Abstract
Purpose
The collum femoris preserving (CFP) uncemented prosthesis has a bone-preserving, high subcapital neck resection and a short anatomical stem. The ideal arthroplasty option in the younger, active patient is a subject of some debate. We evaluated midterm outcomes of the CFP in this patient population.
Methods
A prospective, consecutive cohort of 75 CFP total hip replacement (THR) patients with a mean age of 52 years was followed for a mean of 9.3 years. Patients were assessed using the Harris Hip Score (HHS). Pain was assessed using a visual analogue scale (VAS) and activity levels using the University of California, Los Angeles (UCLA) score. Radiographs were evaluated for evidence of loosening. Survivorship was calculated with an endpoint of revision for aseptic loosening or radiographic evidence of loosening.
Results
Mean HHS improved from a mean of 50 pre-operatively to 91 (p < 0.001) postoperatively. Mean pain score was 1, mean patient satisfaction was 9 and mean UCLA score was 6. Two acetabular components were revised for aseptic loosening; no stem required revision. Radiographically, no cases had evidence of loosening. Survivorship was 96.8 % for the acetabular component and 100 % for the stem at ten years. Three patients died from unrelated causes, and five were lost to follow-up.
Conclusions
Bone-preserving hip replacement has increased in popularity as hip replacement in younger and more active individuals increases. The CFP prosthesis has excellent midterm clinical function and survival and provides high levels of satisfaction in young patients.
Keywords: Hip replacement, Uncemented, Coated, Preserving, Short stem, Midterm
Introduction
As hip replacement in younger and more active individuals increases, surgeons are striving to improve longevity and success of their results while making any future revision surgery less complex. With the withdrawal of large metal-on-metal (MoM) total hip replacements (THR) from clinical use [1] and the numbers of hip resurfacings being reduced [2] in response to concerns of adverse reaction to metal debris (ARMD) [3], orthopaedic surgeons are seeing an increase in alternative prostheses, such as bone-preserving, shorter-stemmed THR implants, being promoted for young and active patients. As is usual with new technologies, there has been a large influx of short-stemmed hip replacements into the market, some with as little as a limited three year follow-up available [4, 5]. The collum femoris preserving (CFP) THR (Waldemar LINK GmbH & Co, Hamburg, Germany) consists of a short-stemmed femoral component and an acetabular component with a contoured inferior rim. The system was specifically designed with the biologically young and active patient in mind with regard to biomechanical loading, fixation principles and retention of normal anatomy [6–8]. Pipino et al. published results from his designer series regarding the success and longevity of the prosthesis [6, 9]. Since its introduction, there have been some design modifications, with the current iteration introduced from the mid-1980s [6]. To date, there have been a number of short-term follow-up studies but no published long-term outcomes outside of the designer centre.
In our unit, the CFP hip was trialled 12 years ago as a single-surgeon cohort series. The study was a prospective evaluation of results of the CFP THR in an attempt to replicate published data. The senior author had reservations over the introduction of hip-resurfacing replacements, with primary concerns surrounding the unevaluated risk of femoral-neck fracture, along with other concerns in view of the failures of MoM implants historically [10, 11]. These opinions have now gained considerable traction [3, 12]. As such, joint registries and close clinical follow-up of newer devices is necessary to avoid the problems of the past and present and hopefully reveal such problems before results have catastrophic consequences for patients. We previously published short-term results (1–5 years) [13] and here present the 10-year results of our prospective cohort.
Materials and methods
From 2001 to 2003, 75 patients were prospectively enrolled, and informed consent was obtained from all patients. The prosthesis used was fully approved within the UK at the time of implantation as a THR for the indication of painful hip arthritis. Inclusion criteria were those under the age of 65 years undergoing a primary procedure with minimal bone loss. Exclusion criteria were osteoporosis, severe dysplasia, previous femoral-neck fracture and severe joint contractures.
