Abstract
Purpose
Despite the high incidence of cases of minimally displaced lateral or posterior malleolus ankle fractures, treatment guidelines are still an issue of controversy. The purpose of this study was to delineate treatment preferences among orthopaedic surgeons in these fractures with and without concomitant posterior malleolus fractures. We hypothesized that concomitant minimally displaced fractures of the posterior malleolus can shift treatment preference towards operative intervention.
Methods
A questionnaire-based study was conducted among orthopaedic surgeons attending the 2012 European Federation of National Associations of Orthopaedics and Traumatology Conference (EFORT) in Berlin, Germany. Treatment preferences were reported for minimally displaced lateral malleolus fractures seen on radiographs and were then compared with treatment preferences when computed tomography (CT) was added revealing a concomitant minimally displaced posterolateral fracture of the posterior malleolus.
Results
The cohort comprised 177 surgeons from all six continents. When radiographs showing a minimally displaced lateral malleolus fracture were presented, nonoperative management was indicated by 35 % (62) of participants, whereas 65 % (115) preferred operative intervention. After CT views were added showing an accompanying minimally displaced posterolateral posterior malleolus fracture, 79 % (140) suggested operative intervention and only 21 % (37) advocated nonoperative management (p = 0.03).
Conclusions
Most surgeons prefer open reduction with internal fixation for minimally displaced lateral malleolar fractures. The presence of concomitant posterior malleolus fractures in these cases shifts treatment preference further towards open reduction with internal fixation. Because the posterior malleolus fragment might not be well delineated on standard ankle radiographs, a high index of suspicion is warranted, and the use of CT should be considered in these cases.
Keywords: Ankle fractures, Lateral malleolus, Posterior malleolus, Internal fixation, Decision making
Introduction
Ankle fractures are among the most common fractures treated by orthopaedic surgeons [21], with an incidence of approximately 187 fractures per 100,000 people each year [6]. Between 60 % and 70 % are unimalleolar fractures, the majority involving the lateral malleolus [5, 6]. Posterior malleolus fractures occur in 7–44 % of ankle fractures [4, 5, 11, 18].
Despite the high incidence of fractures involving the lateral or posterior malleolus, the indications for operative intervention remain an issue of controversy among orthopaedic surgeons. When there is minimal displacement, it is acceptable to treat lateral malleolus fractures nonoperatively [8, 9, 14, 16]. However, fractures of the posterior malleolus, which usually occur in combination with lateral malleolus fractures [20, 21], may alter treatment decisions even when there is minimal displacement of the fragments. Although there is still debate whether the primary role of the posterior malleolus is related to peak stress distribution or to tibiotalar stability [7, 19], indications for operative intervention in cases of posterior malleolus fractures are frequently based on fragment size [7, 8, 10]. Accordingly, 97 % of surgeons preferred operative management for posterior malleolus fractures in one study when >50 % of the articular surface was involved [8]. Yet, common combinations of minimally displaced lateral malleolus fractures with minimally displaced posterior malleolus fractures that involve <50 % of the articular surface increase the uncertainty regarding preferred treatment. Accordingly, in a recent review, no consensus was found as to which posterior malleolus fragment size should be internally fixed [19].
Understanding current treatment preferences among an international community of orthopaedic surgeons in cases of minimally displaced lateral malleolus fractures that occur in combination with minimally displaced posterior malleolus fractures can assist in delineating treatment guidelines for this injury. We therefore conducted a questionnaire-based study among an international group of orthopaedic surgeons by presenting specific management dilemmas that relate to this type of injury. We hypothesized that in cases of minimally displaced lateral malleolus fracture, the presence of concomitant minimally displaced posterior malleolus fracture can shift the preferred treatment approach towards operative intervention, and that type of orthopaedic subspecialty may be associated with such decisions.
Methods
A questionnaire-based study was conducted among surgeons attending the 2012 European Federation of National Associations of Orthopaedics and Traumatology Conference (EFORT) in Berlin, Germany. Participants were asked to complete a questionnaire (Fig. 1) regarding their treatment preferences for minimally displaced lateral malleolus fractures as seen on standard non-weight-bearing trauma series radiographs (Fig. 2). The same questionnaire was then presented to the participants with the addition to the case of sagittal and axial computed tomography (CT) images that disclosed a concomitant minimally displaced posterolateral oblique-type fracture of the posterior malleolus involving between 30 % and 50 % of the articular surface (Fig. 3). Type of subspecialty, type of practice (academic university-affiliated, nonacademic), number of years in practice, and volume of trauma surgery were also provided by each participant.
