Abstract
This paper analyzes Thailand’s 2001 healthcare reform, “30 Baht”. The program increased funding available to hospitals to care for the poor and reduced copays to 30 Baht (~$0.75). Our estimates suggest the supply-side funding of the program increased healthcare utilization, especially amongst the poor. Moreover, we find significant impacts on infant mortality: prior to 30 Baht poorer provinces had significantly higher infant mortality rates than richer provinces. After 30 Baht this correlation evaporates to zero. The results suggest that increased access to healthcare among the poor can significantly reduce their infant mortality rates.
Keywords: Health Insurance, Infant Mortality
In 2001, Thailand initiated the 30 Baht program, one of the largest, most ambitious health reforms ever undertaken in a developing country. The primary aim of this program was to reduce the long-standing geographical disparities in the provision of public healthcare in Thailand by dramatically increasing funding to provide for care to the poor. The program had two key features. First, the program replaced pre-existing funding arrangements with a universal capitation payment of 1,200 Baht (~$35) to provincial hospitals based on the number of people living in the province. Second, the program also sought to reduce the financial burden of health expenses. Therefore, out-of-pocket expenditures were replaced with a 30 Baht copay ($0.75) so that healthcare provision was primarily financed via the capitation payments to the hospital instead of user fees.
The 30 Baht program replaced two previously existing programs. First, roughly 30% of the population were enrolled in the Medical Welfare Scheme (MWS) that theoretically provided free access to healthcare for the poor based on income eligibility requirements. However, this program was significantly under-funded with reimbursements to public hospitals of roughly 250 Baht (~$6) per enrollee per year (Damrongplasit and Melnick (2009); Donaldson et al. (1999)). The MWS group were merged into the 30 Baht program and, as a result, the funding to hospitals to provide for their care increased fourfold to 1,200 Baht.1 Second, the previously uninsured whose incomes were too high to qualify for the MWS program, (~50% of the population) saw a reduction in their cost of care to 30 Baht. Instead of receiving out of pocket payments, the hospital received a fixed capitation of 1,200 Baht to cover the cost of their care. In short, the policy made access to healthcare in public facilities independent of ones’ financial situation and led to an equalization of healthcare access for rich and poor.
We begin by investigating the impact of the 30 Baht reform on medical utilization. Using data on inpatient utilization, we find that the program led to a moderate increase in healthcare utilization for the previously uninsured. However, we find a larger impact for those who were previously insured by the MWS program for the poor, for whom there was rising hospital reimbursement. The impacts for both groups are concentrated in public hospitals, which is consistent with the targeting of the funds. Moreover, for the previously uninsured we find evidence of a switch in utilization from private to public facilities, consistent with a response to the decrease in relative price of care in public versus private facilities induced by the 30 Baht program. Finally, we show that the increase in utilization for the MWS enrollees is especially large amongst infants and women aged 20–30.
We then turn our focus to infant mortality drawing on vital statistics records from the Ministry of Public Health. These contain information on the total number of births and deaths in each year within each province. Prior to 30 Baht, we document a robust significant positive relationship between the fraction of a province that enrolled in the MWS program and the infant mortality rate; poor provinces had higher infant mortality rates. But, after the 30 Baht program, this correlation evaporates to a precisely estimated zero. We conduct a placebo test showing that the program does not lead to any reported change in the number of births, which suggests time-varying measurement error is not driving our results. Moreover, the evaporation of this relationship occurs precisely at the point of introduction of the 30 Baht program, consistent with the increased access to medical care to the poor through the 30 Baht program driving the results.