The CFP is a collared, short-stemmed THR made of Tilastan® [titanium, 6 aluminum, 4 vanadium (Ti-6Al-4VA)] (Fig. 1). The proximal two thirds are coated with a proprietary calcium phosphate coating (HX®, DOT, Rostock, Germany) 25 ± 10-μm thick with a 70-μm pore size applied electrochemically. The stem is designed as a left or right version, with 14° of neck anteversion built in and two anatomic curvatures and three stem sizes available. The stem has an elliptical collar allowing preservation and loading of the femoral neck. The trabecular oriented pattern (TOP) cup is hemispherical and formed from the same titanium alloy and proprietary coating. It has circular segmental rows of teeth and the option for supplemental screw fixation. There is a medioventral recess to allow greater range of motion (ROM) and to reduce psoas irritation (Fig. 2). All patients underwent pre-operative radiographs with templating to determine the correct implant size and curvature. All operations were performed by the senior author in laminar-flow theatres with the patient in the lateral decubitus position. A posterior approach was used with a transosseous capsular repair in all cases. Patients were encouraged to begin full weight bearing from day one postoperatively.
Fig. 1.

Collum femoris preserving (CFP) stem
Fig. 2.
Colum femoris preserving (CFP) cup with its medioventral recess
Sixty-nine patients underwent a total of 75 consecutive THRs (33 men and 36 women). The main indication for surgery was for osteoarthritis (77 %); other indications were rheumatoid arthritis (11 %), avascular necrosis of the femoral head (4 %), slipped upper-femoral epiphysis (3 %), Perthes disease (3 %), developmental dysplasia of the hip (1 %) and psoriatic arthritis (1 %). Average patient age at the time of surgery was 52 (range 13–69) years. A 28-mm femoral head was used in all cases. The bearing surface was ceramic on ultra-high-molecular-weight polyethylene (UHMWPE), except in one case in which the head was metal in order to achieve an extended offset.
All patients underwent clinical assessment pre- and postoperatively with the Harris Hip Score (HHS) [14]. At the latest review point, further evaluation was performed using pain and satisfaction visual analogue scales (VAS), and patients rated their activity level using the University of California, Los Angeles (UCLA) activity score [15]. Quality of life (QoL) was assessed with the EuroQol (EQ)-5D questionnaire.
