Abstract
Although the better-educated are more likely to practice healthy behaviors when measured at one point in time, there is no clear evidence regarding whether more educated people are more likely to initiate healthy behavior changes in the face of new chronic conditions and whether they are better able to adhere to these healthy changes, once made. I use data from the Health and Retirement Study (HRS) (1992–2010) to examine smoking cessation and starting physical activity by educational attainment over an 18-year period among 16,606 respondents ages 50 to 75. The more-educated are the least likely to smoke and most likely to be physically active in middle age. They are also most likely to make healthy changes overall and better adhere to them. Education also shapes behavior change after a new diagnosis, which likely contributes to socioeconomic status differences in chronic disease management and health outcomes.
Keywords: chronic diseases, health behaviors, physical activity, smoking cessation, socioeconomic status
Health behaviors are an important contributor to chronic disease management and overall health in older age (ACCF/AHA 2009). However, there is little research about how common healthy behavior changes are, for how long they are sustained, and whether people are more likely to make behavior changes when they get sick. Understanding social patterns in health behavior changes and trajectories can help locate opportunities for interventions that decrease morbidity and mortality. Moreover, studying the socioeconomic status (SES) gradient in health behavior changes in the face of a new health condition highlights an important mechanism through which education shapes health disparities over the lifespan.
In this analysis, I examine patterns in health behavior changes by educational attainment and how they change in response to a new illness among a representative sample of middle-aged Americans over an 18-year period. I focus on healthy behavior changes for smoking and physical activity, two behaviors that are important for preventing and managing chronic illness (Rogers, Hummer, and Nam 2000). I examine educational differences in the likelihood of making a healthy behavior change during this time period and whether the more-educated are more likely to make healthy changes in the face of a new condition. Lastly, I examine patterns of adherence to healthy changes, once made. I find that there is a large degree of change in smoking and physical activity in middle age, and that diagnosis with a new condition is an important predictor of these changes. Results show that education influences the ways in which people respond to a new health problem, which in turn shapes socioeconomic differences in health over the lifespan. Moreover, education is a more important moderator of behavior change upon diagnosis in earlier than later adulthood, highlighting the importance of life stage in understanding how education works to shape health.
Background
Health Behaviors and the SES Gradient in Health
Health behaviors are often cited as a primary cause of the SES gradient in health because negative health behaviors such as smoking, heavy alcohol consumption, physical inactivity, and obesity are most common among those with low levels of education (Cutler and Lleras-Muney 2010) and they are associated with the onset of chronic diseases (Rogers et al. 2000). However, estimates of the contribution of health behaviors to SES differences in mortality are sensitive to the length of time during which health behaviors are observed.
Studies measuring health behaviors at one point in time in adulthood and subsequent mortality have found that health behaviors account for a substantial proportion of SES differences in mortality (Avendano 2006; Hirdes and Forbes 1992; Schrijvers et al. 1999; Smith, Shipley, and Rose 1990). For example, Lantz et al. (1998) examined the extent to which smoking, alcohol, sedentary life-style, and body weight accounted for differences in mortality by SES among a nationally representative sample of adult Americans. They found that these behavioral factors accounted for 14 percent of SES differences in mortality. Other similar studies report larger estimates among subgroups such as smoking among men (Denney et al. 2010; Jha et al. 2006; Marmot 2006), but lower estimates among older women (Denney et al. 2010).
There has been more recent emphasis on measuring health behaviors dynamically, since health behaviors might explain even more of the SES gradient in health if measured over the life course rather than at one point in time. For example, Stringhini et al. (2010) examined the role of health behaviors in explaining the association between socioeconomic position and mortality among a sample of British civil servants. They found that health behaviors measured at one point in time explained 42 percent of SES differences in all-cause mortality and 72 percent when including multiple measures of health behaviors. The fact that health behaviors over the life course are more strongly tied to mortality highlights the importance of understanding why there are SES differences in health behaviors over the life course and what predicts changes.
Health Behavior Changes and New Chronic Conditions
Health problems arise throughout the life course and how people respond to a new condition may shape future health. Several theories may explain why people with more education might be more likely to make a healthy behavior change in response to a new health condition. Comparing the way in which education moderates two different types of behavior change—smoking cessation and starting physical activity—can help us to understand how education may be influencing health behavior continuity and change and to what extent a new diagnosis is a critical point for shaping health disparities.
First, the more-educated may have more information about the importance of a health behavior change for disease management. This was important in explaining why college-educated smokers quit five times faster than less educated smokers between 1974 and 1985 after evidence accumulated that smoking causes lung cancer and heart disease (de Walque 2010; Pierce et al. 1989). However, educational levels may be less important for current middle-aged and older smokers because there is now widespread understanding that smoking causes health risks (Saad 2006) and there are few differences by SES in people’s reported desire to quit smoking (Barbeau, Krieger, and Soobader 2004; Link 2008). Information may be particularly important for knowledge about the benefits of physical activity (Siahpush et al. 2006). If knowledge about the benefits of making the healthy change is driving educational differences, then one would expect greater differences for physical activity than smoking cessation.
Second, the more-educated might better understand health information, which could translate to decisions to overcome nicotine addiction and the discomfort of exercise (Mirowsky and Ross 2003). The more-educated have a higher locus of control, which is important for quitting smoking (Ockene et al. 2000) and even more important for starting physical activity (Droomers et al. 1998). Making a healthy change for physical activity involves starting something, while smoking cessation involves stopping an unhealthy behavior. The highly educated might be better at translating health information into action through the ability to overcome discomfort.
These theoretical mechanisms focus on individual characteristics and how education serves as a critical feature of agency. However, structural factors also have an important role in shaping life chances and choices. Social class, capturing occupation, income, and wealth, as well as age and race-ethnicity are critical structural variables that shape the context in which individuals make life-style choices and changes (Cockerham 2005). This analysis focuses on education and how it shapes health behavior changes, but these important structural factors shape education and the propensities to make these changes.
Several recent studies found that smoking cessation and weight loss among the obese are more likely after respondents receive a new diagnosis (Clark and Etilé 2002; Falba 2005; Keenan 2009; Wray et al. 1998). However, it is not clear whether there are educational differences in behavior changes in response to a health shock. Only Wray et al. (1998) have addressed SES differences in the propensity to make these healthy changes upon diagnosis. They analyzed Health and Retirement Study (HRS) respondents in their 50s (1992–1994) to see whether education is associated with different rates of smoking cessation following a heart attack in a two-year period. They find that more educated respondents were more likely to stop smoking than less educated respondents after a heart attack. No studies have addressed educational differences in physical activity changes in response to a new condition or how the importance of education as a moderator of behavior change after an illness depends on stage of the life course.
Adherence to Healthy Behavior Changes
Little is known about patterns of adherence to behavior changes once initiated, and whether they differ by education. I hypothesize that the highly educated will have better adherence to healthy behaviors based on the fact that the well-educated better manage chronic conditions with complex treatment regimes (Goldman and Smith 2002) and better adhere to preventive screenings (Carrasquillo, Lantigua, and Shea 2001). If there are educational differences in adherence to smoking cessation and physical activity, there are several factors that could mediate the relationship between education and adherence. The highly educated might better adhere to healthy behaviors because they are in better health, with lower rates of disability, obesity, and later onset of chronic conditions than those of low SES (Hayward et al. 2000). Disability, obesity, and illness may hinder the ability to continue exercise. Similarly, illness can bring on stress, which can affect negative health behaviors. In this analysis, I examine each of these aspects of health status to see whether they mediate the effect of education on adherence to healthy behavior changes.
