Abstract
Background
An adequate door-to-balloon time (<120 minutes) is the necessary condition for the efficacy of primary angioplasty in infarction to translate into effectiveness.
Objective
To describe the effectiveness of a quality of care protocol in reducing the door-to-balloon time.
Methods
Between May 2010 and August 2012, all individuals undergoing primary angioplasty in our hospital were analyzed. The door time was electronically recorded at the moment the patient took a number to be evaluated in the emergency room, which occurred prior to filling the check-in forms and to the triage. The balloon time was defined as the beginning of artery opening (introduction of the first device). The first 5 months of monitoring corresponded to the period of pre-implementation of the protocol. The protocol comprised the definition of a flowchart of actions from patient arrival at the hospital, the team's awareness raising in relation to the prioritization of time, and provision of a periodic feedback on the results and possible inadequacies.
Results
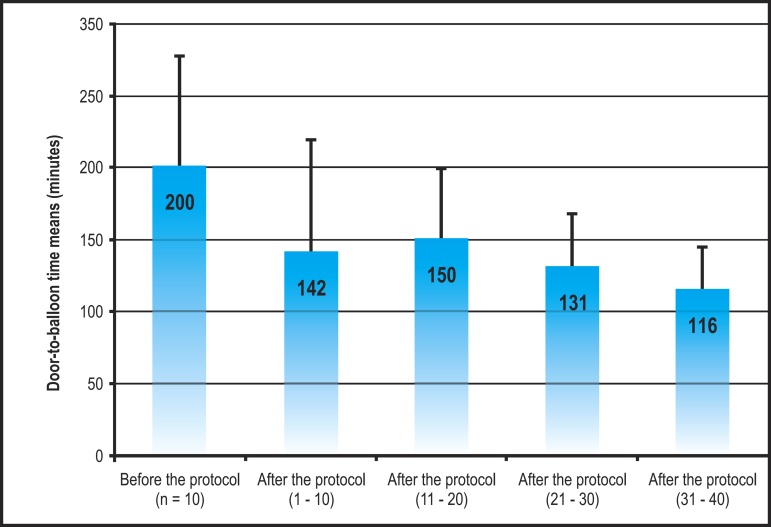
A total of 50 individuals were assessed. They were divided into five groups of 10 sequential patients (one group pre-and four groups post-protocol). The door-to-balloon time regarding the 10 cases recorded before protocol implementation was 200 ± 77 minutes. After protocol implementation, there was a progressive reduction of the door-to-balloon time to 142 ± 78 minutes in the first 10 patients, then to 150 ± 50 minutes, 131 ± 37 minutes and, finally, 116 ± 29 minutes in the three sequential groups of 10 patients, respectively. Linear regression between sequential patients and the door-to-balloon time (r = - 0.41) showed a regression coefficient of - 1.74 minutes.
Conclusion
The protocol implementation proved effective in the reduction of the door-to-balloon time.
Keywords: Angioplasty Balloon, coronary / methods; Myocardial Infarction / physiopathology; Acute Coronary Syndrome, Patient Care Planning
Introduction
Several health services in Brazil prefer to adopt primary angioplasty instead of chemical thrombolysis as the reperfusion treatment of patients with ST-segment elevation myocardial infarction (STEMI)1. The choice of an approach that has a more complex logistics is based on a series of clinical studies suggesting that angioplasty is a more efficient strategy than thrombolysis2. However, the effectiveness of angioplasty depends on a rapid initiation of therapy, defined as an interval between patient arrival at the hospital and the beginning of angioplasty (door-to-balloon time) < 120 minutes3. The concept that the effectiveness of primary angioplasty depends on this important parameter seems not to be widespread in Brazil. This statement is based on the systematic preference for primary angioplasty over chemical thrombolysis, despite the absence of studies showing the door-to-balloon time in our midst, or studies assessing the application of strategies to ensure this quality parameter.
As a measure for monitoring the quality of care, the door-to-balloon time of our patients started to be measured in a systematic, prospective and rigorous manner as from 2010. After the first 10 cases, the inadequacy of outcomes was noted, and this encouraged the creation of an evidence-based protocol aiming at improving the door-to-balloon time. The present study reports the practical impact (effectiveness) of this protocol on time parameters throughout the 22 months of follow-up after its implementation. Additionally, multivariate analysis was carried out to identify potential determinants of this quality of care parameter.
