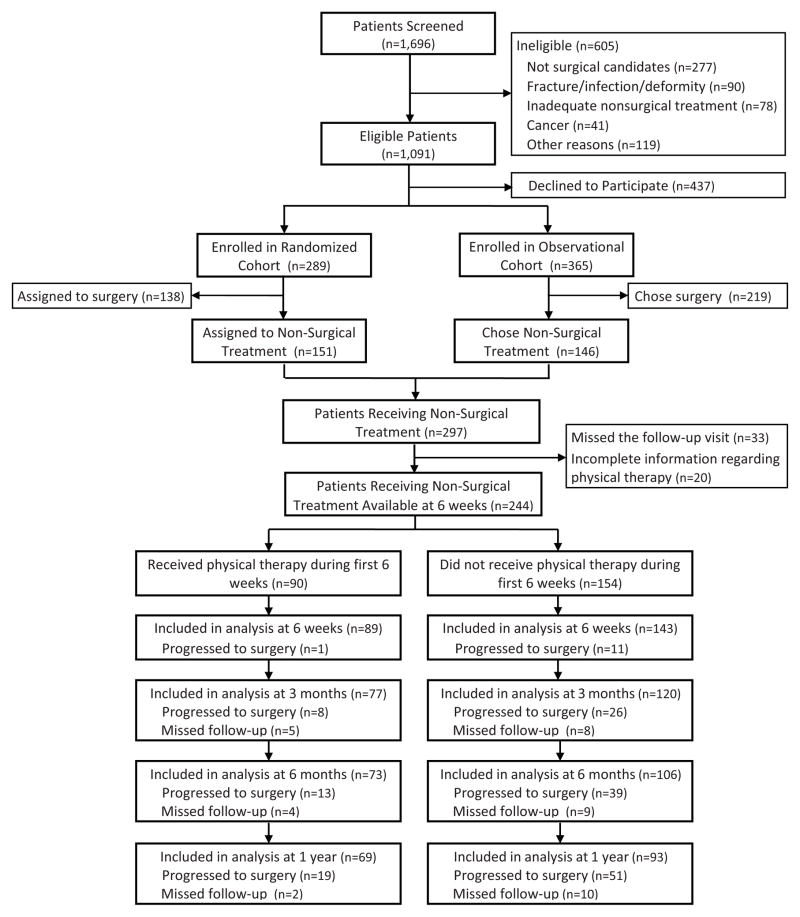
Inclusion criteria for participation in the SPORT study were symptoms of neurogenic claudication (pain in the buttock, thigh, or leg during ambulation that improves with rest) or radicular leg symptoms with associated neurological deficits on the physical examination for at least 12 weeks. Confirmatory cross-sectional magnetic resonance imaging (MRI) or computed tomography (CT) imaging demonstrating the presence of either central or lateral lumbar spinal stenosis at one or more levels was required. Patients were ineligible if there was radiographic evidence of instability, degenerative spondylolisthesis, fracture, or scoliosis of more than 15°. Additional exclusion criteria included co-morbid health conditions precluding surgical management, prior lumbar surgery, progressive neurological deficit, or indication of a potential non-musculoskeletal spinal condition (e.g., active malignancy, infection, etc.) For this analysis only subjects who were in the conservative arm of the SPORT study were included. The SPORT study enrolled a total of 654 patients. Of these 654 patients, 297 were in the conservative arm; 151 from the randomized cohort, and 146 from the the observational cohort (Figure 1).
Figure 1.
Screening, Exclusion, Enrollment, Randomization and Follow-up of SPORT patients included in the analysis of the impact on outcomes of physical therapy in the first six weeks of SPORT enrollment.
Conservative Management
Clinical sites participating in the SPORT study were encouraged to recommend that patients in the conservative cohort consider physical therapy, education/counseling with home exercise instruction, and NSAID medication as initial management strategies. Patients in the conservative cohort could receive any additional conservative treatments deemed appropriate by their physician. Participating clinical sites were encouraged to aggressively pursue conservative interventions if the recommended initial management strategies were not effective.15 The actual treatments received by patients in the conservative cohort, including crossover to surgical treatment, were recorded at each follow-up assessment. The actual treatments received during the initial six weeks after enrollment were used to divide the conservative cohort into those who received physical therapy as an initial management approach versus those who did not receive physical therapy.
Outcome Measurements
Outcome assessments were completed at 6-weeks, 3 months, 6 months, and 1-year following enrollment. Primary outcomes included cross-over to surgical treatment as well as the SF-36 version 1 Health Status Measure,18 a generic health-status measure, and the Oswestry Disability Index (ODI),19 a disease-specific measure of disability attributable to low back pain. These measures were chosen based on recommendations in the literature.20 From the SF-36, the bodily pain and physical functioning subscales were used. Each of these subscales is scored on a 0–100 scale with higher scores indicating better health. The ODI is scored from 0–100 with higher numbers indicating greater disability. Secondary outcomes used were the Stenosis Bothersomeness Index, a 0–24 scale, with higher scores indicating more bothersome symptoms.20 The Index is calculated as the sum of separate 0–6 bothersomeness ratings for leg symptoms of pain, weakness, numbness, and pain after walking. Patient self-ratings of satisfaction with symptoms and degree of progress were also recorded.
Funding
The original SPORT study was funded by a 13.5 million dollar grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health. No funding was received in support of the analyses presented in this manuscript. No benefits have been or will be received from a commercial party related directly or indirectly to the subject of this article.
