Abstract
Purpose
The locking compression extra-articular distal humerus plate (EADHP) is an anatomically shaped, angular stable single-column fixation system for distal third humerus fractures. The purpose of this retrospective study was to evaluate clinical and radiographic outcomes after open reduction and internal fixation of distal humerus fractures with this device.
Methods
Twenty-one consecutive patients with distal humerus fractures were treated with the EADHP system between February 2006 and June 2012. Of these, 19 were clinically and radiographically evaluated after a mean follow-up of 10.4 months. Follow-up assessment included anteroposterior and lateral radiographs, assessment of range of motion (ROM), pain according to a visual analogue scale (VAS) and Disabilities of the Arm, Shoulder and Hand (DASH) score.
Results
All fractures demonstrated satisfactory reduction and healing at an average of 7.3 months. One patient showed post-operative sensory ulnar neuropathy that recovered completely, and nine patients had a preoperative radial nerve palsy, which recovered spontaneously following exploration and plating. Mean post-operative ROM was as follows: flexion 126°, extension −7°, pronation 82° and supination 83°. The VAS score was zero points in eight patients, while the mean DASH score was 25.8 points.
Conclusions
For extra-articular distal humerus fractures, including high-energy injuries often seen in gunshot wounds or motor vehicle injuries, the anatomically shaped angular stable single-column plate provides satisfactory clinical and radiographic results and serves as a valuable tool in the treatment of these injuries.
Keywords: Humerus fracture, Articular fracture, Diaphyseal fracture, Elbow fracture, Anatomical plate, ORIF, Outcome, Clinical study, Outcome study, Results
Introduction
Fractures of the distal humerus are complex and challenging injuries to treat. Humeral shaft and extra-articular supracondylar humerus fractures in adults comprise 16 % of humeral shaft and 10 % of distal humerus fractures [1]. Most of these are either simple spiral diaphyseal fractures or are complicated by extension into the articular surface. The main goal of treatment of extra-articular distal humerus fractures is to restore alignment and achieve stable fixation to allow for early elbow range of motion (ROM), which is crucial for a good functional outcome [2, 3]. Treatment recommendations for this injury have been adopted primarily from studies of intra-articular distal humerus fractures. Many authors have advocated managing these fractures surgically with open reduction and internal fixation (ORIF) and immediate elbow motion [4, 5]. Double-plating techniques using two 3.5-mm plates in orthogonal (90–90) or parallel (180°) patterns are generally accepted. Standard single-plating techniques typically fail to achieve adequate stabilisation [6–8]. Yet despite good functional results, nonunions and infections do occur with double-plating techniques [8, 9]. To minimise extensive soft tissue stripping and to decrease surgical time, some authors have used a single posterolateral compression plate for fixation of non-comminuted extra-articular distal humerus fractures [5, 8, 10]. The advantages of a single plate would include decreased surgical exposure, decreased surgical time and potentially faster rehabilitation due to minimal iatrogenic soft tissue injury.
Laboratory studies of locking plate constructs have shown superior fixation compared to standard compression plates for tibial and femoral metaphyseal and diaphyseal fractures [11, 12]. In a biomechanical study, Korner et al. demonstrated that both two standard reconstruction plates and two pre-contoured locking plates provide adequate fixation in an extra-articular distal humerus model [7]. They showed, however, that the locking plate construct provided enhanced stiffness against anterior-posterior bending and torsional loads. Due to the superior biomechanics of locking plates, other peri-articular long bone fractures have been successfully treated with only one plate, including distal femur [13], proximal tibia [14], distal tibia [15] and distal radius [16] fractures.
The locking compression extra-articular distal humerus plate (EADHP, Synthes, Solothurn, Switzerland), also known as the “J-plate”, is an anatomically shaped, angular stable fixation system designed for extra-articular fractures of the distal humerus. The aim of this retrospective study was to evaluate the early clinical and radiographic results after open reduction and single-column fixation of fractures of the distal humerus with the EADHP system and compare these results with data from the literature. We hypothesised that the EADHP would enable adequate fracture fixation and satisfactory elbow function, even in elderly patients with potentially reduced bone mass.