Contributions
In this analysis, I use nationally representative survey data on Americans ages 50–75 to document patterns in healthy behavior changes and trajectories for smoking and physical activity. First, I examine how frequent healthy behavior changes are among middle-aged Americans. Second, I examine educational differences in the probability of making a healthy behavior change. Third, I examine whether healthy behavior changes are more likely when respondents report new chronic conditions for which behavior changes are desirable for managing those specific conditions, and whether the more-educated are more likely to make healthy changes in the face of a new condition. Last, I examine whether educational attainment is associated with adherence to healthy changes. If so, then I examine whether the better adherence of the highly educated can be explained by their lower rates of disability, obesity, and chronic conditions.
This analysis extends research on SES and health in several ways. First, by examining educational differences in healthy changes after diagnosis, it highlights the way in which education conditions a response to a health shock, which is an important channel through which education affects health. The article highlights that education becomes decreasingly important as a moderator of healthy behavior changes upon diagnosis as age increases. This extends prior research, which assumes the equal importance of education for health throughout the life course (Mirowsky and Ross 2003). Second, prior research has not examined adherence to healthy behaviors, whether these patterns differ by education, and why. Third, a clear understanding of who makes healthy behavior changes and when they are made can improve health interventions. Lastly, if education is positively correlated with healthy behavior changes and adherence, then this pattern may explain why measuring health behaviors over time explains much more of SES differences in health than when measured only once.
Data and Methods
This study is based on the HRS, a longitudinal study of aging that is nationally representative of the U.S. population above age 50 (Juster and Suzman 1995). The HRS allows the analysis of health behavior changes over a long period of time. The longitudinal property is important because respondents’ trajectories are observed starting from when they are in their 50s, when most are still relatively healthy, into their 60s and early 70s, a period during which many report new chronic conditions and change their health behaviors. Another advantage is the ability to take into account confounding factors such as health status, existing chronic conditions, and changes in work hours, which have been linked to behavior change (Evenson et al. 2002).
This analysis examines HRS participants ages 50–75 during the study period 1992–2010. The analytic sample is structured to follow respondents’ health behavior trajectories for as long as the data allow. It includes respondents who were interviewed in two or more interviews until death or attrition.1 Of the 25,838 age-eligible respondents (50–75), I exclude AHEAD respondents (Assets and Health Dynamics Among the Oldest Old) because respondents because questions on health behaviors differed and focus on 18,066 respondents born between 1931 and 1959. I exclude 1,153 respondents because they completed less than two consecutive interviews and 307 because of missing data on education or health behaviors. Thus, the analytic sample consists of 16,606 respondents and 109,107 panel observations—92 percent of the age-cohort-eligible respondents. The analytic sample is similar to the age-eligible sample (Table A1).
Dependent Variables: Health Behavior Changes
In each interview, participants answered questions about their health behaviors. Smoking cessation is defined by whether the respondent reported smoking in one interview, but reported not smoking in the subsequent interview. Questions about smoking refer to cigarette smoking, but exclude pipes or cigars. Starting physical activity is defined as reporting doing “vigorous physical activity” in an interview, but not having done so in the previous interview. Coding draws on the RAND file, which recodes measures across waves to be as consistent as possible. Between 1992 and 2002, vigorous physical activity is defined as participating in vigorous physical activity three times a week or more. From 2004–2010, question wording was slightly different and is coded as vigorous physical activity more than once per week (online supplement details available at http://jhsb.sagepub.com/supplemental). A limitation due to question wording is that questions in 1996–2002 include physical activity due to exercise and work, but other waves exclude physical activity due to work. All analyses therefore take into account changes in work during the period of observation. Related sensitivity analyses are discussed at the end of the article. A limitation inherent in examining physical activity in middle and older age is that physical activity is a measure of health status as well as a predictor of future health status. Therefore, in examining changes in physical activity, I take into account how disability and obesity may be potential mediators.
I measure health behavior changes between two subsequent interviews. To examine whether these changes occur when respondents report new chronic conditions, I examine behavior change during the same two-year period as the new condition because diagnosis offers an opportunity for a turning point in health behaviors as patients are faced with new information about their health. Diagnosis refers to whether the doctor ever told the respondent that he or she has a certain condition. If diagnosis is a turning point for behavior change, then it is most likely that the behavior change would occur immediately or very soon after learning about the new condition.2
Adherence to smoking cessation and physical activity is examined among respondents who make a healthy change from smoking to nonsmoking and from physical inactivity to being physically active, and whom are followed at least one subsequent interview after this change. The length of adherence is measured from the first healthy behavior change to the interview when respondents report the unhealthy behavior or are censored either because of death, attrition from the study, or the end of the follow-up period. The samples are 2,071 respondents who quit smoking and 7,035 respondents who began physical activity during the follow-up period.
This analysis of adherence captures broad health behavior trajectories. The data do not capture short-term changes in behavior since health behaviors are recorded at interviews about two years apart. This measurement of behaviors at infrequent but regular intervals is similar to the study of the maintenance of HPV screening and mammography (Gierisch et al. 2010). This study of adherence starts with the first observed healthy change, which for most respondents is the only healthy change. For example, of those who stop smoking, 84 percent are observed quitting only once. Similarly, of those who start physical activity, 70 percent start only once during the study period. These data allow the examination of broad health behavior trajectories and provide a conservative estimate of the amount of change because very short-term health behavior changes are not observed.
Key Independent Variables: Socioeconomic Status and New Chronic Conditions
Educational attainment is the key measure of socioeconomic status and is analyzed both as a continuous measure (years) and as a categorical variable measuring degrees: less than high school, high school degree or GED, some college, or college degree. I focus on education as the key measure of socioeconomic status, rather than income or wealth, for three reasons. First, the ways in which education is thought to affect health, such as health literacy and self-efficacy, are particularly important for health behavior changes (Mirowsky and Ross 2003). Second, higher education leads to more health-promoting resources such as gym membership and healthy food (Ross and Wu 1995). Last, income and wealth can be volatile in middle age, partially because they are affected by changes in health and retirement (Smith 1999).