Methods
Patient selection
Between May 2010 and August 2012, patients consecutively admitted in our hospital in the acute phase of STEMI who would undergo primary angioplasty were included in the protocol. This strategy represents the preferred reperfusion method in our service. The diagnosis was made at the moment of patient admission in the emergency service, based on the joint opinion of two physicians - the emergency medicine physician and the cardiologist of the coronary unit where the patient would further be transferred to. The clinical criterion of typical chest discomfort for less than 12 hours associated with persistent ST-segment elevation ≥ 0.1 mV (not reversible with nitrate) in two contiguous leads was the main diagnostic parameter. However, the final approach was left at the discretion of the physicians, according to their clinical impression. In the presence of complete left bundle branch block, the diagnosis was mainly based on the patient's symptoms. The only pre-defined exclusion criterion of this study was patient refusal to participate in this registry, which did not happen in any case.
The study patients took part of our hospital's Acute Coronary Syndromes Registry (Registro de Síndromes Coronarianas Agudas - RESCA), for which they gave written informed consent. This registry was approved by the Institutional Research Ethics Committee, and is in accordance with Resolution 196/96 of the Ministry of Health. One of its pre-defined objectives was to measure the door-to-balloon time.
Endpoints analyzed
The endpoints were defined before the protocol was carried out, and were prospectively measured during patient's care. The primary endpoint chosen was the door-to-balloon time, which was described as a numeric variable. The proportion of patients with an adequate door-to-balloon time (< 120 minutes) was recorded as a secondary endpoint. These definitions are in accordance with performance guidelines in the treatment of STEMI4-6.
The door-to-balloon time was defined as the period of time elapsed between patient arrival at the hospital and the beginning of the mechanical reperfusion procedure. The door time is characterized by the patient arrival at the hospital, signaled by the moment they took a number to be evaluated (before the patient is checked-in in that hospital area), which is automatically recorded by the information system. The balloon time refers to the beginning of the reperfusion procedure, defined by the percutaneous insertion of any device with therapeutic purposes. Usually, this first device is the angioplasty guide catheter. Thus, the balloon time is not recorded at the beginning of the diagnostic procedure of coronary angiography, but rather at the beginning of the therapeutic procedure.
Also, as secondary endpoints, the following components of the door-to-balloon time were defined: door-to-diagnosis time, which starts at the moment of patient arrival at the emergency service and ends at the moment the need for a primary coronary intervention is diagnosed; and diagnosis-to-balloon time, which elapses between the diagnostic definition and the beginning of the therapeutic procedure. The first component characterizes the identification of a patient eligible for the procedure, and the second component characterizes patient preparation and activation of the interventional cardiology team.
Chest pain protocol flowchart
The protocol was performed by three different hospital areas: the emergency area, in charge of the identification and diagnosis; the coronary unit, in charge of patient preparation for the procedure and activation of the interventional cardiology team; and the interventional cardiology area, in charge of the performance of the mechanical reperfusion procedure.
The protocol starts with the identification of a potential infarction case at the emergency door, which is made by the management employee at the front desk. These employees were trained to identify chest pain or equivalent, from the patient's complaint or their subjective perception. Once a potential eligible patient is identified, the employee refers the patient for priority care delivered by the triage nurse. This nurse performs an electrocardiogram, even before medical evaluation. The electrocardiogram is immediately sent to an emergency medicine physician, who examines the patient and discusses the case with the coronary unit cardiologist. Once defined that it is an ongoing case of STEMI, the coronary unit team takes charge of the time management. The unit's nurse starts counting with the interventional cardiology team, and immediately refers the patient to the catheterization laboratory, where he will be prepared for the procedure. In this area, the patient is placed on the procedure bed and shaving, asepsis and placement of surgical sheets are carried out. Simultaneously, oral acetylsalicylic acid 200 mg and thienopyridine derivatives (clopidogrel 300 mg, in years 2010 and 2011, then replaced for ticagrelor 180 mg, in 2012) are administered. At this moment, the objective is that the patient be ready to undergo the procedure as soon as the interventional cardiology team arrives; this team comprises a physician, a nursing technician, and a radiology technician. The procedure should start immediately after team arrival. This team is on site during office hours (7 am to 5 pm) and on call during night shifts or weekends. In the first situation, the team will be ready during patient preparation. The goals to be achieved during patient care are a door-to-diagnosis time no longer than 30 minutes and diagnosis-to-balloon time no longer than 90 minutes.