Standard anteroposterior (AP) and lateral pelvic radiographs were assessed for lucency using Gruen zones [16] for the femoral component and DeLee and Charnley zones [17] for the acetabulum. Acetabular inclination, femoral component implantation angles and subsidence were recorded. Component stability and fixation were assessed according to Engh’s criteria [18], which scores for the presence and extent of lucent lines, stem fixation with spot welds and pedestals, additional cortical hypertrophy and calcar remodeling. Higher scores represent greater stability and fixation (Table 1).
Table 1.
Engh’s stability score
| Undetermined | ||||
|---|---|---|---|---|
| Fixation scale | Appearance of porous interface (lines/lucencies) | Extensive ≥50 % | 0 | None |
| −5.0 | +5.0 | |||
| Spot welds | Absent | 0 | Present | |
| −2.5 | +5.0 | |||
| Fixation score: | ||||
| Stability scale | Appearance of smooth interface (lines/lucencies) | Extensive ≥50 % | 0 | None |
| −3.5 | +5.0 | |||
| Pedestal when end is unfixed | Present | 0 | Absent | |
| −3.5 | +2.5 | |||
| Calcar modeling | Hypertrophy | 0 | Atrophy | |
| −4.0 | +3.0 | |||
| Interface deterioration (lines/lucencies) | Present | 0 | Absent | |
| −2.5 | +2.5 | |||
| Migration | Present | 0 | Absent | |
| −5.0 | +3.0 | |||
| Particle shedding | Present | 0 | None | |
| −5.0 | +1.0 | |||
| Stability score: | ||||
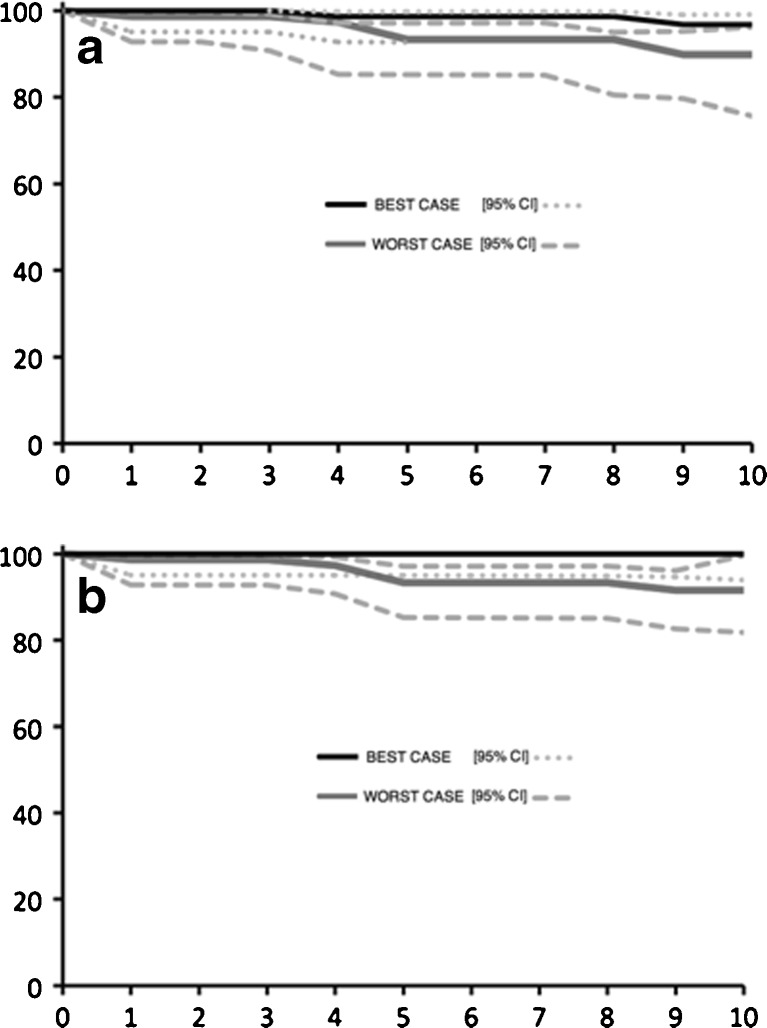
Survivorship of acetabular and femoral components was evaluated using the life table method, with 95 % confidence intervals (CI) calculated using the Rothman equation [19]. Endpoints were revision for aseptic loosening or radiographic evidence of loosening. Survivorship curves were constructed for best- and worst-case scenarios. In the latter, all cases lost to follow-up are assumed to have failed immediately after their last known follow-up date.
Results
The mean follow-up at the latest review was 9.3 years (range 7.4–10.5). Of the 75 hips initially enrolled, five were lost to follow-up and three patients had died of unrelated causes, leaving 67 hips for assessment. Of the patients lost to follow-up, one had left the country and four had left the area, with no contact details available from their general practitioner or previous employers.
