Abstract
Dispositional cancer worry (DCW) is the uncontrollable tendency to dwell on cancer independent of relevant stimuli (e.g., diagnosis of the disease). Past research has suggested that DCW has two underlying dimensions (severity and frequency). Available measures of DCW severity and frequency were translated and validated in two countries: China and Belgium. Participants (N=623) completed translated scales, as well as measures of general dispositional worry, cancer fear, and perceived risk. In both locations, DCW measures were reliable (Cronbach’s alphas ranged from .78 – .93) and demonstrated strong convergent, divergent, and concurrent validity. Severity and frequency factors loaded as expected in exploratory factor analysis. Future research should pursue longitudinal tests of DCW’s predictive validity and explore DCW in theoretical models predicting the relationship between worry and cancer prevention and early detection behaviors.
The National Cancer Institute (NCI) (2013) reports that approximately 7.6 million people worldwide died from cancer in 2008, and the number of worldwide deaths is estimated to grow to 13.2 million by the year 2030. To combat the global burden of cancer, the NCI has an international research agenda, and its Center for Global Health has strong, established roots in both China and Belgium. A variety of collaborative efforts and education opportunities (e.g., conferences, research scientist exchange programs) were created to aid cancer prevention, early detection, and treatment efforts. See Table 1 for summary of cancer incidence and mortality estimates in China and Belgium.
Table 1.
Cancer incidence and mortality rates before age 75
| Incidence | Mortality | |||
|---|---|---|---|---|
|
| ||||
| Males | Females | Males | Females | |
| China | 22.1% | 15.7% | 16.7% | 9.7% |
| Belgium | 34.3% | 26.3% | 15.2% | 9% |
Note. Cancer incidence and mortality by gender for each country in the study (from Ferley et al., 2010).
The NCI (2013) states that 35 percent of worldwide cancer deaths can be averted through prevention or early detection and subsequent treatment efforts. For example, lung cancer caused by smoking is preventable by eliminating the use of cigarettes. Skin cancer is preventable by using sun protection methods (e.g., sunscreen, wearing clothes that cover exposed skin) and is highly treatable when detected in early stages. Nonetheless, while some cancers are highly preventable and treatable, the global burden of cancer remains high due to limited access to screening and/or treatment (NCI, 2013).
Unfortunately, cancer prevention and detection activities are undermined by translation issues; notably, the inability to effectively communicate cancer-related recommendations to target audiences (Sussman et al., 2006). Effective communication could educate and motivate individuals to pursue cancer prevention and early detection, and thus play a pivotal role in global cancer control (Viswanath, 2005). Past research has revealed a challenging communication environment dominated by a litany of negative emotions; people are worried about cancer but also feel fatalistic, confused, and overloaded (Arora et al., 2008; Jensen, Bernat, Davis, & Yale, 2010; Shen & Condit, 2011 & Wright, 2009). Explicating these complex feelings, and identifying their relationship with other variables, is a necessary step in developing effective communication to address translation problems (Shen & Condit, 2011; Sussman et al., 2006).
There is a growing literature examining worry and its impact on cancer prevention and early detection behaviors. This research has often produced discrepant findings that sometimes raise more questions than they answer. For example, whether or not these negative emotions motivate or hinder cancer prevention activities remains unclear (Consedine, Magai, & Neugut, 2004). Some have found that fear or worry leads to lower levels of screening (Bloom, Hayes, Saunders & Flatt, 1987; Vernon, Laville & Jackson, 1990) while others found that worry increased screening intentions and behaviors (Bowen et al., 2003; Consedine et al., 2004; Edwards & Jones, 2000). These discrepant findings are due to the fact that there are some paradoxical themes in the worry concept. Worry is a chain of uncontrollable negative thoughts and/or images (Borkovec, Robinson, Pruzinsky, and Dupree, 1983). It exists as both a state and a disposition/trait and can produce either motivational or avoidant coping mechanisms to deal with the threat (Borkovec et al., 1983). At the same time that the emotional experience is negative and brought about by a fear stimulus, it can result in constructive problem-solving strategies. The interesting differentiation between worry and fear/anxiety is the potential positive impact on individuals because it seems to motivate coping not only with the emotion, but also, with the problem at hand. Past research has demonstrated that state-based cancer worry has the potential to be motivational and urge the worrier to engage in protective behaviors (Lehto & Cimprich, 2009), and dispositional cancer worry (DCW) has the potential to lead to poor decision-making, such as avoiding yearly mammograms (Borkovec, Robinson, Pruzinsky, & Dupree, 1983; Pruzinsky & Borkovec, 1990; Tallis, Eysenck, & Mathews, 1992), but lack of clarity exists when examining the specific mechanisms that make worry positive (motivational) versus negative (avoidant).