Measures implemented for time optimization
In addition to the definition of the patient care flowchart described here, specific measures were used to reduce the door-to-balloon time, based on effectiveness studies7,8, which define predictors of a protocol success, or on peculiarities of our hospital: (1) training of the emergency service front-desk employees for the identification of potential patients eligible to the protocol; (2) empowerment of the triage nurse to perform an electrocardiogram without a medical request form; (3) activation of the interventional cardiology team by the physician who diagnoses infarction; (4) activation of the stopwatch at the moment of diagnosis, so that the patient will be ready for the procedure to start within 40 minutes at most; (5) awareness raising of the interventional cardiologist to arrive quickly at the hospital and perform the procedure while paying attention to timing; (6) awareness raising of all the hospital multidisciplinary team for the importance of the door-to-balloon time; (7) definition of this protocol as being the hospital's main quality of care protocol; (8) feedback on each patient's door-to-balloon time, by displaying posters showing the "last door-to-balloon time" in minutes, in all areas involved; (9) monthly meetings of the teams involved in order to discuss all cases included in the protocol, occasional flaws and improvement strategies.
Data analysis
The first five months of monitoring (May to September 2010) corresponded to the period of protocol pre-implementation, whereas the subsequent months corresponded to post-implementation cases (October 2010 to August 2012). Thus, the pre-protocol period, which included 10 cases, represented the reference used to evaluate whether the protocol had resulted in improvement of the door-to-balloon time. It had been previously defined that the post-protocol period would be divided into subperiods of 10 consecutive cases each, in order to evaluate the evolution of the door-to-balloon time. Since the patients analyzed correspond to the whole population universe of patients seen in this period, the comparison of times was merely descriptive, with no need for statistical tests to estimate the type-I error probability. The door-to-balloon time of each period was described as a mean and standard deviation.
Linear regression analysis was also carried out, considering each patient's door-to-balloon time as a dependent variable and the time sequence of patients as an independent variable. The beta (β) regression coefficient was used to estimate the variation of door-to-balloon time at each sequential patient. Secondarily, the proportions of satisfactory time (< 120 minutes) were compared between the periods of 10 patients. For the same reason described in the previous paragraph, p values were not used in these analyses.
In order to analyze the factors determining the door-to-balloon time, this variable was compared between subgroups of patients divided by demographic and clinical characteristics, and circumstances of care. Although this was not a sample, the o value (< 0.20) was considered as the selection criteria for the variables to be included in the multivariate model. The analysis of covariance (ANCOVA) was the multivariate model used to determine the independent predictors of the door-to-balloon time. In this analysis, p values < 0.05 were considered significant. The Statistical Package for the Social Sciences (SPSS) software program, version 9.0 (SPSS Inc., Chicago, Illinois, USA) was used for data analysis.
Results
Sample characteristics
During the study period, 53 patients were consecutively admitted due to STEMI and indication for reperfusion. Of these, three patients underwent thrombolysis, and the remaining 50 individuals underwent primary angioplasty. These 50 patients comprised the population of the study period. Their mean age was 60 ± 13 years, with a clear predominance of the male gender (78% of the sample), and 42% of blacks or mixeds. The time elapsed between the onset of symptoms and patient arrival at the hospital was relatively long, with a median of 5 hours (interquartile interval = 1.1 - 6.0 hours). Only one patient had received prehospital treatment, which generated an advance warning of arrival of an infarct case at the hospital. Approximately half of our patients were admitted to the hospital out of business hours, when the interventional cardiology team was no longer in the area. The GRACE risk score showed a median of 139 and interquartile interval between 114 and 158, thus indicating that the sample was predominantly at an intermediary risk. Other clinical characteristics and circumstances of care are described in Table 1.
Table 1.