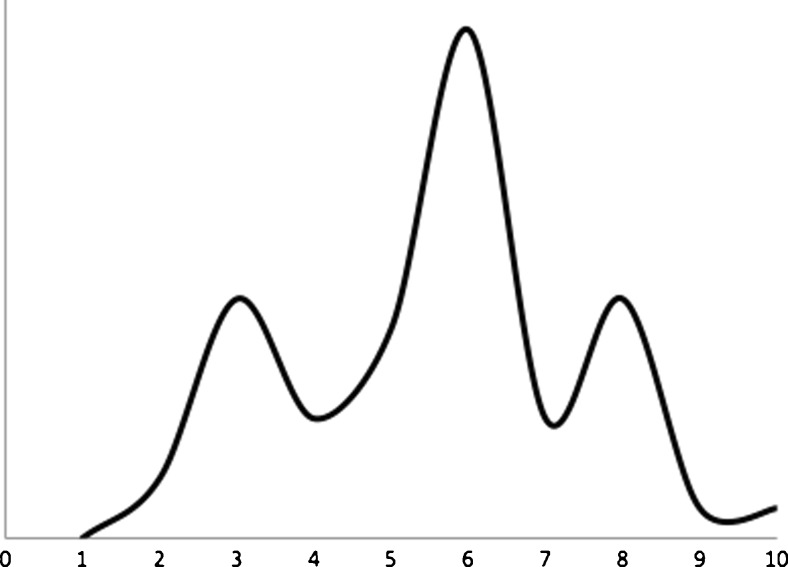
Substantial and sustained improvements were seen in patients’ HHS; using a two-sample paired Student’s t test, results show a statistically significant improvement from a mean of 50 [range 27–77; standard deviation (SD) 12.5] pre-operatively to 91(49–100; SD 12.35) at the latest review (p < 0.0001).;85 % (57/67) reported good to excellent results (HHS >80) [20]. The mean UCLA score was 6 (range 2–10; SD 1.82) (Fig. 3), with 75 % indicating the patient could do unlimited housework and shopping or were participating in some degree of sporting activity. On a scale of 0–10 (10 being completely satisfied), patient satisfaction had a mean score of 9 (0–10, SD 2.11), with 86 % scoring ≥8. The mean pain score on a scale of 0–10 (0 being no pain) was 1.1 (0–7.5, SD 1.7), with 88 % scoring ≤2. The mean EQ-5D score was 0.84 (0.1–1, SD 0.216), with a mean EQ-5D VAS of 90.8.
Fig. 3.
University of California Los Angeles (UCLA) score distribution. X axis UCLA score; Y axis frequency
Radiographic analysis had revealed no significant changes over the last five years [13]. There was no evidence of any loose components or substantial osteolysis. There was no further femoral stem subsidence, with four cases (11 %) showing subsidence that stabilised. The mean acetabular inclination angle was 46° (range 35–63°), with no evidence of movement. There was no evidence of any eccentric polyethylene wear of the acetabular insert.
With regards to Engh’s [18] assessment for stability and fixation, there was no significant change. The mean fixation score was 7 (range 0–10) compared with 5.8 at five years. The mean stability score was 12 (range −4 to 17) compared with 10.8 at 5 years. This resulted in an overall mean score of 19 (range 1–27) compared with 16 at five years, which corresponds to stable, well-fixed stems with good bony ingrowth. Two acetabular components were revised, both for aseptic loosening, at 41 and 94 months, respectively. At revision surgery, both hips had a stable femoral component that was not revised. There were two cases of infection: One was superficial in the initial postoperative period and resolved with antibiotics and no long-term concerns. The second had a confirmed, low-grade, deep infection but the patient declined further surgery for the present in view of comorbidities and acceptable functional status. This patient is receiving long-term antibiotic suppression. Two patients had a single, early dislocation (2.7 %) within the first year, one in the immediate postoperative period and the second after a fall. Both were reduced and examined under anaesthesia and found to be stable. Neither patient had any further orthopaedic intervention or reported further problems thus far. One patient experienced a lateral femoral-wall fracture that was undisplaced and healed with nonoperative management with reduced weight bearing for six weeks. This patient was doing very well at ten years, with HHS of 100 and stable implant on radiographs (Figs. 4, 5 and 6).
Fig. 4.

Immediate postoperative anteroposterior (AP) radiograph, showing a periprosthetic fracture of the femur
Fig. 5.

Eight months’ postoperative anteroposterior (AP) radiograph of the same periprosthetic fracture as in Fig. 4. The patient was asymptomatic by this stage
Fig. 6.