Data Analysis
Initial analyses compared baseline characteristics of patients in the conservative cohort who did or did not receive physical therapy as an initial management approach during the first 6 weeks after enrollment. Baseline factors associated with receiving physical therapy during the first six weeks were examined using stepwise logistic regression. Criterion for entry was a significance level of p<0.10, and p<0.05 was required for retention in the final model. Variables considered for entry into the model included the demographic characteristics, co-morbid health conditions, baseline outcome measure scores, treatment preference and physical examination findings listed in Table 1. Rates of cross-over to surgical treatment within 1 year after enrollment were compared between patients who did or did not receive physical therapy during the initial six weeks using a chi-square statistic. Comparison of outcomes between patients who did or did not receive physical therapy during the first six weeks were performed by evaluating the change from baseline to each follow-up assessment using a mixed-effects model of longitudinal regression including a random individual effect to account for the correlation between repeated measurements from the same patient. Analysis was based on available data from patients continuing with conservative management; therefore, the outcomes data for patients crossing over to surgical management were included from baseline to follow-up assessments before surgery, but were censored from the analyses for assessments occurring post-surgery. Adjustments were made for center, age, gender, baseline score, income, treatment preference, duration of symptoms, compensation, marital status, pain radiation, smoking status, BMI, baseline Sciatica Bothersomeness, and co-morbid health conditions. Computations were done using SAS procedures PROC MIXED for continuous data with normal random effects, and PROC GENMOD for binary and non-normal secondary outcomes, software version 9.1 (SAS Institute Inc, Cary, NC). Statistical significance was defined as p <.05 based on a 2-sided hypothesis test. No adjustments were made for multiple comparisons.
Table 1. Baseline Demographic Characteristics for Included and Excluded Patients.
(Other comorbidities include: stroke, cancer, fibromyalgia, chronic fatigue syndrome, post-traumatic stress disorder, alcohol/drug dependency, lung, liver, kidney, blood vessel, nervous system, migraine, anxiety)
| Included in Analysis (n=244) | Not Included in Analysis (n=53) | p-value | |
|---|---|---|---|
| Age | 66.5 (10.4) | 63.5 (10.0) | 0.06 |
| Sex (female) | 97 (40%) | 19 (36%) | 0.71 |
| Body Mass Index | 29.3 (5.8) | 29.2 (5.9) | 0.91 |
| Race (white) | 214 (88%) | 40 (75%) | 0.04 |
| Education (at least some college) | 155 (64%) | 32 (60%) | 0.78 |
| Marital Status (married) | 169 (69%) | 40 (75%) | 0.46 |
| Work Status | |||
| Full or part-time | 79 (32%) | 16 (30%) | 0.87 |
| Retired | 123 (50%) | 24 (45%) | 0.54 |
| Other | 42 (17%) | 13 (25%) | 0.24 |
| Compensation (receiving any) | 17 (7%) | 5 (9%) | 0.74 |
| Current Smoker (yes) | 23 (9%) | 5 (9%) | 0.80 |
| Co-Morbidities | |||
| Hypertension | 109 (45%) | 24 (45%) | 0.94 |
| Diabetes | 39 (16%) | 9 (17%) | 0.98 |
| Osteoporosis | 30 (12%) | 3 (6%) | 0.25 |
| Heart Problem | 68 (28%) | 11 (21%) | 0.34 |
| Stomach Problem | 54 (22%) | 17 (32%) | 0.17 |
| Depression | 25 (10%) | 6 (11%) | 0.99 |
| Other‡ | 85 (35%) | 20 (38%) | 0.09 |
| Treatment Prior to Enrollment | |||
| Physical Therapy (yes) | 174 (71%) | 33 (62%) | 0.26 |
| Injection (yes) | 130 (53%) | 27 (51%) | 0.88 |
| Symptom Duration (> 6 months) | 127 (52%) | 35 (66%) | 0.09 |
| SF-36 – Bodily Pain | 39.0 (20.7) | 37.6 (21.6) | 0.66 |
| SF-36 – Physical Functioning | 39.9 (25.3) | 37.7 (21.6) | 0.57 |
| Oswestry Disability Index | 37.8 (18.6) | 39.2 (17.3) | 0.63 |
| Stenosis Bothersomeness Index | 13.2 (5.6) | 14.1 (6.0) | 0.31 |
| Back Pain Bothersomeness | 3.9 (1.7) | 4.0 (1.9) | 0.70 |
| Leg Pain Bothersomeness | 4.1 (1.7) | 4.4 (1.4) | 0.15 |
| Treatment Preference | |||
| Non-Surgical | 151 (62%) | 31 (58%) | 0.64 |
| Surgical | 38 (16%) | 10 (19%) | 0.54 |
| Not Sure | 54 (22%) | 12 (23%) | 0.99 |
| Radiating Symptoms Present | 193 (79%) | 44 (83%) | 0.65 |
| Pseudoclaudication Present | 197 (81%) | 42 (79%) | 0.95 |
| Any Neurological Deficit (reflex, sensory or motor) | 150 (61%) | 29 (55%) | 0.45 |
| Stenosis Levels | |||
| L2 – L3 | 66 (27%) | 12 (23%) | 0.63 |
| L3 – L4 | 164 (67%) | 33 (62%) | 0.60 |
| L4 – L5 | 226 (93%) | 47 (89%) | 0.50 |
| L5 – S1 | 72 (30%) | 17 (32%) | 0.84 |
| Stenosis Levels (mod/severe) | |||
| None | 8 (3%) | 2 (4%) | 0.39 |
| One | 85 (35%) | 21 (40%) | 0.86 |
| Two | 105 (41%) | 18 (34%) | 0.53 |
| Three or more | 46 (19%) | 12 (23%) | 0.57 |
| Stenosis Locations | |||
| Central | 210 (86%) | 49 (92%) | 0.30 |
| Lateral Recess | 187 (77%) | 38 (72%) | 0.56 |
| Neuroforamen | 88 (36%) | 16 (30%) | 0.51 |
| Stenosis Severity | |||
| Mild | 8 (3%) | 2 (3%) | 0.39 |
| Moderate | 112 (46%) | 29 (55%) | 0.29 |
| Severe | 124 (51%) | 22 (42%) | 0.23 |
RESULTS
Of the 297 patients in the conservative cohort, 244 (82%) had complete data regarding physical therapy utilization at the 6-week follow-up and are included in the analyses (Figure 1). Compared to patients included in the analyses, those who were excluded (n=53) did not differ on any baseline examination or demographic characteristics with the exception of race; with a higher percentage of non-white patients among excluded patients (25% versus 12%, p=0.04). A summary of baseline variables for included and excluded patients is provided in Table 1. Ninety (37%) of these 244 patients received physical therapy during the initial six weeks following enrollment. Of those receiving physical therapy, 27 (30%) attended 2 or fewer sessions, 42 (47%) attended between 3 – 10 sessions, and 21 (23%) attended more than 10 sessions. There were few baseline differences between patients who did or did not receive physical therapy during the initial six weeks on either baseline demographic or examination characteristics (Table 2). The group that did not receive physical therapy were more likely to have radiating pain (i.e., pain extending below the knee) at baseline (p=0.005), and more likely to have a preference for surgical treatment at baseline (p=0.028). The utilization of various conservative treatments during the first six weeks following enrollment is outlined in Table 3. The only significant difference between groups was that patients who received physical therapy were more likely to consult with a surgeon during the initial six weeks (p<0.001). Logistic regression analysis examining factors associated with receiving physical therapy within the first six weeks retained two variables in the final model: pain radiation and marital status. Patients without pain radiation were more likely to receive physical therapy (adjusted odds ratio = 2.71 (95% CI: 1.40, 5.27) p = 0.003). Patients who were married were less likely than single patients to receive physical therapy (adjusted odds ratio = 0.29 (95% CI: 0.09, 0.90) p = 0.032).