Population characteristics
| Variables | |
| Demographic data | |
| Age (years) | 60 ± 13 |
| Male gender | 39 (78%) |
| Skin color black/mixed | 21 (42%) |
| Circumstances of care | |
| Non-business hours (5pm-7am) | 24 (48%) |
| Weekends | 15 (30%) |
| Rush hour (7am-9am and 5pm-7pm) | 9 (18%) |
| History of | |
| Diabetes mellitus | 14 (28%) |
| Previous coronary artery disease | 6 (12%) |
| Presentation of infarction | |
| Time of onset of symptoms at arrival | 5.0 (1.1 - 6.0) |
| Anterior infarction | 27 (54%) |
| Magnitude of ST elevation (mm) | 3.1 (1.5 - 4.4) |
| Killip class > 1 | 6 (12%) |
| GRACE score | 139 (114 - 158) |
Influence of the care protocol in the door-to-balloon time
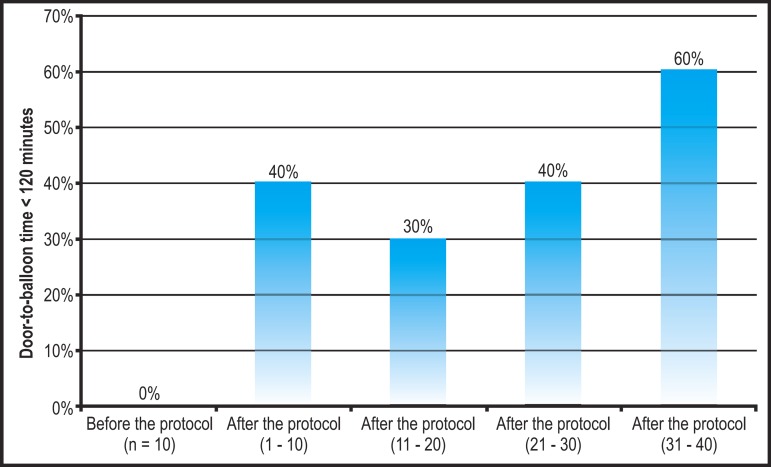
The door-to-balloon time regarding the 10 cases recorded before the protocol implementation was 200 ± 77 minutes, i.e., above the desired values. After the protocol implementation, there was a progressive reduction of the door-to-balloon time, to 142 ± 78 minutes in the first 10 patients, followed by 150 ± 50 minutes, 131 ± 37 minutes and, finally, 116 29 minutes in the three sequential periods of 10 patients, respectively (Figure 1 and Table 2). Considering the mean observed in the last period of 10 patients, in relation to the pre-protocol period, there was a reduction by 42% in the door-to-balloon time. In addition to a reduction of the mean, a progressive increase in the homogeneity of times in each period was also observed, represented by a decrease in the coefficients of variability of the door-to-balloon times (55%, 33%, 28%, and 25%, respectively, in the four periods after protocol implementation). In the period before protocol implementation, no patient showed a desired door-to-balloon time (< 120 minutes). After the protocol, 40%, 30%, 40% and, finally, 60% of patients showed a door-to-balloon time < 120 minutes, respectively, in the four sequential periods of 10 patients (Figure 2).
Figure 1.
Comparison of door-to-balloon time means at each sequential group of 10 patients, showing a progressive reduction on times after protocol implementation.
Table 2.
Evolution of the door-to-balloon time and of its two main components, according to periods relative to the implementation of a care protocol
| Times (minutes) | Pre-protocol | 1st period | 2nd period | 3rd period | 4th period | Reduction (%) |
| Door-to-balloon | 200 ± 77 | 142 ± 78 | 150 ± 50 | 131 ± 37 | 116 ± 29 | 42 |
| Door-to-diagnosis | 30 ± 6.9 | 11 ± 3.6 | 15 ± 7.1 | 10 ± 22 | 8.5 ± 2.7 | 72 |
| Diagnosis-to-balloon | 170 ± 70 | 131 ± 78 | 135 ± 41 | 109 ± 12 | 107 ± 7.9 | 37 |
Pre-protocol corresponds to the 10 patients before protocol implementation; each subsequent period corresponds to 10 sequential patients. P values were not calculated for the differences between groups, because this is a population, not a population sample.
Figure 2.
Comparison of the proportion of individuals with adequate door-to-balloon time (< 120 minutes) at each sequential group of 10 patients, showing a favorable outcome after protocol implementation.
The reduction observed in the door-to-balloon time resulted from an improved time for diagnosis (door-to-diagnosis time) and for patient preparation (diagnosis-to-balloon time). The first one was 30 ± 6.9 minutes prior to the protocol, going to 11 ± 3.6 minutes, 15 ± 7.1 minutes, 10 ± 22 minutes and 8.5 ± 2.7 minutes in the last period (a reduction by 72% observed in the last period in relation to the period prior to the protocol). The diagnosis-to-balloon time went from 170 ± 70 minutes to 131 ± 78 minutes, 135 ± 41 minutes, 109 ± 12 minutes and, finally, 107 ± 7.9 minutes (a 37% reduction), as shown in Table 2.