This paper relates to several literatures. First, our paper builds on a large literature studying public health systems the impact of health reforms in developing countries (Dow et al. (1997); Gertler (1998); Dow and Scmeer (2003); Thornton et al. (2010)). Much of this literature focuses on the impact of lowering out of pocket healthcare costs (Dow et al. (1997); Dow and Scmeer (2003); Thornton et al. (2010)). However, our results highlight the fundamental importance of the supply-side design of programs for the poor.2 Despite no change in the formal out-of-pocket price charged to the poor, the supply-side reforms led to large increases in utilization; in contrast we find smaller impacts on those whose out-of-pocket fees were reduced to 30 Baht. Heuristically, the supply side response mattered more than the demand side: reducing the cost of medical care had less of an impact than providing extra money to hospitals. This suggests the supply-side levers and reimbursement schemes are of first order importance in designing health reforms. It also suggests doctors and hospitals in Thailand had the capability of limiting supply through non-price mechanisms or rationing.3
Second, our paper builds on a large literature attempting to understand the relationship between income and infant mortality. Like many countries, infant mortality in Thailand has fallen over the past decades as economic development has increased (Vapattanawong et al. (2007)). However, it is unclear whether this reduction is due to a direct result of the increased incomes versus the result of factors, like access to medical care, which are directly addressable through public policy. Exploiting the yearly frequency infant mortality vital statistics data, our results isolate the role of healthcare policy in preventing infant mortality. The results suggest healthcare policy can have large impacts and are consistent with other literature suggesting many infant deaths are quite preventable (Dupas (2011)).
Our paper proceeds as follows. In Section 1 we present background on the 30 Baht program. Section 2 presents estimates of the impact of the program on healthcare utilization. Section 3 examines the impact of the program on infant mortality. Section 4 concludes. We also provide several additional robustness tests in the Appendix.
1 The Thai 30 Baht Program
1.1 Background
In 2001, Thailand became one of the first middle income countries to implement a universal health coverage scheme. The 30 Baht program was a primary component of the political platform of Thaksin Shinawatra, a populist leader who came to power in February 2001. The 30 Baht program had two key features. First, it provided universal access to care in public facilities for a cost (copay) of 30 Baht (~$0.75) per visit. Second, it equalized the per-person funding available for healthcare in public hospitals: the program replaced pre-existing public financing schemes with a fixed per capita budget of 1,200 Baht (~$30) to each provincial public hospital system.4
The program began with several pilot provinces in early 2001, expanding to more pilots throughout the summer and covering all provinces by November 2001. In order to understand the potential impact of the program, it is important to understand what it replaced. Prior to the 30 Baht program, much of the relatively poorer population enrolled in the Medical Welfare Scheme (MWS). This program provided free care in public facilities for the poor, young (ages 1–15) and elderly (ages 60+).5 Prior to 30 Baht, this program was generally seen as underfunded, with a global budget of only 250 Baht (~$6) per enrollee per year (Donaldson et al. (1999)). When the 30 Baht program began in 2001, MWS enrollees were automatically enrolled in the 30 Baht program, but waived of its 30 Baht copay. As a result of absorbing this program into the 30 Baht program, funding to public hospitals to care for the poor increased from a global budget of 250 Baht per enrollee to the 1,200 Baht per enrollee, a four-fold increase (~$25). Thus, the 30 Baht program did not change the price faced by the poor in public facilities (it was already zero). Rather, it addressed the supply side by increasing funding to public facilities with the intention of providing more healthcare to the poor.6
In addition to the 30% of the population covered by the MWS, about 20% of the Thai population was enrolled in two employer-based insurance programs that were left largely untouched by the 30 Baht program. The Civil Servant Medical Beneficiary Scheme (CSMBS) provided free care to civil servants and their families in public facilities. The Social Security Scheme (SSS) provided free care to other formal sector workers (program was mandatory for formal sector employers). Because these programs were left unchanged around the introduction of 30 Baht, the combination of these two groups will provide a natural control group for portions of our analysis.7
The remaining 50% of the population was not covered under any of the aforementioned programs. However, they did have access to a previously existing government program, the 500 Baht program, which allowed households to obtain free care in public facilities for an upfront cost of 500 Baht per household per year. The central government matched the 500 Baht payment to the local hospital, so that total hospital revenues were 1,000 Baht per enrollee.8 About two-fifths of the uninsured (or 20% of the total population) took up this option.