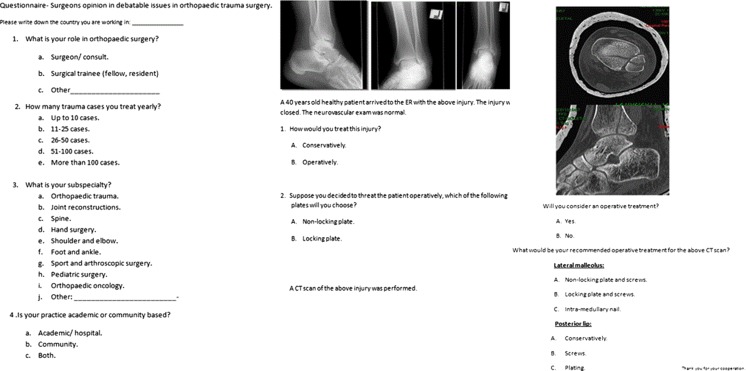
Fig. 1.
Study questionnaire
Fig. 2.
Three ankle trauma radiograph series. A minimally displaced lateral malleolus fracture is seen
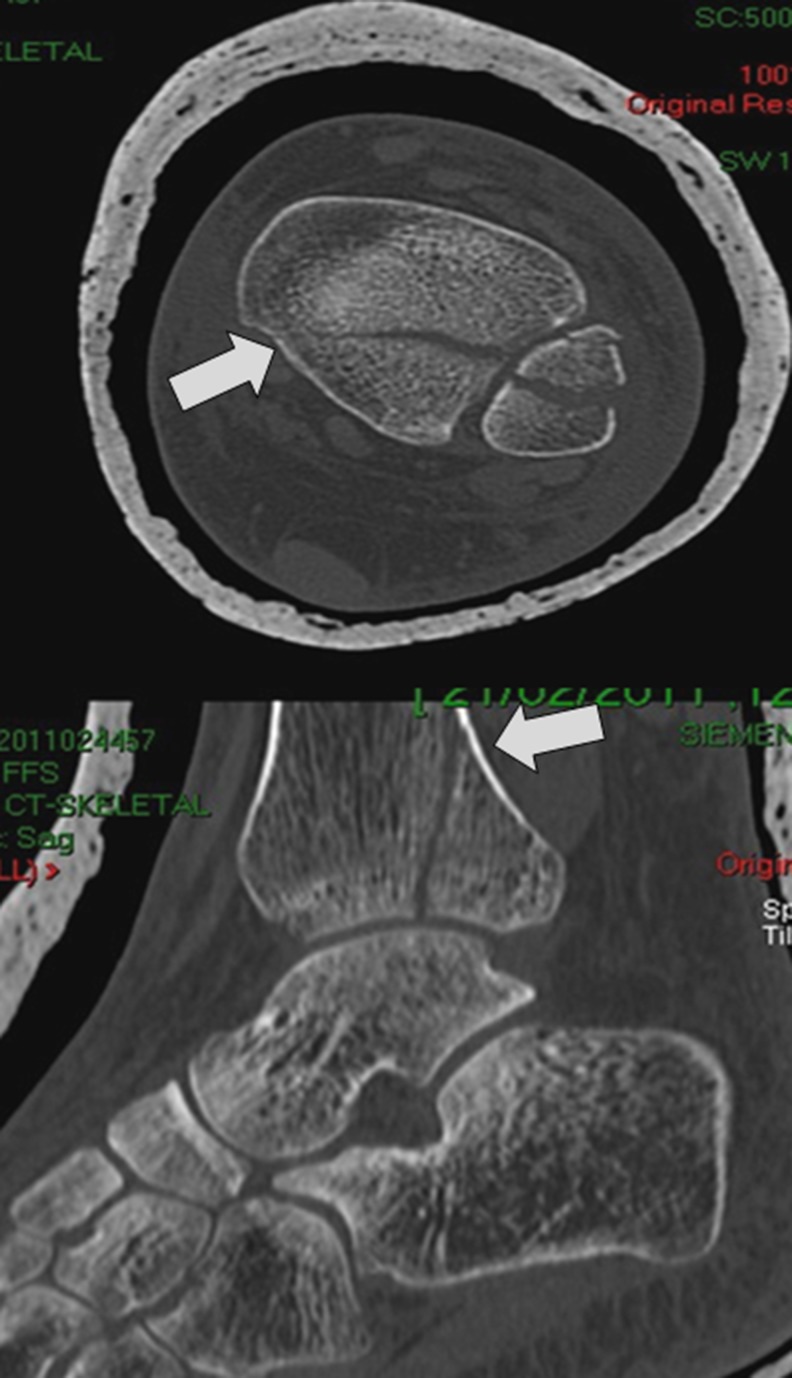
Fig. 3.
