Abstract
Purpose
This study was to evaluate clinical outcomes and complications following multi-plate reconstruction for treating severe bicondylar tibial plateau fractures of young adults.
Methods
Between September 2007 and February 2012, 26 patients with severe bicondylar tibial plateau fractures met inclusion criteria; they were treated using multi-plate technique through combined approaches. Patients received an average follow-up of 40.8 (range, 18–64) months, which included anteroposterior and lateral imaging, postoperative complications, range of motion and stability of the knee. The Rasmussen score was applied for functional and radiological evaluation.
Results
Three to five plates were used for reconstruction. No intra-operative complications occurred. Postoperative complications included bulge of hardware in four patients and superficial dehiscence in three cases in the anterolateral incision of which one developed to deep infection. There was no neurovascular damage, and no implant breakage or loosening. Hardware was removed partly or totally in 16 cases. The average Rasmussen score at final follow-up was 27.2 (range, 21–30) points for functional evaluation and 16.4 (range, 14–18) for radiology.
Conclusions
Multi-plate reconstruction is a valid and safe method for treating severe bicondylar tibial plateau fractures of young adults.
Keywords: Bicondylar tibial plateau fracture, Fracture morphology, Multi-plate reconstruction, Clinical outcome, Complications
Introduction
The management of severe bicondylar tibial plateau fractures remains challenging and controversial; plates, external fixators and total knee arthroplasty have all been recommended in the literature [1–3]. For patients of young age and with a stable soft-tissue envelope, open reduction and internal fixation with plate(s) is preferred by more surgeons. Benefiting from the recent development of concepts and techniques such as staged management, combined approach and buttress fixation for posterior fragments, the clinical outcomes of bicondylar tibial plateau fractures have improved [1, 4–8]. However, the view of “severe” or “complex” was not homogeneous, as some authors regarded it as bicondylar tibial plateau fractures or AO type C fracture [9] and others as Schatzker types V and VI [10] or a high-energy tibial plateau fracture. Therefore, some cases that were not severely comminuted were in previous studies and achieved satisfactory outcomes by a relatively simple approach and fixation.
In our opinion, the morphological characteristics of the fracture should be further clarified. A “severe” bicondylar tibial plateau fracture should meet all of the following: lateral plateau fracture, medial plateau fracture with at least two fragments, coronal fracture with a posterior fragment, and articular surface depression requiring treatment. In order to focus on the fracture morphology and fixation method, in this study, a strict limitation for inclusion such as soft-tissue envelope, concomitant injury and age was set. The aim of this retrospective study was to investigate clinical outcomes and associated complications of severe bicondylar tibial plateau fractures treated with multi-plate reconstruction by combined approaches.
Patients and methods
This study was performed with the approval of our institution’s human subjects review board. Between September 2007 and February 2012, all patients who sustained a fracture of the proximal tibia were identified from our institution’s trauma-database. The criteria for inclusion were (1) lateral tibial plateau fractures (simple or comminuted), medial plateau fractures with at least two fragments, coronal fractures with a medial or lateral posterior fragment and 5-mm or more impacted articular surface; (2) age between 18 and 50 years; (3) the soft-tissue was classified as Gustilo grade I/II for open fracture [11] or Tscherne grade 0/1/2 for closed fracture [12]; and (4) multi-plate (three plates or more) reconstruction was the fixation method. Those with follow-up less than 18 months were excluded from the study. Patients with pre-existing deformity were also excluded, as well as the polytrauma cases. By reviewing the radiological digital data (X-ray and CT scan) and medical records, there were 26 patients making up our final study cohort (19 men, seven women; age range 25–50 years, average 40.7 years). No case had confirmed primary osteoporosis. Eighteen cases were closed fracture (seven were Tscherne grade 1 and 11 were grade 2) and eight were open fracture (five of Gustilo grade I and three of grade II). These 26 cases were all classified as 41-C3 fractures [9] or three-column fractures [7]; according to Schatzker classification, 24 cases were type VI and two were type V. The operations were all performed by the same chief surgeon (CL).
Eighteen cases had ipsilateral proximal fibular fractures, two cases presented with numbness of the dorsum of the foot which had improved at the six-month review without definitive treatment. The average injury-to-surgery interval was 9.2 (range, 4–18) days and average follow-up was 40.8 (range, 18–64) months.