Thus, for the previously uninsured (i.e. those not covered through their employer and those who do not qualify for MWS care) the 30 Baht program lowered the cost of public healthcare from a maximum of 500 Baht per household per year to 30 Baht per disease (a cost reduction in the vast majority of cases). From the public hospital’s perspective the 30 Baht program replaced these out-of-pocket payments and 500 Baht payments (which were matched with an additional 500 Baht from the central government) with the 1,200 Baht per person capitation.
Figure 1 summarizes the three groups in the population and the way in which each was affected by the 30 Baht program. The UNINS faced a price reduction for care but also provided less revenue to hospitals. The MWS faced no change in the price of obtaining care, but the funding to hospitals significantly increased. The Control group (CSMBS and SSS) had no formal change to their programs around the introduction of 30 Baht.
Figure 1.
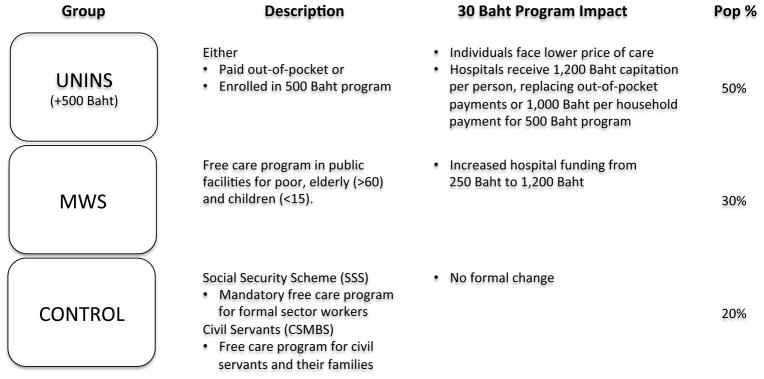
Population Groups Impacted by 30 Baht
Summary of “Supply” and “Demand” Effects
Since the 30 Baht program affected both the out-of-pocket payment requirements (“demand”) and the hospital funding arrangements by instituting capitated payments independent of utilization (“supply”), the net impact on utilization depends on how these two forces play out. For the previously uninsured, their reduction in out-of-pocket payments in public facilities should increase their demand. However, their supply of healthcare may be affected by the inability of hospitals to receive marginal payments for the provision of their care, instead receiving a capitation. Thus, whether their utilization increases or decreases depends on which force is stronger, supply or demand.
For the MWS, their out-of-pocket payment requirements never change. They were technically eligible for free care prior to and after the 30 Baht program. However, the willingness to supply such care may increase because the hospitals now receive a significant funding increase to provide care to this group. Thus, to the extent to which the funding increases the supply of care to the MWS, we expect their utilization to increase.
2 Utilization Impact
2.1 Data and Sample
We begin our analysis of the 30 Baht program with its effects on inpatient utilization. We focus on the impact on both the MWS population and a combined group of previously uninsured and 500 Baht users. Because their ex-ante choice sets were identical, we pool the previously uninsured with the 500 Baht users for our analysis. Our primary empirical approach will consider a difference-in-difference estimation that exploits the fact that the SSS and CSMBS programs were unaffected by the reforms.
We use data from the Health and Welfare Survey (HWS) from years 2001 and 2003–2005.9 This survey is a national cross section of all 76 Thai provinces, with roughly equal sized samples from each province. In 2001, the survey is conducted in April/May, roughly 5 months before the beginning of the 30 Baht program in November. However, six provinces took part in a pilot study which was already underway in April/May of 2001; we therefore exclude these provinces in our analysis since we do not have data prior to the introduction of the 30 Baht program for these provinces.10
The survey provides a wide range of health utilization and insurance coverage information. In particular, respondents are asked whether or not they have been admitted as an inpatient in the last 12 months, which will be our measure of utilization.11 The survey also provides information on insurance status, including whether an individual was part of the MWS, SSS/CSMBS, or UNINS in 2001, and whether an individual was part of SSS/CSMBS or 30 Baht in 2003–2005. Although the survey is not a panel, it distinguishes between individuals enrolled in the free care (no copay) version of the 30 Baht program (i.e. the “roll-over” portion of the MWS) from those who must pay the 30 Baht copay (i.e. those who were previously enrolled in the MWS program). This allows us to classify individuals into the three groups (UNINS, MWS, CONTROL) in each year of the survey.
