Abstract
Objective
Previous findings suggest a relationship between childhood abuse and pain-related conditions. It is yet to be determined whether adult PTSD symptoms may mediate the association between the experience of childhood abuse and reported pain in adulthood. Emotion dysregulation may also play a role in mediating PTSD and pain levels.
Methods
We examined subjects (N=814) recruited from the primary care clinics of an urban public hospital as part of an NIMH-funded study of trauma related risk and resilience. We evaluated childhood abuse with the Childhood Trauma Questionnaire (CTQ), PTSD symptoms with the PTSD Symptom Severity scale (PSS), and emotional dysregulation with the Emotion Dysregulation Scale (EDS). Pain and functional limitations of pain were assessed through self-report.
Results
We found that both childhood abuse and current PTSD symptoms predicted higher levels of reported pain. Childhood abuse, PTSD symptoms, and emotion dysregulation all predicted higher levels of functional impairment related to pain. Using the Sobel method and bootstrapping techniques and controlling for current level of negative affect, we found that PTSD fully mediated the effect of childhood abuse on pain level and pain-related limitations; emotion dysregulation partially mediated the effect of PTSD symptoms in predicting higher levels of pain-related limitations.
Conclusions
Although causality cannot be determined in the present study, these findings suggest that PTSD may serve as the pathway between exposure to childhood abuse and the development of pain-related conditions in adulthood, and that emotion dysregulation is a significant factor in understanding how PTSD relates to specific pain-related functional impairment.
Introduction
Pain is one of the most frequent reasons individuals seek medical care and represents a serious medical problem [1]. One area of particular interest in recent years has been in the relationship between pain and psychological disorders [2]. While the majority of this research has focused on the relation between depression and chronic pain, recent evidence suggests an important link between pain and anxiety disorders, particularly posttraumatic stress disorder (PTSD) [3,4].
PTSD is associated with increased reporting of pain conditions and lower reported quality of life among individuals experiencing pain [5,6]. The rates of chronic pain in PTSD populations are high. A recent study of male veterans [7] found that 66% of veterans presenting for VA PTSD treatment had an already established, physician-diagnosed chronic pain condition. This is consistent with prior research showing high rates of pain conditions present among both veteran and civilian populations with PTSD [4,8,9]. Further research indicates that individuals with co-occurring pain and PTSD show higher levels of disability and life interference as compared to individuals with only pain or PTSD alone [10,11].
The comorbidity between PTSD and pain syndromes suggests the possibility of shared vulnerability pathways [12] and the potential mutual maintenance of symptoms [13]. This was well documented in a recent review of the relevant literature [14]. Bosco and colleagues [15] also suggest that it is a chronic fear-avoidance cycle found in both PTSD and chronic pain that leads to this mutual maintenance of symptoms. In order to make progress in our understanding and treatment of comorbid PTSD and pain conditions, it is critical to examine psychological and behavioral processes that may play a role in the development or exacerbation of their shared relationship.
The capacity to effectively regulate negative affective states is likely an independent process underlying the relationship of co-occurring PTSD and pain. The inability to regulate or manage intense negative emotions, often referred to as emotional dysregulation, plays an important role in PTSD [16]. Researchers have already found strong associations between negative affect and pain. In a longitudinal study of young adults, Breslau, Chilcoat, and Andreski [17] found that negative emotionality predicted risk of developing migraine headaches among female participants. Experimental research supports this, showing that negative mood induction can decrease in-lab pain tolerance and increase reported levels of pain [18].
While emotion dysregulation is certainly related to negative emotionality, it is a distinct construct that impacts many psychiatric conditions on its own and should be considered an important transdiagnostic target for intervention in the treatment of psychopathology [16]. The specific deficits related to emotional awareness, understanding, and regulation strategies that encompass emotion dysregulation appear to provide us with relevant clinical information beyond the presence of high levels of negative emotional states alone. Recent research [16] examined the independent roles of negative affect and emotion dysregulation in relation to psychiatric conditions found that even after accounting for negative affect, emotion dysregulation was significantly related to higher levels of PTSD, depression, and substance abuse symptoms.
Childhood abuse is an additional risk factor for the development of both PTSD and pain in adulthood. The relationship between childhood abuse and risk for the development of PTSD is already well established [19,20]. Evidence of associations between childhood abuse and adult health problems, including chronic pain, is also growing [21,22]. A recent meta-analysis [23] found substantial evidence for childhood abuse as a risk factor for the development of pain conditions in adulthood. Past research has shown that both PTSD symptoms and emotional dysregulation may mediate the relationship between early childhood trauma exposure and risk for adult psychopathology [24–26], and it is possible that both PTSD and emotional dysregulation may also act as mediating variables in the association between childhood abuse and adult pain levels.