Surgical technique
Open fractures were urgently irrigated and debrided in the emergency operation room and, if necessary, repeat debridements were performed. For all cases, a knee-spanning external fixator or a bony skeletal traction was applied before definitive surgical treatment. The open reduction and internal fixation took place when the soft tissues were stabilized and able to withstand incision.
Under general anaesthesia, the patient was brought on the radiolucent table in a lateral floating position that could facilitate combined posterior and anterior approaches. A posteromedial inverted L-shaped incision, which has been previously described in the literature [7, 13, 14], was first indicated to address the medial plateau fracture and the posterior fragment. The restoration of the knee joint was always started from the posterior-dorsal displaced fragment at the medial ridge of the proximal tibia. The fragment was reduced anatomically to be the landmark for the height of the articular surface and diameter in the anterior-posterior direction. It was connected with the shaft by a 3.5-mm medial plate for the proximal tibia (Synthes, Oberdorf, Switzerland), leaving the proximal screws shorter (usually 30-mm) than should be as the articular surface was not elevated. For the dorsal buttress, this plate was required to be placed posteriorly; therefore, it was hard to cover the anterior-medial fragment. Another 3.5-mm locking compression plate was needed for the fixation after reduction of the anterior-medial fragment.
The depressed articular surface, in the posterior-central or posterior-lateral region, was always relatively difficult for reduction by this approach. It could be addressed better through the anterior-lateral approach, however, the surface fragment could displace towards posterior during the reduction procedure from anterior, especially when the posterolateral cortex and proximal fibular were broken. Therefore, an undercontoured 3.5-mm oblique plate (from proximal lateral to the distal medial) was used to buttress the posterolateral fragment and to facilitate later reduction. For extreme comminuted cases, the posterior fragments needed another plate for fixation (Fig. 1a).
Fig. 1.
A 26-year-old male patient sustained a severe bicondylar tibial plateau fracture after a traffic accident. Preoperative (a), four-week postoperative (b), three-month postoperative (c), and 24 months postoperative (d)
The typical anterolateral approach was then performed when the knee joint was in flexion. The joint and articular surface were reduced under direct vision, supported with the rafting technique, and a locking plate was applied. As there are four proximal screws for rafting in the 3.5-mm lateral plate (Synthes, Oberdorf, Switzerland) used in recent years, autograft was only applied in four early cases in this series. After articular surface reduction, the proximal screws in the medial plates were changed for appropriate lengths. The location and alignment of the plate–knee construction was confirmed by C-arm, using both antero-posterior and lateral views. The wounds were closed in layers with drainages applied in both incisions.
Postoperative management and follow up
Early motion and non-weight bearing were emphasized in the postoperative protocols. Patients began passive knee range-of-motion exercises from the first day post-operation. Weight bearing was started from toe-touch at eight weeks and increased progressively from eight to 12 weeks. Full weight bearing was not permitted until 12 weeks.
These patients were regularly followed up postoperatively at one, three, six, 12 and 24 months. Standard anterior-posterior and lateral radiographs were applied to determine bone-plate position and fracture union progress. Functional and radiological outcomes were evaluated according to the Rasmussen score [15] by two surgeons (QZ and CL). The functional scoring system comprises five parts: pain, walking capacity, extension, range of motion and stability; it ranges from 0 to 30 and can be graded as excellent, good, fair or poor. The radiological scoring system comprises three parts: depression, plateau width and deformity of the knee; it ranges from 0 to 18. For this study, all patients were invited to the senior author’s (CL) clinic after January 2013 to evaluate the functional outcomes; for radiological assessment, nine patients took the X-ray examination while the other 17 patients utilized radiographs at 24-months postoperatively.
Results
Operative time was 149.2 minutes on average (range, 120–210 minutes). The mean blood loss was 520 mL (range, 300–850 mL). Three to five plates were applied for reconstruction (two cases had five plates, seven cases had four and the others had three). No intra-operative complications occurred. There were three cases of superficial dehiscence, all in the anterolateral incision; two cases healed by disinfection and dressing without surgical treatment and one developed to deep infection (the only case in this series). This patient received irrigation, debridement and retained drainage in the surgical theatre 11 days after internal fixation; then the drainage was removed and five days later the incision was closed; finally, there were no further complaints. No hardware failure occurred. Hardware was removed partly or totally in 16 cases, including the three cases mentioned above, and in four patients due to the obvious bulge in the lateral side and nine for social and personal reasons. During removal operation, screw breakage occurred in four cases.