Axial and sagittal computed tomography (CT) cuts of the same case presented in Fig. 1 disclosing a concomitant posterolateral oblique-type fracture of the posterior malleolus
Statistical analysis
A univariate analysis was performed using the chi-square test to compare treatment preferences before and after the posterior malleolus fracture was presented on CT cuts. A p value < 0.05 was considered statistically significant.
Results
A total of 177 surgeons participated in the study (Table 1). Demographic data is presented in Fig. 4a–d. In general, >80 % of participants practiced in hospitals. Nearly 60 % had at least ten years of experience; about half were orthopaedic trauma specialists, and 8 % were foot and ankle surgeons.
Table 1.
Percentage and number of orthopaedic surgeons surveyed by country of practice
| Country | Percent (number) |
|---|---|
| Albania | 3 % (5) |
| Argentina | 2.4 % (4) |
| Armenia | less than 1 % (1) |
| Australia | 1.2 % (2) |
| Austria | 1.8 % (3) |
| Belgium | 1.2 % (2) |
| Brazil | 1.8 % (3) |
| Bulgaria | 1.2 % (2) |
| Chile | < 1 % (1) |
| China | < 1 % (1) |
| Colombia | 3.6 % (6) |
| Czech Republic | 1.2 % (2) |
| Denmark | 3.6 % (6) |
| France | 5.4 % (9) |
| Germany | 2.4 % (4) |
| Greece | 3.6 % (6) |
| Holland | < 1 % (1) |
| Hungary | 1.2 % (2) |
| Indonesia | < 1 % (1) |
| Iran | 1.2 % (2) |
| Ireland | 1.2 % (2) |
| Israel | 1.8 % (3) |
| Italy | 6.0 % (10) |
| Japan | 1.2 % (2) |
| Korea | < 1 % (1) |
| Latvia | 1.8 % (3) |
| Lithuania | 3.0 % (5) |
| Mexico | < 1 % (1) |
| Netherlands | 1.8 % (3) |
| Norway | < 1 % (1) |
| Paraguay | < 1 % (1) |
| Poland | 5.4 % (9) |
| Portugal | 2.4 % (4) |
| Rumania | < 1 % (1) |
| Russia | 3.6 % (6) |
| Serbia | 2.4 % (4) |
| Singapore | < 1 % (1) |
| Spain | 4.8 % (8) |
| Switzerland | 2.4 % (4) |
| Turkey | 6.6 % (11) |
| United Kingdom | 12 % (20) |
| Uruguay | 1.2 % (2) |
| USA | < 1 % (1) |
Fig. 4.