Consedine & Moskowitz (2007) stated that there is a need for more psychometric research that strives to define and validate constructs; thus, considerable attention has been devoted to explicating cancer worry. Of the two (i.e., state and disposition/trait), far less attention has been paid to dispositional/trait based cancer worry, possibly because researchers lack a valid measure (Jensen et al., 2011). General dispositional worry scales exist, and they have performed well in research studies (high internal consistency measures); however, they are typically used as diagnostic tools for Generalized Anxiety Disorder (GAD) or Post-traumatic Stress Disorder (PTSD). These scales measure everyday worries (e.g., finances), which are not specific to the cancer context. To address this gap, Jensen, Bernat, Davis, and Yale (2010) recently compared existing measures of DCW using exploratory factor analysis. Consistent with past research (Davey, Hampton, Farrell, & Davidson, 1992), they discovered that DCW had two meaningful dimensions (severity and frequency). DCW severity captures the intensity of the worrying experience whereas DCW frequency is a measure of how often worrying occurs. Based on the data, Jensen et al. (2010) advocated the use of the BWS (Dijkstra & Brosschot, 2003) to evaluate DCW severity and the RIES (Wiess & Marmar, 1997) to evaluate DCW frequency. Two other factors were identified in the analysis; however, one represented a different construct (cancer fear) and the other focused more on the impact of worrying rather than the feeling itself (Jensen et al., 2010).
Cross-cultural validation of scales advances knowledge and understanding of a particular construct. For example, research on self-efficacy has been significantly advanced by cross-cultural validation of the General Self-efficacy Scale (GSS) (Schwarzer & Jerusalem, 1995). Moreover, validating a scale across several cultures has the potential to establish global research agendas (Scholz, Gutiérrez-Doña, Sud, & Schwarzer, 2002). The current study extends the work of Jensen et al. (2010) by translating and examining the psychometric properties of both DCW scales (severity and frequency) in two countries with NCI established Centers for Global Health (China and Belgium). The goal of this research is to facilitate cross-cultural studies and to continue to explicate DCW.
Method
Subject recruitment
Participants from China and Belgium were recruited for this study. The lead author travelled to each country to collect data. In China, participants were solicited in public areas and by using an online university bulletin board system. In Belgium, participants were solicited in communication courses at a large university. In addition to previously mentioned recruitment strategies, both locations utilized a word-of-mouth solicitation technique, where participants were encouraged to pass the survey on to their friends and family members.
After participants agreed to participate, they were provided the URL for the survey, and no compensation was given for completion. Participants, at their own discretion, visited the survey website, read a consent form, and completed both demographic and experimental measures.
Study measures
All participants filled out demographic measures, general dispositional worry, DCW, cancer fear, and perceived cancer risk measures. Measures were translated into each location’s respective national language (Mandarin and Dutch) by a native speaker (China) or a group of native speakers (Belgium). See Appendix A for translated versions of the scales. Demographic measures included sex, age, and ethnicity.
General dispositional worry
General dispositional worry was measured using the Penn State Worry Questionnaire (PSWQ). The PSWQ is a 16-item, 5-point scale ranging from not at all typical of me to very typical of me that measures the intensity and manageability of everyday worry (Meyer, Miller, Metzger, & Borkovec, 1990). Sample items include, “If I do not have enough time to do something, I do not worry about it” and “My worries overwhelm me.”
DCW
DCW was measured using the BWS and the RIES. The BWS is a 4-item, 7-point scale ranging from not at all to very much. According to Jensen et al. (2011), the BWS measures dispositional cancer worry severity (DCW severity). Sample severity items include, “I am afraid of the physical consequences of getting cancer” and “I worry about my health because of my chances of getting cancer.” The RIES is a 7-item, 4-point scale ranging from not at all to often. Per Jensen et al. (2011), the RIES measures dispositional worry frequency (DCW frequency). Sample frequency items include, “I thought about it when I didn’t mean to” and “I had trouble falling asleep or staying asleep, because of picture or thoughts about it that came into my mind.”
Cancer fear
Cancer fear was measured by the Champion Breast Cancer Fear (Champion Fear) scale. The Champion Fear is an 8-item, 5-point scale ranging from strongly agree to strongly disagree originally measures self-reported physiological responses to the threat of developing breast cancer (Champion & Skinner, 2004); however, items were modified to refer to cancer, in general. Previous research has modified the scale to be used in studies targeting general cancer fear (Miles, Voorwinden, Chapman, & Wardle, 2008) and colorectal cancer fear (McQueen, Vernon, & Swank, 2013). Sample items include “The thought of cancer scares me” and “When I think about cancer, I get upset.”
Perceived cancer risk
Perceived cancer risk was measured by a modified version of the Disease Specific Perceived Risk (DSPR) Scale (DiLorenzo et al., 2006). The DSPR measures participants’ perception of their lifetime risk of developing breast, lung, colon, and skin cancer. Participants were asked, “How likely do you think you will develop one of these cancers in your lifetime.” Then, participants estimated their risk for each cancer on a sliding scale ranging from one to 100%.
Study sample
In China, 217 adults participated in this study. The mean age was 26.0 (SD = 7.4), and 55.8% were women Most participants (98.6%) identified themselves as Chinese; only 1.4% self-identified as some other ethnicity.
