Abstract
Purpose
We performed this retrospective study to determine the main causes for early and late failures of unicompartmental knee arthroplasty (UKA).
Methods
Between January 2000 and March 2012, all patients treated for a failed medial UKA in the authors’ institution were retrospectively reviewed. A total of 471 patients were identified, and causes of failure were analysed based on the medical records and radiographs at the time of revision.
Results
The cohort included 161 males and 310 females, with a mean age of 67.7 years (range, 42–91 years; SD = 10.1) at the time of revision. The mean time from index arthroplasty to revision surgery was 6.1 years (range, 0.1–27.9 years; SD = 5.6). A total of 254 cases (53.9 %) failed within five years after primary implantation, and 108 cases (22.9 %) failed after ten years. The major reason for failure was the development of other compartment arthritis (39.5 %), followed by aseptic loosening (25.4 %).
Conclusions
Of importance, the mean time to failure after UKA was 6.1 years, with more than 50 % of failures occurring within the first five years postoperatively.
Keywords: Unicompartmental knee arthroplasty, Unicondylar knee arthroplasty, Failure, Aseptic loosening, Outcome
Introduction
Unicompartmental knee arthroplasty (UKA) has been shown to be a satisfactory and less invasive alternative to total knee arthroplasty (TKA) in selected patients [1]. In recent years, UKA has again gained increased popularity for the treatment of localized, medial compartmental osteoarthritis of the knee [2], although early studies [3, 4] of UKA reported revision rates as high as 32 % within seven years of follow-up.
More recent studies have presented survival rates of greater than 90 % at ten years of follow-up in certain prosthetic designs [5–9], while the use of new technology such as computer-assisted surgery systems in UKA has also resulted in improved postoperative alignment, reduction of outliers and better postoperative clinical results [10–13].
Foran et al. reported on the long-term outcomes and failure modes of UKA, with a survival rate of 93 % at 15 years and 90 % at 20 years [7]. Only four out of 62 patients (9.7 %) were revised to TKA, with no patients revised due to septic or aseptic loosening [7].
The majority of published articles report on the outcomes following medial UKA in a consecutive series. However, there are only a few studies analysing failed medial unicompartmental knee arthroplasties. Epinette et al. reported on the failure modes following UKA in 418 failed UKA patients in a multi-centre study, including 25 hospitals over a 31-year period [14]. More recently, Sierra et al. reported on the outcomes of 175 revised unicompartmental knee arthroplasties in three US centres. Prior studies have been limited by either small patient numbers or the combining of patient groups from different surgical centers [14–16]. Only a few studies analysed a higher number of cases, albeit those studies were derived from arthroplasty registries [17, 18] (Table 1).
Table 1.
Study characteristics
| Studies | Number of cases | Study design |
|---|---|---|
| Epinette et al. [14] | 418 | Multicentre study |
| Saragaglia et al. [15] | 418 | Multicentre study |
| Sierra et al. [16] | 175 | Multicentre study |
| Swedish registry [18] | 1,576 | Arthroplasty registry |
| Australian registry [20] | 2,882 | Arthroplasty registry |
| Present study | 471 | Single center study |
We therefore report on our results of 471 failed medial UKA cases at a single institution. The purpose was to characterize the main causes of failure, as well as the timing of failure after index surgery.
Materials and methods
Study design
Patients who were treated for a failed medial UKA were identified by querying the electronic database from January 2000 through March 2012. Exclusion criteria were index lateral UKA and previous surgery before implantation of UKA. During this time interval, 488 consecutive patients were converted to total knee arthroplasty at our institution. A total of 471 patients met the inclusion criteria and were included in this study.