The goal of this study is to examine the potential relationship among these variables in a highly-traumatized, economically disadvantaged population. Specifically, the current study will explore how childhood abuse, PTSD symptoms, and emotion dysregulation are related to (1) reported pain levels and (2) functional limitations due to pain.
Method
Procedure
Participants were drawn from an NIMH-funded study of risk factors for the development of PTSD in a low socioeconomic, primarily African American urban population. Participants were recruited from waiting rooms in the gynecology and primary care medical (non-psychiatric) clinics at Grady Memorial Hospital, a publicly funded hospital in Atlanta, Georgia. We did not narrow our recruitment to specific selection criteria, but approached any individual in the waiting room. To be eligible for participation, subjects had to be at least 18 years old, not actively psychotic, and able to give informed consent. After signing the informed consent approved by the Emory Institutional Review Board, an initial interview was administered with questionnaires regarding trauma history, PTSD symptoms, and psychological variables. Trained research assistants administered this interview, which took 45–75 minutes to complete (duration largely dependent on participant’s trauma history and symptoms). Subjective reports of pain were obtained during a secondary phase of the study in which a subset of screened participants participated.
Participants
The sample consisted of 814 individuals, with 65% females. The subjects were all adult (>18 years; median age of 41) and primarily African American (92.5%). The remainder of the racial composition was as follows: White (4.3%), mixed/other (2.3%), and Hispanic or Latino (3.7%). The sample was predominately poor, with 78.9% of individuals unemployed and 71% coming from households with a monthly income of less than $1,000. The majority of participants were medical patients (>80%). All participants in the study reported at least one traumatic event and 75% of participants reported experiencing at least two traumas in their lifetime. Only a subset of participants reported childhood abuse or neglect. Based on CTQ data, 45.3% reported moderate or severe childhood abuse (21.4% physical abuse, 26.9% sexual abuse, 19.8% emotional abuse, 16.4% emotional neglect and 16.1% physical neglect).
Measures
Childhood Trauma Questionnaire (CTQ)
The CTQ [27] is a 25-item, brief, reliable and valid self-report instrument assessing sexual, physical, emotional abuse, and neglect in childhood. Researchers created a continuous variable to account for reported rates of moderate-to-severe emotional, physical, and sexual abuse, as well as emotional and physical neglect. Higher scores on the measure indicated higher levels of reported abuse.
Modified PTSD Symptom Scale (PSS)
The PSS [28,29] is a psychometrically valid 17-item self-report measure assessing frequency of PTSD symptoms over the prior two weeks. It distinguishes among re-experiencing, avoidance, and hyperarousal symptom clusters of PTSD. The PSS was used as a continuous outcome measure of PTSD symptom severity.
Emotion Dysregulation Scale (EDS)
The EDS [16] is a 24-item self-report scale adapted from the clinician-rated Affect Regulation and Experience Q-sort Questionnaire. Items are scored on a 7-point Likert scale and assess domains of emotional experiencing (e.g., “Emotions overwhelm me”) cognition (e.g., “When I’m upset, I feel all alone in the world”); and behavior (e.g., “When my emotions are strong, I often make bad decisions”). The internal consistency of the scale is high (3=0.97).
Short Form (36) Health Survey
The SF-36 Health Survey Questionnaire is a widely validated self-report measure of pain and other health domains [30]. For the present study, we utilized questions that assess self-reported current pain ratings: 1) to what degree the participant has experienced bodily pain in the past 4 weeks on a scale from 1 (none) to 6 (severe) (mean=3.31, SD=1.52) and 2) how much bodily pain interfered with functioning in the past four weeks on a scale from 1 (none) to 5 (extremely interfering) (mean=2.49, SD=1.40).
Positive and Negative Affect Schedule
The PANAS [31] is a well-validated self-report measure of general mood state. Participants were asked to rate on a 5-point Likert scale their general experiences with 20 emotional adjectives, 10 describing positive emotional states (e.g., excited, proud) and 10 describing negative emotional states (e.g., distressed, irritable). Analyses for this study focused on the negative affect portion of the scale.
