Abstract
Purpose
The proximal part of the long head of the biceps muscle has become a recognized cause of significant shoulder pain. Tenodesis of the long head of the biceps has been advocated as a treatment for pain resulting from biceps tendonopathy, biceps instability, and biceps tendon tears. All of these pathologies may be encountered during rotator cuff, SLAP or Bankart surgery, or in isolation. Several techniques have been described for this tenodesis, including various arthroscopic and subpectoral methods.
Methods
We present a modified bone bridge technique of Mazzocca et al., for subpectoral biceps tenodesis. In this technique we tenodese the tendon through two bone tunnels back over the muscle itself without implants.
Results
Application of this technique on 30 patients (ages 25–48 years) with short-term follow-up of 12–18 months showed statistically significant improvement (P value < 0.05) of the mean Constant and Oxford shoulder scores (pre-operative mean scores were 39.03 and 21.3, respectively, while postoperative mean scores were 76.43 and 44.8, respectively).
Conclusion
This technique has potential advantages as it allows the possibility of adjusting the tension of the biceps tendon before final suturing, in addition to quicker soft tissue healing.
Keywords: Subpectoral biceps tenodesis, Biceps tenotomy, Bone bridge technique, Bone tunnel fixation, Shoulder
Introduction
Tendonitis of the long head of the biceps brachii is a relatively common occurrence in patients with shoulder pain [1]. Biceps tendon pathology, like chronic degeneration, tears or subluxations, may be encountered during rotator cuff surgery or in isolation [2–4]. Surgical management of the biceps tendon is recommended in patients with persistent anterior shoulder pain after