In Belgium, there were 406 participants. Their mean age was 20.1 (SD = 3.0), and 67.4% were women. Most (96.6%) of the sample identified themselves as Belgian; only 3.4% self-identified as some other ethnicity.
Analysis
The strategy for documenting reliability and validity taken here was parallel to previous work by Jensen et al. (2010). First, to document reliability, Cronbach’s alphas were calculated for the DCW severity and frequency. Second, construct (convergent and divergent) and predictive validity of the DCW severity and frequency measures were assessed. Construct validity was calculated by examining correlations of the DCW severity and frequency measures with established general dispositional worry (PSWQ) and cancer fear (Champion Fear) measures. Consistent with Jensen et al. (2011), we postulated that the items measuring DCW would be highly correlated with the Champion Fear items (convergent validity) and not be highly correlated with the PSWQ items (divergent validity). Regarding predictive validity, we postulated that the DCW severity and frequency measures would predict an individual’s perceived risk of developing breast cancer, lung cancer, colon cancer, or melanoma; this was examined with hierarchical regression analyses. Power analysis was calculated for the hierarchical regression analysis using GPower (Faul, Erdfelder, Lang, & Buchner, 2007). Specifically, we examined power to detect an R2 increase for a linear model with 4 predictors. To consistently detect an effect akin to f2 = .08 (the smallest effect observed in Jensen et al., 2011), a priori power analysis suggested a sample size of 197. Accordingly, the research team targeted a minimum sample size of 200 as the goal for each country.
Results
Exploratory Factor Analysis
Principle axis analysis with direct oblimin rotation was utilized to examine the underlying factor structure for both scales. Separate analyses were conducted for each country. Parallel analysis was employed to establish cut-off points for Eigen values (rather than use the conventional greater than 1 rule of thumb, which is suboptimal). In other words, factors are only explored if their Eigen value exceeds that which is expected by chance.
For China, two factors exceeded their Eigen value cut-offs (see Table 2 for loadings, Eigen values, and percent variance explained). Factor 1 consisted of the four BWS measures and represented DCW severity. The Eigen value for factor 1 was 5.26, which exceeds the 95% cutoff score of 1.49. Factor 2 consisted of the seven RIES measures and represented DCW frequency. The Eigen value for factor 2 was 2.22, which exceeds the 95% cut-off score of 1.36.
Table 2.
Principle Axis Analysis of DCW for China and Belgium
| Item | China | Belgium | ||
|---|---|---|---|---|
|
| ||||
| Factor 1 (Severity) | Factor 2 (Frequency) | Factor 1 (Severity) | Factor 2 (Frequency) | |
| 1. I am afraid of the physical consequences of getting cancer. | .82 | .85 | ||
| 2. I worry about my health because of my chances of getting cancer. | .93 | .66 | ||
| 3. I feel anxiety when I think of the possible consequences of getting cancer. | .82 | .89 | ||
| 4. I brood about the physical consequences of getting cancer. | .70 | .89 | ||
| 5. I thought about it when I didn’t mean to. | .51 | .55 | ||
| 6. I had trouble falling asleep or staying asleep, because of pictures or thoughts about it that came to mind. | .74 | .77 | ||
| 7. I had waves of strong feelings about it. | .86 | .52 | ||
| 8. I had dreams about it. | .82 | .66 | ||
| 9. Pictures about it popped into my mind. | .74 | .71 | ||
| 10. Other things kept making me think about it. | .76 | .47 | ||
| 11. Any reminder brought back feeling about it. | .60 | .60 | ||
| Eigenvalue | 5.26 | 2.22 | 4.34 | 2.12 |
| % of Variance | 47.81 | 20.22 | 39.45 | 19.25 |
Note. Principle axis analysis with direct oblimin rotation. Factor loadings below .30 are omitted to ease interpretation.
For Belgium, two factors exceeded their Eigen value cut-offs. Once again, factor 1 represented DCW severity and the observed Eigen value (4.34) surpassed the 95% cut-off of score of 1.34. Similarly, factor 2 represented DCW frequency and the observed Eigen value (2.12) was greater than that expected by chance (1.24). Thus, both DCW measures loaded as expected and consistent with the findings of Jensen et al. (2010).
Reliability and Construct Validity
In both China and Belgium, the DCW severity and frequency scales were reliable (see Table 3). To investigate construct (convergent and divergent) validity, correlations between the DCW severity, DCW Frequency, Champion Fear, and PSWQ scale items were examined (see Table 4). In China, both dimensions of DCW were not significantly correlated with PSWQ. In Belgium, DCW severity and frequency were moderately correlated with PSWQ. In both locations, there were strong positive correlations between DCW severity, DCW frequency, and the Champion Fear scale though the relationship between DCW frequency and the Champion Fear scale was lower in China. Since all DCW scales and fear scale highly correlated with one another, the BWS and RIES demonstrate strong convergent validity. Moreover, the DCW severity and frequency scales also demonstrated strong divergent validity because the items were moderately/not correlated with PSWQ items.
