Abstract
Purpose
The purposes of the present study were (1) to investigate the variation and accuracy of both acetabular and femoral component version on the axial computed tomographic (CT) images, and (2) to better define the associations between the components version and clinical factors.
Methods
We investigated acetabular and femoral component orientation in 1,411 primary total hip arthroplasties that had been performed without computer-assisted navigation. Version of the acetabular and femoral components was measured on the axial CT images.
Results
The component version was significantly greater than the native version in both acetabular and femoral version. There was a significant correlation between the stem and native femoral versions, but not between the acetabular component and native acetabular versions.
Conclusion
This study identifies several features that might help analyse the effect of pre-operative native acetabular and femoral version on the variation of component alignment.
Keywords: Total hip arthroplasty, Component, Computed tomography, Version
Introduction
Accurate placement of the acetabular and femoral components during total hip arthroplasty (THA) is critical to ensure a successful outcome [1, 2]. To avoid complications, the components should be implanted in a defined safe range, but great variations have been reported for the components’ orientation [3–7]. Optimal position has been studied by many authors, and the combined version of the components is important to avoid impingement and/or dislocation [2, 8, 9]. However, there is little published information based on actual measurements of component alignment in THA, and only one study has compared the component version angles with the native version angles [8].
The purposes of the present study were to (1) investigate the variation and accuracy of version of both acetabular and femoral components implanted using a manual technique, and (2) to better define the associations between the components version and clinical factors (gender, laterality).
Materials and methods
As part of a retrospective study intended to help determine associations between hip dislocation after THA and component version (results reported separately), we reviewed radiographs and CT scans of 1,529 consecutive primary total hip arthroplasties implanted using a manual technique. One hundred eighteen hips with the straight S-ROM femoral prosthesis (DePuy Orthopedics, Warsaw, IN) and/or with cemented cup were excluded from this part of the study. The remaining 1,411 hips in 1,294 patients were included in the study. There were 213 males and 1,081 females. The mean age at the time of surgery was 62.6 years (range, 25–91 years) at time of operation. Seven hundred sixty one (54.6 %) THAs were placed in the patients’ right hip and 650 (45.4 %) in the left. The diagnoses for THA included osteoarthritis (1,296 hips), osteonecrosis (70 hips), rheumatoid arthritis (18 hips), dislocated hips (21 hips), and posttraumatic arthritis (six hips). Patients were classified as type I (1,221 hips), type II (150 hips), type III (30 hips) and type IV (ten hips) according to the Crowe classification.
All THAs were implanted under general anaesthesia with the patient in the lateral position using a posterolateral approach. We fixed the pelvis with two normal positioners held on the pubic symphysis and sacrum. The surgeons always stood on the patient’s right side at the insertion of acetabular component, and inserted the femoral stem from the patient’s posterior side. We attempted to place the acetabular components in an anatomic position and determined the anteversion of the acetabular component by considering the direction of the transverse ligament and anatomic features of the acetabulum fossa. We used alignment guides provided by the implant manufacturer for 45° vertical tilt and 20° anteversion of acetabular component orientation, but no other special instruments such as navigation systems were used. In all patients we used press-fit cup components and straight (0° anteversion) stems. We inserted the stem in the most stable position possible provided by the individual anatomy. Stem position was obtained with the knee flexed 90° and the leg as the reference for anteversion. No special attempt was made to achieve a particular stem anteversion.
Anatomic native anteversion of the acetabulum and femur were measured in a supine position on the axial CT images taken preoperatively. Each patient underwent a pelvic CT examination one week after surgery, and version angles of the acetabular and femoral components were measured. We defined acetabular component version as the angle between a line connecting the lateral anterior and posterior margins of the acetabular component and the sagittal plane defined as the plane perpendicular to a line connecting two identical points on either side of the pelvis (Fig. 1a) [9]. Femoral component version was calculated as the angle between a line from the centre of the femoral head to the centre of the neck of femoral prosthesis, and a line connecting the posterior aspect of the medial and lateral femoral condyles, respectively (Fig. 1b).