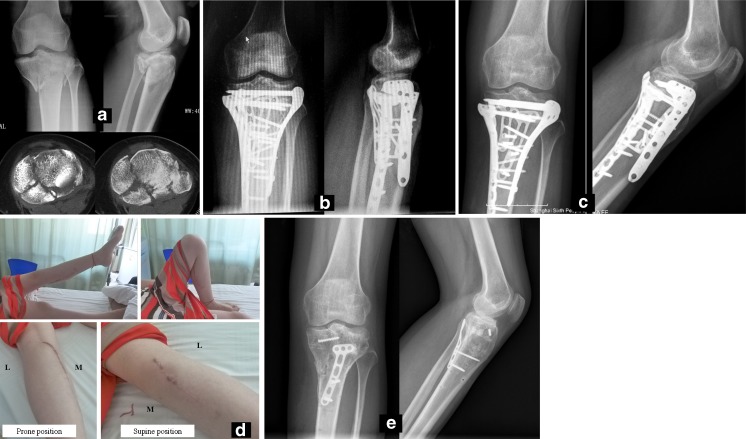
In terms of movement, six patients had limitation in extension, all less than 10°; the mean range of motion was 123.3° (105–140°) (Fig. 2d). Regarding pain, one patient had stabbing pain and eight patients had weather pain, while others claimed no pain. All patients had normal knee stability in extension and 20° in flexion. Three cases had varus deformity less than 10°, and 12 cases had second articular surface depression of less than 5 mm. The average Rasmussen functional score was 27.2 (range, 21–30), whereby 17 cases were excellent (27–30 points) and nine cases were good (20–26 points); the average radiological score was 16.4 (range, 14–18) points, of which all were excellent (Figs. 1 and 2).
Fig. 2.
A 25-year-old female patient sustained a severe bicondylar tibial plateau fracture after a traffic accident. Preoperative (a), three-months postoperative (b), 12-months postoperative (c), the range of motion and scars of combined incisions at 20-months postoperative (d), after hardware removal at 21-months postoperative and one nail breakage during removal (e). L lateral, M medial
Discussion
The fixation methods for bicondylar tibial plateau fracture include plates, external fixators and total knee arthroplasty, etc., but for young adults with a relatively stable soft-tissue envelope, plates may play a major role in fixation according to the literature [1, 5–7]. Dual incisions and combined medial-lateral plates are the mainstream method for the bicondylar tibial plateau fracture [6, 16], also for a large part of so-called complex or high-energy tibial plateau fractures. However, a single locking plate could also solve a high-energy Schatzker type VI fracture and achieve satisfactory outcomes [4, 17]. In contrast, some authors regarded the importance of the posterior fragment [18] and applied a third plate for posterior buttress fixation [1, 7, 13]. Therefore, just using the expressions “bicondylar, complex or high-energy” as criteria could make the patients inhomogeneous for fixation methods. This study benefited from the wide use of CT for intra-articular fracture in our hospital in recent years, whereby we set a clear condition in fracture morphology for inclusion criteria and hoped to retrieve the same severe bicondylar tibial plateau fractures. Restricting the soft-tissue envelope, concomitant injury and age could focus the study on the fixation method and exclude osteoporosis and arthritis as much as possible; however, this could also be a limitation of the study for not including the entire population and presenting better outcomes.
Knee stability and restoration of mechanical axis are important determinants in tibial plateau fracture patient outcome; also, the prevention of knee stiffness should be emphasized. For these patients, we reconstructed the bony stability and strived for anatomical reduction to restore the axis of limb and knee in the surgical procedure. The multi-plate reconstruction was rigid and made the early range-of-motion exercises possible. The exercise started at the first postoperative day, although it was helped by others in a passive way. We believe the mean 123.3° range of motion in outcomes was due to the rigid fixation and early passive motion. In this series, six patients (23 %) could not reach full extension, although all were less than 10°; thus, the postoperative extension exercises should be valued. In the radiological evaluation, we found three cases of varus less than 10° but well-tolerated and reported good functional results. This was similar to the previous literature [19], and we agree that mechanical malalignment greater than 10° would been correlated with poor long-term functional results and might complicate future knee arthroplasty [20].