Table 2. Baseline Demographic Characteristics for Included Patients Based on Physical Therapy Use.
(Other comorbidities include: stroke, cancer, fibromyalgia, chronic fatigue syndrome, post-traumatic stress disorder, alcohol/drug dependency, lung, liver, kidney, blood vessel, nervous system, migraine, anxiety)
| Had Physical Therapy During the First 6 Weeks (n=90) | No Physical Therapy During the First 6 Weeks (n=154) | p-value | |
|---|---|---|---|
| Age | 66.9 (11.8) | 66.3 (9.5) | 0.67 |
| Sex (female) | 36 (40%) | 61 (40%) | 0.94 |
| Body Mass Index | 29.1 (6.3) | 29.4 (5.6) | 0.66 |
| Race (white) | 80 (89%) | 134 (87%) | 0.82 |
| Education (at least some college) | 61 (68%) | 94 (61%) | 0.36 |
| Marital Status (married) | 56 (62%) | 113 (73%) | 0.093 |
| Work Status | |||
| Full or part-time | 25 (28%) | 54 (35%) | 0.24 |
| Retired | 50 (56%) | 73 (47%) | 0.22 |
| Other | 15 (16%) | 27 (18%) | 0.86 |
| Compensation (receiving any) | 3 (3%) | 15 (10%) | 0.15 |
| Current Smoker (yes) | 8 (9%) | 15 (10%) | 0.99 |
| Co-Morbidities | |||
| Hypertension | 39 (43%) | 70 (45%) | 0.85 |
| Diabetes | 17 (19%) | 22 (14%) | 0.44 |
| Osteoporosis | 13 (14%) | 17 (11%) | 0.56 |
| Heart Problem | 21 (23%) | 48 (31%) | 0.24 |
| Stomach Problem | 17 (19%) | 37 (24%) | 0.44 |
| Depression | 6 (7%) | 19 (12%) | 0.23 |
| Other‡ | 29 (32%) | 56 (36%) | 0.61 |
| Treatment Prior to Enrollment | |||
| Physical Therapy (yes) | 64 (71%) | 110 (71%) | 0.93 |
| Injection (yes) | 41 (46%) | 89 (58%) | 0.086 |
| Symptom Duration (> 6 months) | 42 (47%) | 85 (55%) | 0.25 |
| SF-36 – Bodily Pain | 37.6 (18.2) | 39.8 (22.1) | 0.42 |
| SF-36 – Physical Functioning | 39.5 (24.7) | 40.1 (25.6) | 0.87 |
| Oswestry Disability Index | 38.7 (18.1) | 37.3 (18.9) | 0.58 |
| Stenosis Bothersomeness Index | 12.9 (5.6) | 13.4 (5.6) | 0.45 |
| Back Pain Bothersomeness | 4.0 (1.7) | 3.8 (1.8) | 0.58 |
| Leg Pain Bothersomeness | 3.9 (1.8) | 4.2 (1.7) | 0.27 |
| Treatment Preference | |||
| Non-Surgical | 62 (69%) | 89 (58%) | 0.085 |
| Surgical | 8 (9%) | 30 (19%) | 0.028 |
| Not Sure | 20 (22%) | 35 (23%) | 0.93 |
| Radiating Symptoms Present | 62 (69%) | 131 (85%) | 0.005 |
| Pseudoclaudication Present | 69 (77%) | 128 (83%) | 0.29 |
| Any Neurological Deficit (reflex, sensory or motor) | 53 (59%) | 97 (63%) | 0.62 |
| Stenosis Levels | |||
| L2 – L3 | 26 (29%) | 40 (26%) | 0.73 |
| L3 – L4 | 62 (69%) | 102 (66%) | 0.78 |
| L4 – L5 | 80 (89%) | 146 (95%) | 0.15 |
| L5 – S1 | 26 (29%) | 46 (30%) | 0.99 |
| Stenosis Levels (mod/severe) | |||
| None | 3 (3%) | 5 (3%) | 0.97 |
| One | 32 (36%) | 53 (34%) | 0.86 |
| Two | 37 (41%) | 68 (44%) | 0.64 |
| Three or more | 18 (20%) | 28 (18%) | 0.73 |
| Stenosis Locations | |||
| Central | 77 (86%) | 133 (86%) | 0.99 |
| Lateral Recess | 63 (70%) | 124 (81%) | 0.086 |
| Neuroforamen | 32 (36%) | 56 (36%) | 0.99 |
| Stenosis Severity | |||
| Mild | 3 (3%) | 5 (3%) | 0.97 |
| Moderate | 46 (51%) | 66 (43%) | 0.21 |
| Severe | 41 (46%) | 83 (54%) | 0.21 |
Table 3.