Surgical method
All revision surgeries were performed by experienced arthroplasty surgeons, who individually perform more than 300 cases per year at our referral arthroplasty centre. Every patient underwent aspiration of synovial fluid pre-operatively to rule out periprosthetic joint infection (PJI). In cases of confirmed PJI, one-stage revision arthroplasty was performed based on our standard hospital protocol. Patients with stable collateral ligaments were converted to conventional (i.e. unconstrained) TKA, while patients with unstable collateral ligaments were converted to constrained implants. Hospital for Special Surgery (HSS) scores were obtained in all patients at the time of revision through query of the electronic database.
Definition of UKA failure
The Knee Society roentgenographic evaluation system was used to assess the femoro-tibial angle and any radiolucencies about the femur and tibia on the anteroposterior and lateral projections [19]. The reason for revision was based on patient symptoms, documented history, diagnostic imaging, and intra-operative findings. Any revision surgery was defined as failure of the medial UKA.
Outcome measures
Demographics for all patients were recorded at the time of revision surgery, including gender, age, body mass index (BMI), and surgical side. The dates of primary implantation and revision surgery were obtained. All reasons for early and late failure were noted. Other compartment arthritis was defined as arthritis in the lateral and/or patellofemoral compartment. The mean femoro-tibial angles were compared between failed patients due to development of other compartment arthritis and the remaining causes. Furthermore, patients who failed within five years of primary arthroplasty were compared for age at primary implantation, BMI at time of revision, preoperative HSS score, femorotibial angles and causes for failure with those patients who failed after five years.
Statistical analysis
All data were processed using GraphPad Prism (Version 5.0d, La Jolla, CA, USA). Descriptive statistics are presented in the form of number of occurrences and percentage, or mean, and standard deviation (SD) and range. The Mann-Whitney test was used to calculate the differences between groups. Threshold for statistical significance for those analyses was set at α = 0.05.