Table 1 presents the summary statistics of our sample, broken out by group. We provide the mean age, fraction female, and fraction employed (in any paying work, formal or informal) before and after the 30 Baht program began (i.e. 2001 versus 2003–2005 in our sample). We also present the fraction of the sample each group represents both pre and post 30 Baht.
Table 1.
Summary Statistics
| Group | Pre-30 Baht | Post 30-Baht | p-value (Pre Post) | p-value (D-in-D) |
|---|---|---|---|---|
| CONTROL | ||||
| Age | 35.8 | 37.7 | 0*** | |
| Female | 0.530 | 0.528 | 0.57 | |
| Employed | 0.682 | 0.711 | 0*** | |
| % of Sample | 0.201 | 0.226 | 0*** | |
| UNINS1 | ||||
| Age | 32.5 | 33.4 | 0*** | 0*** |
| Female | 0.523 | 0.526 | 0.12 | 0.204 |
| Employed | 0.631 | 0.657 | 0*** | 0.662 |
| % of Sample | 0.497 | 0.485 | 0.106 | |
| MWS | ||||
| Age | 29.7 | 30.5 | 0.021** | 0.002*** |
| Female | 0.525 | 0.523 | 0.636 | 0.93 |
| Employed | 0.310 | 0.318 | 0.39 | 0.02** |
| % of Sample | 0.302 | 0.289 | 0.062* | |
| Sample Size | 200,926 | 182,543 | ||
Includes individuals who owned 500 Baht cards in 2001
Note: CONTROL = SSS + CSMBS members; UNINS = those not qualifying for CSMBS, SSS, or MWS
Standard errors clustered at the province level (70 provinces with data pre an post 30 Baht)
In general, the means are similar, although not identical. The control group experiences a significant increase in age (~2 years) which is larger than the other groups (~1 year for MWS and UNINS). The fraction employed increases for the CONTROL and UNINS groups by about 2.5–3pp but less for the MWS (0.7pp). Gender shares remain virtually unchanged in each group over time. We will be able to control for these demographic variables in our regressions and assess the robustness of our results to their inclusion or exclusion. In general, the relative sizes of each group remains qualitatively similar before versus after 30 Baht, although we do find evidence of a bit of an increase in the size of the CONTROL group (those obtaining insurance through their employer) relative to the other two groups.12
2.2 Specification and Results
Table 2 presents the means of 12 month inpatient utilization rate for the CONTROL, UNINS, and MWS groups, broken out separately before and after the beginning of the 30 Baht program in 2001. The top row shows that overall inpatient utilization increased by 0.36pp, or roughly 5.4% over the pre-30 baht utilization rate of 6.65pp. Thus, the simple time series estimate suggests the 30 Baht program led to an increase in overall inpatient utilization.
Table 2.