Non-Surgical Treatments Received During the First 6 Weeks after Enrollment
| Had Physical Therapy During the First 6 Weeks (n=90) | No Physical Therapy During the First 6 Weeks (n=154) | p-value | |
|---|---|---|---|
| Providers/Services/Treatments | |||
| Education/Counseling | 13 (15%) | 12 (8%) | 0.17 |
| Emergency Room Visits | 5 (6%) | 6 (4%) | 0.78 |
| Surgeon | 28 (31%) | 20 (13%) | 0.001 |
| Other physician (Internist, Neurologist, etc.) | 46 (51%) | 76 (49%) | 0.89 |
| Chiropractor | 9 (10%) | 5 (3%) | 0.057 |
| Acupuncturist | 4 (4%) | 6 (4%) | 0.99 |
| Injections | 27 (30%) | 52 (34%) | 0.64 |
| Activity Restriction | 3 (3%) | 7 (5%) | 0.88 |
| Other | 18 (20%) | 36 (23%) | 0.65 |
| Medications | |||
| NSAIDs | 34 (38%) | 42 (27%) | 0.12 |
| Cox inhibitors | 34 (38%) | 47 (31%) | 0.31 |
| Oral Steroids | 1 (1%) | 2 (1%) | 0.64 |
| Narcotics | 21 (23%) | 36 (23%) | 0.88 |
| Muscle Relaxants | 4 (4%) | 5 (3%) | 0.90 |
| Other Medications | 45 (50%) | 75 (49%) | 0.95 |
| Devices | |||
| Brace/Corset | 2 (2%) | 6 (4%) | 0.48 |
| Magnets | 3 (3%) | 1 (1%) | 0.28 |
| Shoe Inserts | 3 (3%) | 5 (3%) | 0.74 |
| TENS Machine | 0 | 0 | - |
| Orthopedic Pillow | 7 (8%) | 3 (2%) | 0.059 |
Cross over to surgical management occurred during the first year for a total of 70 patients (29%) originally in the conservative cohort. Nineteen of these patients (21%) had received physical therapy during the first six weeks, and 51 (33%) had not received physical therapy during the initial six week post-enrollment (p = 0.045). Comparisons of outcomes for patients who did or did not receive physical therapy during the initial six weeks are summarized in Table 4 and Figures 2 and 3. There were higher levels of patient self-rated major improvement at 3 months (between-group difference = 23.5%, 95% CI: 9.9, 37.1), 6 months (between-group difference = 19.1%, 95% CI: 4.4, 33.7), and 1-year (between-group difference = 25.4%, 95% CI: 10.8, 40.1) in the group receiving physical therapy during the initial six weeks. The group receiving physical therapy also had a greater reduction in leg pain bothersomeness after 1 year (between-group difference = 0.7, 95% CI: 0.1, 1.3), and greater reductions in the SF-36 physical functioning subscale after 6 months (between-group difference =6.0, 95% CI: 0.2, 11.7) and 1 year (between-group difference =6.5, 95% CI: 0.6, 12.4). The global hypothesis tests comparing the primary and secondary outcome measures between groups across all follow-up periods found significant differences favoring the group receiving physical therapy for the outcome of the physical functioning subscale of the SF-36 (p = 0.014) (Figure 2), and the patient self-rating of major improvement (p < 0.001) (Figure 3).
Table 4.
Primary and secondary outcomes for patients who received or did not receive physical therapy during the first 6 weeks after enrollment across the follow-up assessments. Values represent mean change from baseline (standard error) or percentages. Values have been adjusted for center, age, sex, baseline score, income, treatment preference, duration of symptoms, compensation status, marital status, pain radiation, smoking status, BMI, baseline stenosis bothersomeness, joint, stomach and bowel disorders. NA indicates data was not assessed at the assessment
| Outcome | 6 Weeks | 3 Months | 6 Months | 1 Year | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of patients | PT 89 | No PT 143 | Treatment Effect (95% CI) | p-value | PT 77 | No PT 120 | Treatment Effect (95% CI) | p-value | PT 73 | No PT 106 | Treatment Effect (95% CI) | p-value | PT 69 | No PT 93 | Treatment Effect (95% CI) | p-value |
| SF-36 Bodily Pain | 7.1 (2.3) | 9.2 (1.8) | −2.2 (−8.0, 3.7) | 0.47 | 11.1 (2.4) | 10.7 (1.9) | 0.40 (−5.7, 6.5) | 0.89 | 12.9 (2.4) | 9.8 (2.0) | 3.1 (−3.1, 9.4) | 0.33 | 14.2 (2.4) | 11.4 (2.1) | 2.8 (−3.7, 9.2) | 0.40 |
| SF-36 Physical Function | 9.3 (2.1) | 4.5 (1.7) | 4.8 (−0.6, 10.1) | 0.08 | 10.7 (2.2) | 5.6 (1.7) | 5.2 (−0.4, 10.8) | 0.07 | 11.0 (2.2) | 5.1 (1.8) | 6.0 (0.2, 11.7) | 0.04 | 11.3 (2.2) | 4.8 (1.9) | 6.5 (0.6, 12.4) | 0.03 |
| Oswestry Disability Index (0–100) | −5.5 (1.7) | −3.6 (1.3) | −1.8 (−6.2, 2.6) | 0.42 | −7.2 (1.8) | −4.0 (1.4) | −3.2 (−7.8, 1.3) | 0.16 | −8.6 (1.8) | −4.8 (1.5) | −3.8 (−8.5, 0.8) | 0.11 | −8.2 (1.8) | −5.1 (1.5) | −3.1 (−7.9, 1.6) | 0.20 |
| Stenosis Bother- someness Index (0–24) | NA | NA3 | NA3 | NA3 | −3.0 (0.71) | −1.7 (0.56) | −1.2 (−3.0, 0.6) | 0.19 | NA | NA3 | NA3 | NA3 | −4.6 (0.72) | −2.6 (0.62) | −2.0 (−3.9, −0.1) | 0.04 |