Same patient as in Fig. 4 at 10 years’ follow-up
At ten years, the effective number of hips at risk was 60 and by 11 years 35. Cup survival was 96.8 % (95 % CI 85–99) at ten years, falling to 89.8 % (95 % CI 76–96) in a worst-case scenario. For the stem, ten year survival was 100 % (95 % CI 94–100) in a best-case scenario and 91.6 % (95 % CI 82–99) in a worst-case scenario. (Fig. 7).
Fig. 7.
Survival curves for the cup (a) and stem (b)
Discussion
Of patients undergoing hip replacement surgery in the UK today, 35 % are <65 [2]; this figure is close to 50 % in the United States [21]. As the baby boom generation ages, the requirement for THR will increase [22]. As this trend continues, patients will ask more of their THR, and inevitably, more patients will need revision surgery. The current revision burden in the UK is approximately 8,000, according to the 2010 UK National Joint Registry, and is expected to be >50,000 in the US by 2016; again, these figures are increasing annually [22]. In such a situation, two things are required from the prosthesis. Firstly, they should provide a maximal longevity and function, which we expect to achieve through implant engineering and meticulous surgical technique. Secondly, the implants must allow future revision surgery to be as straightforward as possible. One available option to facilitate these requirements is the implantation of devices that preserve bone stock at the initial surgery, such as allowed when using the CFP. There has been a design progression from metaphyseal-loading implants to neck-loading implants, with the intention of loading the femur more proximally in order to mimic natural biomechanics and prevent stress shielding of the metaphysis, thus leaving healthy bone stock for the future, if necessary. This requirement is well demonstrated with use of the CFP prosthesis [6–8].
There are limitations of this study: there is no control group, and complete follow-up was not attained. The potential effect of the latter problem is demonstrated in our survival analysis. We felt multiple outcome measures would give a better indication of patients’ level of function, but we had no pre-operative record of all scores used. Also, the study sample was quite small.
There is little published literature on the long-term survival of the short, neck-preserving femoral stems. Also, little is known about the functional status that young, active patients achieve with such implants and whether the implants will prove to be a good option in the long term. A recent study looking at worldwide hip registries showed a significant variation in the use of THRs in young patients, as well as variation in revision rates and survival of each age group [23]. At the time of writing, 12 other implants with a short stem option were identified. These include the MiniHip® (Corin®); Balance Microplasty® and TaperLoc® Microplasty (Biomet®); Proxima® and the Silent Hip® (Depuy®); CUT® femoral neck (Orthodynamics®); SMF® Hip system (Smith and Nephew®); the Fitmore®; and the Mayo Conservative Hip (Zimmer®). This list is not exhaustive and likely out of date by the time of publication. Only two of those named here—the Mayo Conservative and the CFP—have any published peer-reviewed results with greater than ten years of follow-up confirming they are comparable with more conventional THRs [9, 24–26]. In fact, some of these short-stem hip replacements have also shown some worryingly high rates of early revision—up to 11 % at five years—emphasising the importance of reliable clinical follow-up of these implants and surgical techniques [27, 28].
We prospectively evaluated the outcomes of a cohort of 75 patients who underwent THR with a CFP, demonstrating good clinical outcomes with high levels of patient satisfaction and implant survival at a level consistent with all acceptable and long-lasting hip replacement systems currently available [2, 26, 29, 30]. Although there are publications that highlight the potential for proximal bone loss with neck-preserving prostheses [24, 31, 32], our radiographic analysis shows little subsidence and consistent preservation of metaphyseal bone, along with good osseointegration of both the femoral and acetabular components. As shown in previous studies [24, 31, 32], remodelling and further bone growth appears around the diaphysis near the level of the distal tip of the implant. The majority of our cohort is high functioning, happy with their prosthesis and pain free with well-preserved femoral bone stock for the future. Only longer-term follow-up will reveal the true success of this implant, and we continue to keep this young cohort of patients under review.