I examine whether healthy behavior changes are more likely when respondents report new chronic conditions for which healthy behavior changes are important for disease management as suggested by treatment guidelines (ACCF/AHA 2009). The chronic conditions examined are chosen because they are highlighted in medical guidelines that doctors follow for recommending behavior change at diagnosis. Smoking cessation is particularly important for managing the following six conditions: hypertension, heart disease, diabetes, lung disease, stroke, and cancer. I analyze three of them—hypertension, heart disease, and diabetes—in the analysis of physical activity because it is especially important for the treatment of these conditions and because they do not inhibit physical activity. Stroke, cancer, and lung disease may limit movement or lung capacity. New reported conditions are coded from questions that ask if a doctor ever told the respondent that he or she had the conditions listed below. If the condition is reported for the first time in a given wave after the baseline interview, it is coded as a new chronic condition.3
Other Explanatory Variables
Three sets of variables are potential mediators between educational attainment and healthy behavior changes and adherence. First, I include demographic characteristics: age, sex, race-ethnicity, and partnership status. Race is coded as non-Hispanic white, non-Hispanic black, and Hispanic/other. Partnership status is coded as partnered (married or cohabiting) or un-partnered (widowed, separated, divorced, or never married). Health status may also mediate the effect of education on health behavior changes and I measure it with four time-varying variables. The first is whether the respondent reports any new chronic conditions (of those listed above) or none. The second is the number of existing chronic conditions (of the six examined) that the respondent reported in the interview prior to reporting the new chronic condition. Additionally, the more-educated may be more likely to start physical activity because they are less likely to be obese or affected by disability. Therefore in the physical activity analysis, I also control for whether the respondent was obese (BMI ≥ 30), which was coded from questions that asked weight at each interview and height at baseline.4 Mobility limitations are coded as whether the respondent had difficulty with any of the following tasks: walking several blocks, one block, or across the room; climbing several flights of stairs; and climbing one flight of stairs. These questions were asked in every interview after 1992. I also control for labor force participation at first interview (works full-time, part-time, or not working) and changes in labor force participation (no change, worked more hours, or worked fewer hours). Change in labor force participation is time-varying and refers to the same period as behavior change, when it is most likely to affect behavior change.
Two additional control variables are included. First is a dummy variable for whether the respondent was reported dead during the study period to examine whether attrition due to death affects the results. Second, analysis of smoking cessation includes a variable for the number of cigarettes smoked in the previous period. This is to take into account the fact that smoking is an addictive behavior and because different levels of smoking intensity by education may explain educational differences in smoking cessation.
Analytical Approach
I estimate a series of logistic regressions to model the odds of making a healthy behavior change among a sample of respondents who practiced the unhealthy behavior at the previous interview. First, I examine whether there are differences by educational attainment in the odds of making a healthy behavior change during the follow-up period. Then I analyze SES patterns in behavior change when reporting new chronic conditions with an interaction term for education and any new chronic condition. To test whether education moderates behavior change differently depending on age, I run the interaction model for respondents ages 50–60 and 61–75. The age groups are chosen to be comparable to that of Wray et al. (1998) and to split the sample into similar size groups. The logistic regression model is used rather than conditional logit models with individual fixed effects in order to examine patterns of behavior change for the whole sample at risk of making a change. Including a fixed-effects term would control for time-invariant unobserved factors, but would exclude respondents who did not experience a change in the outcome of interest. This analysis includes all respondents at risk of making a healthy behavior change, including those who change and those who do not.
To account for the nonindependence of observations for each individual, I estimate the models on pooled data using robust standard errors (Huber-White method). The regression models are weighted to be representative of the population of that age group. Because respondents can change a health behavior more than once during the study period, the analysis includes more than one change for some respondents. However, results do not differ qualitatively when restricting the sample to the first observed healthy change.
The last part of the analysis addresses whether there are differences by educational attainment in adherence to healthy behavior changes after they are initiated. I chart adherence to smoking cessation and physical activity with Kaplan-Meier survival curves. Then, I estimate adherence to healthy behavior changes using a discrete-time event history framework, estimating binary logistic regression models on pooled person-interview observations (Allison 1982). This method is ideal because it is not biased by censoring and allows time-varying covariates. It is also more appropriate than continuous survival analysis because the data on health behaviors are available at each biennial interview, not at the exact time that the change occurs, making it inappropriate to treat the data as continuous.
I estimate the conditional probability of reverting to an unhealthy behavior, given that the individual has started practicing the healthy behavior at the previous interview. Respondents cease contributing person-interviews when they revert back to an unhealthy behavior or are censored, either because of the end of the study, death, attrition, or missing values. First, I examine whether there are differences in adherence to each health behavior by educational attainment, when controlling for age, number of months between interviews, and time since the change was made. Then I estimate a series of nested models to explore the other correlates of adherence. The first model includes education and demographic characteristics. The second model tests whether poorer adherence to healthy behaviors among those with low education is due to poorer health and higher levels of disability. The last model controls for labor force participation at first interview and changes.
Results
Table 1 presents weighted characteristics for the analytic sample. At first interview, respondents are on average 54.2 years old (SD = 3.1). Respondents are relatively healthy at first interview. More than half (56 percent) have no existing chronic conditions, 30 percent have only one, and 13 percent have two or more. Almost 80 percent report being in excellent, very good, or good health. During the study period, half of respondents report one or more new chronic conditions. Hypertension is the most common new condition, with one quarter (26 percent) of respondents reporting the new condition during the study. Fifteen percent report new heart disease, 13 percent new diabetes, 10 percent new cancer, 8 percent new lung disease, and 6 percent report new stroke. The majority of respondents in the sample (62 percent) are followed for six or more interviews, and 13 percent are reported dead during the study period.5
Table 1.
Weighted Sample Characteristics, Health and Retirement Study (N = 16,606).
| Characteristic | % or M (SD) | Characteristic | % or M (SD) | |
|---|---|---|---|---|
| Demographic characteristicsa | Labor force participation changeb | |||
| Age | 54.2 (3.1) | No change | 40.1 | |
| Female | 49.4 | Worked less | 51.9 | |
| Educational attainment | Worked more | 25.7 | ||
| Less than high school | 16.3 | Cigarettes smoked per day among smokers | 17.4 (11.8) | |
| High school degree | 34.2 | Reported dead (1992–2010) | ||
| Some college | 24.8 | Number of completed consecutive interviewsc | 12.9 | |
| College degree | 24.8 | |||
| Race-ethnicity | 10 | 20.0 | ||
| Non-Hispanic white | 79.5 | 9 | 12.4 | |
| Non-Hispanic black | 10.8 | 8 | 9.3 | |
| Hispanic/other race | 9.8 | 7 | 13.6 | |
| Partnership status | 6 | 6.5 | ||
| Partnered | 74.8 | 5 | 5.9 | |
| Unpartnered | 25.2 | 4 | 17.5 | |
| Health statusa | 3 | 8.3 | ||
| Number existing chronic conditions | 2 | 6.2 | ||
| None | 56.4 | 1 | 0 | |
| One | 30.2 | Health behavior continuity and change | ||
| Two | 10.2 | Smoking behavior summary | ||
| Three or more | 3.2 | Nonsmoker throughout study | 71.5 | |
| Self-rated health | Smoker throughout study | 13.7 | ||
| Good, very good, excellent | 79.1 | Stops smoking once | 7.9 | |
| Fair or poor | 20.9 | Starts smoking once | 1.4 | |
| Obese (BMI ≥ 30) | 28.0 | Starts and stops smoking | 5.5 | |
| Any mobility limitation | 32.6 | Total | 100 | |
| Health changesb | Smoking | |||
| Number new chronic conditions | % smokes during study periodd | 28.4 | ||
| None | 48.7 | % stops smoking | 13.4 | |
| One | 31.6 | % smokes at baseline | 25.2 | |
| Two | 14.2 | Physical activity behavior summary | ||
| Three or more | 5.5 | Always physically active | 6.8 | |
| Type of new chronic conditione | Never physically active | 30.2 | ||
| Hypertension | 25.9 | Stops physical activity once | 13.1 | |
| Heart disease | 14.8 | Starts physical activity once | 8.6 | |
| Diabetes | 13.4 | Starts and stops physical activity | 41.3 | |
| Cancer | 10.2 | Total | 100 | |
| Lung disease | 7.8 | Physical activity | ||
| Stroke | 5.6 | % inactive during studyf | 93.1 | |
| Labor force participation at baseline | % starts physical activity | 49.9 | ||
| Not working | 25.6 | % physically active at baseline | 31.8 | |
| Works part-time | 13.2 | |||
| Works full-time | 61.2 | |||
Measured at first interview.