Data Analysis
The overall analytic approach was to examine the predictive utility of childhood abuse, current PTSD symptoms, and emotion dysregulation on reported pain levels and functional limitations due to pain using SPSS software. We examined the distributions of all key predictor and outcome variables. The PTSD, childhood abuse, emotion dysregulation, negative affect, and pain-related functional limitations variables were positively skewed, and the self-reported bodily pain variable was negatively skewed. However, the level of skewness (range −.11 to 1.01), as well as the level of kurtosis (range −1.2 to .51), fell within acceptable parameters for the sample size [32]. Descriptive statistics were computed and bivariate correlations among variables were described. Predictor variables were scaled on a 0–10 scale for ease of interpretation and comparison of coefficients. Hierarchical linear regressions were utilized to examine the unique predictive value of childhood abuse and PTSD symptoms in estimating pain levels and functional limitations due to pain. Then, the predictive value of emotion dysregulation, over and above PTSD symptoms and childhood abuse, was evaluated. Mediation analyses were performed with INDIRECT [33] for SPSS, which allows for the examination of the mediating effects of a variable conditional on the effects of other variables in the model. Bootstrapping with 95% confidence intervals (CI) was utilized to determine significance of mediation effects. Bootstrapping is a preferred method for interpreting mediation analyses because it does not assume that sampling distributions of the indirect effects are normally distributed [33]. Age, sex, race, education level, and negative affect were included as covariates in all analyses.
Results
To determine the extent of association among our predictor variables and pain variables, we first calculated Pearson correlation coefficients. As shown in Table 1, all variables of interest were significantly correlated with each other (p<.01). Self-reported pain level and functional limitations due to pain were highly correlated at r 814=0.74 (p<.001). Correlations of the predictor variables with pain level and functional limitations ranged from r(814)=0.15 – 0.28 (p<.01) and r(814)=0.13 – 0.29 (p<.01), respectively.
Table 1.
Bivariate Correlations for Variables of Interest
| Pain | Limitations from pain | Negative affect | Child abuse | PTSD symptoms | Emotion dysregulation | |
|---|---|---|---|---|---|---|
| Pain | ||||||
| Limitations from pain | 0.74 | |||||
| Negative affect | 0.23 | 0.22 | ||||
| Child abuse | 0.15 | 0.13 | 0.32 | |||
| PTSD symptoms | 0.28 | 0.29 | 0.53 | 0.40 | ||
| Emotion dysregulation | 0.21 | 0.27 | 0.62 | 0.31 | 0.58 |
All correlations are significant at p<0.1
We then conducted a series of linear regressions to examine the unique and combined associations of childhood trauma, PTSD symptoms, and emotion dysregulation ratings with variation in pain level and functional limitations due to pain. While the selected predictor variables were significantly correlated, relationships were not large enough to create concerns about multi-collinearity or variance inflation within a regression model (VIF values ranged from 1.09–1.95) [34]. In each regression, age, sex, race, education level, and negative affect were entered in the first step of the model; this was done to control for demographic variations and overlap between negative affect and our predictor variables.
Regression Analyses for PTSD Symptoms and Emotion Dysregulation
As shown in Tables 2 and 3, childhood abuse was significantly predictive of both pain level and functional limitations due to pain (β=.08, p<.05; β=.08, p<.05, respectively). When PSS score was entered into the models, childhood abuse was no longer significant and only PTSD symptoms predicted pain level and functional limitations due to pain (β=.22, p<.001; β=.22, p<.001, respectively). For pain, emotion dysregulation was not a significant predictor over PTSD symptoms (β=.01, p=.97); PSS score remained significant (β=.22, p<.001). For functional limitations due to pain, emotion dysregulation was a significant predictor above and beyond PTSD symptoms (β=.11, p<.001; see Table 3). In the final step with emotion dysregulation, PTSD symptoms remained significantly predictive of functional limitations, although the coefficient decreased suggesting a partial mediation effect (β=.19, p<.001). In both models, age was predictive of higher reported pain and functional limitations (β=.31, t=9.03, p<.001; β=.27, t=7.93, p<.001, respectively).
Table 2.