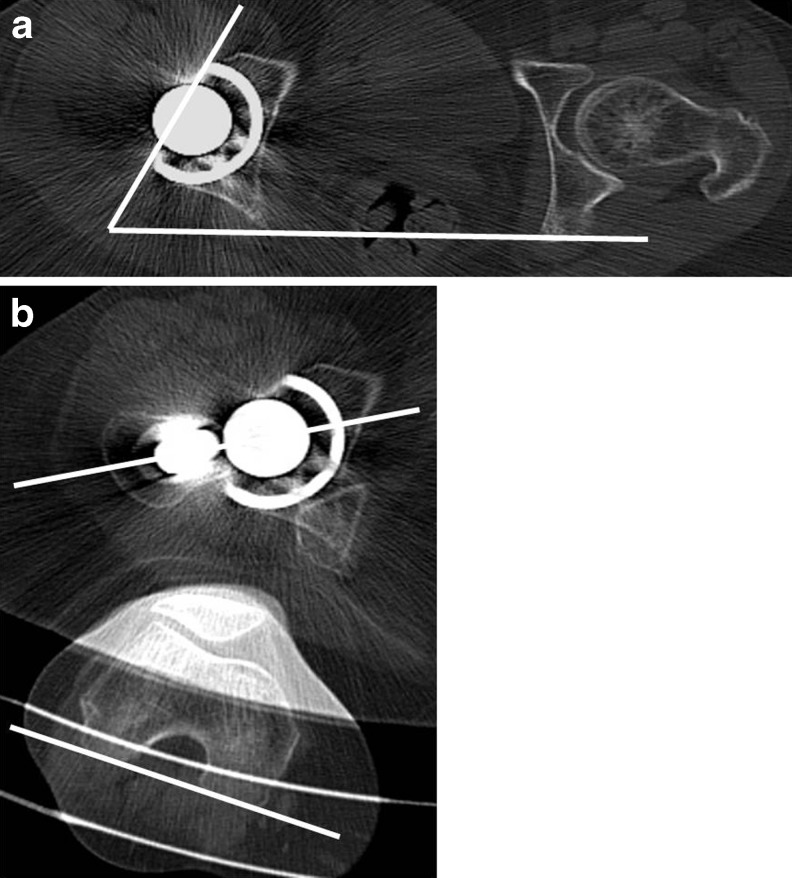
Fig. 1.
CT allows accurate measurement of prosthetic version. a Acetabular component version defined as the angle between a line connecting the lateral anterior and posterior margins of the acetabular component and the sagittal plane defined as the plane perpendicular to a line connecting two identical points on either side of the pelvis. b Femoral component version calculated as the angle between a line from the head of the femoral prosthesis to the centre of the proximal femoral diaphysis and a line connecting the posterior aspect of the medial and lateral femoral condyles
Inclination of the acetabular component was measured using anteroposterior pelvic radiographs in the supine position. The degree of abduction of the acetabular component was measured with respect to a horizontal line through the bottom edge of the teardrops as recommended by Sutherland et al. [10]. A single investigator (TF) performed all of the measurements in order to minimize inter-observer variability.
Statistical analysis
The Kruskal-Wallis and post-hoc Scheffe statistical tests were used to compare acetabular, femoral and combined component version among each subdivided three groups described in detail subsequently. The Mann–Whitney test was used to compare acetabular, femoral and combined component version to the native version. The Mann–Whitney test was also used to compare the mean cup inclination between the right and the left hips, and acetabular, femoral and combined between the male patients and the females. The correlation between the acetabular, femoral and combined component versions and native versions were evaluated using Pearson’s correlation coefficient test. P values below 0.05 were regarded as statistically significant.