Results
Demographic data
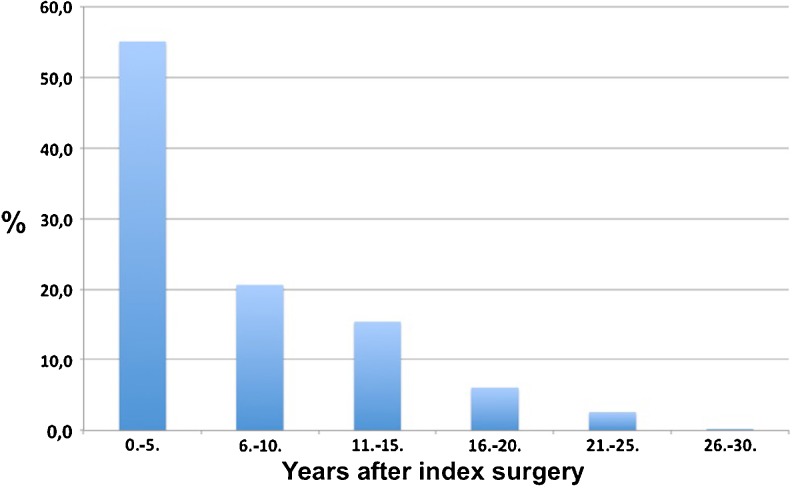
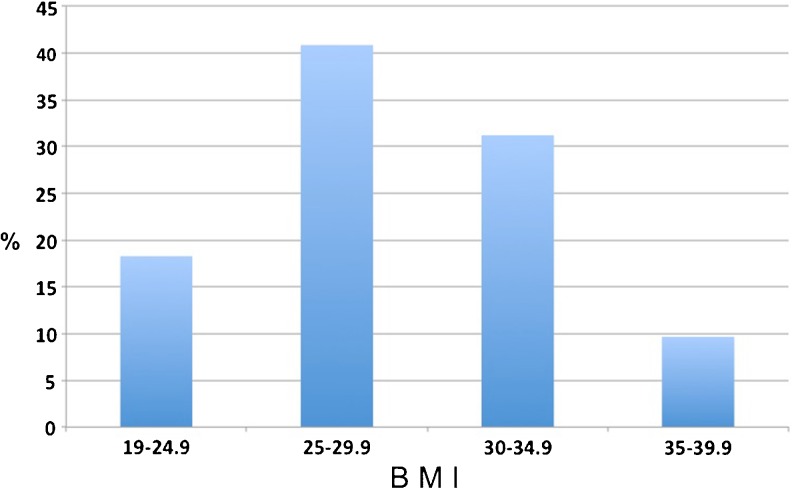
The cohort of failed medial UKA patients included in the study consisted of 161 males (34.2 %) and 310 females (65.8 %). The mean age at time of revision was 67.7 years (range, 42–91 years; SD = 10.1). The mean age at time of index surgery was 61.3 years (range, 29–84 years; SD = 9.7). In 234 cases (49.7 %), the right knee was revised, while the left side was affected in 237 cases (50.3 %). The mean pre-operative HSS score was 53.2 (range, 5–87; SD = 15.2). The mean time from index arthroplasty to revision surgery was 6.1 years (range, 0.1–27.9 years; SD = 5.6). A total of 254 cases (53.9 %) failed within five years after primary implantation, and 108 cases (22.9 %) failed after ten years (Fig. 1). The mean BMI at time of revision was 28.7 kg/m2 (range, 19–38 kg/m2; SD = 4.2), with approximately 60 % of the failed UKA patients having a BMI less than 30 kg/m2 (Fig. 2).
Fig. 1.
Time interval distribution of failed unicompartmental knee arthroplasties (UKAs). More than 50 % of the failures occurred within five years of primary arthroplasty
Fig. 2.
Distribution of body mass index (BMI) for failed unicompartmental knee arthroplasties (UKAs) at the time of revision surgery. Less than 10 % of patients had a BMI greater than 35 kg/m2
Causes for failure
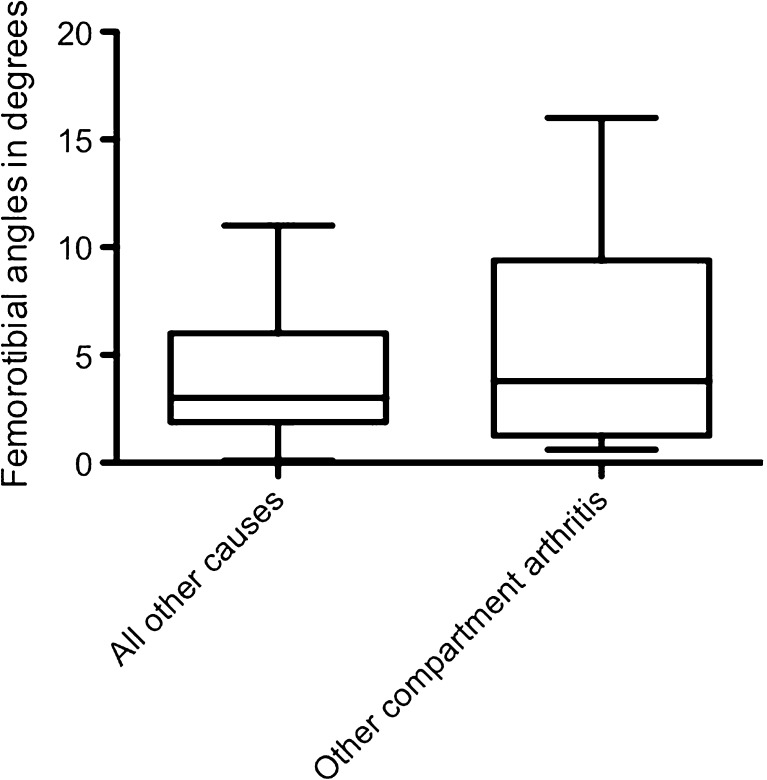
Overall, the major reasons for failure were development of other compartment arthritis of the lateral and/or patellofemoral compartment (39.5 %), aseptic loosening (25.4 %), and instability (15.3 %). Infection was present in 1.5 % of cases. Revision due to persistent pain and arthrofibrosis was performed in 1.8 % and 2.5 % of patients, respectively. Relevant polyethylene wear was noted in 14 % of patients (Table 2). The mean femorotibial angle of the failed patients due to development of other compartment arthritis was 5.3° (range, 0.6°–16°; SD = 4.4), while the femorotibial angle in failed cases due to other reasons was 3.9° (range, 0.1°–11°; SD = 2.7). However, there were no significant differences between these groups (p = 0.47) (Fig. 3).