Hierarchical Linear Regression Predicting Pain Level as a Result of Pain from Childhood Abuse and Adult PTSD Symptoms
| Stand.β | T | P | R | R2 change | F change | P change | |
|---|---|---|---|---|---|---|---|
| Predicting Reported Pain Level | |||||||
| Step 1: | 0.36 | .13 | 24.01 | <.001** | |||
| Age | 0.29 | 8.61 | <.001 | ||||
| Sex | 0.06 | 1.83 | .07 | ||||
| Race | −0.02 | −0.54 | .59 | ||||
| Education level | −0.04 | −1.03 | .30 | ||||
| Negative affect | 0.22 | 6.64 | <.001 | ||||
| Step 2: | 0.37 | 0.01 | 5.48 | .02* | |||
| Child Abuse | 0.08 | 2.34 | .02 | ||||
| Step 3: | 0.41 | 0.03 | 29.94 | <.001** | |||
| Child abuse | 0.03 | 0.71 | 0.28 | ||||
| PTSD symptoms | 0.22 | 5.47 | <.001 | ||||
| Step 4: | 0.41 | 0.00 | 0.01 | .97 | |||
| Child abuse | 0.03 | 0.70 | .48 | ||||
| PTSD symptoms | 0.24 | 5.95 | <.001 | ||||
| Emotion dysregulation | 0.01 | 0.04 | 0.97 |
p ≤ .01;
≤.05;
Age, sex, race, education, and negative affect were controlled.
Table 3.
Hierarchical Linear Regression Predicting Functional Limitations as a Result of Pain from Childhood Abuse and Adult PTSD Symptoms
| Stand.β | T | P | R | R2 change | F change | P change | |
|---|---|---|---|---|---|---|---|
| Predicting Pain-related Limits | |||||||
| Step 1: | 0.35 | 0.12 | 22.00 | <.001** | |||
| Age | 0.27 | 7.93 | <.001 | ||||
| Sex | 0.02 | 0.66 | .51 | ||||
| Race | −0.04 | −1.29 | .20 | ||||
| Education level | −0.04 | −1.25 | .21 | ||||
| Negative affect | 0.23 | 6.72 | <.001 | ||||
| Step 2: | 0.36 | 0.01 | 4.08 | .04* | |||
| Child Abuse | 0.07 | 2.02 | .04 | ||||
| Step 3: | 0.40 | 0.03 | 30.53 | <.001** | |||
| Child abuse | 0.01 | 0.35 | 0.73 | ||||
| PTSD symptoms | 0.22 | 5.53 | <.001 | ||||
| Step 4: | 0.41 | 0.01 | 6.06 | .01** | |||
| Child abuse | 0.01 | 0.19 | .85 | ||||
| PTSD symptoms | 0.19 | 4.32 | <.001 | ||||
| Emotion dysregulation | 0.11 | 2.46 | .01 |
p ≤ .01;
<.05;
Age, sex, race, education, and negative affect were controlled.
Mediation Analyses
Following the guidelines of Preacher and Hayes [33], we used Sobel and bootstrapping techniques to formally test for mediation effects among our variables. We again included age, sex, race, education level, and negative affect as control variables. We first formally tested for the mediation effects of PTSD on the association between childhood abuse and reported pain level. As expected based on regression findings, there was a significant full mediation effect of PTSD (F=24.26, p<.001, bias-corrected 95% confidence interval (CI) = 0.01 – 0.03). These results are depicted in Figure 1. Then, we formally tested for the mediation effects of PTSD and emotion dysregulation. We found a full mediation effect of PTSD on the association between childhood abuse and functional limitations due to pain (F=19.56, p<.001, 95% CI − 0.01 – 0.03). However, because the regression analyses suggested a partial mediation effect of emotion dysregulation on the relation of PTSD with functional limitations, we ran an additional indirect model to determine if this mediation was significant. As shown in Figure 2, emotion dysregulation score did partially mediate the relation between PTSD symptoms and functional limitations of pain (F=22.98, p<.001, 95% CI = 0.01 – 0.04).
Figure 1.
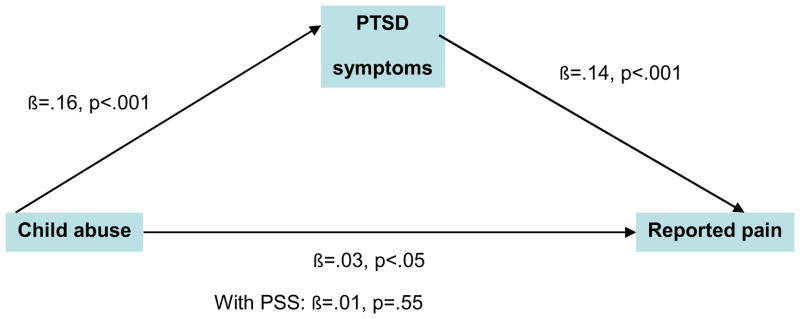
The full mediating effect of adult PTSD symptoms on the relation between childhood abuse and reported pain level. Age, sex, race, education level, and negative affect at time of assessment were controlled.