Results
Acetabular version
The native acetabular version as measured from the pre-op CT scans ranged from 24.0° of retroversion to 56.7° of anteversion with a mean of 20.2° ± 6.1°. The acetabular anteversion was less than 10° in 54 (3.8 %) hips, 10°–20° in 625 (44.3 %) hips, 20°–30° in 653 (46.3 %) hips, and greater than 30° in 79 (5.6 %) hips.
The acetabular component version angles ranged from 22.7° of retroversion to 56.6° of anteversion with a mean of 24.7° ± 11.3°. The anteversion was less than 10° in 135 (9.6 %) cups, 10°–20° in 271 (19.2 %) cups, 20°–30° in 553 (39.2 %) cups, 30°–40° in 367 (26.0 %) cups, and greater than 40° in 85 (6.0 %) cups. The acetabular component version was significantly greater than the native version (P < 0.0001). However, there was no correlation between the acetabular component and native acetabular versions (r = 0.119, p < 0.0001).
The acetabular discrepancy was defined as the absolute value of the difference between the acetabular component version and native acetabular version in each patient. The acetabular discrepancy was less than –10° in 148 (10.5 %) hips, –10° to 0° in 296 (21.0 %) hips, 0°–10° in 499 (35.4 %) hips, 10°–20° in 344 (24.4 %) hips, and greater than 20° in 124 (8.8 %) hips.
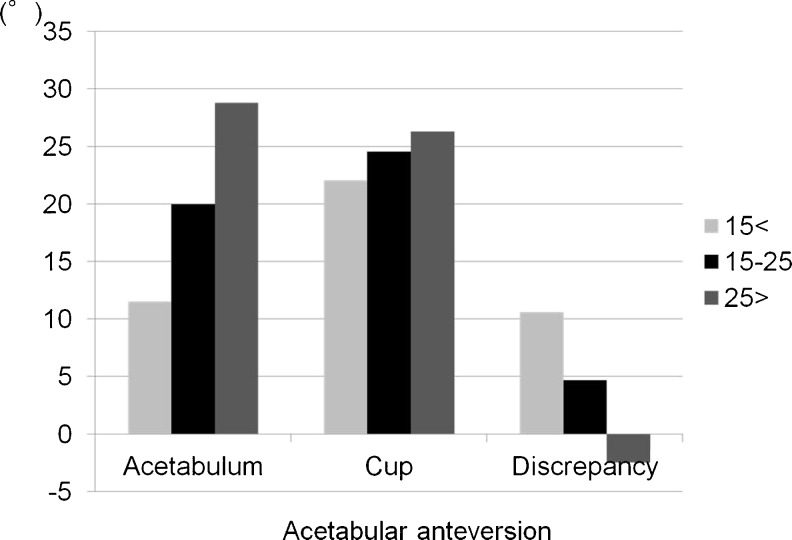
The 1,411 hips were subdivided into three groups: less than 15° native acetabular anteversion (250 hips), 15°–25° acetabular anteversion (878 hips), and more than 25° acetabular anteversion (283 hips) (Fig. 2). Acetabular anteversion angles of each group were 11.5° ± 4.0°, 19.9° ± 2.8°, and 28.6° ± 3.6°, respectively (Fig. 2). There were significant differences among each group. Acetabular implant anteversion angles of each group were 22.4° ± 12.3°, 24.9° ± 11.1°, and 26.2° ± 10.8°, respectively (Fig. 2). Acetabular implant anteversion in the group with less than 15° native acetabular anteversion was significantly smaller than in the other two groups. The acetabular discrepancy of each group was 10.8° ± 12.7°, 4.9° ± 11.3°, and –2.4° ± 11.3°, respectively (Fig. 2). There were significant differences among each group.
Fig. 2.
Results of acetabular version among three groups: those with less than 15° native acetabular anteversion, those with 15°–25°anteversion, and those with more than 25° anteversion
Femoral version
The native femoral version as measured from the pre-op CT scans ranged from 13.4° of retroversion to 80.0° of anteversion with a mean of 31.0° ± 12.6°. The femoral anteversion was less than 10° in 55 (3.9 %) hips, 10°–20° in 230 (16.3 %) hips, 20°–30° in 368 (26.1 %) hips, 30°–40° in 471 (33.4 %) hips, 40°–50° in 248 (17.6 %) hips, and greater than 50° in 93 (6.6 %) hips.