| Leg Pain Bother- someness (0–6) | NA3 | NA3 | NA3 | NA3 | −0.8 (0.2) | −0.8 (0.2) | 0.0 (−0.5, 0.6) | 0.93 | NA3 | NA3 | NA3 | NA3 | −1.7 (0.2) | −0.9 (0.2) | −0.7 (−1.3, −0.1) | 0.02 |
| Low Back Pain Bothersomeness (0–6) | NA3 | NA3 | NA3 | NA3 | −0.8 (0.2) | −0.9 (0.1) | 0.0 (−0.4, 0.5) | 0.85 | NA3 | NA3 | NA3 | NA3 | −1.0 (0.2) | −0.9 (0.2) | −0.1 (−0.6, 0.4) | 0.66 |
| Very/Somewhat Satisfied with Symptoms (%) | 19.4% | 23.7 % | −4.3 (−15.8, 7.1) | 0.45 | 30.0 % | 27.5 % | 2.6 (−11.2, 16.4) | 0.70 | 33.7% | 30.5% | 3.2 (−11.6, 18.1) | 0.66 | 43.1% | 28.7% | 14.5 (−1.3, 30.2) | 0.08 |
| Self-Rated Progress: Major Improvement (%) | 27.5% | 19.5 % | 8.0 (−4.3, 20.2) | 0.18 | 39.4 % | 15.9 % | 23.5 (9.9, 37.1) | <0.001 | 41.2% | 22.1% | 19.1 (4.4, 33.7) | 0.007 | 43.1% | 17.7% | 25.4 (10.8, 40.1) | 0.001 |
| Opioid Use (%) | 19.5% | 14.5 % | 5.0 (−5.8, 15.7) | 0.36 | 13.4 % | 12.5 % | 0.9 (−9.0, 10.7) | 0.86 | 8.1% | 16.4% | −8.3 (−17.8, 1.1) | 0.083 | 13.2% | 9.7% | 3.5 (−6.3, 13.4) | 0.45 |
Figure 2.
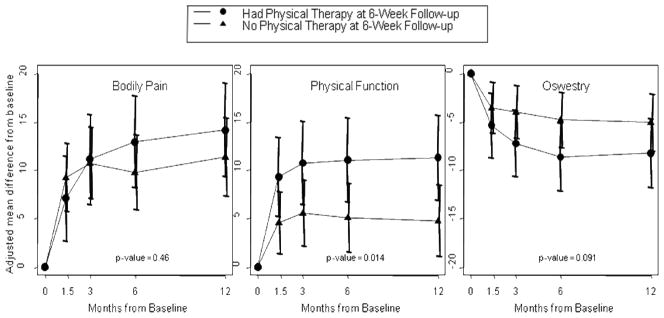
Primary outcomes for patients who received or did not receive physical therapy during the first six weeks after enrollment during 1 year of follow-up. Graphs show adjusted mean change from baseline. Bodily pain and physical function scores from the SF-36 range from 0–100 with higher scores indicating less severe symptoms. The Oswestry index ranges from 0–100 with lower scores indicating less disability. Horizontal bars represent 95% confidence intervals. P-values are time-weighted average 1-year area under curve p-values.
Figure 3.
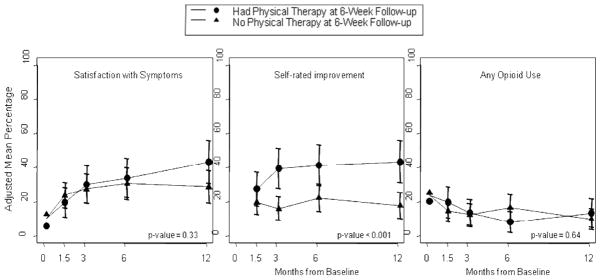
Secondary outcomes for patients who received or did not receive physical therapy during the first six weeks after enrollment during 1 year of follow-up. Graphs show adjusted mean percentages for each outcome. Horizontal bars represent 95% confidence intervals. P-values are time-weighted average 1-year area under curve p-values.
DISCUSSION
The results of this secondary analysis of the SPORT study provide information on the utilization of physical therapy by patients with lumbar spinal stenosis receiving conservative management in a nationally-representative cohort. Associations between receiving physical therapy in the initial six weeks after enrollment in the SPORT study and long-term outcomes were identified. The results of this study appear to be consistent with the observations of others describing current patterns of conservative management of patients with lumbar spinal stenosis in the United States as encompassing a mix of interventions, medications and procedures.21 Receiving physical therapy within the first six weeks after enrollment in the SPORT study was associated with a lower rate of progression to surgery over the 1-year follow-up period. Other outcomes evaluated including the Oswestry Disability Index, bodily pain and rates of opioid use did not differ based on physical therapy use.
The most common conservative treatments received during the first six weeks after enrollment in this analysis were medications (particularly non-steroidal medications and opioids), physical therapy, and injections; as well as visits to surgeons or other physicians. There are few reports in the literature documenting the prevalence of specific conservative treatment options used by patients with lumbar spinal stenosis in a large sample of patients from multiple sites across the United States. The Maine Lumbar Spine Study (MLSS),22 conducted in one geographic region (the state of Maine) in the early 1990’s, provides some information for comparison. The 69 patients choosing conservative management in the MLSS reported a higher utilization of activity restriction (specifically bed rest, 29%), and lower utilization of physical therapy (23%) and epidural injections (18%) over a 1-year time frame following enrollment,23 compared with 4%, 37%, and 32%, respectively in the SPORT study patients. These differences may reflect a regional pattern and/or a small sample size; however, they appear consistent with the emergence of evidence over the past 2 decades of the detrimental effects of bed rest.24 Differences also appear to reflect reported trends towards increased use of spinal injections for back pain in older adults,25,26 and increasing use of physical therapy for back pain27 in the time period between these studies. Higher utilization of physical therapy for patients with lumbar spinal stenosis is also reflected in the treatments sought by patients in the SPORT study prior to enrollment.10 Considering all patients with lumbar spinal stenosis entering the SPORT study, the utilization of physical therapy was approximately 70%.