failure of nonoperative management, partial thickness tears of 50 % or greater, and medial subluxations [5–7]. Several techniques have been described for tenodesis of the long head of the biceps tendon. Among these procedures, differences arise between arthroscopic versus open techniques, location of the tenodesis, and methods of fixation. Fixation methods include tenodesis through a bone tunnel, the keyhole method, soft tissue tenodesis to the rotator interval or conjoint tendon, interference screw fixation, and suture anchors [5–11].
Here we present a modified bone bridge technique of Mazzocca et al. [12] for subpectoral biceps tenodesis.
Surgical technique
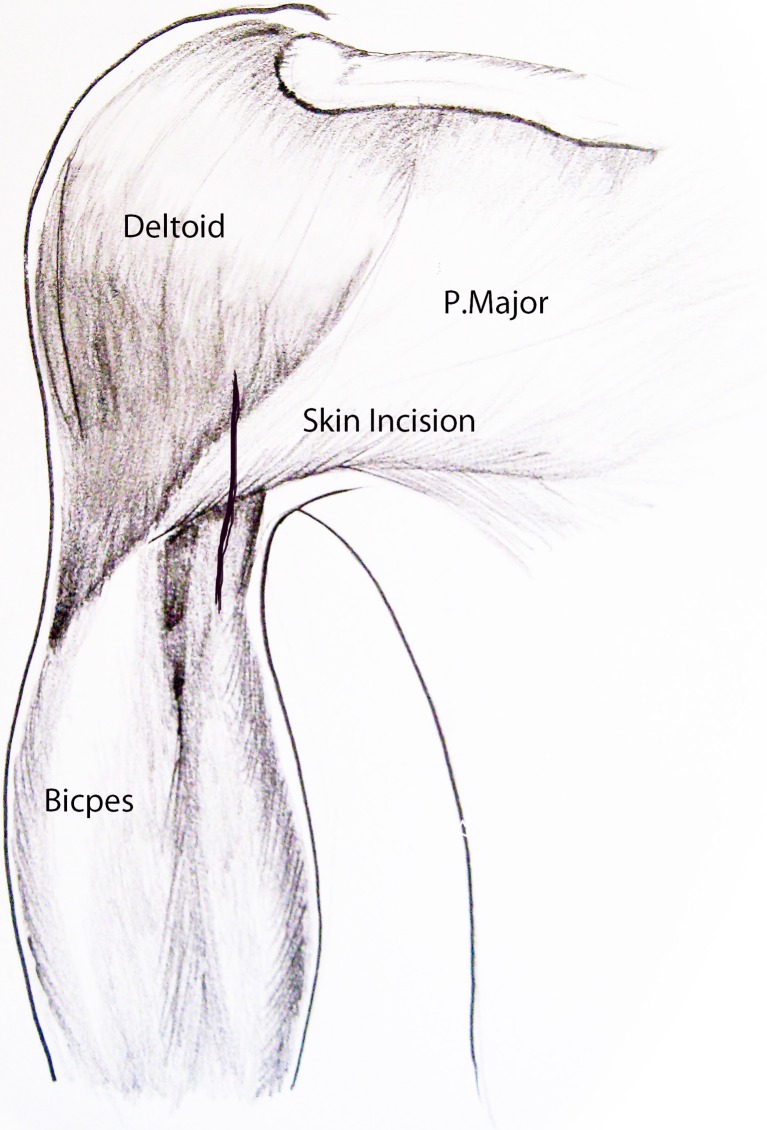
After completion of the arthroscopic part of the procedure including dealing with other pathologies associated with biceps tendinitis like rotator cuff pathology, SLAP or Bankart lesions, we perform a biceps tenotomy. After which, we turn to the subpectoral approach. The inferior border of the pectoralis major muscle is identified and its insertion on the humerus is palpated. Abduction and internal rotation can aid in identifying its exact location. A longitudinal incision (2–3 cm) in line with the axillary fold is then made starting 1 cm superior to the inferior border of the pectoralis tendon to 2–3 cm below the inferior border on the medial aspect of the arm (Fig. 1). Sharp dissection is completed through the subcutaneous fat layer and hemostasis is achieved with electrocautery. Blunt dissection is used at the level of the underlying biceps tendon. Two Hohmann retractors are placed medial and lateral to the humeral shaft, to retract the pectoralis major muscle superiorly.
Fig. 1.
The skin incision for the subpectoral biceps tenodesis
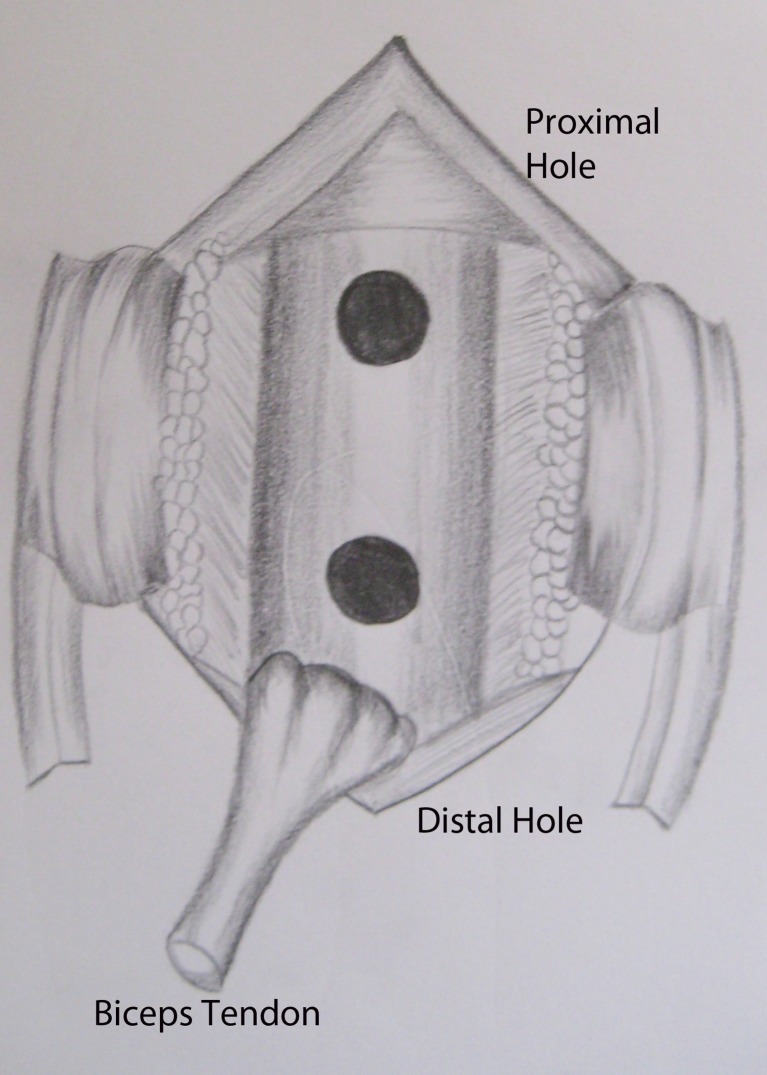