Table 3.
Descriptive statistics
| Mean | SD | Alpha | |
|---|---|---|---|
| PSWQ | |||
| China | 2.97 | .71 | .89 |
| Belgium | 3.13 | .77 | .93 |
| Champion Fear | |||
| China | 2.85 | 1.04 | .93 |
| Belgium | 2.57 | .89 | .93 |
| BWS | |||
| China | 2.92 | 1.55 | .90 |
| Belgium | 4.26 | 1.47 | .90 |
| RIES | |||
| China | 1.56 | .60 | .89 |
| Belgium | 1.47 | .47 | .78 |
Table 4.
Correlation Matrix for Measures of Dispositional Worry and Dispositional Cancer Worry
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| 1. PSWQ | ||||
| China | – | |||
| Belgium | – | |||
| 2. Champion Fear | ||||
| China | .20** | – | ||
| Belgium | .36** | – | ||
| 3. BWS | ||||
| China | .10 | .44** | – | |
| Belgium | .33** | .61** | – | |
| 4. RIES | ||||
| China | .12 | .25** | .42** | – |
| Belgium | .30** | .46** | .38** | – |
p < .05,
p < .01
(n=208 in China; n=351 in Belgium)
Predictive Validity
Predictive validity is the ability of a measure to predict outcomes consistent with the explication of the construct. The optimal test of predictive validity is a longitudinal design that can rule out other plausible confounds. However, longitudinal designs are cost prohibitive and typically pursued only after a measure has been thoroughly vetted in other ways (to maximize the opportunity). A good first step is to examine the ability of a measure to predict an outcome above and beyond other known/expected predictors. This can be referred to as concurrent validity or as early stage predictive validity.
To examine predictive validity, hierarchical regression analyses were employed to determine if DCW (severity and frequency) could predict a person’s risk perceptions of developing a specific type of cancer (above and beyond gender, general dispositional worry). Perceived risk of developing four types of cancer were examined: breast, lung, colon, and melanoma. Sex was entered in the first block because people’s risk perceptions of developing specific types of cancer (e.g., breast cancer) vary between men and women. The general dispositional worry measure (PSWQ) was entered into the second block, and the DCW scales were entered in the third block. Hierarchical regression analyses were completed for each country. See Table 5 for a summary of results at each step.
Table 5.
Hierarchical Regression Predicting Perceived Cancer Risk from DCW Severity and Frequency
| Type of Cancer | Breast | Lung | Colon | Melanoma | ||||
|---|---|---|---|---|---|---|---|---|
| B (SE) | R2Δ | B (SE) | R2Δ | B (SE) | R2 | B (SE) | R2Δ | |
| China | ||||||||
|
| ||||||||
| Block 1 | .11** | .00 | .00 | .03 | ||||
| Gender | 19.35 (6.95)** | −2.36 (3.98) | −1.73 (5.40) | −4.21 (3.13) | ||||
| Block 2 | .03** | .15** | .08* | .04† | ||||
| PSWQ | 5.04 (3.71) | 10.09 (2.97)** | 9.26 (3.92)** | 2.27 (2.51) | ||||
| Block 3 | .04* | .10** | .13** | .10* | ||||
| BWS (Severity) | 2.36 (1.56) | 4.37 (1.35)** | 6.21 (1.91)** | 2.08 (1.20)† | ||||
| RIES (Frequency) | −.79 (4.10) | .63 (3.69) | .53 (5.34) | 3.43 (3.00) | ||||
|
| ||||||||
| Belgium | ||||||||
|
| ||||||||
| Block 1 | .34** | .00 | .00 | .01† | ||||
| Gender | 31.60 (2.85)** | −2.23 (2.84) | −2.82 (2.62) | 2.64 (2.73) | ||||
| Block 2 | .00 | .02* | .04** | .04** | ||||
| PSWQ | .60 (1.62) | 3.50 (1.84)† | 4.87 (1.72)** | 5.20 (1.76)** | ||||
| Block 3 | .01† | .01 | .01 | .02* | ||||
| BWS (Severity) | 1.94 (.85)* | 1.40 (.95) | 1.68 (.91)† | 1.93 (.91)* | ||||
| RIES (Frequency) | −.24 (2.51) | −2.66 (3.15) | 2.58 (1.81) | −6.01 (2.98)* | ||||
p < .10,
p < .05,
p < .01
The number of subjects providing data for breast, lung, colon, and melanoma was 68, 86, 78, and 66 for China; 297, 287, 275, and 270 for Belgium.