Table 2.
Modes of failure for all patients and for patients who failed within five years after index surgery
| Mode of failure | Percent of all patients (%) | Percent of patients who failed within five years after index surgery (%) |
|---|---|---|
| Contralateral arthritis | 39.5 | 44.1 |
| Aseptic loosening | 25.4 | 30.7 |
| Instability | 15.3 | 12.6 |
| Infection | 1.5 | 3.9 |
| Arthrofibrosis | 2.5 | 3.1 |
| Persistent pain | 1.8 | 3.5 |
| Polyethylene wear | 14 | 2 |
Fig. 3.
Femoro-tibial angles for failed unicompartmental knee arthroplasty (UKA) due to development of other compartment arthritis and for all other causes of failure. There were no significant differences in coronal plane deformity between groups
Early and late failures
For patients who failed within five years after index implantation, the major reason for failure was development of arthritis in other compartments, followed by aseptic loosening (Table 2). Polyethylene wear was less common in this subset of patients. When comparing patients who failed within five years of primary arthroplasty with those patients who failed after five years, there were no significant differences with respect to age at primary implantation, BMI at time of revision, pre-operative HSS score, and femoro-tibial angles (Table 3).
Table 3.
Variables for cases that failed within five years versus those that failed after five years following primary surgery
| Variable | Within five years | More than five years | p-value |
|---|---|---|---|
| Age (years) | 61.9 | 60.7 | 0.187 |
| BMI (kg/m2) | 28.2 | 28.9 | 0.232 |
| HSS score | 53.3 | 53.9 | 0.771 |
| Femoro-tibial angle (°) | 4.9 | 4.2 | 0.771 |
BMI body mass index, HSS Hospital for Special Surgery
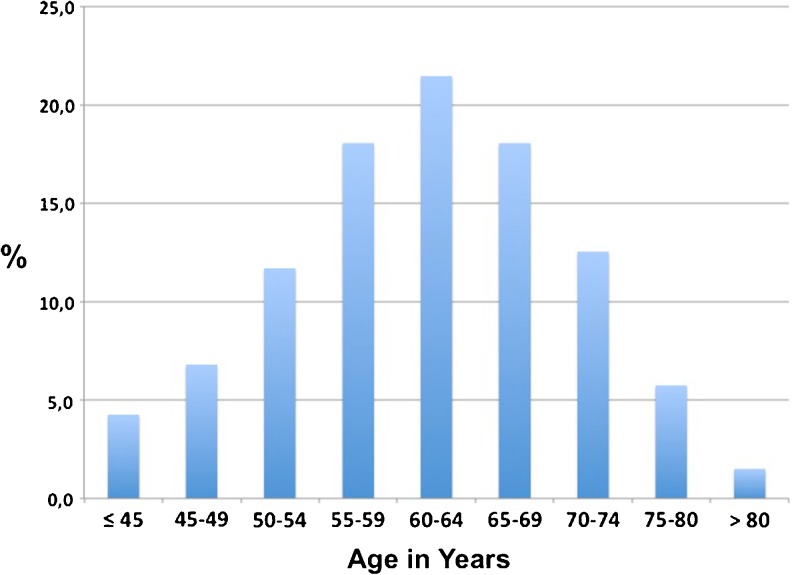
Interestingly, patients with implant survival more than ten years were significantly younger at the time of primary implantation, compared to the patients who failed within five years (Table 4). However, there were no significant differences with respect to BMI, HSS score, and femorotibial angles between these two groups (Table 4). At the time of index surgery, 40.8 % of patients were younger than 60 years old, and 59.2 % were ≥60 years of age (Fig. 4).