Respondents may have experienced more than one change (1992–2010); therefore, changes do not sum to 100 percent.
Unweighted for sample description.
The respondents at risk of smoking cessation are all except those who are nonsmokers throughout the study.
Reported throughout study period (1992–2010).
The respondents at risk of starting physically activity are all except those who are always physically active.
Healthy behavior changes are common in middle and older age. Three in ten respondents smoke during the study period (28.4 percent) and half of those smokers stop (13.4 percent of the sample). A minority of respondents do not change their physical activity during the study period. Only 7 percent are physically active each time they are interviewed and three in ten are never physically active. Most respondents start physical activity during the study, whether it is their only change (9 percent) or whether they make more than one change (41 percent). The high proportion of respondents who change their physical activity is noteworthy, however not surprising, given that many respondents retire and start new activities during this time. Many also develop new health problems and disability over the study period, which may make it more difficult to stay active.
Table A2 in the online supplement shows that there are large differences by education in health behavior continuity and change. Those with high levels of education are more likely to be nonsmokers. Only 15 percent of college-educated respondents smoke compared to 41 percent of high school dropouts. In the past, these cohorts had very high rates of smoking, and other research has documented high rates of smoking cessation in the past, especially among the highly educated (de Walque 2010). There are also large differences by education in physical activity over the study period. The college-educated are the most likely to be consistently active. For example, 14 percent of the college-educated are physically active throughout the study compared with 2 percent of those with less than a high school education.
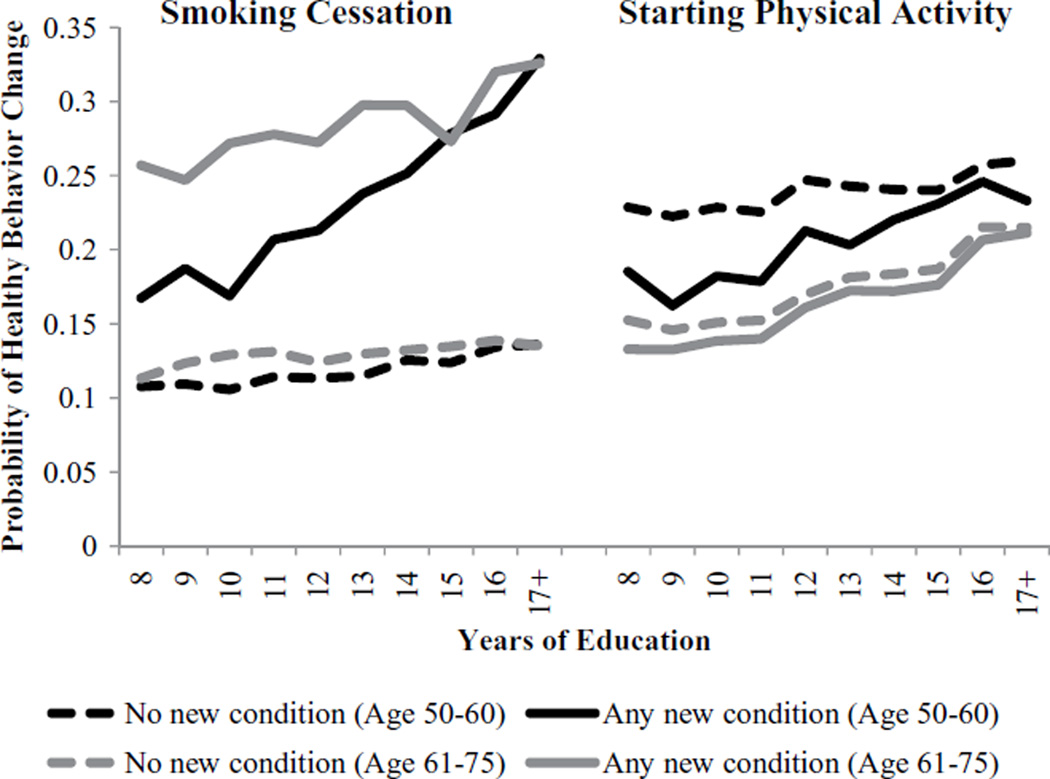
Education Differences in Healthy Behavior Changes
Next, I examine whether the more-educated are more likely to make healthy behavior changes. Results in Table 2 show that education is positively associated with smoking cessation (Models 1–3). Each year of education is associated with a 3 percent increase in the odds of quitting in middle age when including all controls (Model 3). Moreover, reporting a new chronic condition is a strong predictor of smoking cessation, associated with an odds ratio of 2.38 relative to when reporting no new condition. Model 4 examines whether the more-educated are more likely to quit smoking upon reporting a new chronic condition. Among the whole sample (ages 50–75) there is no interaction between education and a new chronic condition (Model 4). However, education is a significant moderator of smoking cessation upon diagnosis among adults ages 50–60 (Model 4b), but not among adults ages 61–75 (Model 4c). Figure 1 charts the predicted probabilities of this behavior change from Models 4b and 4c. Respondents of all educational levels are more likely to stop smoking when they report a new condition relative to when reporting none. However, among respondents in their 50s, those with higher education are more likely to stop smoking when reporting a new condition. Those with less than a high school education have a .15–.20 probability of quitting at this time compared to the college-educated, who have more than a .30 probability of quitting after a new diagnosis. Among the older age group, the lines are not exactly parallel, but the interaction is not statistically significant.
Table 2.
Odds Ratios from Logistic Regression Models Predicting Smoking Cessation, Health, and Retirement Study (1992–2010).
| Smoking Cessation among Smokers | |||||||
|---|---|---|---|---|---|---|---|
| Bivariate | Model 1 | Model 2 | Model 3 | Model 4a | Model 4b Age 50–60 |
Model 4c Age 61–75 |
|
| Sample size | 4,404 | 4,404 | 4,404 | 4,404 | 4,404 | 3,663 | 2,739 |
| Education (years) | 1.01 | 1.04*** | 1.04*** | 1.03** | 1.02 | 1.03** | 1.01 |
| Age | 1.02*** | 1.02*** | 1.01** | 1.01 | 1.01** | 1.03 | 1.00 |
| Female (male) | .91 | .95 | .97 | .89 | .89 | .84* | .93 |
| Race-ethnicity (non-Hispanic white) | |||||||
| Non-Hispanic black | 1.14 | 1.25** | 1.23* | .97 | .97 | .91 | 1.05 |
| Hispanic/other | 1.51*** | 1.72*** | 1.77*** | 1.40** | 1.39** | 1.48** | 1.29 |
| Partnered (un-partnered) | 1.20** | 1.23** | 1.24** | 1.21** | 1.21** | 1.17 | 1.24** |
| Any new chronic condition (None) | 2.29*** | 2.28*** | 2.38*** | 1.62 | .94 | 2.28* | |
| Number of previous chronic conditions | 1.11*** | 1.11*** | 1.11*** | 1.11*** | 1.11*** | 1.11*** | |
| Cigarettes/day reported at previous interview | .97*** | .97*** | .97*** | .96*** | .97*** | ||
| Labor force participation at baseline (full-time) | |||||||
| Part-time | .94 | .94 | .94 | 1.00 | .87 | ||
| Not working | .97 | .96 | .96 | .93 | .99 | ||
| Change in labor force participation (no change) | |||||||
| Working less | 1.11 | 1.11 | 1.12 | 1.12 | 1.11 | ||
| Working more | 1.02 | 1.02 | 1.04 | 1.05 | .97 | ||
| Reported dead during follow-up | .97 | 1.04 | 1.04 | .99 | 1.08 | ||
| Education × New Chronic Condition | 1.03 | 1.03 | 1.07* | 1.01 | |||
p < .05.
p < .01.
p < .001.