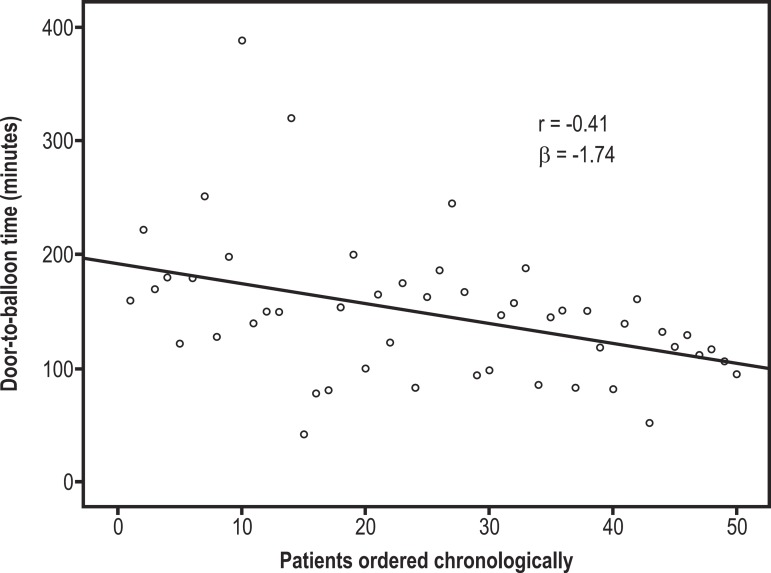
A continuous improvement of the door-to-balloon time was also observed when each patient was considered individually, in a sequential order, by linear regression analysis. This analysis demonstrated a coefficient of regression (β) of - 1.74, which corresponds to the estimate of door-to-balloon time reduction at each patient in the sequence. The linearity of this association was represented by a correlation coefficient (r) of - 0.41 (Figure 3).
Figure 3.
Linear regression analysis describing the influence of each patient in the time sequence (variable X, predictive) on the door‑to‑balloon time (variable Y, endpoint).
Determinants of the door-to-balloon time
The door-to-balloon time was compared according to the presence or absence of several clinical characteristics and circumstances of patient care. Time was significantly longer in women, when compared to men (190 ± 86 minutes versus 136 ± 49 minutes; p = 0.01); in night shifts, when compared to day shifts (174 ± 68 minutes versus 124 ± 49 minutes; p = 0.007); and on weekends, when compared to weekdays (174 ± 84 minutes versus 138 ± 49 minutes; p = 0.08), as shown in Table 3. Likewise, there was a positive correlation between the time of onset of symptoms and the door-to-balloon time (r = 0.40; p = 0.001), as shown in Table 4.
Table 3.
Association of the door-to-balloon time with patients characteristics described as dichotomous variables
| Characteristics | Door-to-balloon time (minutes) | p value* | |
| Characteristic present | Characteristic absent | ||
| Demographic data | |||
| Female gender | 190 ± 86 | 136 ± 49 | 0.01 |
| Skin color black/mixed | 48 ± 11 | 59 ± 12 | 0.58 |
| Circumstances of care | |||
| Night shift | 174 ± 68 | 124 ± 49 | 0.007 |
| Weekends | 174 ± 84 | 138 ± 49 | 0.08 |
| Rush hour | 156 ± 36 | 149 ± 70 | 0.77 |
* p value calculated using the non-paired Student t test.
Table 4.
Correlation of the door-to-balloon time with patients characteristics described as numerical variables
| Correlation coefficient (Spearman) | p value | |
| Demographic characteristics | ||
| Age | - 0.07 | 0.63 |
| Creatinine | - 0.02 | 0.89 |
| Presentation of infarction | ||
| Time of onset of symptoms | 0.45 | 0.001 |
| Magnitude of ST elevation | 0.03 | 0.87 |
| GRACE score | - 0.10 | 0.51 |
These variables were included in a multivariate analysis of covariance model, using the door-to-balloon time as a dependent variable. In this analysis, the female gender (p = 0.11) and weekends (p = 0.23) lost their predictive value, whereas night shifts (p = 0.008) and time of onset of symptoms (p = 0.002) remained as independent predictors. The coefficient of determination (R2) of the final multivariate model was 0.32.
Among the 60 patients of the total sample, 33 had a door-to-balloon time < 120 minutes. The analysis of the cause for the delay for each patient identified delayed diagnosis in 15%, delayed patient/material/team preparation in 49%, and both in 36% of the cases.