Figure 2.
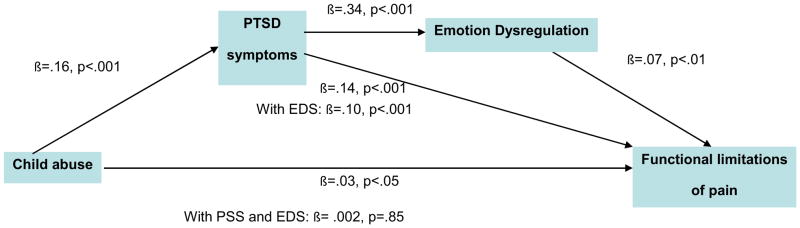
The mediating effects of adult PTSD symptoms and emotion dysregulation on the relation between childhood abuse and functional limitations of pain. Age, sex, race, education level and negative affect at time of assessment were controlled.
Discussion
The findings from this study suggest that current PTSD symptoms contribute to the connections between exposure to childhood abuse and both current reported pain and current pain-related limitations within this sample of highly traumatized, economically disadvantaged adults. We examined the independent effects of childhood abuse and current PTSD symptoms on these pain variables, finding that current PTSD symptoms fully mediated the relationship between higher levels of reported childhood abuse and higher levels of pain as well as pain-related limitations. This finding suggests that adult symptoms of PTSD may serve as a pathway through which the relationship between childhood abuse and adult pain manifests.
The present data extend earlier findings in both veteran and civilian populations [8,9] by examining the role of emotion in the association between PTSD symptoms and pain. Our data points to the importance of emotion dysregulation in predicting higher levels of pain-related impairment even after accounting for the contribution of childhood abuse, PTSD, and negative affect. Although our data do not show that emotion dysregulation has an impact on reported levels of pain, greater difficulty with emotion regulation appears to contribute to the relationship between pain and impaired ability to manage daily tasks within this sample. It makes sense that difficulty regulating emotions in the presence of high levels of pain could impact pain-related functioning. Other research has shown that individuals who are able to adaptively regulate and manage emotions tend to be healthier [35]. There is also evidence that cognitive-behavioral interventions among individuals with arthritis help improve pain management [36]. However, to our knowledge, no prior studies have shown this distinction in which emotional dysregulation predicts not pain levels per se but rather the impact of pain on adaptive functioning. This distinction may be similar to the distinction between negative affect and emotional dysregulation previously discussed [e.g., 16], in that the difficulty of managing and regulating high levels of negative affect that reflects emotion dysregulation may end up having more negative, long term consequences than simply the presence of negative affect alone.
This result is particularly important when considering the long-term effects of pain-related conditions on individuals’ lives. These effects emerge not only through the physical and emotional toll of the condition, but also by affecting whether someone can hold down a job, manage household duties, and continue to engage in leisure activities. Research has already shown that the presence of PTSD symptoms is associated with greater life interference among individuals with pain conditions [10,11], and our findings suggest that emotion regulation difficulties may be in part driving this effect. Because there is currently no cure for chronic pain, it becomes particularly critical in the treatment of pain conditions to help patients maintain as much normalcy in life and promote active engagement in as many areas as possible. Identification of specific factors that may impede individuals from functioning in the presence of pain then allows for interventions that can target such factors, thus having a larger impact on improving individuals’ quality of life. Several psychological interventions, such as Dialectical Behavior Therapy [37] and mindfulness-based therapies [38] have already shown effectiveness in increasing the capacity to regulate emotions with a focus on enhancing patient’s emotion regulation strategies through enhanced awareness of affective states. These treatments may also be effective in decreasing the potential negative impact of pain on daily adaptive functioning, and it would be beneficial in future studies to evaluate whether enhancing emotion regulation strategies also has a positive impact on functioning among individuals with physical pain. Of note, prior research has pointed to attachment security as a factor contributing to both the ability to regulate emotional responsiveness and to the ability to cope with pain [39,40]. Future research should further address this topic as researchers continue to explore how these variables interact to affect functioning. Additionally, future research in this area should use measures of emotion dysregulation which capture a broad range of emotion regulation strategies (e.g., the Difficulties in Emotion Regulation Scale) in order to help us understand whether there are specific aspects of emotion regulation that may be particularly important to target.