The utilization of physical therapy as an aspect of the initial post-enrollment management strategy by 37% of patients in SPORT study who were either randomized to or chose to pursue conservative management may be biased towards an overestimation by the fact that surgeons participating in the SPORT trial were encouraged to recommend physical therapy to patients in the conservative cohort. A recent large study of 439,195 Medicare enrollees with back pain due to various diagnoses reported a lower utilization rate of physical therapy (16.2%) over a 1-year period from the physician encounter, with a high degree of variability based on the specialty of the physician seen for the initial visit.28 Similar to the current study, an association was found between lower rates of surgery and receiving physical therapy;28 however, both studies used observational designs that preclude conclusions on the effectiveness of physical therapy as a management strategy.
We found mixed results with respect to the potential benefit of physical therapy on outcomes for patients with lumbar spinal stenosis. Receiving physical therapy was associated with greater improvement in physical functioning, a reduced likelihood of receiving surgery, and a higher likelihood of a patient self-rating of major improvement over a 1-year follow-up period. The percentage of patients receiving surgery was 12% lower, and the percentage noting major improvement was 16% higher after 1 year among patients receiving physical therapy. Differences in the physical function subscale of the SF-36 exceeded the minimum clinically important difference of 3 points and favored the group receiving physical therapy at each follow-up assessment.46 The nature of this analysis and the lack of randomization to conservative treatment approaches preclude conclusions about the cause of these more favorable outcomes. There were differences in co-interventions that accompanied receiving physical therapy, notably consultation with a surgeon that may help to explain these associations. In addition, several important outcome measures including the Oswestry Index and bodily pain SF-36 subscale did not demonstrate any differences across time based on receiving physical therapy or not.
It is difficult to judge the value of physical therapy for lumbar spinal stenosis based on current literature. There have been several randomized, or large observational studies, including the SPORT study, comparing surgical to conservative management,6,17,29–31 but none have standardized the conservative management to include physical therapy for all patients. Recent randomized trials with small sample sizes and short-term follow-ups have found physical therapy regimens to be superior to no-treatment control groups,32,33 and epidural injections superior to physical therapy in the short-term but equally effective in the long-term33 for the conservative management of patients with lumbar spinal stenosis. More research is needed to evaluate the relative merits of different conservative management strategies for patients with lumbar spinal stenosis. The need to optimize the effectiveness of conservative management for lumbar spinal stenosis is clear from a consideration of the costs and potential for complications associated with surgery.34,35 Maximizing the effectiveness of the recommended period of conservative care could help limit exposure to surgery to those patients whose symptoms are unresponsive to a conservative approach.
The specific content of the physical therapy provided to patients in this analysis was not known. Numerous physical therapy interventions have been recommended for patients with lumbar spinal stenosis including treadmill or stationary cycling, various stretching, strengthening and repeated end-range movement exercise strategies, and manual therapy.12–14,36–38 Few randomized trials have directly compared different interventions, making it difficult to define the parameters of an evidence-based physical therapy program for patients with lumbar spinal stenosis. Available studies suggest a role for general conditioning using body weight-supported treadmill walking or stationary cycling, strengthening exercises for the trunk and lower extremities, and manual therapy for the spine and hips.13,32,38–40 Further research is needed to examine specific elements of physical therapy that may benefit patients with spinal stenosis and the optimal dosage. In this study 30% of patients receiving physical therapy only attended 1 or 2 sessions. We cannot determine what the content of physical therapy was for these patients. It may be that advice and education in self-care activities was the goal of these sessions, or the small number of sessions attended could indicate that patients were dissatisfied or did not perceive that additional sessions would be beneficial.
There has been little research examining factors related to whether or not patients with lumbar spinal stenosis receive physical therapy. Previous studies41,42 examining patients with low back pain of varied ages and diagnoses have not evaluated the two factors identified as predictive in this study; marital status and symptom radiation. This may reflect an attitude among providers that the presence of radicular symptoms indicates a need for alternative treatments such as spinal injections.43,44 Links between health care utilization and marital status have been identified;45 however, the lower utilization of physical therapy by married patients in the present study is difficult to explain from the data collected. It is not clear if patients who were married were seeking different forms of health care, or were more likely to choose to manage their symptoms without seeking additional care. Additional research is needed to clarify factors that impact care-seeking in patients with lumbar spinal stenosis.
The results of this study should be considered in light of several notable limitations. This study represents a secondary analysis of a subset of the subjects recruited into the SPORT study and was not proposed as an a priori aim of the larger study. As mentioned previously, the lack of randomization to treatment groups in this analysis does not permit conclusions regarding the efficacy of physical therapy. The observational nature of this study cannot eliminate the potential for selection bias in explaining differences between groups. The non-standardized approach to conservative management in the SPORT study further complicates an evaluation of relative benefits of specific treatment components. Additional research is needed to evaluate the relative effectiveness and cost-effectiveness of well-defined, standardized conservative approaches.
CONCLUSION
This secondary analysis of a nationally-representative cohort of patients from the SPORT study demonstrates that a wide variety of conservative interventions are utilized by patients with lumbar spinal stenosis who pursue non-surgical management. The most common conservative treatments used were spinal injections and physical therapy. Receiving physical therapy within the first six weeks after enrollment was related to a lack of radiating symptoms, and being single instead of married. Receiving physical therapy within the first six weeks was associated with better patient self-rating of improvement, greater improvement in physical functioning, and a reduced likelihood of surgery across a 1-year follow-up period. Other outcomes did not differ based on receiving physical therapy or not. The results of this analysis emphasize the need for further research to define the most effective conservative management strategies for patients with lumbar spinal stenosis.