Discussion
The present study represents the first Brazilian evidence of the effectiveness of a quality of care program in improving the mechanical reperfusion time of patients admitted in the acute phase of STEMI. The protocol implementation, whose aim was to improve diagnosis time, patient preparation time, and logistic conditions of the premises, provided a significant and progressive reduction of the door-to-balloon time throughout 22 months. This improvement saved 84 minutes in the mean door-to-balloon time, taking the present study population out of a level in which the effectiveness of the reperfusion strategy was questionable.
In health centers in which a catheterization laboratory is available, primary angioplasty has been adopted as the preferred reperfusion strategy since the 1990's, based on clinical studies demonstrating a modest superiority of this approach, in comparison to thrombolysis, in the prevention of death in patients with STEMI2,9. Meta-regression analyses of these studies indicated that this superiority depended on the performance of primary angioplasty within a short period of time from patient arrival3,10. In the mid-2000's, data from the National Registry of Myocardial Infarction in the United States showed that the door-to-balloon time was unsatisfactory in most of the health centers in that country11. From this finding, the campaign Door-to-Balloon: an Alliance for Quality8 was launched in 2008. In the past year, data from the national registry showed a significant improvement of the door-to-balloon time in the United States, reaching a mean of approximately 60 minutes12. Likewise, studies from specific health centers compared the door-to-balloon time before and after protocol implementation, showing the effectiveness of this approach in time reduction13,14. Unlike the American emphasis on this issue, in Brazil there are no data published on the door-to-balloon time or studies demonstrating the effectiveness of specific protocols. This study represents the first Brazilian evidence that a protocol was effective in reducing the door-to-balloon time substantially.
The measures adopted in the Alliance for Quality campaign were based on a seminal study, which analyzed 365 hospitals, and on multivariate analysis, which identified five independent predictors of a better performance in the door-to-balloon time that apply to patients not previously treated by emergency medical services: having emergency medicine physicians activate the catheterization laboratory; having a single phone call to a central page operator to activate the laboratory; having a time goal for arrival of the interventional team at the hospital; having an attending cardiologist always on site; having all staff members use feedback data on the door-to-balloon time of each case7. The present protocol incorporated all these measures, except for the use of a central operator to activate the team, due to logistic difficulties. Also, additional measures were implemented aiming at a prompt diagnosis, such as the training of receptionists and performance of electrocardiogram by the nurse, without the need for a medical request. Finally, the purpose of the use of a stopwatch was to emphasize the importance of a quick patient preparation to have the procedure started. Thus, the elaboration of the protocol included a combination of strategies proved effective, with intuitive measures related to our real-life conditions.
A substantial reduction of the mean door-to-balloon time was observed from the first 10 cases, thus indicating that the non-systematization of the process had a great negative impact on quality, which was not subjectively perceived. On the other hand, after an initial improvement, there was stagnation in the two following periods, and an optimal time was achieved only in the period corresponding to the last 10 patients. The last improvement observed probably resulted from a continuous awareness of the team and joint discussions of each new case, focusing on flaws that could be corrected. Thus, the present study demonstrates that achieving an optimal time is a challenge to be met progressively. It should be pointed out that the time reduction observed was a result both from the reduction in diagnosis time, and in the time between diagnosis and the procedure, thus indicating that both components are sensitive to the protocol implementation.
In addition to describing the impact of the care protocol, multivariate analysis was used to identify possible determinants of the door-to-balloon time. Several clinical characteristics and circumstances of care were analyzed, and two independent predictors were identified: the moment of treatment (day or night) and the time of onset of symptoms. The absence of an association with predictors of severity suggests that physicians are aware of the importance of time, regardless of the patient's characteristics. The fact that the main determinant was the time of treatment indicates that the logistic issue preponderates. Secondly, there was an association with time of onset of symptoms; thus, it can be presumed that the shortest the onset of symptoms, the more motivated is the team to quickly take action. Although this seems natural, it may be a sign that, in patients with a longer duration of symptoms, the motivation is below the desired. This suggests the need for measures aiming at determining maximum motivation, regardless of how short is the duration of symptoms.
In addition to the effectiveness result of the protocol applied, the value of this study becomes evident from the baseline measurements of the door-to-balloon time. In the hospital where the present study was carried out, it was believed that a high-standard care was delivered. However, there was surprise when the time was measured systematically. The mean of 200 ± 77 minutes reflected a reality previously unnoticed, which led to the conclusion that the subjective notion of quality is not accurate, and systematic time measurements are necessary.