Inpatient Utilization (12mo)
| Group | Pre 30 Baht | Post 30 Baht | Difference |
|---|---|---|---|
| All Groups | 0.0664921 (.0018886) | 0.0701205 (.0023431) | 0.0036** (0.0017) |
| CONTROL | 0.0792515 (.0033922) | 0.07889 (.004141) | −0.0004 (0.0027) |
| UNINS | 0.0585472 (.0018215) | 0.0606406 (.0021355) | 0.0021 (0.0017) |
| MWS | 0.0710707 (.0023581) | 0.0791735 (.0022474) | 0.0081*** (0.0027) |
| Difference | |||
| UNINS - CONTROL | −0.0207*** (0.0026) | −0.0182*** (0.0026) | 0.0025 (0.0023) |
| MWS - CONTROL | −0.0082** (0.0035) | 0.0003 (0.0038) | 0.0085*** (0.0032) |
Standard errors clustered by province (70 provinces)
p<.01,
p<.05,
p<.10
Consistent with the aims of the program of expanding healthcare access to the poor, we find that the increase in overall utilization is primarily driven by an increase in utilization by the MWS group. The utilization rate for the MWS group increases from 0.0711 to 0.0792, a difference of 0.0081 (p<0.01). For the previously uninsured, we find a modest, yet statistically insignificant increase of 0.0021 (~3% of baseline utilization of 0.0585). Finally, we find no significant change for the control group (−0.0004), which is consistent with the fact that these programs were left in tact around the introduction of the 30 Baht program.
The bottom two rows show the estimated difference in utilization between the treatment groups and the CONTROL group. The UNINS have lower utilization than the CONTROL group both before (−0.0207) and after (−0.0182) the introduction of 30 Baht. This implies a difference-in-difference estimate of 0.0025 (p>0.10), which suggests the 30 Baht program had a modest but statistically insignificant impact on inpatient utilization. For the MWS group, prior to 30 Baht this group had significantly lower utilization rates than the CONTROL group (−0.0085); after 30 Baht, the difference is positive and statistically insignificant (0.0003; p>0.10). This implies a difference-in-difference estimate of 0.0088 (p<0.01), which implies that the 30 Baht program led to a 12% increase in utilization for the MWS group.13
The analysis heretofore has not included any controls for demographics, which are potentially important given the nonzero changes in sample composition outlined in Table 1. We estimate regressions of the form
| (1) |
where subscripts i index individuals, g indexes insurance groups (e.g. UNINS, MWS, CONTROL), and t indexes year (2001, 2003, 2004, 2005). The variable inpatigt is an indicator for inpatient utilization in the past 12 months, αt is a year fixed effect, κg is a group fixed effect (MWS, UNINS, CONTROL), and Xigt is a set of demographic control variables including age deciles interacted with gender and 15 household income bins14. The variables UNINSg and MWSg are indicators for the previously uninsured and MWS group, and Post30t is an indicator for years 2003–200515. The coefficient βUNINS and βMWS capture the difference-in-difference estimate of the impact of the program on the previously uninsured and the MWS group.
The results in Table 3 largely support the findings of the difference-in-difference spec-ification of a large increase in utilization for the MWS and a more modest effect on the previously uninsured. Our estimate of 0.0086 (p<0.01), an increase of 12%, for the MWS group in column I remains very similar to the results in Table 2. For the UNINS, we now estimate a slightly larger (and now statistically significant) increase in inpatient utilization of 0.0048 (p<0.05), an increase of 8% over the baseline utilization rate of 0.0585 in 2001.
Table 3.