Materials and methods
The implant
The EADHP is distally contoured for dorsal application on the lateral column of the distal humerus and has optimised angles within the distal screw holes and increased hole density at the distal portion. The proximal screw holes have a combination-hole system allowing for either locking or non-locking screws in the humeral shaft. Additionally, the plate has an angular offset, which allows it to contour to the posterolateral column, thereby avoiding impingement on the olecranon fossa.
Surgical technique
Surgery was performed with the patient in the prone or lateral position and under general anaesthesia. The injured arm was placed on a support allowing elbow flexion up to 120°. The modified posterior approach [17] to the distal humerus was used in all but one case, with identification of the radial and posterior brachial cutaneous nerves (Fig. 1). The ulnar nerve was identified and isolated in six cases. Reduction of the fracture was performed first and held with K-wires. Then, the EADHP was placed and fixed with 3.5-mm locking screws in the distal portion and 3.5-mm cortical screws in the proximal part. The plate was positioned so that its shaft portion was located centrally on the posterior aspect of the humerus while the distal end curved along the posterior aspect of the lateral column (Fig. 2). Care was taken not to impinge on the olecranon fossa and the plate was taken as far distally down the lateral column as necessary for stable fixation. The position and extent of the EADHP are demonstrated in Fig. 3.
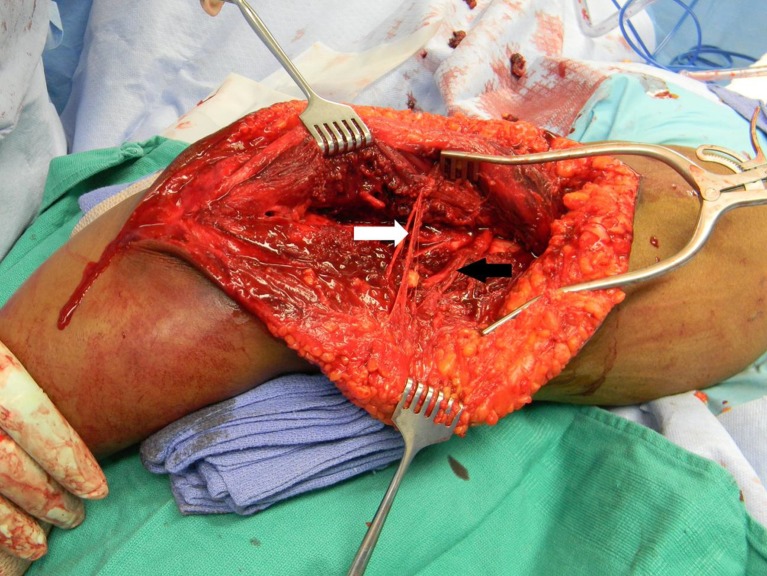
Fig. 1.
Intra-operative photograph of the posterolateral approach with identification of the posterior brachial cutaneous nerve (white arrow) and radial nerve (black arrow)
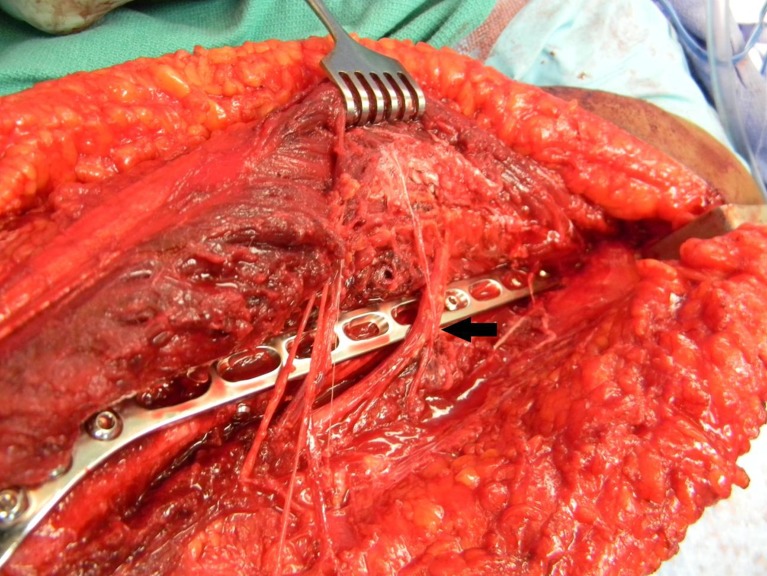
Fig. 2.