Figure 1.
Predicted Probabilities of Smoking Cessation and Physical Activity, by Education and Whether Reported a New Chronic Condition, Health and Retirement Study (1992–2010).
Note: Predicted probabilities are calculated from Models 4b and 4c on Tables 2 and 3, holding other covariates at mean levels.
Table 3 shows that education is also positively associated with starting physical activity. Each year of education is associated with 3 percent higher odds of starting exercise in middle age (Model 1). Model 2 examines whether differences in health status explain why the more-educated are more likely to start physical activity. Educational differences in physical activity disappear when controlling for health status, measured by any new chronic condition, existing conditions, obesity, and mobility limitations. Of these factors, mobility limitations alone can account for educational differences in physical activity (Model 2b). Disability is much more important than any of the other factors in explaining education differences in this behavior change.
Table 3.
Odds Ratios from Logistic Regression Models Predicting Starting Physical Activity, Health and Retirement Study (1992–2010).
| Starting Physical Activity among Inactive | ||||||||
|---|---|---|---|---|---|---|---|---|
| Bivariate | Model 1 | Model 2aa |
Model 2b |
Model 3 | Model 4a | Model 4b Age 50–60 |
Model 4c Age 61–75 |
|
| Sample size | 14,479 | 14,479 | 14,479 | 14,479 | 14,479 | 14,479 | 11,066 | 10,650 |
| Education (years) | 1.04*** | 1.03*** | 1.00 | 1.00 | 1.00 | .99** | .97*** | 1.01 |
| Age | .97*** | .97*** | .99*** | .99*** | .99*** | .99*** | 1.00 | .94*** |
| Female | .77*** | .83*** | .89*** | .92** | .90*** | .90*** | .95 | .81*** |
| Race-ethnicity (non-Hispanic white) | ||||||||
| Non-Hispanic Black | .83*** | .93 | 1.02 | .96 | 1.02 | 1.02 | 1.01 | 1.03 |
| Hispanic/other | .95 | 1.07 | 1.04 | 1.05 | 1.04 | 1.04 | 1.05 | 1.02 |
| Partnered (un-partnered) | 1.44*** | 1.32*** | 1.23*** | 1.23*** | 1.23*** | 1.23*** | 1.19*** | 1.25*** |
| Any new chronic condition (none) | .86*** | .92 | .92* | .64* | .64 | .67 | ||
| Number of previous chronic conditions | .71*** | .84*** | .84*** | .85*** | .86*** | .84*** | ||
| Obese (not obese)a | .59*** | .76*** | .76*** | .76*** | .73*** | .78*** | ||
| Any mobility limitation (none) | .38*** | .48*** | .41*** | .49*** | .49*** | .47*** | .50*** | |
| Labor force participation at baseline (full-time) | ||||||||
| Not working | .96 | 1.04 | 1.04 | .97 | 1.13* | |||
| Part-time | .67*** | .91** | .91** | .89 | .93 | |||
| Change in labor force participation (no change) | ||||||||
| Working less | 1.34*** | 1.29*** | 1.29*** | 1.19** | 1.30*** | |||
| Working more | 1.26*** | 1.15* | 1.15* | 1.16* | 1.22*** | |||
| Reported dead during follow-up | .82*** | 1.00 | .99 | 1.11 | 1.01 | |||
| Education × New Chronic Condition | 1.03 | 1.02* | 1.02 | 1.03 | ||||
Model 2a controls for all four health variables, each of which alone does not explain education differences in starting physical activity (results not shown) except mobility limitations, which is shown in Model 2b, highlighting its importance for explaining education differences in starting physical activity.
p < .05.
p < .01.
p < .001.
In contrast to smoking cessation, reporting a new chronic condition is associated with lower, not higher, odds of starting physical activity. This may be because those who report new chronic conditions are negatively selective in terms of health and exercise. It also may be that people are dealing with health complications. Model 4 examines whether the pattern of starting activity upon a new health problem differs by education. The interaction term shows that education is a significant moderator of this relationship among all respondents ages 50–75. The last two models test whether there are differences by age and find that although the coefficients hardly differ, the interaction is not statistically significant among the smaller samples. The probability of starting physical activity is plotted from Models 4b and 4c in Figure 1. The degree to which reporting a new condition is associated with a lower probability of starting activity differs by education. There is no difference among the highly educated in the odds of starting activity depending on reporting a new illness, but among the less educated, those who report a new illness are less likely to start activity at this time. Similar to smoking cessation, the differences in the probabilities of behavior change upon diagnosis seem larger for adults ages 50–60 than 61–75.
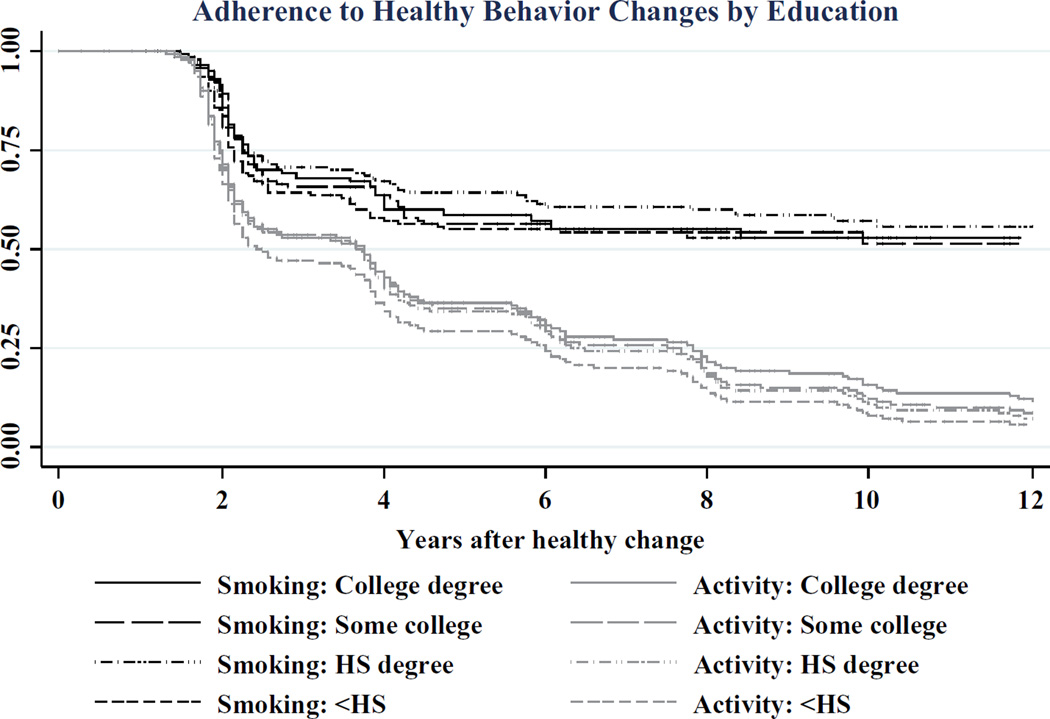
Adherence to Smoking Cessation and Physical Activity
Last, I turn to patterns in adherence to healthy behavior changes shown in Figure 2.6 Examining the proportion of those who remain nonsmokers at each subsequent interview after quitting shows that there is a large drop off in the period following cessation. Thirty percent of those who stopped smoking report smoking again at the next interview. Of the 70 percent who remain nonsmokers after two years, most adhere to smoking cessation. Just over half who quit remain nonsmokers over the study period. The college-educated and those with a high school degree have better adherence to smoking cessation than those with less than a high school education or some college. In Table A3 in the online supplement, the bivariate and multivariate discrete-time event history models clearly show that the more-educated have better adherence to smoking cessation.