Several study limitations are worth noting. First, given the cross-sectional nature of this study and the use of retrospective reports, we cannot make assertions about causality or time of onset for PTSD symptoms, pain, or pain-related functional impairment. Prospective, longitudinal studies are required to examine the temporal onset of PTSD symptomatology and pain symptoms. It is possible that pain symptoms preceded the onset of PTSD symptoms and emotion dysregulation, and therefore should serve as a predictor rather than outcome variable. However, previous longitudinal research showing the presence of psychological difficulties before the onset of chronic pain conditions, led us to formulate our model. Additionally, pain ratings utilized in the study were based on only two variables and were current (prior 4 weeks), which does not allow us to accurately differentiate between acute and chronic pain and limits the conclusions that can be drawn from present findings. Further research in this area should be done to determine these relationships when chronic pain conditions are examined, as this will be a critical next step in understanding the role of emotion dysregulation in pain-related impairment. Relatedly, it would be extremely useful to measure medical conditions in addition to pain to help tease apart how PTSD and emotion dysregulation relate to pain and pain-related limitations independent of medical conditions. Unfortunately, we did not have data on current or past medical conditions within our sample and therefore cannot make any assertions regarding how medical illness load may have influenced the associations described in this study. Also, the small effect sizes we observed limit the extent of conclusions that can be drawn from this study. Another limitation is that our sample was largely low income and African American, and although we suspect that these effects are general, we do not yet have the data to demonstrate if these same findings would be present in other populations. However, this weakness is counterbalanced by the public health importance of studying these variables in an often under-researched and under-served population with such high rates of trauma exposure as well as mental and physical health problems. Finally, since the comorbidity between pain syndromes and depression has been widely analyzed in the literature, and its comorbidity with PTSD has been largely ignored, we chose to focus on this component of trauma-related sequellae. However, work examining interactions between PTSD, substance abuse, depression, and other potential trauma-related psychopathology is underway and should further aid in our understanding of the complex relationship between trauma, psychiatric symptomology, and pain syndromes.
Conclusion
The association between childhood abuse, PTSD symptoms, and reported physical pain provides further evidence that trauma and trauma-related conditions may affect pain syndromes and the need for increased awareness of such associations in civilian medical populations. Not only are PTSD symptoms associated with higher pain levels, but also with lower levels of functioning as a result of pain, therefore further influencing overall functioning and quality of life among these individuals. Notably, emotion dysregulation appears to play a role in the relationship between PTSD symptoms and functional limitations due to pain. Our data suggest that a focus on emotion regulation strategies in the treatment of PTSD symptoms within medical populations may likely improve management of pain syndromes through addressing issues related to pain-related functional limitations.
Footnotes
Disclosure
This work was primarily supported by the National Institute of Mental Health (MH071537). Support also included Emory and Grady Memorial Hospital General Clinical Research Center, NIH National Centers for Research Resources (M01 RR00039), and the Burroughs Welcome Fund.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gureje O, Von Korff M, Simon G, Gater R. Persistent pain and well-being. A World Health Organization study in primary care. JAMA. 1998;280:147–151. doi: 10.1001/jama.280.2.147. [DOI] [PubMed] [Google Scholar]