Intraoperative view of the EADHP system placed on the distal humerus. Note the radial nerve crossing the plate at the mid-shaft of the humerus (black arrow)
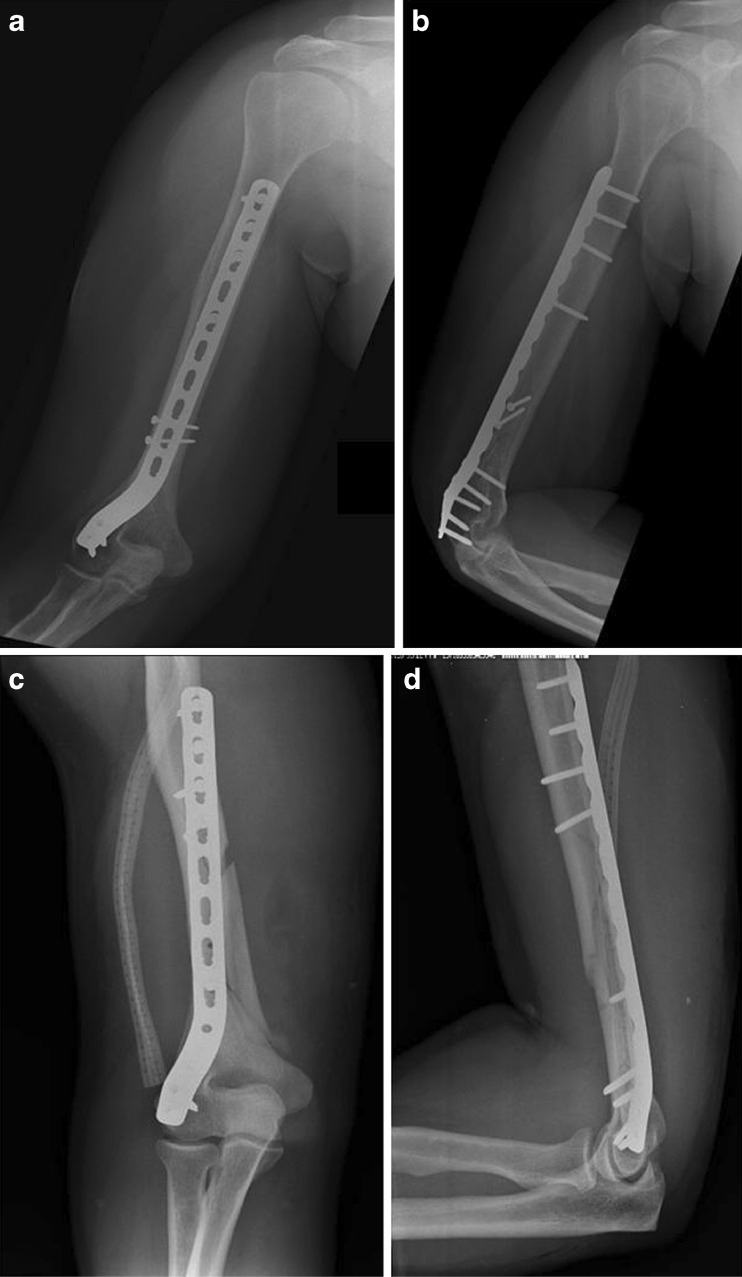
Fig. 3.