References
- 1.Medicines and Healthcare products Regulatory Agency (MHRA) www.mhra.gov.u. (2012) Press release: MHRA updates advice for metal-on-metal hip replacements. Available at: http://www.mhra.gov.uk/NewsCentre/Pressreleases/CON143784. Accessed March 12 2013
- 2.The National Joint Registry for England and Wales 2011 8th Annual Report. Available at: http://www.njrcentre.org.uk/NjrCentre/Portals/0/Documents/NJR%208th%20Annual%20Report%202011.pdf
- 3.Langton DJ, Joyce TJ, Jameson SS, et al. Adverse reaction to metal debris following hip resurfacing: The influence of component type, orientation and volumetric wear. J Bone Joint Surg Br. 2011;93(2):164–171. doi: 10.1302/0301-620X.93B2.25099. [DOI] [PubMed] [Google Scholar]
- 4.Ghera S, Pavan L. The DePuy Proxima hip: A short stem for total hip arthroplasty. Early experience and technical considerations. Hip Int. 2009;19(3):215–220. doi: 10.1177/112070000901900305. [DOI] [PubMed] [Google Scholar]
- 5.Schmidutz F, Grote S, Pietschmann M, et al. Sports activity after short-stem hip arthroplasty. Am J Sports Med. 2012;40(2):425–432. doi: 10.1177/0363546511424386. [DOI] [PubMed] [Google Scholar]
- 6.Pipino F, Molfetta L. Femoral neck preservation in total hip replacement. Ital J Orthop Traumatol. 1993;19(1):5–12. [PubMed] [Google Scholar]
- 7.Biggi F, Franchin F, Lovato R, Pipino F. DEXA evaluation of total hip arthroplasty with neck-preserving technique: 4-year follow-up. J Orthop Traumatol. 2004;5(3):156–159. doi: 10.1007/s10195-004-0063-4. [DOI] [Google Scholar]
- 8.Carlson L, Albrektsson B, Freeman MA. Femoral neck retention in hip arthroplasty. A cadaver study of mechanical effects. Acta Orthop Scand. 1988;59(1):6–8. doi: 10.3109/17453678809149333. [DOI] [PubMed] [Google Scholar]
- 9.Pipino F, Molfetta L, Grandizio M. Preservation of the femoral neck in hip arthroplasty: Results of a 13-to 17-year follow-up. J Orthop Traumatol. 2000;1(1):31–39. doi: 10.1007/s101950070026. [DOI] [Google Scholar]
- 10.Jantsch S, Schwägerl W, Zenz P, Semlitsch M, Fertschak W. Long-term results after implantation of McKee-Farrar total hip prostheses. Arch Orthop Trauma Surg. 1991;110(5):230–237. doi: 10.1007/BF00572878. [DOI] [PubMed] [Google Scholar]
- 11.Dobbs HS. Survivorship of total hip replacements. J Bone Joint Surg Br. 1980;62-B(2):168–173. doi: 10.1302/0301-620X.62B2.7364829. [DOI] [PubMed] [Google Scholar]
- 12.Chana R, Esposito C, Campbell PA, Walter WK, Walter WL. Mixing and matching causing taper wear: Corrosion associated with pseudotumour formation. J Bone Joint Surg Br. 2012;94(2):281–286. doi: 10.1302/0301-620X.94B2.27247. [DOI] [PubMed] [Google Scholar]
- 13.Gill IR, Gill K, Jayasekera N, Miller J. Medium term results of the collum femoris preserving hydroxyapatite coated total hip replacement. Hip Int. 2008;18(2):75–80. doi: 10.1177/112070000801800202. [DOI] [PubMed] [Google Scholar]
- 14.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755. [PubMed] [Google Scholar]
- 15.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13(8):890–895. doi: 10.1016/S0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]
- 16.Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: A radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 17.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 18.Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990;257:107–128. [PubMed] [Google Scholar]
- 19.Rothman KJ. Estimation of confidence limits for the cumulative probability of survival in life table analysis. J Chronic Dis. 1978;31(8):557–560. doi: 10.1016/0021-9681(78)90043-7. [DOI] [PubMed] [Google Scholar]