Table 4.
Variables for cases that failed within five years versus those that failed after ten years following primary surgery
| Variable | Within five years | More than ten years | p-value |
|---|---|---|---|
| Age (years) | 61.9 | 58.7 | 0.0049 |
| BMI (kg/m2) | 28.2 | 29.0 | 0.321 |
| HSS score | 53.3 | 54.1 | 0.544 |
| Femorotibial angle (°) | 4.9 | 4.6 | 0.991 |
BMI body mass index, HSS Hospital for Special Surgery
Fig. 4.
Age distribution at the time of index surgery
Discussion
The majority of published articles report on the outcomes following medial UKA in consecutive series with relatively small numbers of cases, varying from 60 to 203 patients [5–9, 20–25]. There are only a few studies analysing failed medial unicompartmental knee arthroplasties. However, to the authors’ knowledge, this is the largest single-centre study to date evaluating the failure modes after medial UKA. Only a few studies analysed a higher number of cases, albeit those studies were derived from arthroplasty registries [17, 18] (Table 1).
The most important finding of our single-centre study was that more than 50 % of revised cases failed within the first five years after implantation. This result is similar to that of a prior cohort study by Epinette et al. [14]. Interestingly, patients who failed within five years were significantly older at the time of first implantation, when compared to patients with prosthetic survival more than ten years. In our cohort, more than 59.2 % of patients were ≥60 years of age at the time of index surgery. The reason for early failure in the older patients might be the advanced underlying arthritis in other compartments at baseline/pre-operatively. Another reason could be the poorer bone stock leading to aseptic loosening.
In contrast to most previous studies, aseptic loosening was not the most common reason for failure in our study (Table 5) [14, 16, 24]. In our cohort, the development of arthritis in other compartments was the main reason for revision surgery. We hypothesized that failed medial UKAs due to unresurfaced compartment arthritis had a higher femorotibial angle compared to failed cases due to other aetiologies. However, despite the finding that femoro-tibial angles tended to be higher in patients with contralateral arthritis, there were no significant differences between the groups. The degree of angular deformity was also similar between patients who failed within five years and patients who failed after ten years following primary arthroplasty. Other compartment arthritis was also the most common reason for failure in patients who failed within five years. As expected, polyethylene wear was less common in this patient group compared to the remaining collective.
Table 5.
Comparison of data in previous and the present study
The mean BMI at time of revision in this study was 28.7 kg/m2, with approximately 60 % of the failed UKA patients exhibiting a BMI less than 30 kg/m2. Less than 40 % were obese. In our series, the BMI showed no significant relation to time of revision, i.e. within five years and after ten years following primary implantation. However, it must be noted that BMI was noted only at the time of revision. Those patients could have theoretically higher/lower BMI at the time of index surgery. Berend et al. concluded that BMI greater than 32 kg/m2 increased failure rates [26].
Limitations of the study include that radiographs prior to medial UKA do not exist in the majority of cases. Therefore, we cannot draw definitive conclusions regarding potential poor radiographic indications for surgery, especially for those UKAs that failed early. Another limitation is that the implant type (e.g. “metal-backed” versus “all-polyethylene” tibial tray) was not analysed, since the information about the implant type did not exist in every case. Primary implantation was performed in several hospitals, including low-volume and high-volume centres, which may affect the outcomes following knee arthroplasty [27]. Other weaknesses include a retrospective study design and coded diagnosis data, lack of multiple regression analysis, and the unknown causes for failure for those patients that might have been revised elsewhere or were lost to follow-up. A key strength of this report is the large number of consecutive patients with failed UKAs available for study inclusion. Another strength is the single-centre study design, with general consistency in surgical technique, philosophy for unicompartmental surgery patient indications, and rehabilitation.