General position and extent of the EADHP implant. a Anteroposterior humerus. b Lateral humerus. c Anteroposterior elbow. d Lateral elbow radiographs. Note the proximal extension of the plate. The humerus and elbow radiographs are from two different cases
Patients
We treated 21 consecutive patients (12 men and nine women) with metaphyseal extra-articular distal humerus fractures or nonunions between February 2006 and June 2012 at our institution using the EADHP (Table 1). Inclusion criteria included skeletally mature patients with a closed or open fracture of the distal humerus (AO type A) with or without neurovascular deficits. Of these, 19 patients had adequate follow-up and were included in the final analysis. The average age of the patients at the time of operation was 39 years (range 19–91 years). Of the 21 patients with distal humerus fractures, eight were due to motor vehicle accidents (38 %), five were nonunions from previous distal humerus operations (24 %), four were due to falls (19 %), three were due to gunshot wounds (14 %) and one was due to a forklift injury (5 %). Sixteen patients (76 %) sustained additional injuries, while five patients (24 %) sustained isolated distal humerus fractures. Of the 16 patients with multi-trauma injuries, nine suffered radial nerve injuries (56 %), three sustained forearm fractures (19 %), three suffered non-upper extremity fractures (19 %), one sustained a median nerve injury (6 %), one injured their brachial artery (6 %) and one dislocated their elbow (6 %). The mean follow-up time was 10.4 months, ranging from three to 36 months.
Table 1.
Clinical series
| Patient no. | Age/sex | Mechanism of injury | Indication for operative treatment | Radiographic healing | Complications |
|---|---|---|---|---|---|
| 1 | 23/M | Forklift injury | Multiple trauma and radial shaft fracture | Yes | Rotational forearm contracture |
| 2 | 91/F | Fall | Open fracture, radial nerve deficit | Yes | None |
| 3 | 19/M | GSW | Open fracture and multiple trauma, arterial injury | Yes | Elbow stiffness, HO |
| 4 | 22/M | MVA | Multiple trauma and radial nerve deficit | Yes | None |
| 5 | 41/F | MVA | Multiple trauma | Yes | Symptomatic hardware requiring removal |
| 6 | 31/M | MVA | Nonunion | Yes | None |
| 7 | 72/F | MVA | Progressive fracture displacement | Yes | Transient ulnar nerve deficit |
| 8 | 23/M | GSW | Multiple trauma and median nerve deficit | Yes | None |
| 9 | 29/F | Fall | Fracture displacement and radial nerve deficit | Yes | None |
| 10 | 33/M | GSW | Open fracture | Yes | None |
| 11 | 47/M | Fall | Open fracture and radial nerve deficit | Yes | None |
| 12 | 41/F | MVA | Fracture displacement and radial nerve deficit | Yes | None |
| 13 | 21/M | Fall | Fracture displacement and radial nerve deficit | Yes | None |
| 14 | 48/F | MVA | Multiple trauma and radial nerve deficit | Yes | None |
| 15 | 50/M | MVA | Open fracture | Yes | Infection |
| 16 | 34/M | MVA | Fracture displacement and radial nerve deficit | Yes | None |
| 17 | 40/F | MVA | Nonunion | Yes | None |
| 18 | 29/F | GSW | Nonunion | Yes | None |
| 19 | 31/F | MVA | Nonunion, radial nerve deficit | Yes | None |
| 20 | 53/M | Wrestling injury | Nonunion | Yes | None |
| 21 | 47/M | Crush injury | Nonunion, hardware failure | Yes | HO |
M male, F female, GSW gunshot wound, MVA motor vehicle accident, HO heterotopic ossification
In order to assess post-operative clinical outcomes at the time of follow-up, a Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire was completed by each patient and the degree of pain was also recorded using a visual analogue scale (VAS). The VAS is a subjective scale used for measuring pain, and the pain level was indicated on a continuous scale extending from 0 to 10. Additionally, the elbow/forearm flexion, extension, supination and pronation ROM were determined for each patient. Radiographic parameters were also evaluated. Anteroposterior and lateral radiographs were obtained and used to determine the healing progress of the distal humerus fracture as well as plate location and stability. The metaphyseal-diaphyseal angle, humeral-ulnar angle and shaft-condylar angle were measured using these radiographs (Fig. 4). Lastly, the per cent of anterior capitellum was calculated using the anterior humeral line as a reference.
Fig. 4.