The femoral component version as measured from the CT scan ranged from 0.2° to 72.0° of anteversion with a mean of 40.3° ± 11.3°. The anteversion was less than 20° in 57 (4.0 %) stems, 20°–30° in 177 (12.5 %) stems, 30°–40° in 428 (30.3 %) stems, 40°–50° in 491 (34.8 %) stems, and greater than 50° in 258 (18.3 %) stems. The component version was significantly greater than the native femoral version (p < 0.0001). Moreover, there was correlation between the stem and native femoral versions (r = 0.487, p < 0.0001).
The femoral discrepancy was defined as the absolute value of the difference between the femoral component version and native femoral version from the CT radiographs. The femoral discrepancy was less than –10° in 71 (5.0 %) hips, –10° to 0° in 216 (15.3 %) hips, 0°–10° in 456 (32.3 %) hips 10°–20° in 392 (27.8 %) hips, and greater than 20° in 276 (19.6 %) hips.
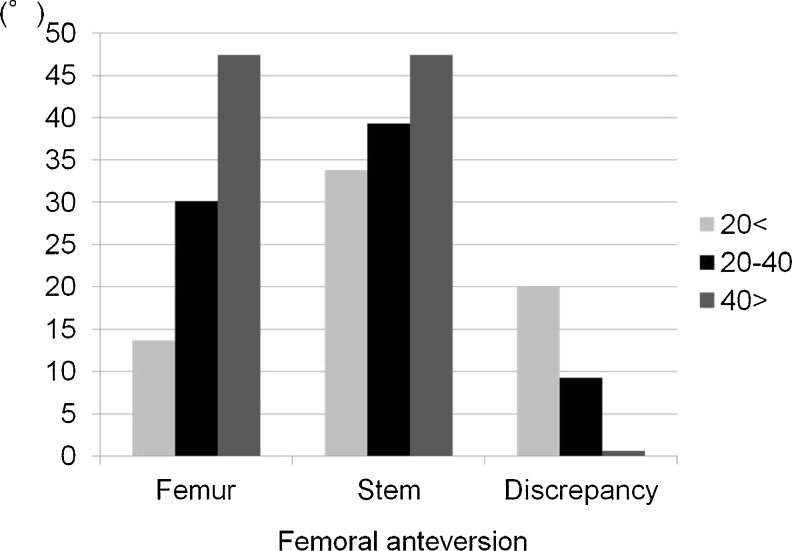
The 1,411 hips were subdivided into three groups: those with less than 20° femoral anteversion (285 hips), those with 20°–40° femoral anteversion (785 hips), and those with more than 40° femoral anteversion (341 hips) (Fig. 3). Femoral anteversion angles of each group were 13.8° ± 5.1°, 30.1° ± 5.5°, and 47.4° ± 6.8°, respectively (Fig. 3). There were significant differences among each group. Femoral implant anteversion angles of each group were 33.8° ± 10.0°, 39.3° ± 10.4°, and 48.0° ± 10.2°, respectively (Fig. 3). There were significant differences among each group. The femoral discrepancy of each group was 20.0° ± 9.9°, 9.2° ± 10.3°, and 0.60° ± 10.6°, respectively (Fig. 3). There were significant differences among each group.
Fig. 3.
Results of femoral version among three groups: those with less than 20° native femoral anteversion, those with 20°–40° anteversion, and those with more than 40° anteversion
Combined version
The native combined version ranged from 22.0° of retroversion to 105.0° of anteversion with a mean of 51.2° ± 15.0°. The anteversion was less than 30° in 90 (6.3 %) hips, 30°–40° in 235 (16.7 %) hips, 40°–50° in 326 (23.1 %) hips, 50°–60° in 360 (25.5 %) hips, 60° to 70° in 234 (16.6 %) hips, and greater than 70° in 157 (11.1 %) hips.