Acknowledgments
The authors would like to acknowledge funding from the following sources:
The National Institute of Arthritis and Musculoskeletal and Skin Diseases (U01-AR45444) and the Office of Research on Women’s Health, the National Institutes of Health, and the National Institute of Occupational Safety and Health, the Centers for Disease Control and Prevention.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg. 1990;72:403–8. [PubMed] [Google Scholar]
- 2.Kalichman L, Cole R, Kim DH, Li L, Suri P, Guermazi A, et al. Spinal stenosis prevalence and association with symptoms: the Framingham Study. Spine J. 2009;9:545–50. doi: 10.1016/j.spinee.2009.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benoist M. The natural history of lumbar degenerative spinal stenosis. J Bone Spine. 2002;69:450–7. doi: 10.1016/s1297-319x(02)00429-3. [DOI] [PubMed] [Google Scholar]
- 4.Diagnosis and treatment of degenerative lumbar spinal stenosis. Burr Ridge, IL: North American Spine Society (NASS); 2007. [Google Scholar]
- 5.Evidence report/technology assessment number 32. Rockville, MD: Agency for Healthcare Quality and Research; Jun, 2001. Treatment of degenerative lumbar spinal stenosis: summary. [Google Scholar]
- 6.Atlas SJ, Delitto A. Spinal stenosis: surgery versus nonsurgical treatment. Clin Orthop Relat Res. 2006;443:198–207. doi: 10.1097/01.blo.0000198722.70138.96. [DOI] [PubMed] [Google Scholar]
- 7.Haig AJ, Tomkins CC. Diagnosis and management of lumbar spinal stenosis. JAMA. 2010;303:71–2. doi: 10.1001/jama.2009.1946. [DOI] [PubMed] [Google Scholar]
- 8.de Tran QH, Duong S, Finlayson RJ. Lumbar spinal stenosis: a brief review of the nonsurgical management. Can J Anaesth. 2010;57:694–703. doi: 10.1007/s12630-010-9315-3. [DOI] [PubMed] [Google Scholar]
- 9.Atlas SJ, Deyo RA, Patrick DL, Convery K, Keller RB, Singer DE. The Quebec Task Force classification for Spinal Disorders and the severity, treatment, and outcomes of sciatica and lumbar spinal stenosis. Spine. 1996;21:2885–92. doi: 10.1097/00007632-199612150-00020. [DOI] [PubMed] [Google Scholar]
- 10.Cummins J, Lurie JD, Tosteson TD, Hanscom B, Abdu WA, Birkmeyer NJ, et al. Descriptive epidemiology and prior healthcare utilization of patients in the Spine Patient Outcomes Research Trial’s (SPORT) three observational cohorts: disc herniation, spinal stenosis, and degenerative spondylolisthesis. Spine. 2006;31:806–14. doi: 10.1097/01.brs.0000207473.09030.0d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bodack MP, Monteiro M. Therapeutic exercise in the treatment of patients with lumbar spinal stenosis. Clin Orthop Relat Res. 2001;384:144–52. doi: 10.1097/00003086-200103000-00017. [DOI] [PubMed] [Google Scholar]
- 12.Comer CM, Redmond AC, Bird HA, Conaghan PG. Assessment and management of neurogenic claudication associated with lumbar spinal stenosis in a UK primary care musculoskeletal service: a survey of current practice among physiotherapists. BMC Musculoskel Dis. 2009;10:121. doi: 10.1186/1471-2474-10-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simotas AC, Dorey FJ, Hansraj KK, Cammisa F. Nonoperative treatment for lumbar spinal stenosis: clinical outcome results and 3-year survivorship analysis. Spine. 2000;25:197–203. doi: 10.1097/00007632-200001150-00009. [DOI] [PubMed] [Google Scholar]
- 14.Whitman JM, Flynn TW, Fritz JM. Nonsurgical management of patients with lumbar spinal stenosis: a literature review and a case series of three patients managed with physical therapy. Phys Med Clin N Am. 2003;14:77–103. doi: 10.1016/s1047-9651(02)00076-1. [DOI] [PubMed] [Google Scholar]
- 15.Birkmeyer NJ, Weinstein JN, Tosteson AN, Tosteson TD, Skinner JS, Lurie JD, et al. Design of the Spine Patient outcomes Research Trial (SPORT) Spine. 2002;27:1361–72. doi: 10.1097/00007632-200206150-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Eng J Med. 2008;358:794–810. doi: 10.1056/NEJMoa0707136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Blood E, Herkowitz H, et al. Surgical versus nonoperative treatment for lumbar spinal stenosis four-year results of the Spine Patient Outcomes Research Trial. Spine. 2010;35:1329–38. doi: 10.1097/BRS.0b013e3181e0f04d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ware JE, Sherbourne CD. The MOS 36-item short form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 19.Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–3. [PubMed] [Google Scholar]
- 20.Patrick DL, Deyo RA, Atlas SJ, Singer DE, Chapin A, Keller RB. Assessing health-related quality of life in patients with sciatica. Spine. 1995;20:1899–908. doi: 10.1097/00007632-199509000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Djurasovic M, Glassman SD, Carreon LY, Dimar JR. Contemporary management of symptomatic lumbar spinal stenosis. Orthop Clin N Am. 2010;41:183–91. doi: 10.1016/j.ocl.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 22.Keller RB, Atlas SJ, Singer DE, Chapin AM, Mooney NA, Patrick DL, et al. The Maine Lumbar Spine Study, Part I: Background and concepts. Spine. 1996;21:1769–76. doi: 10.1097/00007632-199608010-00010. [DOI] [PubMed] [Google Scholar]
- 23.Atlas SJ, Deyo RA, Keller RB, Chapin AM, Patrick DL, Long JM, et al. The Maine Lumbar Spine Study, Part III: 1-year outcomes of surgical and nonsurgical management of lumbar spinal stenosis. Spine. 1996;21:1787–94. doi: 10.1097/00007632-199608010-00012. [DOI] [PubMed] [Google Scholar]