Anteroposterior and lateral radiographic angles of the elbow. a Metaphyseal-diaphyseal angle (α), humeral-ulnar angle (β). b Shaft-condylar angle (arrow), the anterior humeral line (A)
Results
Complete clinical and radiographic evaluations were performed at a minimum of three months post-operatively in 19 patients. The mean time to radiographic fracture healing was 7.3 months (range three to 13 months). ROM and DASH scores are presented in Table 2. At final follow-up, the mean flexion-extension arc was 120° (SD 20°) with a mean flexion of 126° (SD 16°) and a mean extension of 7° (SD 7°). The mean supination-pronation arc was 165° (SD 45°) with a mean supination of 83° (SD 22°) and a mean pronation of 82° (SD 23°). Additionally, the mean DASH score was 25.8 points (SD 17.7 points), ranging from 13.3 to 38.3 points. VAS scores are also presented in Table 2 (of note, the scores of only 14 patients were able to be obtained). At final follow-up, eight patients were completely pain free (47 %), three patients experienced mild pain (17 %) and three patients experienced moderate pain (17 %). No patients suffered severe pain. Furthermore, the final elbow radiographic outcomes are presented in Table 3. The mean metaphyseal-diaphyseal angle was 87.8° (SD 4.5°, normal 82–84°), the mean humeral-ulnar angle was 13.5° (SD 9.2°, normal 17.8° valgus), and the mean shaft-condylar angle was 41.1° (SD 2.7°, normal 40°). The anterior humeral line passed through 52.4 % (SD 18.3 %) of the capitellar width (normal, middle third).
Table 2.
Clinical patient outcomes
| Clinical outcomes | Mean ± SD | Degree of pain (VAS) | Number (%) |
|---|---|---|---|
| Elbow flexion | 126 ± 16° | None (0) | 8 (47) |
| Elbow extension | 7 ± 7° | Mild (1–3) | 3 (17) |
| Supination | 83 ± 22° | Moderate (4–6) | 3 (17) |
| Pronation | 82 ± 23° | Severe (7–10) | 0 (0) |
| DASH | 25.8 ± 17.7 |
DASH Disabilities of the Arm, Shoulder and Hand, VAS visual analogue scale
Table 3.
Radiographic outcomes data
| Radiographic outcomes | Mean ± SD |
|---|---|
| Metaphyseal-diaphyseal angle | 87.8 ± 4.5° |
| Humeral-ulnar angle | 13.5 ± 9.2° |
| Shaft-condylar angle | 41.1 ± 2.7° |
| Anterior line | 52.4 ± 18.3 % |
One 50-year-old male patient with an open fracture developed osteomyelitis, which was treated with debridement, antibiotics and retention of the hardware. The fracture went on to healing within 14 weeks. Additionally, one 19-year-old male patient had a laceration of the brachial artery in association with proximal radius and ulna fractures inflicted by a gunshot wound; in this case, successful revascularisation was achieved. Overall, nine patients had a preoperative radial nerve palsy, all of which recovered spontaneously. Furthermore, one patient developed post-operative ulnar neuropathy which spontaneously recovered. One patient developed elbow stiffness as well as heterotopic ossification as a result of concomitant proximal ulnar and radial fractures due to a gunshot wound. In addition, one patient required hardware removal due to symptomatic irritation.
Discussion
Distal humerus fractures remain one of the most challenging orthopaedic injuries to manage. They are commonly multi-fragmented, occur in osteopenic bone and have complex anatomy with limited options for internal fixation. Treatment outcomes are often associated with elbow stiffness, weakness and pain. A painless, stable and mobile elbow joint is desired as it allows the hand to conduct the activities of daily living, including personal hygiene and feeding. Our case series comprised type A fractures, which are extra-articular and typically occur at the distal humerus metaphyseal level. Although these fractures receive less attention in the literature than the more complex intra-articular type C fractures, they do account for one fourth of all distal humerus fractures [18].
Clinical studies using a single-column plate have demonstrated adequate fixation for extra-articular distal humerus fractures [3, 5, 10]. It appears that some degree of cortical contact is necessary to provide adequate stability to achieve sufficient fixation with a single plate. A recent biomechanical study has shown that a locking plate placed on the lateral column with no medial buttress to prevent varus deformity provided less resistance to varus stresses compared to double-plating [19]. This may be clinically relevant in situations with severe comminution as seen in gunshot injuries and in the absence of cortical contact between fragments. Despite these biomechanical data, our three (14 %) gunshot injury cases did not experience any secondary fracture displacement or hardware failure. This may be attributable to the relatively newer design of the EADHP which has increased thickness and width compared to previous plates used in the aforementioned biomechanical study. It is probable that the EADHP system, if tested, will show increased fixation rigidity over earlier designs.