Figure 2.
Kaplan Meier Survival Curves for Adherence to Smoking Cessation and Physical activity after Initiation by Education, Health and Retirement Study.
Note: The log-rank test of equality across strata finds significant differences between the adherence patterns by education to smoking cessation (p < .05) and physical activity (p < .001).
The survival curves for adherence to physical activity are steeper than those for smoking cessation. For all education groups, the shape of the survival curve is steadily downward, with the largest drop-off at the next interview. The superior adherence to physical activity by the more-educated remains throughout the period of observation. Table A3 presents nested models to examine whether educational differences in adherence to physical activity can be explained by the better health of those with more education. Results from Model 1 show that relative to high school dropouts, respondents with more education have much lower odds of reverting to inactivity. Model 2 examines whether health explains these differences. Health does not explain the differences between those with the least education and those with higher levels of education. However, controlling for mobility limitations explains differences between those with a high school degree, some college, and a college degree (results not shown), highlighting that disability is an important factor in explaining the differences in adherence to activity between those with all but the least education. Model 3 includes changes in labor force participation, which also cannot explain the differences in adherence between high school dropouts and those with more education. In summary, differences in adherence to physical activity remain between those with the least education and all other groups, which cannot be explained by the examined factors.
Discussion
One puzzle about SES and health is why health behaviors explain so much more of SES differences in mortality when capturing health behaviors measured at multiple times (Stringhini et al. 2010) than when measured at one point in time (Lantz et al. 1998). This article documents that there are very large differences by education in smoking and physical activity trajectories in middle age, even though many health habits are already set by this stage of the life course. Health behavior changes are surprisingly common between ages 50 and 75 and the fact that the more-educated are more likely to stop smoking, start physical activity, and maintain both of these behaviors over time likely contributes to SES differences in chronic disease incidence and management in middle and older age. The fact that SES differences in health behavior trajectories by education are so large may help to explain why much more of SES differences in mortality are explained when capturing trajectories rather than when measured once.
I examined whether the more-educated respond differently than the less-educated in making healthy behavior changes when diagnosed with chronic conditions for which changes are important for disease management. Education increases the odds of a healthy behavior change upon diagnosis. This highlights the way in which education conditions a response to a health shock, which is an important channel through which education affects health. Importantly, I find that education becomes decreasingly important as a moderator of healthy behavior changes upon diagnosis as age increases. Education increases the odds of smoking cessation when reporting a new illness among respondents in their 50s, but not those in their 60s or early 70s.
This has two implications for research on education and health behaviors. First, research on how education influences health should examine how the importance of education for health behaviors and health changes varies over the life course. Previous work on the mechanisms through which education shapes health and health behaviors has assumed that education is equally important across age (Link and Phelan 1995; Mirowsky and Ross 2003). Understanding when education has the greatest effect in conditioning behavior changes is important for understanding how and why health inequalities change across age. Second, the more-educated are more likely to make changes when they get sick, even when the health shock is not that serious. Wray et al. (1998) examined this interaction for a relatively serious health event—a heart attack. However, this article highlights that education moderates behavior change upon a broader set of health events, including hypertension diagnosis. Future research should examine which kinds of new health shocks people respond to, because if the more-educated respond more to less serious shocks, then this may be another mechanism shaping health disparities.
Why does education moderate the effect of a new condition on smoking cessation for respondents in their 50s, but not in their 60s and early 70s? One explanation is that the sample of smokers becomes more and more select over the lifespan. The examined cohorts experienced high rates of smoking cessation before middle age whereby smokers who were the least attached to smoking and cared most about their health quit earlier on. In the 1970s and 1980s, more educated smokers quit much more quickly than less educated smokers (de Walque 2010; Pierce et al. 1989). Thus, well-educated smokers in their 60s and early 70s are a small and select group. They may be the most addicted or the most stubborn. I find that older well-educated smokers are less likely to quit than younger smokers of the same education level and just as likely to quit as less educated smokers when they get sick. This explanation implies that for smoking, a behavior which is increasingly negatively selective over the life course, the predictors of behavior change vary over the lifespan. Education becomes decreasingly important as a moderator of behavior change upon diagnosis as age increases.
A second explanation is that the longer people expect to live when they get sick, the more likely they are to make a healthy behavior change. This could explain why the more-educated are more likely to quit smoking when they get sick in their 50s than less educated smokers (the more-educated live longer) and also why education is a more important moderator of behavior change in the 50s than in older ages. Wray et al. (1998) tested various explanations for why education moderates smoking cessation after a heart attack and found that the only factor that mattered was future orientation, as measured by financial planning timeline. In additional analyses (results not shown), I find that future orientation and cognitive functioning can explain the differential behavior at diagnosis by education. This suggests that perhaps the more-educated are more likely to quit smoking upon diagnosis than less educated smokers because they expect to live for longer, better understand how quitting smoking can increase their lifespan, or can better translate the will or knowledge into actually quitting (Mirowsky and Ross 2003; Ockene et al. 2000).
Disability was the most important mediator explaining SES differences in starting and maintaining physical activity. However, other aspects of health, such as number of chronic conditions and obesity, were also important. Higher levels of physical activity also likely contribute to better health. Even after accounting for health status, there still remained differences in adherence to physical activity between the least educated and all others. Future research should try to differentiate between various proposed mechanisms that were not directly measured here, such as knowledge about importance of physical activity, investment in future health, and self-control, as suggested by Pampel et al. (2010).
The more-educated also responded differently in starting physical activity upon diagnosis than their less-educated counterparts. In additional analyses (results not shown), I found that the differential behavior by education was not explained by differences in future orientation or cognitive function. Future research should test whether the educational differences in starting physical activity upon diagnosis are due to the highly educated having better information about the short- and long-run benefits of physical activity for health, which has been highlighted in previous work (Siahpush et al. 2006). This information could be coming from the doctor at the time of diagnosis or from peer or family networks. Other research should also test whether there are SES differences in knowledge of the importance of physical activity for specific chronic conditions like hypertension and diabetes. If so, policy could affect this by targeting information at the point of diagnosis.