In China, DCW significantly predicted perceived risk of all four cancer types. For perceived breast cancer risk, the regression equation was significant at all three blocks (reported at the third block): R = .41, R2 = .17, F(4, 65) = 3.16, p = .02. DCW accounted for approximately 4% of the variance in perceived breast cancer risk. The coefficient for DCW severity approached statistical significance as a predictor in the model (p = .14). For perceived lung cancer risk in China, the regression equation was significant for the second and third blocks (reported at the third block): R = .50, R2 = .25, F(4, 85) = 6.79, p < .01. DCW accounted for approximately 11% of the variance in perceived lung cancer risk. Specifically, DCW severity was a significant predictor in the model (p < .01). For perceived colon cancer risk in China, the regression equation was significant for the second and third blocks (reported at the third block): R = .46, R2 = .21, F(4, 77) = 4.86, p < .01. DCW accounted for approximately 13% of the variance in perceived colon cancer risk. Specifically, DCW severity was a significant predictor in the model (p < .01). For perceived melanoma risk in China, the regression equation was significant for the second and third blocks (reported at the third block): R = .41, R2 = .17, F(4, 65) = 3.10, p = .02. DCW accounted for approximately 10% of the variance in perceived melanoma risk. Again, DCW severity approached statistical significance as a predictor in the model (p = .08).
In Belgium, DCW was significantly related to risk perceptions for three of the four cancer types. For perceived breast cancer risk, the regression equation was significant at all three blocks (reported at the third block): R = .60, R2 = .35, F(4, 296) = 40.03, p < .01. DCW accounted for approximately 1% of the variance in perceived breast cancer risk. The coefficient for DCW severity was a significant predictor in the model (p = .02). For perceived lung cancer risk in Belgium, the regression equation approached statistical significance for the second block only: R = .13, R2 = .02, F(2, 286) = 2.42, p = .09. DCW did not account for any variance in perceived lung cancer risk above and beyond dispositional worry. For perceived colon cancer risk in Belgium, the regression equation was significant for the second and third blocks (reported at the third block): R = .23, R2 = .06, F(4, 274) = 3.90, p < .01. DCW accounted for approximately 1% of the variance in perceived colon cancer risk. Specifically, DCW severity approached statistical significance as a predictor in the model (p = .07). For perceived melanoma risk in Belgium the regression equation was significant for all three blocks (reported at the third block): R = .27, R2 = .07, F(4, 269) = 5.06, p < .01. DCW accounted for approximately 2% of the variance in perceived melanoma risk. Specifically, both DCW severity and cancer worry frequency were significant predictors in the model (p < .05).
Discussion
The BWS and RIES were found to be reliable and valid measures of DCW severity and frequency in two different cultures. Consistent with past research, DCW had two factors that loaded as expected in exploratory factor analysis, and the two dimensioned functioned differently in other analyses. For example, across both cultures, DCW severity was more consistent than DCW frequency at predicting cancer risk perceptions. This parallels the findings of Jensen et al. (2010) and further suggests that worry severity may be more powerful at shaping risk perceptions.
DCW is a context-specific construct that raises the question, “Is a context-specific measure necessary?” Jensen et al. (2010) found that DCW severity and frequency were moderately correlated with measures of general dispositional worry; and that DCW predicted significant variance in risk perceptions above and beyond the latter. The current results replicate these findings as (once again) DCW was distinct from general dispositional cancer worry. In Belgium, DCW was moderately correlated with general dispositional worry (mirroring findings from Jensen et al., 2010). Of interest, DCW was not significantly correlated with general dispositional worry in China. In other words, Chinese worriers are not more likely to worry about cancer. Initially, this finding seems at odds with actual health data. For instance, cancer has long been a health issue in China as exemplified by the formation of a China National Office for Cancer Prevention and Control in 1986 (Zhao, Dai, Chen, & Li, 2010). However, perhaps other health threats are more salient in China or cancer is framed or constructed differently in media/communication channels. For example, there is evidence that cancer has increased as a topic of discussion in Chinese media. Cai and colleagues (2009) found that the number of cancer news stories increased steadily from 2000 – 2007. Moreover, in a content analysis of 2007 news coverage, Peng and Tang (2010) found that cancer receives more coverage than any other illness in China. Accordingly, cross-cultural research should explore potential causes and effects of this difference in perception. Since the relationship between DCW and cancer-related behaviors is currently unclear, it is not apparent whether this difference is a concern or a resource for Chinese public health efforts.
The relationship between DCW and cancer fear was different in China as well. Among Americans, DCW severity (r = .69) and frequency (r = .41) were strongly correlated with cancer fear, a pattern that was replicated in the Belgium sample (severity: r = .61; frequency: r = .46). In China, the relationship between cancer fear and DCW was smaller (r = .44 and .25, respectively). For example, cancer fear and DCW severity are strongly correlated across all three cultures, yet the size of that relationship decreases within China. Thus, there are several relationships in the data that suggest DCW could function differently in China. Related findings have emerged in other research; for instance, Hambrick and colleagues (2010) found that worry measures (e.g., the PSWQ) performed differently in White and Asian American students.