Many bicondylar tibial fractures in previous studies only had a single main medial fragment [1, 17], which is recommended as a landmark for reduction. In this series, the medial plateau fracture had at least two fragments, but given the bony strength, medial plateau fractures were always simpler than those in the lateral plateau. Therefore, the reduction began from the fragment in the medial ridge, which is a solid region with the main fragment, and the correct reduction could be identified easily. Another fragment in the medial area was always anterior to the previous one and could not be covered by the same plate. It was rare but in some extremely complex cases, the posterior region between the medial ridge and proximal fibula had comminuted a fracture, needing two smaller plates for posterior-medial and posterior-lateral fixation (Fig. 2a). In most patients, the posterior region fracture was posterior-lateral shearing or depression. As the posterior-lateral region is complex because of the peroneal nerve [21] and anterior tibial artery [22], we applied an oblique plate and left proximal holes empty just for a posterior blocking. The reduction of the posterior-lateral fracture was from an anterior approach. This posterior blocking could prevent the fragment from dorsal displacement and avoid fixation in the anterior-posterior direction; the lateral-medial direction for fixation was safer.
The multi-plate and as long as 210 minutes of operation time were definitely risks of soft tissue complication. Although status of the soft-tissue envelope was restricted as criteria, there were still three cases of superficial dehiscence and deep infection. The average 9.2 days interval made it possible that the soft tissue in all cases appeared healthy enough to withstand incisional trauma. During the surgical procedure, the preservation of vascularity and soft-tissue integrity was also emphasized. As the wound complications were all in the anterolateral incision and the four-plate bearing posteromedial incision had none, and additionally, the four patients with an obvious bulge in the lateral side required removal, we supposed the high profile of the lateral plate shape for the Chinese population, instead of the number of plates might be a factor.
Hardware removal was a social issue rather than a medical problem in China. Although there was no loosening or breakage, no infection or dehiscence history, and the functional and radiological outcomes were satisfactory, many patients firmly required a hardware removal surgery (Fig. 2). Respecting the patients’ choice and traditional concept, we performed several removal operations and insisted on a non-weight bearing interval of four to six weeks after removal.
To our knowledge, this is the first study which clarified the severe bicondylar tibial plateau fracture by restricting the fracture morphology. Although the multi-plate reconstruction is beneficial for severe bicondylar tibial plateau fracture, especially in young adults with fair soft-tissue envelope, skilled management including surgical techniques and peri-operative treatment are necessary. In summary, multi-plate reconstruction is a valid and safe method for treating severe bicondylar tibial plateau fracture of young adults, and longer clinical outcomes are also expected in the future.
References
- 1.Eggli S, Hartel MJ, Kohl S, Haupt U, Exadaktylos AK, Röder C. Unstable bicondylar tibial plateau fractures: a clinical investigation. J Orthop Trauma. 2008;22(10):673–679. doi: 10.1097/BOT.0b013e31818b1452. [DOI] [PubMed] [Google Scholar]
- 2.Canadian Orthopaedic Trauma Society Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures. Results of a multicenter, prospective, randomized clinical trial. J Bone Joint Surg Am. 2006;88(12):2613–2623. doi: 10.2106/JBJS.E.01416. [DOI] [PubMed] [Google Scholar]
- 3.Kini SG, Sathappan SS. Role of navigated total knee arthroplasty for acute tibial fractures in the elderly. Arch Orthop Trauma Surg. 2013;133(8):1149–1154. doi: 10.1007/s00402-013-1792-8. [DOI] [PubMed] [Google Scholar]