The combined version of the components ranged from 12.9 to 112° of anteversion with a mean of 65.0° ± 15.7°. The anteversion was less than 40° in 98 (6.9 %) hips, 40°–50° in 120 (8.5 %) hips, 50°–60° in 271 (19.2 %) hips, 60°–70° in 375 (26.6 %) hips, 70°–80° in 322 (22.8 %) hips, and greater than 80° in 225 (15.9 %) hips.
The combined version discrepancy was defined as the absolute value of the difference between the acetabular and femoral component's orientation and native combined version orientation from the CT radiographs. The combined version discrepancy was less than –10° in 135 (9.6 %) hips, –10° to 0° in 155 (11.0 %) hips, 0°–10° in 279 (19.8 %) hips, 10°–20° in 328 (23.2 %) hips, 20°–30° in 248 (17.6 %) hips, 30°–40° in 162 (11.5 %) hips, and greater than 40° in 104 (7.4 %) hips (Fig. 4).
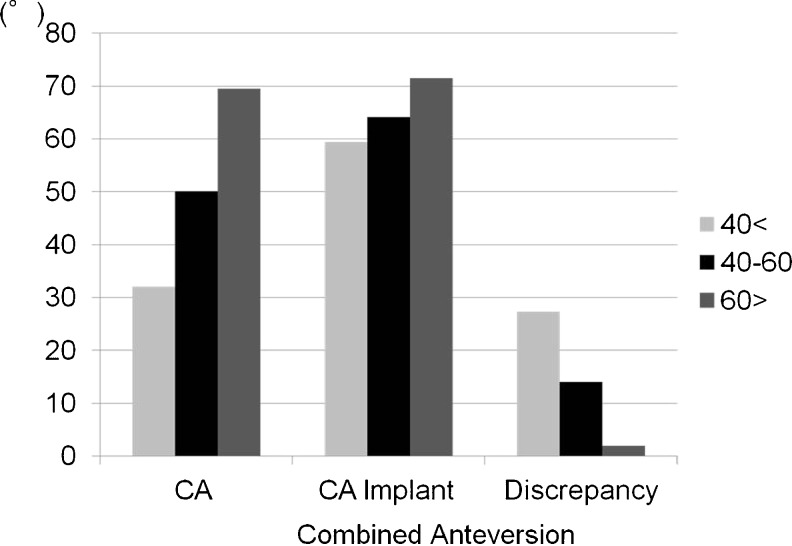
Fig. 4.
Results of combined version among three groups: those with less than 40° native combined anteversion, those with 40°–60° anteversion, and those with more than 60° anteversion
The 1,411 hips were subdivided into three groups: those with less than 40° combined anteversion (334 hips), those with 40°–60° combined anteversion (686 hips), and those with more than 60° combined anteversion (391 hips) (Fig. 4). The combined anteversion angles of each group were 32.1° ± 7.2°, 50.1° ± 15.4°, and 69.5° ± 7.8°, respectively (Fig. 4). There were significant differences among each group (p < 0.0001). Combined implant anteversion angles of each group were 59.4° ± 15.2°, 64.1° ± 15.4°, and 71.5° ± 14.4°, respectively (Fig. 4). There were significant differences among each group (p < 0.0001). Combined version discrepancy of each group was 27.3° ± 15.7°, 14.0° ± 15.9°, and 2.0° ± 15.2°, respectively (Fig. 4). There were significant differences among each group (p < 0.0001).