In Belgium, DCW was significantly related to cancer risk perceptions, yet cancer worry explained significantly less variance than for other samples (China, America). For instance, DCW explained between 4 – 13% of the variance in Chinese cancer risk perceptions, but only 1–2% of the variance among Belgium participants. Researchers have found worry measures (e.g., PSWQ) to be reliable and valid for Dutch populations (van der Heiden, Muris, Bos, & van der Molen, 2010; Verkuil & Brosschot, 2012); however, more research needs to investigate the Dutch worry process.
Limitations and future research directions
In retrospect, there were two issues that may have impacted the results of the study. First, a native speaker translated each survey; however, back-translations were not conducted. Due to the subjective nature of translation, there may have been slight transformations in the survey’s initial items, which may have led to differences in interpreting the measure. Future research should conduct back-translations on the surveys, and then, conduct data collection and analysis for replication. Second, our study groups represented a convenience sample of individuals willing to enroll through our recruitment strategies and thus probably are affected by some degree of selection bias.
Lastly, and most importantly, future research should pursue longitudinal tests of DCW’s predictive validity. Examining whether DCW severity and frequency predicts meaningful cancer outcomes over time is a priority. Research could explore whether individuals with higher DCW severity and/or frequency are more likely to engage in cancer prevention or detection. DCW could also shape (or be shaped by) risk perceptions; a postulate that could be tested by surveying individuals before and after genetic counseling (for example).
In a larger sense, Consedine & Moskowitz (2007) have advocated for increased theoretical work explicating relationships between emotions and health. Both DCW severity and frequency measures have proved to be reliable and valid in several cultures, thus they could be used alongside a theoretical model predicting health behavior, like the Theory of Planned Behavior (Ajzen, 1985). The clinical implications of using a theoretical model will help researchers understand the relationship between DCW and behavior and to be able to predict how DCW may impact cancer prevention and early detection activities. Ultimately, this knowledge could inform message construction to counteract any adverse reactions DCW may have on one’s future health decisions and to increase uptake of prevention and early detection activities.
Implications for Clinical Practice
Patients often worry about cancer, and the results of the current study provide practitioners with a means for measuring DCW severity and frequency in China and Belgium. This will support continued international research of DCW as well as enhance practitioners understanding of how worry facilitates or undermines their efforts. Importantly, practitioners should be aware that there is a growing body of evidence suggesting that DCW severity is central to understanding this situation. That is, available evidence indicates that how frequently a person worries about cancer is less important than DCW severity. Patients who report worrying about the severe consequences of cancer appear to have greater risk perceptions, and perhaps are more likely to act on those concerns.
Acknowledgments
This work was supported by the National Cancer Institute’s Training in Research for Behavioral Oncology & Cancer Control program (R25 – CA117865); the National Science Foundation East Asia and Pacific Summer Institutes program (Award #0913493); and Purdue University Office of Programs for Study Abroad Overseas Research Internship.
Appendix A. Final measures of DCW with prompts and scale anchors in English, Mandarin, and Dutch
INSTRUCTIONS
Now we are going to ask you a lot of questions about how you feel about cancer. We’re going to ask these questions in a number of ways, and at times, you might think we’re asking the same question twice. Many of the questions will sound similar, but we’re interested in understanding the answers to these questions as best we can.
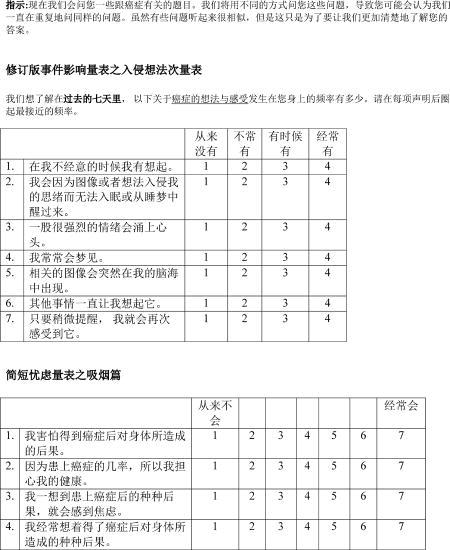
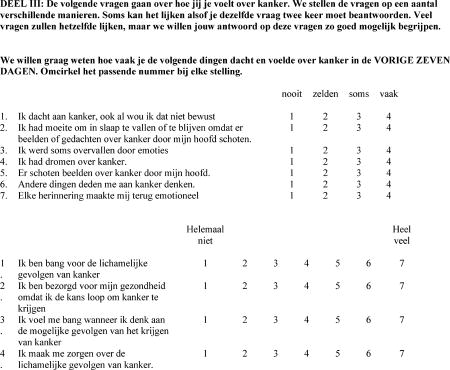
Intrusive Thoughts Subscale of Revised Impact of Events Scale
We wish to know how frequently the following thoughts and feelings about cancer happened for you DURING THE PAST SEVEN DAYS. Simply circle one number by each statement.