- 4.Biggi F, Di Fabio S, D’Antimo C, Trevisani S. Tibial plateau fractures: internal fixation with locking plates and the MIPO technique. Injury. 2010;41(11):1178–1182. doi: 10.1016/j.injury.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 5.Weil YA, Gardner MJ, Boraiah S, Helfet DL, Lorich DG. Posteromedial supine approach for reduction and fixation of medial and bicondylar tibial plateau fractures. J Orthop Trauma. 2008;22(5):357–362. doi: 10.1097/BOT.0b013e318168c72e. [DOI] [PubMed] [Google Scholar]
- 6.Barei DP, Nork SE, Mills WJ, Coles CP, Henley MB, Benirschke SK. Functional outcomes of severe bicondylar tibial plateau fractures treated with dual incisions and medial and lateral plates. J Bone Joint Surg Am. 2006;88(8):1713–1721. doi: 10.2106/JBJS.E.00907. [DOI] [PubMed] [Google Scholar]
- 7.Luo CF, Sun H, Zhang B, Zeng BF. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma. 2010;24(11):683–692. doi: 10.1097/BOT.0b013e3181d436f3. [DOI] [PubMed] [Google Scholar]
- 8.Nikolaou VS, Tan HB, Haidukewych G, Kanakaris N, Giannoudis PV. Proximal tibial fractures: early experience using polyaxial locking-plate technology. Int Orthop. 2011;35(8):1215–1221. doi: 10.1007/s00264-010-1153-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audigé L. Fracture and dislocation classification compendium 2007: orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma. 2007;21(10 Suppl):S1–S133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 10.Schatzker J, McBroom R, Bruce D. The tibial plateau fracture: the Toronto experience 1968–1975. Clin Orthop Relat Res. 1979;138:94–104. [PubMed] [Google Scholar]
- 11.Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24:742–746. doi: 10.1097/00005373-198408000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Tscherne H, Oestern HJ. A new classification of soft-tissue damage in open and closed fractures. Unfallheilkunde. 1982;85:111–115. [PubMed] [Google Scholar]
- 13.Chang SM, Wang X, Zhou JQ, Huang YG, Zhu XZ. Posterior coronal plating of bicondylar tibial plateau fractures through posteromedial and anterolateral approaches in a healthy floating supine position. Orthopedics. 2012;35(7):583–588. doi: 10.3928/01477447-20120621-03. [DOI] [PubMed] [Google Scholar]
- 14.He X, Ye P, Hu Y, Huang L, Zhang F, Liu G, Ruan Y, Luo C. A posterior inverted L-shaped approach for the treatment of posterior bicondylar tibial plateau fractures. Arch Orthop Trauma Surg. 2013;133(1):23–28. doi: 10.1007/s00402-012-1632-2. [DOI] [PubMed] [Google Scholar]
- 15.Rasmussen PS. Tibial condylar fractures: impairment of knee joint stability as an indication for surgical treatment. J Bone Joint Surg Am. 1973;55:1331–1350. [PubMed] [Google Scholar]
- 16.Prasad GT, Kumar TS, Kumar RK, Murthy GK, Sundaram N. Functional outcome of Schatzker type V and VI tibial plateau fractures treated with dual plates. Indian J Orthop. 2013;47(2):188–194. doi: 10.4103/0019-5413.108915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weaver MJ, Harris MB, Strom AC, Smith RM, Lhowe D, Zurakowski D, Vrahas MS. Fracture pattern and fixation type related to loss of reduction in bicondylar tibial plateau fractures. Injury. 2012;43(6):864–869. doi: 10.1016/j.injury.2011.10.035. [DOI] [PubMed] [Google Scholar]
- 18.Barei DP, O’Mara TJ, Taitsman LA, Dunbar RP, Nork SE. Frequency and fracture morphology of the posteromedial fragment in bicondylar tibial plateau fracture patterns. J Orthop Trauma. 2008;22(3):176–182. doi: 10.1097/BOT.0b013e318169ef08. [DOI] [PubMed] [Google Scholar]
- 19.Weigel DP, Marsh JL. High-energy fractures of the tibial plateau. Knee function after longer follow-up. J Bone Joint Surg Am. 2002;84-A:1541–1551. doi: 10.2106/00004623-200209000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Honkonen SE. Indications for surgical treatment of tibial condyle fractures. Clin Orthop. 1994;302:199–205. [PubMed] [Google Scholar]
- 21.Sun H, Luo CF, Yang G, Shi HP, Zeng BF. Anatomical evaluation of the modified posterolateral approach for posterolateral tibial plateau fracture. Eur J Orthop Surg Traumatol. 2013;23(7):809–818. doi: 10.1007/s00590-012-1067-z. [DOI] [PubMed] [Google Scholar]
- 22.Heidari N, Lidder S, Grechenig W, Tesch NP, Weinberg AM. The risk of injury to the anterior tibial artery in the posterolateral approach to the tibia plateau: a cadaver study. J Orthop Trauma. 2013;27(4):221–225. doi: 10.1097/BOT.0b013e318271f8f0. [DOI] [PubMed] [Google Scholar]