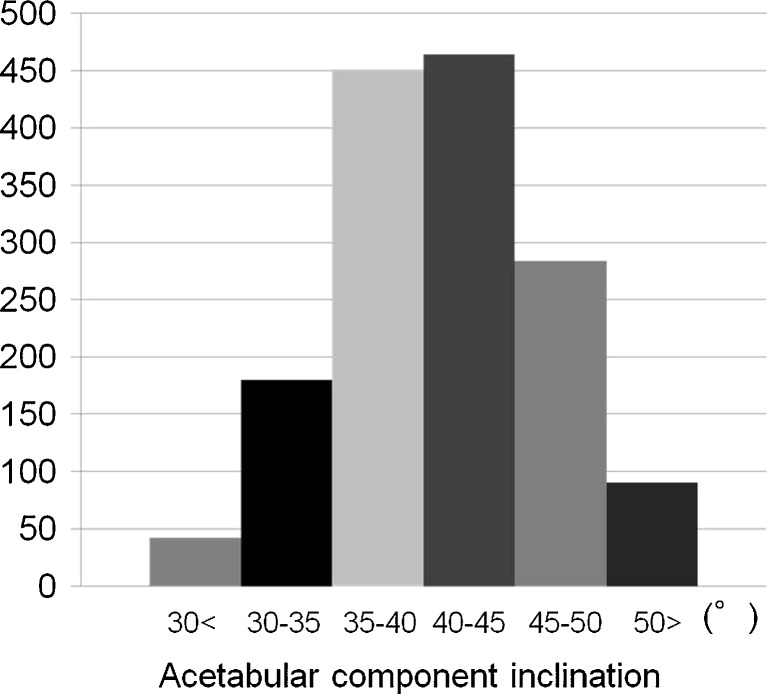
Inclination of the acetabular component
Inclination of the acetabular components was 41.0° ± 6.2° (mean ± standard deviation). The inclination of the acetabular components was less than 30° in 42 (3.0 %) hips, 30°–35° in 180 (12.8 %) hips, 35°–40° in 451 (32.0 %) hips, 40°–45° in 467 (33.1 %) hips, 45°–50° in 284 (20.1 %) hips, and greater than 50° in 90 (6.4 %) hips (Fig. 5). The mean cup inclination in the right hips (42.7° ± 6.0°) was significantly greater than in the left hips (39.6° ± 5.7°) (p < 0.0001).
Fig. 5.
Distribution of acetabular component inclination
Relationship between gender and acetabular and femoral version
The native acetabular version was less in male patients (16.5° ± 5.3°) compared to females (20.9° ± 6.0°) (p < 0.0001), and the version of the acetabular component was less in male patients (21.8° ± 11.9°) compared to females (25.2° ± 11.1°) (p < 0.0001). There were no significant differences between the male patients (5.3° ± 12.4°) and the female patients (4.4° ± 12.2°) in the acetabular discrepancy according to gender (p = 0.289).
The native femoral version was less in male patients (25.5° ± 11.3°) compared to the females (32.0° ± 12.6°) (p < 0.0001), and the version of the femoral component was less in male patients (36.8° ± 11.5°) compared to females (41.0° ± 11.2°) (p < 0.0001). The femoral discrepancy was greater in the male patients (11.2° ± 12.1°) than in the females (9.0° ± 12.1°) (p = 0.011).
The native combined version was less in the male patients (42.0° ± 13.2°) compared to the females (52.9° ± 14.8°) (p < 0.0001). The combined version of the components was less in the male patients (58.5° ± 16.8°) compared to the females (66.2° ± 15.2°) (p < 0.0001). The combined version discrepancy was greater in the male patients (16.6° ± 18.5°) than in the females (13.4° ± 18.0°) (p = 0.016).
Discussion
Accurate placement of the femoral and acetabular components during THA can reduce mechanical wear and the risk of dislocation [2]. Navigation systems were developed to improve accuracy and minimize variations in component orientation during THA [2, 11, 12]; however, navigation systems are expensive and require learning curves and extra surgical time. Therefore, we investigated the variation and accuracy of acetabular and femoral components that had been inserted without the use of computer-assisted navigation. We also analysed the effect of pre-operative native acetabular and femoral version on the variation of component orientation.
Our measurements of native acetabular anteversion (20.2° ± 6.1°) are similar to those of other studies (23° ± 6° by Stem et al. [13] and 20° ± 9° by Sugano et al. [14]).