- 2.Turk D, Okifuji A. Psychological factors in chronic pain: Evolution and revolution. Journal of Consulting and Clinical Psychology. 2002;70:678–690. doi: 10.1037//0022-006x.70.3.678. [DOI] [PubMed] [Google Scholar]
- 3.Phifer J, Skelton K, Weiss T, Schwartz A, Wingo A, et al. Pain symptomatology and pain medication use in civilian PTSD. Pain. 2010;152:2233–2240. doi: 10.1016/j.pain.2011.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schwartz AC, Bradley R, Penza KM, Sexton M, Jay D, Haggard PJ, Garlow SJ, Ressler KJ. Pain medication use among patients with posttraumatic stress disorder. Psychosomatics. 2006;47(2):136–42. doi: 10.1176/appi.psy.47.2.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kimerling R, Clum G, Wolfe J. Relationships among trauma exposure, chronic posttraumatic stress disorder symptoms, and self-reported health in women: Replication and extension. Journal of Traumatic Stress. 2000;13:115–128. doi: 10.1023/A:1007729116133. [DOI] [PubMed] [Google Scholar]
- 6.Wagner A, Wolfe J, Rotnitsky A, Proctor S, Erickson D. An investigation of the impact of posttraumatic stress disorder on physical health. Journal of Traumatic Stress. 2000;13:41–55. doi: 10.1023/A:1007716813407. [DOI] [PubMed] [Google Scholar]
- 7.Shipherd J, Keyes M, Jovanovic T, Ready D, Baltzell D, et al. Veterans seeking treatment for posttraumatic stress disorder: What about comorbid chronic pain? Journal of Rehabilitation Research & Development. 2007;44:153–166. doi: 10.1682/jrrd.2006.06.0065. [DOI] [PubMed] [Google Scholar]
- 8.Beckham J, Crawford A, Feldman M, Kirby A, Hertzberg M, et al. Chronic posttraumatic stress disorder and chronic pain in Vietnam combat veterans. Journal of Psychosomatic Research. 1997;43:279–289. doi: 10.1016/s0022-3999(97)00129-3. [DOI] [PubMed] [Google Scholar]
- 9.Schwartz A, Bradley B, Sexton M, Sherry A, Ressler K. Posttraumatic stress disorder among African Americans in an inner city mental health clinic. Psychiatric Services. 2005;56:212–216. doi: 10.1176/appi.ps.56.2.212. [DOI] [PubMed] [Google Scholar]
- 10.Sherman J, Turk D, Okifuji A. Prevalence and impact of posttraumatic stress disorder-like symptoms on patients with fibromyalgia syndrome. Clinical Journal of Pain. 2000;16:127–134. doi: 10.1097/00002508-200006000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Turk D, Okifuji A. Perception of traumatic onset, compensation status, and physical fundings: Impact on pain severity, emotional distress, and disability in chronic pain patients. Journal of Behavioral Medicine. 1996;19:435–453. doi: 10.1007/BF01857677. [DOI] [PubMed] [Google Scholar]
- 12.Asmundson G, Coons M, Taylor S, Katz J. PTSD and the experience of pain: Research and clinical implications of shared vulnerability and mutual maintenance models. Canadian Journal of Psychiatry. 2002;47:930–937. doi: 10.1177/070674370204701004. [DOI] [PubMed] [Google Scholar]
- 13.Sharp T, Harvey A. Chronic pain and posttraumatic stress disorder: Mutual maintenance? Clinical Psychology Review. 2001;21:857–877. doi: 10.1016/s0272-7358(00)00071-4. [DOI] [PubMed] [Google Scholar]
- 14.Otis J, Keane T, Kerns R. An examination of the relationship between chronic pain and posttraumatic stress disorder. Journal of Rehabilitation Research & Development. 2003;40:397–406. doi: 10.1682/jrrd.2003.09.0397. [DOI] [PubMed] [Google Scholar]
- 15.Bosco M, Gallinati J, Clark M. Conceptualizing and treating comorbid chronic pain and PTSD. Pain Research and Treatment. 2013:1–10. doi: 10.1155/2013/174728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bradley B, DeFife J, Guarnaccia C, Phifer J, Fani N, et al. Emotion dysregulation and negative affect: Association with psychiatric symptoms. The Journal of Clinical Psychiatry. 2011;72:685–691. doi: 10.4088/JCP.10m06409blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Breslau N, Chilcoat H, Andreski P. Further evidence on the link between migraine and neuroticism. Neurology. 1996;47:663–667. doi: 10.1212/wnl.47.3.663. [DOI] [PubMed] [Google Scholar]
- 18.Zelman D, Howland E, Nichols S, Cleeland C. The effect of induced mood on laboratory pain. Pain. 1991;46(1):105–111. doi: 10.1016/0304-3959(91)90040-5. [DOI] [PubMed] [Google Scholar]
- 19.Kendler K, Bulik C, Silberg J, Hettema J, Myers J, et al. Childhood sexual abuse and adult psychiatric and substance use disorders in women. Archives of General Psychiatry. 2000;57:953–959. doi: 10.1001/archpsyc.57.10.953. [DOI] [PubMed] [Google Scholar]