This study evaluated clinical and radiographic outcomes after ORIF of extra-articular distal humerus fractures with a single lateral column plate. The results confirm our hypothesis that adequate fracture fixation and satisfactory functional outcome may be achieved with this device. All 19 of the reviewed charts documented radiographic healing with maintained reductions, adequate alignment and bridging callus. The mean elbow ROM was 7–126° at the last follow-up examination with no patients having a flexion contracture greater than 20°. Early physical therapy and ROM exercises were initiated immediately after splint removal in all of our cases to mitigate such contractures. The DASH score revealed a good subjective overall evaluation with a mean of 25.8 points, with 0 points as the best possible score result and 100 points as the worst possible score result. A DASH score in a normal arm has been shown to be 7–9 points [20]. This is comparable to the mean DASH scores found in modern series of distal humerus fractures that have been reported to range from 18.5 to 46.1 points, indicating mild to moderate residual impairment [21, 22].
With regard to neurologic injury, the nine patients who had a radial nerve palsy present pre-operatively had continuity of the nerve confirmed at surgery, and all regained radial nerve function by their last follow-up visit. In all cases, the radial nerve was explored and protected as part of the surgical approach. There were no cases of secondary radial nerve palsy. We had only one case (5 %) of post-operative ulnar neuropathy, an incidence which is lower than the numbers reported elsewhere in the literature [23]. The literature on this topic remains somewhat unclear, and the management of the ulnar nerve following ORIF of a distal humerus fracture in patients who had normal findings on a preoperative neurological examination remains an unresolved issue.
The treatment of distal humerus fractures is labour-intensive and complex, with an expected high incidence of complications [18]. Over one fourth (28 %) of our patients developed a complication after operative treatment, and one required further surgery (hardware removal). In our study, we treated five patients with nonunions of the distal humerus with the EADHP system. All five patients healed successfully. Furthermore, none of these five patients suffered from complications or infections. The mean flexion-extension arc for these patients was 121° and the mean supination-pronation arc was 170°. Two of these patients had no pain at all, one experienced mild pain and two experienced moderate pain. Wenzl et al. found that using the limited contact dynamic compression plate (LC-DCP) for internal fixation with locking screws demonstrated high consolidation rates [24]. Given our high consolidation rates as well as high functional outcomes and low complication rates, we feel that the EADHP is a reliable implant for the treatment of distal humerus fractures and humeral shaft nonunions.
According to our radiographic outcomes, the mean metaphyseal-diaphyseal angle, the mean humeral-ulnar angle and the mean shaft-condylar angle were all within the normal range. Additionally, more than half of the anterior capitellum was anterior to the anterior line, which is within the normal range. These radiographic outcomes demonstrate that the EADHP system is successful in maintaining elbow joint alignment and bone reduction over the long term. Furthermore, although not directly measured in our study, single-column fixation is reported to be less time-consuming than both-column fixation in either orthogonal or parallel mode [25]. A decreased surgical time often indirectly results in less bleeding, and less surgical dissection and manipulation of soft tissues. The absence of an olecranon osteotomy also improves the post-operative therapy course and facilitates early ROM. Consequently, these factors serve as potential additional benefits of using the EADHP system.
The limitations of this study include the relatively small sample size and the fact that two patients were lost to follow-up. Furthermore, in this study, the majority of patients had relatively high-energy trauma compared with other clinical trials. This may limit comparability of our data with studies dealing with low-energy trauma in the elderly. In addition, only one type of plating was tested, so no direct comparison may be made with other plating systems or techniques such as parallel plating.
Summary
For extra-articular distal humerus fractures, including high-energy injuries often seen in gunshot wounds or motor vehicle injuries, the use of an anatomically shaped angular stable single-column plate results in satisfactory clinical and radiographic results. We did not see any cases of loss of reduction or nonunion, and the relatively high rate of transient radial nerve deficit that occurred at injury was more related to the severity of the fracture than to the mode of fixation. Future research should aim to directly compare the EADHP to other extant fixation systems with regard to patient outcomes.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
Contributor Information
John T. Capo, Phone: +1-212-5986000, FAX: +1-212-5987654, Email: John.Capo@nyumc.org
Monika P. Debkowska, Phone: +1-973-9724783, Email: debkowmp@njms.rutgers.edu
Frank Liporace, Phone: +1-212-5986000, Email: Frank.Liporace@nyumc.org.