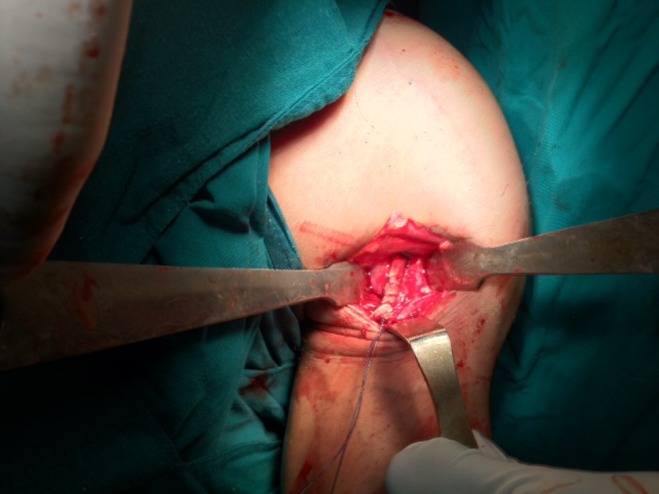
The tendon of the long head of the biceps is then identified and the sheath is split vertically (Fig. 2). A clamp is placed deep to it and the tendon is pulled, delivering it into the wound (Fig. 3). To ensure appropriate tensioning of the biceps tendon, the proximal portion of the tendon, which is the thickened part of the tendon, is resected (about 30 mm) to leave 20–25 mm of tendon proximal to the musculotendinous portion of the biceps [11] while the remaining portion is weaved by Vicryl #2 suture using a whip-stitch (Fig. 4). The electrocautery is used to open the periosteum and expose bone of the bicipital tunnel. A 4.5-mm drill is used to drill a proximal hole at the top of exposed bone through the anterior cortex of the humerus, and a second distal hole is also made 1.5–2 cm below the first one, at the level of the lower border of the pectoralis major muscle (Figs. 5 and 6).
Fig. 2.

Identification of biceps tendon
Fig. 3.

Delivering of biceps tendon
Fig. 4.

Weaving the tendon by absorbable suture using a whip-stitch
Fig. 5.
The two holes on the anterior cortex of the humerus
Fig. 6.

The two holes on the anterior cortex of the humerus and the tendon is ready for passing through the hole
The vicryl needle used to weave the tendon is inserted reversely (suture side first) through the distal hole and retrieved from the proximal one by an arthroscopic suture hook, which is an integral instrument to shorten the time and facilitate this step. The tendon is pulled through both holes, after that tensioning is adjusted by pulling the muscultotendionous junction to the distal hole and the tendon is sutured on the muscle itself (Figs. 7 and 8). The wound is then irrigated and closed with subcuticular stiches.