In summary, this study showed that the mean time of failure after UKA was 6.1 years, with more than 50 % of failures occurring within the first five years after primary arthroplasty. The main reason for early and late failure after medial UKA was advancing arthritis in other compartments, followed by aseptic loosening. Polyethylene wear as a contributing factor in early failure is extremely rare. Also periprosthetic infection does not play a strong role in UKA failures. Appropriate patient indications, as well as consideration of age at the time of implantation, may reduce the overall incidence of failure following medial UKA.
References
- 1.Berger RA, Nedeff DD, Barden RM, Sheinkop MM, Jacobs JJ, Rosenberg AG, Galante JO. Unicompartmental knee arthroplasty. Clinical experience at 6- to 10-year followup. Clin Orthop Relat Res. 1999;367:50–60. doi: 10.1097/00003086-199910000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Ohdera T, Tokunaga J, Kobayashi A. Unicompartmental knee arthroplasty for lateral gonarthrosis: midterm results. J Arthroplasty. 2001;16(2):196–200. doi: 10.1054/arth.2001.2090. [DOI] [PubMed] [Google Scholar]
- 3.Insall J, Aglietti P. A five to seven-year follow-up of unicondylar arthroplasty. J Bone Joint Surg Am. 1980;62(8):1329–1337. [PubMed] [Google Scholar]
- 4.Lindstrand A, Stenstrom A, Lewold S. Multicenter study of unicompartmental knee revision. PCA, Marmor, and St Georg compared in 3,777 cases of arthrosis. Acta Orthop Scand. 1992;63(3):256–259. doi: 10.3109/17453679209154777. [DOI] [PubMed] [Google Scholar]
- 5.Berger RA, Meneghini RM, Jacobs JJ, Sheinkop MB, Della Valle CJ, Rosenberg AG, Galante JO. Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J Bone Joint Surg Am. 2005;87(5):999–1006. doi: 10.2106/JBJS.C.00568. [DOI] [PubMed] [Google Scholar]
- 6.Cartier P, Sanouiller JL, Grelsamer RP. Unicompartmental knee arthroplasty surgery. 10-year minimum follow-up period. J Arthroplasty. 1996;11(7):782–788. doi: 10.1016/S0883-5403(96)80177-X. [DOI] [PubMed] [Google Scholar]
- 7.Foran JR, Brown NM, Della Valle CJ, Berger RA, Galante JO. Long-term survivorship and failure modes of unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2013;471(1):102–108. doi: 10.1007/s11999-012-2517-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murray DW, Goodfellow JW, O’Connor JJ. The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg Br. 1998;80(6):983–989. doi: 10.1302/0301-620X.80B6.8177. [DOI] [PubMed] [Google Scholar]
- 9.Svard UC, Price AJ. Oxford medial unicompartmental knee arthroplasty. A survival analysis of an independent series. J Bone Joint Surg Br. 2001;83(2):191–194. doi: 10.1302/0301-620X.83B2.10966. [DOI] [PubMed] [Google Scholar]
- 10.Manzotti A, Cerveri P, Pullen C, Confalonieri N. Computer-assisted unicompartmental knee arthroplasty using dedicated software versus a conventional technique. Int Orthop. 2013 doi: 10.1007/s00264-013-2215-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saragaglia D, Picard F, Refaie R. Navigation of the tibial plateau alone appears to be sufficient in computer-assisted unicompartmental knee arthroplasty. Int Orthop. 2012;36(12):2479–2483. doi: 10.1007/s00264-012-1679-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buckup K, Linke LC, Hahne V. Minimally invasive implantation and computer navigation for a unicondylar knee system. Orthopedics. 2007;30(8 Suppl):66–69. [PubMed] [Google Scholar]