The mean door-to-balloon time recorded in the present study before and after the protocol is high above that described in American registries12-14. We should point out that, at least in part, the results of this study derive from a more strict method of time measuring, which was used to prevent underestimation of this variable. First, there was no case selection, with all consecutive patients undergoing primary angioplasty being included. In American registries, the hospitals may exclude cases for which a long door-to-balloon time is justified12 and, in fact, the frequency of these cases has increased in the past few years15. Second, these measurements were taken prospectively during the procedure, thus preventing a measurement bias, which can occur when these time data are retrieved from medical record review. Special attention was also paid to define a realistic door-to-balloon time. The main risk of underestimating time lies in defining the door time as the moment of patient check-in in the emergency service (or diagnosis time), when a time lapse between the patient arrival at the hospital and patient check-in is known to exist. For this reason, we sought to make an electronic record of the moment at which the patients enter the waiting room (when they take a number to be evaluated), even before the receptionist starts their check-in procedures. The second potential error in the time estimate is to consider the beginning of the intervention procedure as the balloon time. We took care to consider this moment as that when the first device aimed at reperfusion is inserted.
The parameter of quality used was a door-to-balloon time < 120 minutes, which is an acceptable delay, according to the guideline of the European Society of Cardiology6, although it is above the time recommended by the American guideline (< 90 minutes)5. However, this document acknowledges that the limit of time to ensure benefit is possibly beyond the 90 minutes, as suggested by meta-regression analyses. Considering the aspects previously mentioned with respect to the more strict time measurement in this study, we chose to define a door-to-balloon time < 120 minutes as satisfactory. The Brazilian Guideline suggests time < 90 minutes after the diagnosis4, which probably represents time between 90 and 120 minutes from the moment of patient arrival at the hospital, thus indicating that we are in accordance with the Brazilian recommendation.
While this study suggests the effectiveness of a quality of care protocol in the improvement of the door-to-balloon time, we should recognize that the absence of a control group did not allow the regression toward the mean phenomenon to be ruled out as an explanation for the improvement obtained after the protocol. On the other hand, this limitation is an inherent characteristic of studies on effectiveness, which are based on the assumption that the proof of the concept that a protocol provides improved care already exists. The non-controlled and observational character of this study is common to all large international studies, which demonstrated the effect of a protocol on the reduction of the door-to-balloon time.
In Brazil, there are no statistics on door-to-balloon time monitoring or campaigns to improve this quality parameter. This makes us blind in relation to the effectiveness of primary angioplasty in our midst. This study was the first to demonstrate that the systematic measurement of the door-to-balloon time can reveal inadequacies in the process, and that the adoption of a protocol based on evidence may improve our performance. This study should serve as motivation for local and national registries on door-to-balloon time to be created, with further implementation of campaigns, should the results of the registries show the need for quality improvement.
Author contributions
Conception and design of the research: Correia LCL, Matos I, Jacobs P, Noya-Rabelo M; Acquisition of data: Brito M, Kalil F, Sabino M, Garcia G, Ferreira F, Noya-Rabelo M; Analysis and interpretation of the data: Correia LCL, Noya-Rabelo M; Statistical analysis: Correia LCL; Writing of the manuscript: Correia LCL, Noya-Rabelo M; Critical revision of the manuscript for intellectual content: Matos I, Jacobs P, Ronzoni L, Noya-Rabelo M.
Footnotes
Potential Conflict of Interest: No potential conflict of interest relevant to this article was reported.
Sources of Funding: There were no external funding sources for this study.
Study Association: This study is linked to Grupo de Pesquisa RESCA, basead in post-graduation of Escola Bahiana de Medicina.