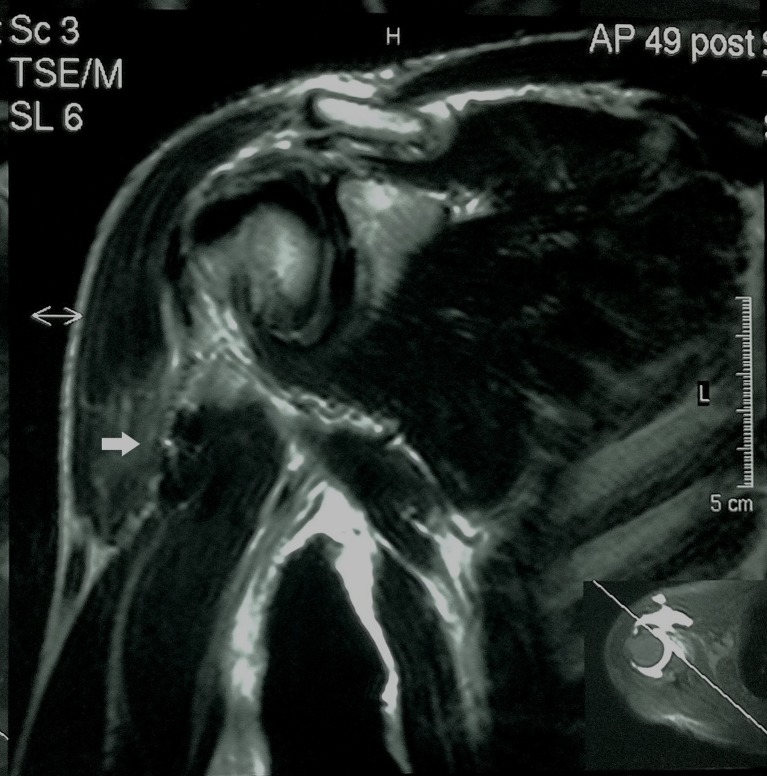
Fig. 7.
The tendon is secured through the bone tunnel
Fig. 8.
Postoperative MRI of the shoulder shows the tendon folding on the muscle (white arrow)
Patient and methods
Our present series included 30 patients (aged 25–48 years) with isolated biceps pathology non responsive to conservative treatment nor local injections. The follow-up period was between 12 and 18 months. None of the repairs failed and none of the patients reported persistent pain or loss of function. Clinical analysis of the results in our series compare the preoperative and postoperative Constant and Oxford shoulder scores. Results showed a significant improvement of the average in both shoulder scores (preoperative mean scores were 39.03 and 21.3, respectively, while postoperative mean scores were 76.43 and 44.8, respectively).
Postoperative management
Postoperative activity is typically dictated by the procedures that have been performed in conjunction with the biceps tenodesis. However in this series of isolated biceps tenodesis, a sling was worn for the first four weeks and we started passive ROM from day one and active abduction and external rotation was allowed, but active shoulder and elbow flexion was avoided for four weeks. Between four weeks and six weeks, gradual active ROM is started as well as weaning of the sling. After eight weeks the strengthening phase should be started.
Discussion
Proximal biceps tenodesis has become popular in recent years. The subpectoral approach offers a minimally invasive technique, with easy access. Methods of fixation vary from interference screws, soft tissue fixation, or transosseous sutures.
Mazzocca et al. [13] performed a biomechanical evaluation of four fixation techniques for proximal biceps tenodesis: subpectoral bone tunnel, arthroscopic interference screw, subpectoral interference screw and arthroscopic suture anchor. They concluded that there were no statistically significant differences in ultimate failure strength between them.
We describe our modified technique for subpectoral biceps tenodesis, with two bone tunnels and suturing over a bony bridge. The bone bridge technique is well known in tendon fixations and has been described previously [12].
Biomechanical and clinical studies have shown that the bone tunnel fixation is comparable, if not superior to other techniques regarding tensile strength, tendon to bone healing and postoperative outcomes [14–17].
This method has potential advantages over the previous described techniques as it allows the possibility of adjusting the tension of the biceps tendon before final suturing, in addition to quicker soft tissue healing. Also it is technically less demanding and does not use any hardware. Moreover, this procedure has not been associated with an increased risk of infection, nerve injury, or wound complications.
Conclusion
Modified subpectoral biceps tenodesis via bone bridge technique has potential advantages including that it is technically less demanding, there is no use of hardware and it allows the possibility of adjusting the tension of the biceps tendon before final suturing, in addition to having quicker soft tissue healing.