Bryan G. Beutel, Phone: +1-212-5986000, Email: bryanbeutel@gmail.com
Eitan Melamed, Phone: +1-212-5986000, Email: Eitan.Melamed@nyumc.org.
References
- 1.Ekholm R, Adami J, Tidermark J, Hansson K, Törnkvist H, Ponzer S. Fractures of the shaft of the humerus. An epidemiological study of 401 fractures. J Bone Joint Surg Br. 2006;88(11):1469–1473. doi: 10.1302/0301-620X.88B11.17634. [DOI] [PubMed] [Google Scholar]
- 2.Self J, Viegas SF, Buford WL, Jr, Patterson RM. A comparison of double-plate fixation methods for complex distal humerus fractures. J Shoulder Elbow Surg. 1995;4(1 Pt 1):10–16. doi: 10.1016/S1058-2746(10)80002-3. [DOI] [PubMed] [Google Scholar]
- 3.Waddell JP, Hatch J, Richards R. Supracondylar fractures of the humerus–results of surgical treatment. J Trauma. 1988;28(12):1615–1621. doi: 10.1097/00005373-198812000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Korner J, Lill H, Müller LP, Hessmann M, Kopf K, Goldhahn J, Gonschorek O, Josten C, Rommens PM. Distal humerus fractures in elderly patients: results after open reduction and internal fixation. Osteoporos Int. 2005;16(Suppl 2):S73–S79. doi: 10.1007/s00198-004-1764-5. [DOI] [PubMed] [Google Scholar]
- 5.Levy JC, Kalandiak SP, Hutson JJ, Zych G. An alternative method of osteosynthesis for distal humeral shaft fractures. J Orthop Trauma. 2005;19(1):43–47. doi: 10.1097/00005131-200501000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Schwartz A, Oka R, Odell T, Mahar A. Biomechanical comparison of two different periarticular plating systems for stabilization of complex distal humerus fractures. Clin Biomech (Bristol, Avon) 2006;21(9):950–955. doi: 10.1016/j.clinbiomech.2006.04.018. [DOI] [PubMed] [Google Scholar]
- 7.Korner J, Diederichs G, Arzdorf M, Lill H, Josten C, Schneider E, Linke B. A biomechanical evaluation of methods of distal humerus fracture fixation using locking compression plates versus conventional reconstruction plates. J Orthop Trauma. 2004;18(5):286–293. doi: 10.1097/00005131-200405000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Jawa A, McCarty P, Doornberg J, Harris M, Ring D. Extra-articular distal-third diaphyseal fractures of the humerus. A comparison of functional bracing and plate fixation. J Bone Joint Surg Am. 2006;88(11):2343–2347. doi: 10.2106/JBJS.F.00334. [DOI] [PubMed] [Google Scholar]
- 9.Paris H, Tropiano P, Clouet D'orval B, Chaudet H, Poitout DG. Fractures of the shaft of the humerus: systematic plate fixation. Anatomic and functional results in 156 cases and a review of the literature. Rev Chir Orthop Reparatrice Appar Mot. 2000;86(4):346–359. [PubMed] [Google Scholar]
- 10.Moran MC (1997) Modified lateral approach to the distal humerus for internal fixation. Clin Orthop Relat Res 340:190–197 [DOI] [PubMed]
- 11.Egol KA, Su E, Tejwani NC, Sims SH, Kummer FJ, Koval KJ. Treatment of complex tibial plateau fractures using the less invasive stabilization system plate: clinical experience and a laboratory comparison with double plating. J Trauma. 2004;57(2):340–346. doi: 10.1097/01.TA.0000112326.09272.13. [DOI] [PubMed] [Google Scholar]
- 12.Fulkerson E, Egol KA, Kubiak EN, Liporace F, Kummer FJ, Koval KJ. Fixation of diaphyseal fractures with a segmental defect: a biomechanical comparison of locked and conventional plating techniques. J Trauma. 2006;60(4):830–835. doi: 10.1097/01.ta.0000195462.53525.0c. [DOI] [PubMed] [Google Scholar]