This analysis is limited by several features of the available data. Health behaviors are measured in each interview approximately every two years and questions refer to smoking at the time of the survey and physical activity over the 12 months before the interview. These data allow the examination of broad health behavior trajectories, but may underestimate the amount of change because short-term behavior changes are not observed. Other studies do not have a long follow-up, but have more detailed short-term data on patterns of smoking relapse. Some find no differences by education in short-term relapse (Garvey et al. 1992), but others document differences by confidence and self-efficacy, which are correlated with education (McBride and Pirie 1990; Ockene et al. 2000). More short-term changes may be missed for those with lower education. In these data, the education distribution of respondents making two or more changes for physical activity is no different than for the cohort at large. However, respondents that make two or more smoking changes are, on average, slightly less educated. Thus, the results do not have external validity for short-term changes. However, given that short-lived healthy changes do not affect health as much as long-term trajectories, these results may be more important for explaining SES differences in broad health behavior trajectories.
A second limitation is that the data do not allow us to distinguish the intentionality of physical activity. Physical activity could be part of work due to question wording in four interviews, and work changes during the study period. However, this limitation does not discount the article’s results. The multivariate models control for work status at baseline and changes in labor force participation. The same pattern of results is found when controlling for whether the respondent’s work is physically challenging at least some of the time or controlling for whether the respondent was working in a physically demanding occupation. But even then, the analysis likely underestimates the degree of educational differences in starting physical activity because low-SES men who do physically demanding jobs are not at risk of starting activity.
As the respondents move from middle age to older age during the study period, 13 percent are reported dead. Unsurprisingly, those who died were more likely to be male, less educated, more likely to smoke, and less likely to be physically active at baseline than the whole sample (Table A1 in the online supplement). The selective mortality means that those with higher education and better health behaviors are observed for longer on average. However, the results do not differ when excluding those who die from the analysis altogether. Lastly, this study did not examine patterns of behavior change for chronic conditions separately or the severity of conditions at diagnosis, but future research can address these questions.
Despite limitations, this analysis shows that the way in which education conditions a response to a health shock is an important channel through which education shapes health. The fact that education moderates the effect of a new health problem on smoking cessation and starting physical activity may account for why the better-educated are better able to manage chronic conditions and have better health outcomes. Results highlight the importance of life stage in understanding how education works to shape health.
Acknowledgments
I am grateful to Irma Elo, Sam Preston, Jason Schnittker, Nirav Mehta, and Bill Avison, as well as the JHSB anonymous reviewers and editor, for their helpful feedback on this manuscript. I also acknowledge the University of Michigan and RAND for making the HRS data accessible and clearly documented.
Funding
The author disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the National Institutes of Health (NIA T32-AG000177, P30AG12836 and NICHDT32HD007242, R24HD044964) at the University of Pennsylvania, and the University of Western Ontario.
Biography
Rachel Margolis is an assistant professor of sociology at the University of Western Ontario. Her research examines factors throughout the life course that contribute to social disparities in health and well-being.
Footnotes
An earlier version of this article was presented at the 2010 Population Association of American meeting.
Proxy interviews are included, but results do not differ if they are excluded.
Smoking cessation is no more likely in the period before or after reporting new chronic conditions, compared to when reporting no new conditions. Similarly, there are no differences in starting physical activity in the period after reporting a new condition relative to none. However, starting physical activity is less likely (OR = .90, p < .10) in the period before reporting a new chronic condition, relative to no new condition (results not shown).
New conditions are coded from the RAND data file and are based on questions that ask respondents whether a doctor ever told the respondent that he or she had the following conditions: high blood pressure or hypertension, diabetes or high blood sugar, cancer or a malignant tumor of any kind except skin cancer, chronic lung disease except asthma such as chronic bronchitis or emphysema, heart attack, coronary heart disease, angina, congestive heart failure or other heart problems, and stroke or transient ischemic attack.
Results for physical activity are robust to controlling for body mass index (BMI) ≥ 35 rather than BMI ≥ 30.
Characteristics of respondents who die are reported in Table A1 in the online supplement.
The data do not allow the observation of the exact length of adherence. The change could be maintained for a very short time or could be until just before the next interview.
REFERENCES
- ACCF/AHA. ACCF/AHA 2009 Expert Consensus Document on Pulmonary Hypertension. Circulation. 2009;119(16):2250–2294. doi: 10.1161/CIRCULATIONAHA.109.192230. [DOI] [PubMed] [Google Scholar]
- Allison Paul D. Discrete-time Methods for the Analysis of Event Histories. Sociological Methodology. 1982;13(1):61–98. [Google Scholar]
- Avendano Mauricio. Smoking and Inequalities. The Lancet. 2006;368(9545):1417–1418. doi: 10.1016/S0140-6736(06)69600-1. [DOI] [PubMed] [Google Scholar]
- Barbeau Elizabeth M, Krieger Nancy, Soobader Mah-Jabeen J. Working Class Matters: Socioeconomic Disadvantage, Race/Ethnicity, Gender, and Smoking in NHIS 2000. American Journal of Public Health. 2004;94(2):269–278. doi: 10.2105/ajph.94.2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrasquillo Olveen, Lantigua Rafael A, Shea Steven. Preventive Services among Medicare Beneficiaries with Supplemental Coverage versus HMO Enrollees, Medicaid Recipients, and Elders with no Additional Coverage. Medical Care. 2001;39(6):616–626. doi: 10.1097/00005650-200106000-00009. [DOI] [PubMed] [Google Scholar]
- Clark Andrew, Etilé Fabrice. Do Health Changes Affect Smoking? Evidence from British Panel Data. Journal of Health Economics. 2002;21(4):533–562. doi: 10.1016/s0167-6296(01)00140-0. [DOI] [PubMed] [Google Scholar]
- Cockerham William C. Health Lifestyle Theory and the Convergence of Agency and Structure. Journal of Health and Social Behavior. 2005;46(1):51–67. doi: 10.1177/002214650504600105. [DOI] [PubMed] [Google Scholar]