Reikerås et al. [8] reported that 58.2 % of the acetabular components were within the target zone of 10°–30° version. We found 824 of 1,411 (58.4 %) of the acetabular components were within the target zone. Other studies reported a variable range (20°– 72.2 %) of acetabular component orientation being within the safe zone of Lewinneck (5°–25° anteversion and 30°–50° inclination in radiographic measurements) with manual techniques. Although our measurements of acetabular component were anatomical measurement for version, and our results strictly are not comparable to other results of study about the safe zone of Lewinneck, 564 of 1,411 hips (40.0 %) in our study were within the safe range.
We found more than 90 % of acetabular components were oriented inside the presumed safe range for inclination (30°–50°). The mean cup abduction in the right hips was significantly greater than in the left hips. Minoda et al. [15] noted a reduced likelihood of achieving implant position inside the safe range for hip implants inserted on the right side. The authors concluded that when gripping the holder of the acetabular component for right THA, the surgeon stretched across the patient to achieve the appropriate anteversion. This posture could disturb the sense of orientation in the right THA.
In our series, 57.6 % of native femoral anteversion was greater than 30°, and our anteversion was greater than reported by others [5, 8]. This could reflect the relatively high proportion of osteoarthritis secondary to developmental dysplasia of the hip in Japan compared to other countries [16]. In THA the anteversion of the femoral component tends to be dictated by the shape of the proximal femur. We also tended to decrease the anteversion of the stems in the greater native acetabular version, the theoretical risk of anterior dislocation with excessively anteverted stem could explain this observation. Therefore, there could be a discrepancy between the anteversion of the femoral component and the native anteversion of the femoral neck.
In the present series, we tended to increase the combined version in the smaller native combined version. Wines et al. [9] reported that femoral and acetabular anteversion was overestimated with a posterior as compared to a lateral approach, and suggested this was due to the theoretical risk of posterior dislocation with a posterior approach.
Reikerås et al. [8] reported both the native acetabular and femoral versions were less in the male patients as compared to the females but there was no significant differences in the versions between males and females. They showed that both acetabular component and combined versions were less in the male patients as compared to the females. While we found that both native acetabular and femoral versions were significantly less in males than in females, both acetabular and femoral components version were significantly less in males compared to the females. Our findings suggest that a tendency to follow the native anatomy can explain both the higher acetabular and femoral components anteversion in females than in males.
There are certain limitations to the present study. First, our measurements of both acetabular and femoral components were anatomical measurement for version, so our results are not comparable to other studies about the safe zone of Lewinneck. We believe the measurements using CT have great advantages of accurate measurements for version of the components. Second, CT-scan studies of component positioning should be interpreted with caution because there are variations of the pelvic and femur orientation depending on patient positioning. The position of the cup can be assessed in relation to the entire pelvis, giving information about pelvic tilt. Further study about measurements for version of the components using 3D template software is needed. Finally, this study does not show the associations between hip dislocation after THA and the components version; thus, we will report separately the associations in the future.