References
- 1.Murthi AM, Vosburgh CL, Neviaser TJ. The incidence of pathologic changes of the long head of the biceps tendon. J Shoulder Elbow Surg. 2000;9:382–385. doi: 10.1067/mse.2000.108386. [DOI] [PubMed] [Google Scholar]
- 2.Neer CS. Impingement lesions. Clin Orthop Relat Res. 1983;173:70–77. [PubMed] [Google Scholar]
- 3.Post M, Benca P. Primary tendinitis of the long head of the biceps. Clin Orthop Relat Res. 1989;246:117–125. [PubMed] [Google Scholar]
- 4.Moros C, Levine WN, Ahmad CS. Suture anchor and percutaneous intra-articular transtendon biceps tenodesis. Sports Med Arthrosc. 2008;16:177–179. doi: 10.1097/JSA.0b013e3181824efd. [DOI] [PubMed] [Google Scholar]
- 5.Sekiya JK, Elkousy HA, Rodosky MW. Arthroscopic biceps tenodesis using the percutaneous intra-articular transtendon technique. Arthroscopy. 2003;19:1137–1141. doi: 10.1016/j.arthro.2003.10.022. [DOI] [PubMed] [Google Scholar]
- 6.Gartsman GM, Hammerman SM. Arthroscopic biceps tenodesis: operative technique. Arthroscopy. 2000;16:550–552. doi: 10.1053/jars.2000.4386. [DOI] [PubMed] [Google Scholar]
- 7.Boileau P, Neyton L. Arthroscopic tenodesis for lesions of the long head of the biceps. Oper Orthop Traumatol. 2005;17:601–623. doi: 10.1007/s00064-005-1154-y. [DOI] [PubMed] [Google Scholar]
- 8.Castagna A, Conti M, Mouhsine E, Bungaro P, Garofalo R. Arthroscopic biceps tendon tenodesis: the anchorage technical note. Knee Surg Sports Traumatol Arthrosc. 2006;14:581–585. doi: 10.1007/s00167-005-0026-1. [DOI] [PubMed] [Google Scholar]
- 9.Boileau P, Krishnan SG, Coste JS, Walch G. Arthroscopic biceps tenodesis: a new technique using bioabsorbable interference screw fixation. Arthroscopy. 2002;18:1002–1012. doi: 10.1053/jars.2002.36488. [DOI] [PubMed] [Google Scholar]
- 10.Millett PJ, Sanders B, Gobezie R, Braun S, Warner JJ. Interference screw vs. suture anchor fixation for open subpectoral biceps tenodesis: does it matter? BMC Musculoskelet Disord. 2008;9:121. doi: 10.1186/1471-2474-9-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mazzocca AD, Rios CG, Romeo AA, Arciero RA. Subpectoral biceps tenodesis with interference screw fixation. Arthroscopy. 2005;21:896. doi: 10.1016/j.arthro.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 12.Mazzocca AD, Noerdlinger MA, Romeo AA. Mini open and sub pectoral bicepstenodesis. Oper Tech Sports Med. 2003;11:24–31. doi: 10.1053/otsm.2003.35887. [DOI] [Google Scholar]
- 13.Mazzocca AD, Bicos J, Santangelo S, Romeo AA, Arciero RA. The biomechanical evaluation of four fixation techniques for proximal biceps tenodesis. Arthroscopy. 2005;21:1296–1306. doi: 10.1016/j.arthro.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 14.Large TM, Coley ER, Peindl RD, Fleischli JE. A biomechanical comparison of 2 ulnar collateral ligament reconstruction techniques. Arthroscopy. 2007;23:141–150. doi: 10.1016/j.arthro.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 15.Armstrong AD, Dunning CE, Ferreira LM, Faber KJ, Johnson JA, King GJ. A biomechanical comparison of four reconstruction techniques for the medial collateral ligament-deficient elbow. J Shoulder Elbow Surg. 2005;14:207–215. doi: 10.1016/j.jse.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 16.Stuby FM, Langenbeck JE, Eingartner C, Weise K, Rolauffs B. Bone tunnel fixation versus suture anchor: mid- and long-term results after distal biceps tendon rupture. Z Orthop Unfall. 2007;145:181–185. doi: 10.1055/s-2007-965203. [DOI] [PubMed] [Google Scholar]
- 17.ElMaraghy A, Devereaux MW. Bone tunnel fixation for repair of tibialis anterior tendon rupture. Foot Ankle Surg. 2010;16:e47–e50. doi: 10.1016/j.fas.2009.10.013. [DOI] [PubMed] [Google Scholar]