| not at all | rarely | sometimes | often | ||
|---|---|---|---|---|---|
| 1. | I thought about it when I didn’t mean to. | 1 | 2 | 3 | 4 |
| 2. | I had trouble falling asleep or staying asleep, because of pictures or thoughts about it that came into my mind. | 1 | 2 | 3 | 4 |
| 3. | I had waves of strong feelings about it. | 1 | 2 | 3 | 4 |
| 4. | I had dreams about it. | 1 | 2 | 3 | 4 |
| 5. | Pictures about it popped into my mind. | 1 | 2 | 3 | 4 |
| 6. | Other things kept making me think about it. | 1 | 2 | 3 | 4 |
| 7. | Any reminder brought back feelings about it. | 1 | 2 | 3 | 4 |
Brief Worry Scale
| not at all | very much | |||||||
|---|---|---|---|---|---|---|---|---|
| 1. | I am afraid of the physical consequences of getting cancer. | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| 2. | I worry about my health because of my chances of getting cancer. | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| 3. | I feel anxiety when I think of the possible consequences of getting cancer. | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| 4. | I brood about the physical consequences of getting cancer | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
Contributor Information
Jennifer Kim Bernat, Indiana University.
Jakob D. Jensen, University of Utah
References
- Arora NK, Hesse BW, Rimer BK, Viswanath K, Clayman ML, Croyle RT. Frustrated and confused: The American public rates its cancer-related information-seeking experiences. Journal of General Internal Medicine. 2008;23:223–228. doi: 10.1007/s11606-007-0406-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajzen I. From intentions to actions: A theory of planned behavior. In: Kuhl J, Beckmann J, editors. Action control: From cognition to behavior. New York: Springer –Verlag; 1985. pp. 11–39. [Google Scholar]
- Bloom JR, Hayes WA, Saunders F, Flatt C. Cancer awareness and secondary prevention practices in Black Americans: Implications for intervention. Family Community Health. 1987;10:19–30. [Google Scholar]
- Borkovec TD, Robinson E, Pruzinsky T, Dupree JA. Preliminary exploration of worry: Some characteristics and processes. Behaviour Research and Therapy. 1983;21:9–16. doi: 10.1016/0005-7967(83)90121-3. [DOI] [PubMed] [Google Scholar]
- Bowen DJ, Helmes A, Powers D, Andersen MR, Burke W, McTiernan A, Durfy S. Predicting breast cancer screening intentions and behavior with emotion and cognition. Journal of Social and Clinical Psychology. 2003;22:213–232. [Google Scholar]
- Cai J, Yang L, Liu Z, Ma Z, Liu Y. Comprehensive analysis of cancer coverage in important Chinese newspapers between 2000 and 2007. Supportive Care International. 2009;17:329–332. doi: 10.1007/s00520-008-0494-1. [DOI] [PubMed] [Google Scholar]
- Champion VL, Skinner CS. A breast cancer fear scale: Psychometric development. Journal of Health Psychology. 2004;9:753–762. doi: 10.1177/1359105304045383. [DOI] [PubMed] [Google Scholar]
- Consedine NS, Moskowitz JT. The role of discrete emotions in health outcomes: A critical review. Applied and Preventative Psychology. 2007;12:59–75. [Google Scholar]
- Consedine NS, Magai C, Neugut AI. The contribution of emotional characteristics to breast cancer screening. Preventative Medicine. 2004;38:64–77. doi: 10.1016/j.ypmed.2003.09.030. [DOI] [PubMed] [Google Scholar]
- Davey GCL, Hampton J, Farrell J, Davidson S. Some characteristics of worrying: Evidence for worrying and anxiety as separate constructs. Personality & Individual Differences. 1992;13:133–47. [Google Scholar]
- DiLorenzo TA, Schnur J, Montgomery GH, Erblich J, Winkel G, Bovbjerg DH. A model of disease-specific worry in heritable disease: The influence of family history, perceived risk, and worry about other illness. Journal of Behavioral Medicine. 2006;29(1):37–49. doi: 10.1007/s10865-005-9039-y. [DOI] [PubMed] [Google Scholar]
- Dijkstra A, Brosschot J. Worry about health in smoking behaviour change. Behaviour Research and Therapy. 2003;41:1081–1092. doi: 10.1016/s0005-7967(02)00244-9. [DOI] [PubMed] [Google Scholar]
- Edwards NI, Jones DA. Uptake of breast cancer screening in older women. Age Ageing. 2000;29:131–5. doi: 10.1093/ageing/29.2.131. [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang AG, Buchner A. G*power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39(2):175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. GOBOCAN 2008, Cancer Incidence and Mortality Worldwide. IARC CancerBase No. 10. 2010 Retrieved February 28, 2010 from http://globocan.iarc.fr.