Inpatient Utilization (12mo)
| Group | I | II | III | IV | V | VI |
|---|---|---|---|---|---|---|
| Inpatient Utilization | Inpatient Utilization | Inpatient Utilization (Public) | Inpatient Utilization (Private) | Inpatient (Women & Child Sample) | Inpatient (non-women & child) | |
| Individual Classification | ||||||
| UNINS* Post30 | 0.0049** (0.0023) | 0.0045* (0.0023) | 0.0069*** (0.0021) | =0.0017* (0.0010) | 0.0065 (0.0064) | 0.0053** (0.0025) |
| MWS* Post30 | 0.0088*** (0.0031) | 0.0078** (0.0031) | 0.0083*** (0.0031) | 0.0009 (0.0013) | 0.0216** (0.0098) | 0.0087** (0.0033) |
| Mean Dep Var (03=05) | 0.0720 | 0.0720 | 0.0621 | 0.0096 | 0.1000 | 0.0689 |
| Sample Size (# Respondents) | 383469 | 383469 | 383469 | 383469 | 40834 | 342635 |
| Sample Size (# Clusters) | 70 | 70 | 70 | 70 | 70 | 70 |
| Controls | ||||||
| Year FE | X | X | X | X | X | X |
| Group FE | X | X | X | X | X | X |
| Age, Gender, Income | X | X | X | X | X | X |
| Province FE | X | |||||
| Province x Year FE | X | |||||
Standard errors clustered by province
p<.01,
p<.05,
p<.10
Column II adds province-by-year fixed effects which capture potential provincial-level supply or demand shocks, such as the opening of a new private clinic or an outbreak of sickness. Since these fixed effects may be soaking up causal impacts of the program (e.g. a private clinic may be less likely to open because of the 30 Baht program), we do not include these controls in our primary specification. But it is re-assuring that including these additional controls does not significantly affect our results. We estimate an increase of 0.0076 (p<0.05) for the MWS and 0.0044 (p<0.05) for the previously uninsured, statistically indistinguishable from our results without province-by-year fixed effects.
Private vs. Public Utilization
The 30 Baht program provided free care only in public, not private hospitals. Columns III and IV present separate estimates for inpatient utilization in public and private hospitals. Re-assuringly, we find the increase in utilization for the MWS group is entirely concentrated in public utilization (0.0081, p<0.01) as opposed to private utilization (0.0009, p>0.10).
Moreover, this breakout reveals that the program led to a substitution of public for private utilization amongst the previously uninsured: we find an increase of 0.0068 (p<0.01) in public utilization and a decrease of −0.0017 (p<0.10) in private utilization. This is consistent with public options becoming relatively less expensive as a result of the 30 Baht program.
Women and Children
In addition to analyzing the impact on each group as a whole, we can also analyze the impact for subgroups. Setting the stage for our subsequent focus on infant mortality, we focus on women aged 20–30 and infants aged 0–1. Columns V present results of the difference-in-difference specification restricted to a sample of only women aged 20–30 and infants; Column VI presents the results from the complementary sample of those who are neither women aged 20–30 or infants.
The results suggest that the 30 Baht program had a disproportionate impact on the utilization of women of childbearing age and infants, especially amongst the MWS group. In particular, among the MWS we find an increase of 0.0217 (p<0.05) for women aged 20–30 and infants, compared to an increase of 0.0085 (p<0.05) for the rest of the MWS group. We also find a larger increase amongst women aged 20–30 and infants for the UNINS (0.0065 versus 0.0052), although the increase for women and children is not statistically significant (arguably due to the smaller sample size).
Summary
In short, the utilization results are consistent with the aims of the program to increase access to medical care for the poor. We find modest increases in utilization for the UNINS, and a switch from private to public hospitals consistent with the demand increase resulting from the reduction in out-of-pocket payments required in public hospitals. However, our results suggest the largest impacts on the poor (MWS) population. Despite not facing any change in their out-of-pocket payment requirements, our results suggest the supply-side reforms of the program (and in particular the fourfold increase in funding) led to a significant increase in access to care for the poor. Moreover, we find especially large increases for women aged 20–30 and children under 1 year old, motivating our subsequent analysis of the impact of the program on infant mortality.
3 Infant Mortality Specification and Results
3.1 Data Sources
We now turn to an analysis of the effect of the program on infant mortality. We draw on provincial-level vital statistics records compiled from death certificate registries, made available to us by the Thailand Ministry of Public Health for years 1997 through 2008. Thailand has a relatively high-quality vital statistics registry, especially compared to other low and middle-income countries (Setel et al. (2007)). This makes it a well-suited environment for assessing the impact of the expansion of medical access to the poor on infant mortality. However, it is widely recognized that vital statistics registries do not fully capture all infant mortality. Existing literature has documented under-reporting of infant deaths in Thailand, especially among deaths occurring outside of hospitals (Tangcharoensathien et al. (2006)).16 For the present analysis we ignore the potential impact under-reporting, but in Section 3.3.1 and Appendix C we return to a detailed discussion of its potential impact on our results.