- 13.Kregor PJ, Stannard JA, Zlowodzki M, Cole PA. Treatment of distal femur fractures using the less invasive stabilization system: surgical experience and early clinical results in 103 fractures. J Orthop Trauma. 2004;18(8):509–520. doi: 10.1097/00005131-200409000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Cole PA, Zlowodzki M, Kregor PJ. Treatment of proximal tibia fractures using the less invasive stabilization system: surgical experience and early clinical results in 77 fractures. J Orthop Trauma. 2004;18(8):528–535. doi: 10.1097/00005131-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Bedi A, Le TT, Karunakar MA. Surgical treatment of nonarticular distal tibia fractures. J Am Acad Orthop Surg. 2006;14(7):406–416. doi: 10.5435/00124635-200607000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Liporace FA, Kubiak EN, Jeong GK, Iesaka K, Egol KA, Koval KJ. A biomechanical comparison of two volar locked plates in a dorsally unstable distal radius fracture model. J Trauma. 2006;61(3):668–672. doi: 10.1097/01.ta.0000234727.51894.7d. [DOI] [PubMed] [Google Scholar]
- 17.Gerwin M, Hotchkiss RN, Weiland AJ. Alternative operative exposures of the posterior aspect of the humeral diaphysis with reference to the radial nerve. J Bone Joint Surg Am. 1996;78(11):1690–1695. doi: 10.2106/00004623-199611000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Robinson CM, Hill RM, Jacobs N, Dall G, Court-Brown CM. Adult distal humeral metaphyseal fractures: epidemiology and results of treatment. J Orthop Trauma. 2003;17(1):38–47. doi: 10.1097/00005131-200301000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Tejwani NC, Murthy A, Park J, McLaurin TM, Egol KA, Kummer FJ. Fixation of extra-articular distal humerus fractures using one locking plate versus two reconstruction plates: a laboratory study. J Trauma. 2009;66(3):795–799. doi: 10.1097/TA.0b013e318181e53c. [DOI] [PubMed] [Google Scholar]
- 20.Nauth A, McKee MD, Ristevski B, Hall J, Schemitsch EH. Distal humeral fractures in adults. J Bone Joint Surg Am. 2011;93(7):686–700. doi: 10.2106/JBJS.J.00845. [DOI] [PubMed] [Google Scholar]
- 21.Theivendran K, Duggan PJ, Deshmukh SC. Surgical treatment of complex distal humeral fractures: functional outcome after internal fixation using precontoured anatomic plates. J Shoulder Elbow Surg. 2010;19(4):524–532. doi: 10.1016/j.jse.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 22.Greiner S, Haas NP, Bail HJ. Outcome after open reduction and angular stable internal fixation for supra-intercondylar fractures of the distal humerus: preliminary results with the LCP distal humerus system. Arch Orthop Trauma Surg. 2008;128(7):723–729. doi: 10.1007/s00402-007-0428-2. [DOI] [PubMed] [Google Scholar]
- 23.Vazquez O, Rutgers M, Ring DC, Walsh M, Egol KA. Fate of the ulnar nerve after operative fixation of distal humerus fractures. J Orthop Trauma. 2010;24(7):395–399. doi: 10.1097/BOT.0b013e3181e3e273. [DOI] [PubMed] [Google Scholar]
- 24.Wenzl ME, Porté T, Fuchs S, Faschingbauer M, Jürgens C. Delayed and non-union of the humeral diaphysis–compression plate or internal plate fixator? Injury. 2004;35(1):55–60. doi: 10.1016/S0020-1383(02)00381-9. [DOI] [PubMed] [Google Scholar]
- 25.Aggarwal S, Kumar V, Bhagwat KR, Behera P. AO extra-articular distal humerus locking plate: extended spectrum of usage in intra-articular distal fractures with metaphyseal extension-our experience with 20 cases. Eur J Orthop Surg Traumatol. 2013 doi: 10.1007/s00590-013-1217-y. [DOI] [PubMed] [Google Scholar]