- Hambrick JP, Rodebaugh TL, Balsis S, Woods CM, Mendez JL, Heimberg RG. Cross-ethnic measurement equivalence of measures of depression, social anxiety, and worry. Assessment. 2010;17(2):155–171. doi: 10.1177/1073191109350158. [DOI] [PubMed] [Google Scholar]
- Horowitz MJ, Wilner N, Alverez W. Impact of event scale: A measure of subjective stress. Psychosomatic Medicine. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Jensen JD, Bernat JK, Davis LA, Yale R. Dispositional cancer worry: Convergent, divergent, and predictive validity of existing scales. Journal of Pyschosocial Oncology. 2010;28(5):470–489. doi: 10.1080/07347332.2010.498459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehto RH, Cimprich B. Worry and the formation of cognitive representations of illness in individuals undergoing surgery for suspected lung cancer. Cancer Nursing. 2009;32:2–10. doi: 10.1097/01.NCC.0000343363.75752.f1. [DOI] [PubMed] [Google Scholar]
- McQueen A, Vernon SW, Swank PR. Construct definition and scale development for defensive information processing: An application to colorectal cancer screening. Health Psychology. 2013;32(2):190–202. doi: 10.1037/a0027311. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Miles A, Voorwinden S, Chapman S, Wardle J. Psychologic predictors of cancer information avoidance among older adults: The role of cancer fear and fatalism. Cancer Epidemiol Biomarkers Prev. 2008;17:1872–1879. doi: 10.1158/1055-9965. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. Global burden of cancer. Center for Global Health; 2013. Retrieved July 17,2013 from http://www.cancer.gov/aboutnci/globalhealth. [Google Scholar]
- National Cancer Institute. Mission statement. Health Communication and Informatics Research: Cancer Control and Population Sciences; 2008. Retrieved November 6,2008 from http://dccps.nci.nih.gov/hcirb/about.html. [Google Scholar]
- Peng W, Tang L. Health content in Chinese newspapers. Journal of Health Communication. 2010;15:695–711. doi: 10.1080/10810730.2010.514028. [DOI] [PubMed] [Google Scholar]
- Pruzinsky T, Borkovec TD. Cognitive and personality characteristics of worriers. Behaviour Research and Therapy. 1990;28:507–512. doi: 10.1016/0005-7967(90)90137-8. [DOI] [PubMed] [Google Scholar]
- Scholz U, Gutiérrez-Doña B, Sud S, Schwarzer R. Is general self-efficacy a universal construct? Psychometric findings from 25 countries. European Journal of Psychological Assessment. 2002;18:242–251. [Google Scholar]
- Schwarzer R, Jerusalem M. Generalized Self-Efficacy scale. In: Weinman J, Wright S, Johnston M, editors. Measures in health psychology: A user’s portfolio. Causal and control beliefs. Windsor, UK: NFER-NELSON; 1995. pp. 35–37. [Google Scholar]
- Shen L, Condit CM. Addressing fatalism with health messages. In: Cho H, editor. Health communication message design: Theory and practice. Thousand Oaks, CA: Sage; 2011. pp. 191–208. [Google Scholar]
- Shen L, Condit CM, Wright L. The psychometric property and validation of a fatalism scale. Psychology and Health. 2009;24:597–613. doi: 10.1080/08870440801902535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman S, Valente TW, Rohrbach LA, Skara S, Pentz MA. Translation in the health professions: Converting science into action. Evaluation & the Health Professions. 2006;29(1):7–32. doi: 10.1177/0163278705284441. [DOI] [PubMed] [Google Scholar]
- Tallis F, Eysenck MW, Mathews A. A questionnaire for the measurement of nonpathological worry. Personality and Individual Differences. 1992;13(2):161–168. [Google Scholar]
- van der Heiden C, Muris P, Bos AR, van der Molen HT. Factor structure of the Dutch version of the Penn State Worry Questionnaire. Journal Of Behavior Therapy And Experimental Psychiatry. 2010;41(3):304–309. doi: 10.1016/j.jbtep.2010.02.009. [DOI] [PubMed] [Google Scholar]
- Verkuil B, Brosschot JF. The online version of the Dutch Penn State Worry Questionnaire: Factor structure, predictive validity and reliability. Journal Of Anxiety Disorders. 2012;26(8):844–848. doi: 10.1016/j.janxdis.2012.08.002. [DOI] [PubMed] [Google Scholar]
- Vernon SW, Laville EA, Jackson GL. Participation in breast screening programs: A review. Social Science and Medicine. 1990;30:1107–1118. doi: 10.1016/0277-9536(90)90297-6. [DOI] [PubMed] [Google Scholar]
- Viswanath K. The communications revolution and cancer control. Nature Reviews Cancer. 2005;5:828–835. doi: 10.1038/nrc1718. [DOI] [PubMed] [Google Scholar]
- Weiss D, Marmar C. The impact of event scale – revised. In: Wilson J, Keane T, editors. Assessing psychological trauma and PTSD. New York: Guilford; 1997. pp. 168–189. [Google Scholar]
- Zhao P, Dai M, Chen W, Li N. Cancer trends in China. Japanese Journal of Clinical Oncology. 2010;40:281–285. doi: 10.1093/jjco/hyp187. [DOI] [PubMed] [Google Scholar]