3.2 Vital Statistics Analysis
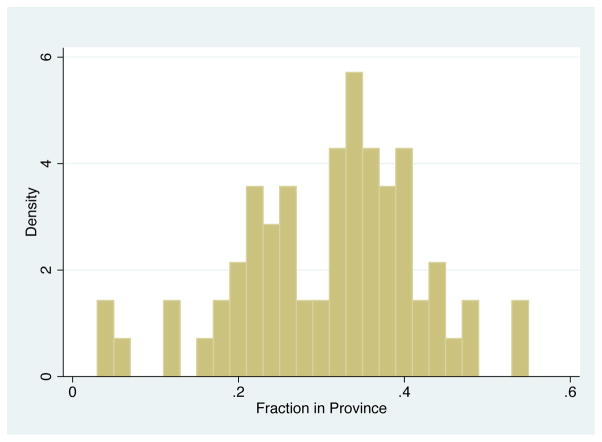
We begin with an analysis of the vital statistics records. Although our utilization data was at the individual level, the vital statistics records are only made available to us to the province-by-year level. To relate the infant mortality rate to the potential impact of the 30 Baht program, we use the HWS data to construct a variable FracMWSp equal to the fraction of a province enrolled in the MWS program in 2001. Figure 2 plots the distribution of , showing substantial variation with a std deviation of 0.11, which reflects the unequal distribution of income across provinces.17
Figure 2.
Histogram of FracMWS in 2001 (Pre 30 Baht)
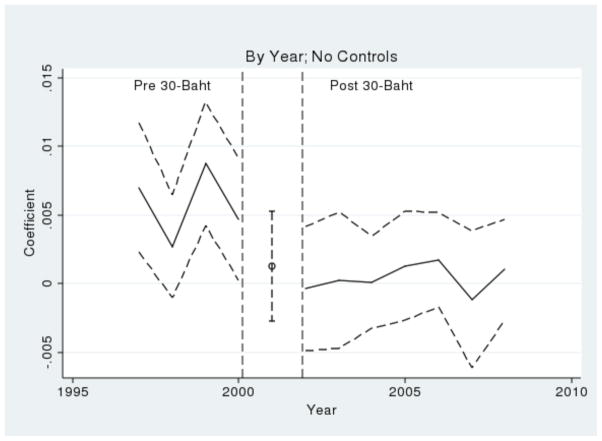
We first document the historical pattern of infant mortality rates across provinces. We estimate separate regressions for each year t = 1997,…,2008 of the form
where in f antmortpt is the 1-year infant mortality rate (per 1000 births) in province p in year t. The coefficient captures cross-provincial the relationship between the fraction enrolled in the MWS program in 2001 and the infant mortality rate (in percent deaths per births) of the province in year t.
Figure 3 plots the coefficients, , for each year, along with their 95% confidence interval. The cross-provincial relationship within Thailand prior to 30 Baht exhibits a positive relationship between poorer areas (higher FracMWS) and higher infant mortality. However, after 30 Baht this relationship evaporates; the coefficients for are near zero for every year after 30 Baht18. This suggests the 30 Baht program, and the dramatic increase in funding for the MWS program removed the historical cross-provincial correlation between FracMWS and infant mortality.
Figure 3.
Effect of Fraction MWS on Infant Mortality
Regression Specification
We now turn to a regression specification given by
| (2) |
We also include current and lagged provincial GDP levels as controls. Our primary specification focuses on a 2-year window around the introduction of 30 Baht (1999–2003) and excludes the year 2001 (since 30 Baht began in the middle of this year). We include year fixed effects and province fixed effects.