- 20.Marchetti P, Binazzi R, Vaccari V, et al. Long-term results with cementless Fitek (or Fitmore) cups. J Arthroplasty. 2005;20(6):730–737. doi: 10.1016/j.arth.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 21.FASTSTATS - Inpatient Surgery. Available at: http://www.cdc.gov/nchs/fastats/insurg.htm. Accessed May 18, 2012
- 22.Iorio R, Robb WJ, Healy WL, et al. Orthopaedic surgeon workforce and volume assessment for total hip and knee replacement in the United States: Preparing for an epidemic. J Bone Joint Surg. 2008;90(7):1598–1605. doi: 10.2106/JBJS.H.00067. [DOI] [PubMed] [Google Scholar]
- 23.Sadoghi P, Schröder C, Fottner A, Steinbrück A, Betz O, Müller PE, Jansson V, Hölzer A. Application and survival curve of total hip arthroplasties: A systematic comparative analysis using worldwide hip arthroplasty registers. Int Orthop Nov. 2012;36(11):2197–203. doi: 10.1007/s00264-012-1614-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Briem D, Schneider M, Bogner N, et al. Midterm results of 155 patients treated with a collum femoris preserving (CFP) short stem prosthesis. Int Orthop. 2011;35(5):655–660. doi: 10.1007/s00264-010-1020-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morrey BF, Adams RA, Kessler M. A conservative femoral replacement for total hip arthroplasty a prospective study. J Bone Joint Surg Br. 2000;82-B(7):952–958. doi: 10.1302/0301-620X.82B7.10420. [DOI] [PubMed] [Google Scholar]
- 26.Bojescul JA, Xenos JS, Callaghan JJ, Savory CG. Results of porous-coated anatomic total hip arthroplasty without cement at fifteen years: A concise follow-up of a previous report. J Bone Joint Surg Am. 2003;85-A(6):1079–1083. doi: 10.2106/00004623-200306000-00015. [DOI] [PubMed] [Google Scholar]
- 27.Ender SA, Machner A, Pap G, Hubbe J, Grashoff H, Neumann H-W. Cementless CUT femoral neck prosthesis: Increased rate of aseptic loosening after 5 years. Acta Orthop. 2007;78(5):616–621. doi: 10.1080/17453670710014301. [DOI] [PubMed] [Google Scholar]
- 28.Gilbert RE, Salehi-Bird S, Gallacher PD, Shaylor P. The mayo conservative hip: Experience from a district general hospital. Hip Int. 2009;19(3):211–214. doi: 10.1177/112070000901900304. [DOI] [PubMed] [Google Scholar]
- 29.Ling RSM, Charity J, Lee AJC, Whitehouse SL, Timperley AJ, Gie GA. The long-term results of the original Exeter polished cemented femoral component: A follow-up report. J Arthroplasty. 2009;24(4):511–517. doi: 10.1016/j.arth.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 30.Vidalain J-P. Twenty-year results of the cementless Corail stem. Int Orthop. 2011;35(2):189–194. doi: 10.1007/s00264-010-1117-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kress AM, Schmidt R, Nowak TE, Nowak M, Haeberle L, Forst R, Mueller LA. Stress-related femoral cortical and cancellous bone density loss after collum femoris preserving uncemented total hip arthroplasty: a prospective 7-year follow-up with quantitative computed tomography. Arch Orthop Trauma Surg. 2012;132(8):1111–1119. doi: 10.1007/s00402-012-1537-0. [DOI] [PubMed] [Google Scholar]
- 32.Nowak M, Nowak TE, Schmidt R, Forst R, Kress AM, Mueller LA. Prospective study of a cementless total hip arthroplasty with a collum femoris preserving stem and a trabeculae oriented pressfit cup: Minimun 6-year follow-up. Arch Orthop Trauma Surg. 2011;131(4):549–555. doi: 10.1007/s00402-010-1189-x. [DOI] [PubMed] [Google Scholar]