- 20.MacMillan H, Fleming J, Streiner D, Lin E, Boyle M, et al. Childhood abuse and lifetime psychopathology in a community sample. American Journal of Psychiatry. 2001;158:1878–1883. doi: 10.1176/appi.ajp.158.11.1878. [DOI] [PubMed] [Google Scholar]
- 21.Finestone H, Stenn P, Davies F, Stalker C, Fry R, Koumanis J. Chronic pain and health care utilization in women with a history of childhood sexual abuse. Child Abuse & Neglect. 2000;24:547–556. doi: 10.1016/s0145-2134(00)00112-5. [DOI] [PubMed] [Google Scholar]
- 22.Walker E, Gelfand A, Katon W, Koss M, Von Korff M, et al. Adult health status of women with histories of childhood abuse and neglect. The American Journal of Medicine. 1999;107:332–339. doi: 10.1016/s0002-9343(99)00235-1. [DOI] [PubMed] [Google Scholar]
- 23.Davies D, Luecken L, Zautra A. Are reports of childhood abuse related to the experience of chronic pain in adulthood?: A meta-analytic review of the literature. Clinical Journal of Pain. 2005;21(5):398–405. doi: 10.1097/01.ajp.0000149795.08746.31. [DOI] [PubMed] [Google Scholar]
- 24.Weierich M, Nock M. Posttraumatic stress symptoms mediate the relation between childhood sexual abuse and nonsuicidal self-injury. Journal of Consulting and Clinical Psychology. 2008;76(1):39–44. doi: 10.1037/0022-006X.76.1.39. [DOI] [PubMed] [Google Scholar]
- 25.Powers A, Thomas K, Ressler K, Bradley B. The differential effects of child abuse and posttraumatic stress disorder on schizotypal personality disorder. Comprehensive Psychiatry. 2011;52(4):438–445. doi: 10.1016/j.comppsych.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cloitre M, Miranda R, Stovall-McClough K, Han H. Beyond PTSD: Emotion regulation and interpersonal problems as predictors of functional impairment in survivors of childhood abuse. Behavior Therapy. 2005;36(2):119–124. [Google Scholar]
- 27.Bernstein D, Stein J, Newcomb M, Walker E, Pogge D, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 28.Coffey S, Dansky B, Falsetti S, Saladin M, Brady K. Screening for PTSD in a substance abuse sample: psychometric properties of a modified version of the PTSD Symptom Scale Self-Report. J Trauma Stress. 1998;11:393–9. doi: 10.1023/A:1024467507565. [DOI] [PubMed] [Google Scholar]
- 29.Foa E, Tolin D. Comparison of the PTSD Symptom Scale-Interview Version and the Clinician-Administered PTSD scale. J Trauma Stress. 2000;13:181–91. doi: 10.1023/A:1007781909213. [DOI] [PubMed] [Google Scholar]
- 30.Ware J, Kosinski M, Gandek B, Aaronson N, Apolone G, et al. The factor structure of the SF-36 Health Survey in 10 countries: results from the IQOLA Project. J Clin Epidemiol. 1998;51:1159–65. doi: 10.1016/s0895-4356(98)00107-3. [DOI] [PubMed] [Google Scholar]
- 31.Watson D, Clark L, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 32.Tabachnick BG, Fidell LS. Using multivariate statistics. 4. Boston: Allyn & Bacon; 2000. [Google Scholar]
- 33.Preacher K, Hayes A. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 34.O’Brien R. A caution regarding rules of thumb for variance inflation factors. Qual Quant. 2007;41(5):673–690. [Google Scholar]
- 35.Salovey P, Rothman A, Detweiler J, Steward W. Emotional states and physical health. American Psychologist. 2000;55:110–121. doi: 10.1037//0003-066x.55.1.110. [DOI] [PubMed] [Google Scholar]
- 36.Nicassio P, Greenberg M. The effectiveness of cognitive-behavioral and psychoeducational interventions in the management of arthritis. In: Weisman M, Weilblatt M, Louie J, editors. Treatment of rheumatic diseases. 2. William Saunders; Orlando: 2001. pp. 147–161. [Google Scholar]
- 37.Linehan M. Cognitive behavioral treatment of borderline personality disorder. Guilford Press; New York, NY: 1993. [Google Scholar]
- 38.Segal Z, Williams M, Teasdale J. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. Guilford Press; New York, NY: 2002. [Google Scholar]
- 39.Gross J. Handbook of emotion regulation. Guilford Press; New York, NY: 2009. [Google Scholar]
- 40.Kratz AL, Davis MC, Zautra AJ. Attachment predicts daily catastrophizing and social coping in women with pain. Health Psychology. 2012;31(3):778. doi: 10.1037/a0025230. [DOI] [PubMed] [Google Scholar]