- 13.Molfetta L, Caldo D. Computer navigation versus conventional implantation for varus knee total arthroplasty: a case-control study at 5 years follow-up. Knee. 2008;15(2):75–79. doi: 10.1016/j.knee.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 14.Epinette JA, Brunschweiler B, Mertl P, Mole D, Cazenave A. Unicompartmental knee arthroplasty modes of failure: wear is not the main reason for failure: a multicentre study of 418 failed knees. Orthop Traumatol Surg Res. 2012;98(6 Suppl):S124–S130. doi: 10.1016/j.otsr.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 15.Saragaglia D, Bonnin M, Dejour D, Deschamps G, Chol C, Chabert B, Refaie R. Results of a French multicentre retrospective experience with four hundred and eighteen failed unicondylar knee arthroplasties. Int Orthop. 2013;37(7):1273–1278. doi: 10.1007/s00264-013-1915-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sierra RJ, Kassel CA, Wetters NG, Berend KR, Della Valle CJ, Lombardi AV. Revision of unicompartmental arthroplasty to total knee arthroplasty: not always a slam dunk! J Arthroplasty. 2013;28(8 Suppl):128–132. doi: 10.1016/j.arth.2013.02.040. [DOI] [PubMed] [Google Scholar]
- 17.Sundberg M, Lidgren L, Dahl A, Robertson O (2011) The Swedish knee arthroplasty register. Annual report 2011 [DOI] [PMC free article] [PubMed]
- 18.Tomkins A (2011) Australian Orthopaedic Association. National joint replacement registry. Annual report 2011
- 19.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed] [Google Scholar]
- 20.Hernigou P, Deschamps G. Patellar impingement following unicompartmental arthroplasty. J Bone Joint Surg Am. 2002;84-A(7):1132–1137. doi: 10.2106/00004623-200207000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Jarvenpaa J, Kettunen J, Miettinen H, Kroger H. The clinical outcome of revision knee replacement after unicompartmental knee arthroplasty versus primary total knee arthroplasty: 8–17 years follow-up study of 49 patients. Int Orthop. 2010;34(5):649–653. doi: 10.1007/s00264-009-0811-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mercier N, Wimsey S, Saragaglia D. Long-term clinical results of the Oxford medial unicompartmental knee arthroplasty. Int Orthop. 2010;34(8):1137–1143. doi: 10.1007/s00264-009-0869-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Newman J, Pydisetty RV, Ackroyd C. Unicompartmental or total knee replacement: the 15-year results of a prospective randomised controlled trial. J Bone Joint Surg Br. 2009;91(1):52–57. doi: 10.1302/0301-620X.91B1.20899. [DOI] [PubMed] [Google Scholar]
- 24.Saragaglia D, Estour G, Nemer C, Colle PE. Revision of 33 unicompartmental knee prostheses using total knee arthroplasty: strategy and results. Int Orthop. 2009;33(4):969–974. doi: 10.1007/s00264-008-0585-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Steele RG, Hutabarat S, Evans RL, Ackroyd CE, Newman JH. Survivorship of the St Georg Sled medial unicompartmental knee replacement beyond ten years. J Bone Joint Surg Br. 2006;88(9):1164–1168. doi: 10.1302/0301-620X.88B9.18044. [DOI] [PubMed] [Google Scholar]
- 26.Berend KR, Lombardi AV., Jr Liberal indications for minimally invasive oxford unicondylar arthroplasty provide rapid functional recovery and pain relief. Surg Technol Int. 2007;16:193–197. [PubMed] [Google Scholar]
- 27.Baker P, Jameson S, Critchley R, Reed M, Gregg P, Deehan D. Center and surgeon volume influence the revision rate following unicondylar knee replacement: an analysis of 23,400 medial cemented unicondylar knee replacements. J Bone Joint Surg Am. 2013;95(8):702–709. doi: 10.2106/JBJS.L.00520. [DOI] [PubMed] [Google Scholar]