In summary, the component version was significantly greater than the native version in both acetabular and femoral version angles. There was a correlation between the stem and native femoral versions, but not between the acetabular component and native acetabular versions. The present study identifies several features that might help analyse the effect of preoperative native acetabular and femoral version on the variation of component alignment.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip replacement arthroplasties. J Bone Joint Surg Am. 1978;60(2):217–220. [PubMed] [Google Scholar]
- 2.Sugano N, Takao M, Sakai T, Nishii T, Miki H. Does CT-based navigation improve the long-term survival in ceramic-on-ceramic THA? Clin Orthop Relat Res. 2012;470(11):3054–3059. doi: 10.1007/s11999-012-2378-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bosker BH, Verheyen CC, Horstmann WG, Tulp NJ. Poor accuracy of freehand cup positioning during total hip arthroplasty. Arch Orthop Trauma Surg. 2007;127(5):375–379. doi: 10.1007/s00402-007-0294-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dorr LD, Wan Z, Malik A, Zhu J, Dastane M, Deshmane P. A comparison of surgeon estimation and computed tomographic measurement of femoral component anteversion in cementless total hip arthroplasty. J Bone Joint Surg Am. 2009;91(11):2598–2604. doi: 10.2106/JBJS.H.01225. [DOI] [PubMed] [Google Scholar]
- 5.Emerson RH., Jr Increased anteversion of press-fit femoral stems compared with anatomic femur. Clin Orthop Relat Res. 2012;470(2):477–481. doi: 10.1007/s11999-011-1993-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saxler G, Marx A, Vandevelde D, Langlotz U, Tannast M, Wiese M, Michaelis U, Kemper G, Grützner PA, Steffen R, von Knoch M, Holland-Letz T, Bernsmann K. The accuracy of free-hand cup positioning-a CT based measurement of cup placement in 105 total hip arthroplasties. Int Orthop. 2004;28(4):198–201. doi: 10.1007/s00264-004-0542-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sendtner E, Tibor S, Winkler R, Wörner M, Grifka J, Renkawitz T. Stem torsion in total hip replacement. Acta Orthop. 2010;81(5):579–582. doi: 10.3109/17453674.2010.524596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reikerås O, Gunderson RB. Components anteversion in primary cementless THA using straight stem and hemispherical cup: A prospective study in 91 hips using CT-scan measurements. Orthop Traumatol Surg Res. 2011;97(6):615–621. doi: 10.1016/j.otsr.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 9.Wines AP, McNicol D. Computed tomography measurement of the accuracy of component version in total hip arthroplasty. J Arthroplasty. 2006;21(5):696–701. doi: 10.1016/j.arth.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 10.Sutherland CJ, Wilde AH, Borden LS, Marks KE. A 10-year follow-up of one hundred consecutive Müller curved-stem total hip-replacement arthroplasties. J Bone Joint Surg Am. 1982;64(7):970–982. [PubMed] [Google Scholar]
- 11.Hayashi S, Nishiyama T, Fujishiro T, Hashimoto S, Kanzaki N, Nishida K, Kuroda R, Kurosaka M. Evaluation of the accuracy of femoral component orientation by the CT-based fluoro-matched navigation system. Int Orthop. 2013;37(6):1063–1068. doi: 10.1007/s00264-013-1852-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nogler M, Kessler O, Prassl A, Donnelly B, Streicher R, Sledge JB, Krismer M. Reduced variability of acetabular cup positioning with use of an imageless navigation system. Clin Orthop Relat Res. 2004;426:159–163. doi: 10.1097/01.blo.0000141902.30946.6d. [DOI] [PubMed] [Google Scholar]
- 13.Stem ES, O’Connor MI, Kransdorf MJ, Crook J. Computed tomography analysis of acetabular anteversion and abduction. J Skeletal Radiol. 2006;35(6):385–389. doi: 10.1007/s00256-006-0086-4. [DOI] [PubMed] [Google Scholar]
- 14.Sugano N, Noble PC, Kamaric E. A comparison of alternative methods of measuring femoral anteversion. J Comput Assist Tomogr. 1998;22(4):610–614. doi: 10.1097/00004728-199807000-00019. [DOI] [PubMed] [Google Scholar]
- 15.Minoda Y, Kadowaki T, Kim M. Acetabular component orientation in 834 total hip arthroplasties using a manual technique. Clin Orthop Relat Res. 2006;445:186–191. doi: 10.1097/01.blo.0000201165.82690.f8. [DOI] [PubMed] [Google Scholar]
- 16.Jingushi S, Ohfuji S, Sofue M, et al. Multiinstitutional epidemiological study regarding osteoarthritis of the hip in Japan. J Orthop Sci. 2010;15(5):626–631. doi: 10.1007/s00776-010-1507-8. [DOI] [PubMed] [Google Scholar]