- 24.Dahm KT, Brurberg KC, Jamtvedt G, Hagen KB. Advice to rest in bed versus advice to stay active for acute low-back pain and sciatica. Cochrane Database Syst Rev. 2010;16(6):CD007612. doi: 10.1002/14651858.CD007612.pub2. [DOI] [PubMed] [Google Scholar]
- 25.Manchikanti L, Pampati V, Singh V, Boswell MV, Smith HS, Hirsch JA. Explosive growth of facet joint interventions in the Medicare population in the United States: a comparative evaluation of 1997, 2002, and 2006 data. BMC Health Serv Res. 2010;10:84. doi: 10.1186/1472-6963-10-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Friedly J, Chan L, Deyo R. Increases in lumbosacral injections in the Medicare population: 1994 to 2001. Spine. 2007;32:1754–60. doi: 10.1097/BRS.0b013e3180b9f96e. [DOI] [PubMed] [Google Scholar]
- 27.Feuerstein M, Marcus SC, Huang GD. National trends in nonoperative care for nonspecific back pain. Spine J. 2004;4:56–63. doi: 10.1016/j.spinee.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 28.Gelhorn AC, Chan L, Martin BI, Friedly J. Management patterns in acute low back pain: the role of physical therapy. Spine. 2010 doi: 10.1097/BRS.0b013e3181d79a09. e-pub ahead of print, Nov. 19, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Amundsen T, Weber H, Nordal HJ, Magnaes B, Abdelnoor M, Lilleas F. Lumbar stenosis: conservative or surgical management? A prospective 10-year study. Spine. 2000;25:1424–35. doi: 10.1097/00007632-200006010-00016. [DOI] [PubMed] [Google Scholar]
- 30.Malmivaara A, Slätis P, Heliövaara M, et al. Surgical or non-operative treatment for lumbar spinal stenosis? A randomized controlled trial. Spine. 2007;32:1–8. doi: 10.1097/01.brs.0000251014.81875.6d. [DOI] [PubMed] [Google Scholar]
- 31.Mariconda M, Fava R, Gatto A. Unilateral laminectomy for bilateral decompression of lumbar spinal stenosis: a prospective comparative study with conservatively treated patients. J Spinal Dis. 2002;15:39–46. doi: 10.1097/00024720-200202000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Goren A, Yildiz N, Topuz O, Findikoglu G, Ardic F. Efficacy of exercise and ultrasound in patients with lumbar spinal stenosis: a prospective randomized controlled trial. Clin Rehabil. 2010;24:623–31. doi: 10.1177/0269215510367539. [DOI] [PubMed] [Google Scholar]
- 33.Koc Z, Ozcakir S, Siviroglu K, Gurbet A, Kucukoglu S. Effectiveness of physical therapy and epidural steroid injections in lumbar spinal stenosis. Spine. 2009;34:985–9. doi: 10.1097/BRS.0b013e31819c0a6b. [DOI] [PubMed] [Google Scholar]
- 34.Carragee EJ. The increasing morbidity of elective spinal stenosis surgery. Is it necessary? JAMA. 2010;303:1309–10. doi: 10.1001/jama.2010.402. [DOI] [PubMed] [Google Scholar]
- 35.Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303:1259–65. doi: 10.1001/jama.2010.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Creighton DS, Krauss J, Marcoux B. Management of lumbar spinal stenosis through the use of translatoric manipulation and lumbar flexion exercises: a case series. J Manual Manip Ther. 2006;14:E1–10. [Google Scholar]
- 37.Fritz JM, Erhard RE, Vignovic M. A nonsurgical approach for patients with lumbar spinal stenosis. Phys Ther. 1997;77:962–73. doi: 10.1093/ptj/77.9.962. [DOI] [PubMed] [Google Scholar]
- 38.Pua YH, Cai CC, Lim KC. Treadmill walking with body weight support is no more effective than cycling when added to an exercise program for lumbar spinal stenosis: a randomised controlled trial. Aust J Physiother. 2007;53:83–9. doi: 10.1016/s0004-9514(07)70040-5. [DOI] [PubMed] [Google Scholar]
- 39.Whitman JM, Flynn TW, Childs JD, Wainner RS, Gill HC, Garber MB, et al. A comparison between two physical therapy treatment programs for patients with lumbar spinal stenosis: a randomized clinical trial. Spine. 2006;31:2541–9. doi: 10.1097/01.brs.0000241136.98159.8c. [DOI] [PubMed] [Google Scholar]
- 40.Murphy DR, Hurwitz EL, Gregory AA, Clary R. A non-surgical approach to the management of lumbar spinal stenosis: a prospective observational cohort study. BMC Musculoskel Dis. 2006;7:16. doi: 10.1186/1471-2474-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Freburger JK, Carey TS, Holmes GM. Physician referrals to physical therapists for the treatment of spine disorders. Spine J. 2005;5:530–41. doi: 10.1016/j.spinee.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 42.Freburger JK, Holmes GM, Carey TS. Physician referrals to physical therapy for the treatment of musculoskeletal conditions. Arch Phys Med Rehabil. 2003;84:1839–49. doi: 10.1016/s0003-9993(03)00375-7. [DOI] [PubMed] [Google Scholar]
- 43.Botwin K, Brown LA, Fishman M, Rao S. Fluoroscopically guided caudal epidural steroid injections in degenerative lumbar spine stenosis. Pain Physician. 2007;10:547–58. [PubMed] [Google Scholar]
- 44.Bederman SS, Mahomed NN, Kreder HJ, McIssac WJ, Coyte PC, Wright JG. In the eye of the beholder: preferences of patients, family physicians, and surgeons for lumbar spinal surgery. Spine. 2010;35:108–15. doi: 10.1097/BRS.0b013e3181b77f2d. [DOI] [PubMed] [Google Scholar]
- 45.Joung IM, van der Meer JB, Mackenbach JP. Marital status and health care utilization. Int J Epidemiol. 1995;24:569–75. doi: 10.1093/ije/24.3.569. [DOI] [PubMed] [Google Scholar]
- 46.Lauridsen HH, Hartvigsen J, Manniche C, Korsholm L, Grunnet-Nilsson N. Responsiveness and minimal clinically important difference for pain and disability instruments in low back pain patients. BMC Musculoskel Dis. 2006;7:82. doi: 10.1186/1471-2474-7-82. [DOI] [PMC free article] [PubMed] [Google Scholar]