- Cutler David M, Lleras-Muney Adriana. Understanding Differences in Health Behaviors by Education. Journal of Health Economics. 2010;29(1):1–28. doi: 10.1016/j.jhealeco.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denney Justin T, Rogers Richard D, Hummer Robert A, Pampel Fred C. Education Inequality in Mortality: The Age and Gender Specific Mediating Effects of Cigarette Smoking. Social Science Research. 2010;39(4):662–673. doi: 10.1016/j.ssresearch.2010.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Walque Damien. Education, Information, and Smoking Decisions: Evidence from Smoking Histories in the United States, 1940–2000. Journal of Human Resources. 2010;45(3):682–717. [Google Scholar]
- Droomers Mariel, Schrijvers Carola TM, van de Mheen H, Mackenbach Johan P. Educational Differences in Leisure-time Physical Inactivity: A Descriptive and Explanatory Study. Social Science & Medicine. 1998;47(11):1665–1676. doi: 10.1016/s0277-9536(98)00272-x. [DOI] [PubMed] [Google Scholar]
- Evenson Kelly R, Rosamond Wayne D, Cai Jianwen, Diez-Roux Ana V, Brancati Frederick L for the Atherosclerosis Risk in Communities Study Investigators. Influence of Retirement on Leisure-time Physical Activity. American Journal of Epidemiology. 2002;155(8):692–699. doi: 10.1093/aje/155.8.692. [DOI] [PubMed] [Google Scholar]
- Falba Tracy. Health Events and the Smoking Cessation of Middle Aged Americans. Journal of Behavioral Medicine. 2005;28(1):21–33. doi: 10.1007/s10865-005-2560-1. [DOI] [PubMed] [Google Scholar]
- Garvey Arthur J, Bliss Ryan E, Hitchcock Jan L, Heinold Jerilyn W, Rosner Bernard. Predictors of Smoking Relapse among Self-quitters: A Report from the Normative Aging Study. Addictive Behaviors. 1992;17(4):367–377. doi: 10.1016/0306-4603(92)90042-t. [DOI] [PubMed] [Google Scholar]
- Gierisch Jennifer M, Reiter Paul. L, Rimer Barbara. K, Brewer Noel. T. Standard Definitions of Adherence for Infrequent Yet Repeated Health Behaviors. American Journal of Health Behavior. 2010;34(6):669–679. doi: 10.5993/ajhb.34.6.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman Dana P, Smith James P. Can Patient Self-management Help Explain the SES Health Gradient? Proceedings of the National Academy of Sciences. 2002;99(16):10929–10934. doi: 10.1073/pnas.162086599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward Mark D, Miles Toni P, Crimmins Eileen M, Yang Yu. The Significance of Socioeconomic Status in Explaining the Racial Gap in Chronic Health Conditions. American Sociological Review. 2000;65(6):910–930. [Google Scholar]
- Hirdes John P, Forbes William F. The Importance of Social Relationships, Socioeconomic Status and Health Practices with Respect to Mortality among Healthy Ontario Males. Journal of Clinical Epidemiology. 1992;45(2):175–182. doi: 10.1016/0895-4356(92)90010-k. [DOI] [PubMed] [Google Scholar]
- Jha Prabhat, Peto Richard, Zatonski Witold, Boreham Jillian, Jarvis Martin J, Lopez Alan D. Social Inequalities in Male Mortality, and in Male Mortality from Smoking: Indirect Estimation from National Death Rates in England and Wales, Poland, and North America. The Lancet. 2006;368(9533):367–370. doi: 10.1016/S0140-6736(06)68975-7. [DOI] [PubMed] [Google Scholar]
- Juster F Thomas, Suzman Richard. An Overview of the Health and Retirement Study. Journal of Human Resources. 1995;30:S7–S56. [Google Scholar]
- Keenan Patricia S. Smoking and Weight Change after New Health Diagnoses in Older Adults. Archives of Internal Medicine. 2009;169(3):237–242. doi: 10.1001/archinternmed.2008.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lantz Paula M, House James S, Lepkowski James M, Williams David R, Mero Richard P, Chen Jieming. Socioeconomic Factors, Health Behaviors, and Mortality. JAMA: The Journal of the American Medical Association. 1998;279(21):1703–1708. doi: 10.1001/jama.279.21.1703. [DOI] [PubMed] [Google Scholar]
- Link Bruce G. Epidemiological Sociology and the Social Shaping of Population Health. Journal of Health and Social Behavior. 2008;49(4):367–384. doi: 10.1177/002214650804900401. [DOI] [PubMed] [Google Scholar]
- Link Bruce G, Phelan Jo C. Social Conditions as Fundamental Causes of Disease. Journal of Health and Social Behavior. 1995;35(1):80–94. [PubMed] [Google Scholar]
- Marmot Michael. Smoking and Inequalities. The Lancet. 2006;368(9533):341–342. doi: 10.1016/S0140-6736(06)68976-9. [DOI] [PubMed] [Google Scholar]
- McBride Colleen M, Pirie Phyllis L. Postpartum Smoking Relapse. Addictive Behaviors. 1990;15(2):165–168. doi: 10.1016/0306-4603(90)90020-x. [DOI] [PubMed] [Google Scholar]
- Mirowsky John, Ross Catherine E. Education, Social Status, and Health. Hawthorn, NY: Aldine de Gruyter; 2003. [Google Scholar]
- Ockene Judith K, Mermelstein Robin J, Bonollo Debra S, Emmons Karen M, Perkins Kenneth A, Voorhees Carolyn, Hollis Jack F. Relapse and Maintenance Issues for Smoking Cessation. Health Psychology. 2000;19(S1):17–31. doi: 10.1037/0278-6133.19.suppl1.17. [DOI] [PubMed] [Google Scholar]
- Pampel Fred C, Krueger Patrick M, Denney Justin T. Socioeconomic Disparities in Health Behaviors. Annual Review of Sociology. 2010;36:349–370. doi: 10.1146/annurev.soc.012809.102529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce John P, Fiore Michael C, Novotny Thomas E, Hatziandreu Evridiki J, Davis Ronald M. Trends in Cigarette Smoking in the United States. JAMA: The Journal of the American Medical Association. 1989;261(1):56–60. [PubMed] [Google Scholar]
- Rogers Richard G, Hummer Robert A, Nam Charles B. Living and Dying in the USA: Behavioral, Health, and Social Differentials of Adult Mortality. San Diego, CA: Academic Press; 2000. [Google Scholar]
- Ross Catherine E, Wu Chia-ling. The Links between Education and Health. American Sociological Review. 1995;60(5):719–745. [Google Scholar]
- Saad Lydia. Many Americans Still Downplay Risk of Passive Smoking. Gallup News Service. 2006 http://www.gallup.com/poll/23851/many-americans-still-downplay-risk-passive-smoking.aspx. [Google Scholar]
- Schrijvers Carola T, Stronks H Karien, van de Mheen D, Mackenbach Jonan P. Explaining Educational Differences in Mortality: The Role of Behavioral and Material Factors. American Journal of Public Health. 1999;89(4):535–540. doi: 10.2105/ajph.89.4.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siahpush M, McNeill A, Hammond D, Fong GT. Socioeconomic and Country Variations in Knowledge of Health Risks of Tobacco Smoking and Toxic Constituents of Smoke: Results from the 2002 International Tobacco Control (ITC) Four Country Survey. Tobacco Control. 2006;15(S3):iii65–iii70. doi: 10.1136/tc.2005.013276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith George D, Shipley Martin J, Rose Geoffrey. Magnitude and Causes of Socioeconomic Differentials in Mortality: Further Evidence from the Whitehall Study. Journal of Epidemiology and Community Health. 1990;44(4):265–270. doi: 10.1136/jech.44.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith James P. Healthy Bodies and Thick Wallets: The Dual Relation between Health and Economic Status. The Journal of Economic Perspectives. 1999;13(2):145–166. [PMC free article] [PubMed] [Google Scholar]
- Stringhini Silvia, Sabia Séverine, Shipley Martin, Brunner Eric, Nabi Hermann, Kivimaki Mika, Singh-Manoux Archana. Association of Socioeconomic Position with Health Behaviors and Mortality. JAMA: The Journal of the American Medical Association. 2010;303(12):1159–1166. doi: 10.1001/jama.2010.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wray Linda A, Herzog A Regula, Willis Robert J, Wallace Robert B. The Impact of Education and Heart Attack on Smoking Cessation among Middle-aged Adults. Journal of Health and Social Behavior. 1998;39(4):271–294. [PubMed] [Google Scholar]