a–d. Academic and professional characteristics of the study cohort
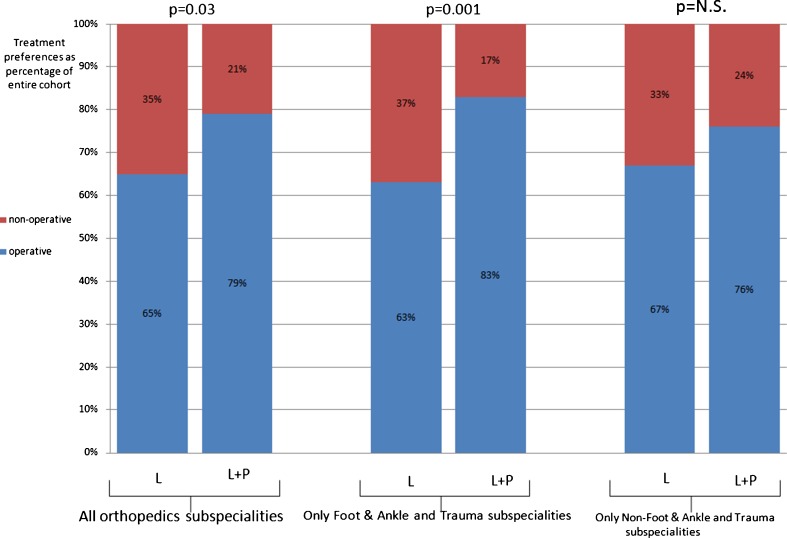
Nonoperative management was suggested by 35 % (62) of participants when ankle radiographs showing minimally displaced lateral malleolus fracture were presented; 65 % (115) preferred operative treatment (Fig. 5). After presenting CT images disclosing a concomitant minimally displaced posterolateral posterior malleolus fracture, operative treatment was suggested by 79 % (140) and nonoperative treatment by 21 % (37). This shift in preferred treatment approach was significant (p = 0.03). Among surgeons suggesting open reduction with internal fixation (140), two thirds [63 % (88)] preferred nonlocking plates for lateral malleolus fixation, a third [33 % (46)] preferred locking plates and 4 % (6) suggest intramedullary fixation. Regarding treatment preference for posterior malleolus fractures among this group of 140 surgeons, 81 % (113) indicated they would address this posterior fragment with internal fixation as well.
Fig. 5.
Treatment preferences among orthopaedic surgeons. L lateral malleolus fracture only is seen on radiographs; L+P concomitant posterior malleolus fracture is seen on computed tomography (CT) cuts
When the study cohort was divided in groups—one including only foot and ankle and trauma surgeons [48 % (85)] and another all other subspecialties [52 % (92)]—the following treatment preferences were observed: Based on radiographs only, in the foot and ankle and trauma group, 37 % (32) suggested nonoperative management and 63 % (53) internal fixation; with the addition of CT images, only 17 % (15) supported nonoperative management, and 83 % (70) recommended surgery (p = 0.001) (Fig. 5). In the other subspecialty groups, based on radiographs only, 33 % (30) recommended nonoperative management, and 67 % (62) advocated operative treatment. After CT images were provided and the posterior malleolus fracture could be appreciated, 24 % (22) recommended nonoperative management and 76 % (70) internal fixation. The addition of CT images did not change preferred treatment approach regarding nonoperative vs. operative treatment in this group of surgeons (p = 0.1) (Fig. 5).
Discussion
This survey showed that the majority of surgeons preferred operative treatment for minimally displaced fracture of the lateral malleolus. The appearance of concomitant minimally displaced fracture of the posterior malleolus involving <50 % of the articular surface significantly shifted treatment decision further towards internal fixation. To the best of our knowledge, surgical indications for this type of malleolar injury have not been clearly defined until now, and preferences among an international community of orthopaedic surgeons have not previously been presented. Whereas some investigators recommend nonoperative treatment for minimally displaced fractures [2, 3, 21], others suggest internal fixation of the lateral malleolus fragment [7, 8] and then fixation of the posterior malleolus fragment only if reduction of this fragment was not achieved following lateral malleolus fixation. Our findings suggest that in this scenario of ankle fractures, the majority of orthopaedic surgeons prefer internal fixation of both fragments. It seems that most surgeons are concerned by inadequate reduction and stabilisation of these fragments, which involve the articular surface. This is in accordance with data showing that 1 mm of tibiotalar displacement was sufficient to result in a 42 % increase in tibiotalar contact pressure [15, 20], thereby potentially promoting early ankle-joint arthritis. Moreover, this study revealed that surgeons involved in foot and ankle and trauma practice are essentially those that most likely shifted treatment preference further towards operative intervention when concomitant posterior malleolar fragment is observed on CT. Surgeons who were not foot and ankle or trauma subspecialists were not significantly affected in their treatment preferences when viewing radiographs only compared with viewing CT images. As foot and ankle and trauma surgeons are more likely to have follow-up on patients with these types of injuries their every-day practice, and as these groups of surgeons are likely more familiar with the literature in this respect, it may be advisable to adopt their opinions when delineating international treatment guidelines.