References
- 1.Mattos LA, Sousa AG, Pinto IM, Campos Cde M, Neto, Labrunie A, Alves CR, et al. Central Nacional de Intervenções Cardiovasculares, Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista Primary coronary angioplasty in 9,434 patients during acute myocardial infarction: predictors of major in- hospital adverse events from 1996 to 2000 in Brazil. Arq Bras Cardiol. 2002;79(4):405–418. doi: 10.1590/s0066-782x2002001300008. [DOI] [PubMed] [Google Scholar]
- 2.French JK, Canborn TA, Sleeper LA. Primary coronary angioplasty versus thrombolysis for acute myocardial infarction. Lancet. 2003;361(9365):1303–1304. doi: 10.1016/S0140-6736(03)13011-5. [DOI] [PubMed] [Google Scholar]
- 3.Pinto DS, Kirtane AJ, Nallamothu BK, Murphy SA, Cohen DJ, Laham RJ, et al. Hospital delays in reperfusion for ST-elevation myocardial infarction: implications when selecting a reperfusion strategy. Circulation. 2006;114(19):2019–2025. doi: 10.1161/CIRCULATIONAHA.106.638353. [DOI] [PubMed] [Google Scholar]
- 4.Piegas LS, Feitosa G, Mattos LA, Nicolau JC, Rossi JM, Neto, Timerman A, et al. Sociedade Brasileira de Cardiologia Diretriz da Sociedade Brasileira de Cardiologia sobre tratamento do infarto agudo do miocárdio com supradesnível do segmento ST. Arq Bras Cardiol. 2009;93(6) supl.2:e179–e264. [PubMed] [Google Scholar]
- 5.Kushner FG, Hand M, Smith SC, Jr, King 3rd SB, Anderson JL, Antman EM, et al. 2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction (updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (updating the 2005 Guideline and 2007 Focused Update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2009;120(22):2271–2306. doi: 10.1161/CIRCULATIONAHA.109.192663. Erratum in: Circulation. 2010;121(12):e257. [DOI] [PubMed] [Google Scholar]
- 6.Steg PG, James SK, Atar D, Badano LP, Lundqvist CB, Borger MA, et al. The Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC) ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33(20):2569–2619. doi: 10.1093/eurheartj/ehs215. [DOI] [PubMed] [Google Scholar]
- 7.Bradley EH, Herrin J, Wang Y, Barton BA, Webster TR, Mattera JA, et al. Strategies for reducing the door-to-balloon time in acute myocardial infarction. N Engl J Med. 2006;355(22):2308–2320. doi: 10.1056/NEJMsa063117. [DOI] [PubMed] [Google Scholar]
- 8.Krumholz HM, Bradley EH, Nallamothu BK, Ting HH, Batchelor WB, Kline-Rogers E, et al. A campaign to improve the timeliness of primary percutaneous coronary intervention: Door-to-Balloon: An Alliance for Quality. JACC Cardiovasc Interv. 2008;1(1):97–104. doi: 10.1016/j.jcin.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 9.Grines C, Patel A, Zijlstra F, Weaver WD, Granger C, Simes RJ, PCAT Collaborators Percutaneous transluminal coronary angioplasty. Primary coronary angioplasty compared with intravenous thrombolytic therapy for acute myocardial infarction: six-month follow up and analysis of individual patient data from randomized trials. Am Heart J. 2003;145(1):47–57. doi: 10.1067/mhj.2003.40. [DOI] [PubMed] [Google Scholar]
- 10.Nallamothu BK, Bates ER. Percutaneous coronary intervention versus fibrinolytic therapy in acute myocardial infarction: is timing (almost) everything? . Am J Cardiol. 2003;92(7):824–826. doi: 10.1016/s0002-9149(03)00891-9. [DOI] [PubMed] [Google Scholar]
- 11.Magid DJ, Wang Y, Herrin J, McNamara RL, Bradley EH, Curtis JP, et al. Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. JAMA. 2005;294(7):803–812. doi: 10.1001/jama.294.7.803. [DOI] [PubMed] [Google Scholar]
- 12.Krumholz HM, Herrin J, Miller LE, Drye EE, Ling SM, Han LF, et al. Improvements in door-to-balloon time in the United States, 2005 to 2010. Circulation. 2011;124(9):1038–1045. doi: 10.1161/CIRCULATIONAHA.111.044107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nestler DM, Noheria A, Haro LH, Stead LG, Decker WW, Scanlan-Hanson LN, et al. Sustaining improvement in door-to-balloon time over 4 years: the Mayo clinic ST-elevation myocardial infarction protocol. Circ Cardiovasc Qual Outcomes. 2009;2(5):508–513. doi: 10.1161/CIRCOUTCOMES.108.839225. [DOI] [PubMed] [Google Scholar]
- 14.Parikh SV, Treichler DB, DePaola S, Sharpe J, Valdes M, Addo T, et al. Systems-based improvement in door-to-balloon times at a large urban teaching hospital: a follow-up study from Parkland Health and Hospital System. Circ Cardiovasc Qual Outcomes. 2009;2(2):116–122. doi: 10.1161/CIRCOUTCOMES.108.820134. [DOI] [PubMed] [Google Scholar]
- 15.Haut ER, Pronovost PJ. Surveillance bias in outcomes reporting. JAMA. 2011;305(23):2462–2463. doi: 10.1001/jama.2011.822. [DOI] [PubMed] [Google Scholar]