Ankle malleolar fractures with minimal displacement pose treatment dilemmas to orthopaedic surgeons. Intra-articular displacement, talus subluxation and failure to achieve or maintain closed reduction [8, 10, 21] may all justify surgical intervention. Some authors show that nonoperative treatment in minimally displaced lateral malleolar fractures result in good outcomes [2, 3, 21]. Moreover, this type of injury is regarded as supination–external rotation type II (Lauge Hansen classification type II) [13], which is considered a stable fracture; therefore, the advisability of operative intervention may be questionable. However, our data indicate that the majority of surgeons preferred operative treatment in this type of injury. It may be argued that the preference towards operative intervention is due to reasons such as early mobilisation and possibly faster rehabilitation; this, however, was not explored in our study. The occurrence of concomitant posterior malleolus fractures, which frequently accompany lateral malleolus fractures [20, 21], may affect treatment decisions. Surgical intervention may then be indicated in cases involving posterior tibiotalar subluxation [10] and may also depend on the size of the posterior malleolus fragment [7, 8, 10]. In this survey, the significant change in surgeon opinion towards operative intervention may relate to the fact this type of fracture, regarded as supination–external rotation type III according to Lauge-Hansen classification, is considered unstable [17].
In recent years, locking plates became popular in orthopaedic surgery, as they allow transferring loads from the plate itself directly to the screws, thus sparing loads from bone fragments [1, 12]. This may be of particular importance in cases of fractures with comminution and those involving osteopenic bone. That advantage, however, has not been clinically demonstrated in the case of lateral malleolus fractures in active adult populations. Accordingly, using nonlocking plates was still the preferred method of fixation for the lateral malleolus by most surgeons in this survey.
When an operative approach is selected for cases of minimally displaced lateral malleolus and concomitant minimally displaced posterior malleolus fractures, it is possible to either reduce and internally fix the lateral malleolus only, assuming that reduction of the posterior malleolus is achieved by simple ligamentotaxis [10]. The other possibility is to fix and ascertain rigid stabilisation of both malleoli. Our study shows that most surgeons support internal fixation of both fragments in these cases. Whereas this approach might expose patients to additional risks when unnecessary hardware is added (i.e. for the posterior malleolus), it has the advantage of solid fixation of all fragments and the potential of recreating a more congruent joint.
The majority of our study population comprised surgeons with greater than ten years in practice; one third had >20 years in practice. Moreover, >80 % were practicing in academic facilities. These data indicate that extensive surgical experience as well as academic knowledge was likely common to most participants, supporting the consideration of using of our findings as a basis for delineating internationally accepted guidelines for this injury.
Limitations of this study include the fact it relied on one type of injury. With more cases and variations in fracture type, a wider spectrum of decisions could have been expected. Moreover, the fact that a majority of the international group of orthopaedic surgeons supported operative intervention for an injury that involved a combination of minimally displaced lateral malleolus fractures with posterolateral oblique-type posterior malleolus fractures is not by itself a guarantee that this approach provides the best patient-care strategy. However, results of our study could be used as a rationale for further clinical trials.
Conclusion
Most surgeons prefer open reduction with internal fixation for minimally displaced lateral malleolar fractures. The presence of concomitant posterior malleolus fractures in these cases shifts treatment preference further towards open reduction with internal fixation. Because the posterior malleolus fragment might not be well delineated on standard ankle radiographs, a high index of suspicion should be reserved and the use of CT considered in these cases.
References
- 1.Anglen J, Kyle RF, Marsh JL, Virkus WW, Watters WC, 3rd, Keith MW, Turkelson CM, Wies JL, Boyer KM. Locking plates for extremity fractures. Review. J Am Acad Orthop Surg. 2009;17(7):465–472. doi: 10.5435/00124635-200907000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Bauer M, Bergström B, Hemborg A, Sandegård J (1985) Malleolar fractures: nonoperative versus operative treatment. A controlled study. Clin Orthop Relat Res (199):17-27 [PubMed]
- 3.Bauer M, Jonsson K, Nilsson B. Thirty-year follow-up of ankle fractures. Acta Orthop Scand. 1985;56(2):103–106. doi: 10.3109/17453678508994329. [DOI] [PubMed] [Google Scholar]
- 4.Broos PL, Bisschop AP. Operative treatment of ankle fractures in adults: correlation between types of fracture and final results. Injury. 1991;22(5):403–406. doi: 10.1016/0020-1383(91)90106-O. [DOI] [PubMed] [Google Scholar]
- 5.Court-Brown CM, McBirnie J, Wilson G. Adult ankle fractures–an increasing problem? Acta Orthop Scand. 1998;69:43–47. doi: 10.3109/17453679809002355. [DOI] [PubMed] [Google Scholar]
- 6.Daly PJ, Fitzgerald RH, Jr, Melton LJ, Ilstrup DM. Epidemiology of ankle fractures in Rochester, Minnesota. Acta Orthop Scand. 1987;58:539–544. doi: 10.3109/17453678709146395. [DOI] [PubMed] [Google Scholar]
- 7.Gardner MJ, Streubel PN, McCormick JJ, Klein SE, Johnson JE, Ricci WM. Surgeon practices regarding operative treatment of posterior malleolus fractures. Foot Ankle Int. 2011;32:385–393. doi: 10.3113/FAI.2011.0385. [DOI] [PubMed] [Google Scholar]
- 8.Haraguchi N, Haruyama H, Toga H, Kato F. Pathoanatomy of posterior malleolar fractures of the ankle. J Bone Joint Surg Am. 2006;88(5):1085–1092. doi: 10.2106/JBJS.E.00856. [DOI] [PubMed] [Google Scholar]
- 9.Harper MC, Hardin G. Posterior malleolar fractures of the ankle associated with external rotation-abduction injuries. Results with and without internal fixation. J Bone Joint Surg Am. 1988;70:1348–1356. [PubMed] [Google Scholar]
- 10.Irwin TA, Lien J, Kadakia AR. Posterior malleolus fracture. J Am Acad Orthop Surg. 2013;21(1):32–40. doi: 10.5435/JAAOS-21-01-32. [DOI] [PubMed] [Google Scholar]
- 11.Klammer G, Kadakia AR, Joos DA, Seybold JD, Espinosa N. Posterior pilon fractures: a retrospective case series and proposed classification system. Foot Ankle Int. 2013;34(2):189–199. doi: 10.1177/1071100712469334. [DOI] [PubMed] [Google Scholar]
- 12.Krettek C, Gösling T (2006) Rockwood & Green’s fractures in adults, 6th edn: Lippincott Williams & Wilkins VOL I, Chapter 6. Principles of internal fixation
- 13.Lauge-Hansen N. Fractures of the ankle III. Genetic roentgenologic diagnosis of fractures of the ankle. Am J Roentgenol Radium Ther Nucl Med. 1954;71(3):456–471. [PubMed] [Google Scholar]
- 14.Lindsjö U. Operative treatment of ankle fracture-dislocations. A follow-up study of 306/321 consecutive cases. Clin Orthop Relat Res. 1985;199:28–38. [PubMed] [Google Scholar]
- 15.Lloyd J, Elsayed S, Hariharan K, Tanaka H. Revisiting the concept of talar shift in ankle fractures. Foot Ankle Int. 2006;27(10):793–796. doi: 10.1177/107110070602701006. [DOI] [PubMed] [Google Scholar]
- 16.McDaniel WJ, Wilson FC. Trimalleolar fractures of the ankle. An end result study. Clin Orthop Relat Res. 1977;122:37–45. [PubMed] [Google Scholar]
- 17.Okanobo H, Khurana B, Sheehan S, Duran-Mendicuti A, Arianjam A, Ledbetter S. Simplified diagnostic algorithm for Lauge-Hansen classification of ankle injuries. Radiographics. 2012;32(2):71–84. doi: 10.1148/rg.322115017. [DOI] [PubMed] [Google Scholar]
- 18.Tejwani NC, Pahk B, Egol KA. Effect of posterior malleolus fracture on outcome after unstable ankle fracture. J Trauma. 2010;69(3):666–669. doi: 10.1097/TA.0b013e3181e4f81e. [DOI] [PubMed] [Google Scholar]
- 19.van den Bekerom MP, Haverkamp D, Kloen P. Biomechanical and clinical evaluation of posterior malleolar fractures. A systematic review of the literature. J Trauma. 2009;66(1):279–284. doi: 10.1097/TA.0b013e318187eb16. [DOI] [PubMed] [Google Scholar]
- 20.van den Bekerom MP, van Dijk CN. Is fibular fracture displacement consistent with tibiotalar displacement. Clin Orthop Relat Res. 2010;468(4):969–974. doi: 10.1007/s11999-009-0959-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van der Griend R, Michelson JD, Bone LB. Fractures of the ankle and the distal part of the tibia. Instr Course Lect J Bone Joint Surg Am. 1997;78-A(11):1772–1783. [PubMed] [Google Scholar]