The coefficient βIn f ant captures the equalizing force of the 30 Baht program. It measures how much the 30 Baht program reduced infant mortality in areas with a high fraction of MWS (i.e. poor) relative to those with a lower fraction of MWS. In Appendix B, we show this measures the reduction in infant mortality on the MWS group under the assumption of no impact on the UNINS or control group.19 In the absence of this assumption, the coefficient includes any spillovers on the non-MWS in high versus low FracMWS provinces.
The results for βIn f ant are presented in Table 4. We estimate a significant coefficient of −.0065 (p<0.01). This suggests that a 10% increase (~1sd) in the fraction enrolled in MWS prior to 30 Baht leads to a reduction in infant mortality of 0.65 per 1000 births.
Table 4.
Infant Mortality Rate (Provincial Level Vital Statistics)
| Dependent Variable | I | II | III | IV | V | VI | VII |
|---|---|---|---|---|---|---|---|
| Infant Mort (% of Births) | Infant Mort (% of Births) | Infant Mort (% of Births) | Infant Mort (% of Births) | Infant Mort (% of Births) | Infant Mort (% of Births) | Births (1000s) | |
| FracMWS* Post30 | −0.0065*** (0.0023) | −0.0068*** (0.0022) | −0.0054* (0.0030) | −0.0054*** (0.0020) | −0.0082*** (0.0028) | −0.0076** (0.0032) | −0.2426 (1.8170) |
| Specification | |||||||
| Year FE | X | X | X | X | X | X | X |
| Province FE | X | X | X | X | X | X | |
| Provincial GDP | X | X | X | X | X | ||
| Prov GDP (Lagged) | X | X | X | X | X | ||
| Province Trends (Linear) | X | ||||||
| Median Regression | X | ||||||
| FracMWS | X | ||||||
| Sample Range | 1999–2003 (excl 2001) | 1999–2003 (excl 2001) | 2000–2002 (excl 2001) | 1997–2005 (excl 2001) | 1997–2005 (excl 2001) | 1999–2003 (excl 2001) | 1999–2003 (excl 2001) |
Standard errors clustered by province (76 provinces)
p<.01,
p<.05,
p<.10
The remaining columns show the robustness of the coefficient to alternative specifications. Column II removes controls for current and lagged provincial GDP. Column III contracts the analysis to a 1-year window (2000–2002) and shows that the impact of the 30 Baht program remains quite stable. Column IV expands the analysis to a 4 year window (1997–2005) and Column V adds province-specific linear trends. With province-specific linear trends in this expanded timeline, the coefficient increases slightly to −0.0082. This suggests our estimates are not driven by underlying heterogeneous geographical trends in infant mortality. Column VI estimates a median regression, as opposed to the standard mean regression, which is generally more robust to the presence of outliers. We estimate a coefficient of −7.6486 (p<0.05) in the median regression specification, statistically indistinguishable from our estimate of −6.4512 in the mean regression.
3.3 Threats to Identification
3.3.1 Measurement Error
It is of course a concern that infant mortality is under-reported to the vital statistics registry.20 To address potential concerns, we conduct three analyses. First, one may be concerned that there was some other change in vital statistics recording around the introduction of 30 Baht or that the program increased general reporting of deaths and births. To test this, we ask whether the 30 Baht program had any impact on recorded births in the vital statistics registry. Column VI reports results from a regression of recorded births using our primary specification in equation (2). The results show that we cannot reject the null hypothesis of no relationship between the 30 Baht program and recorded births. This is reassuring and suggests results are not driven by changes in vital statistics recording around the introduction of 30 Baht.
However, one may still be concerned that deaths may be differentially affected by reporting errors than births. Therefore, we consider the theoretical impact on our results of three potential sources of under-reporting error. All of these forms of measurement error render our estimate a lower bound for the equalizing impact of the 30 Baht program on infant mortality.
First, suppose under-reporting is a level effect, so that where is the vital statistics report and at > 0 is the under-reporting level by year. In this case, at will be absorbed into the time fixed effect and will not introduce any bias into the estimates of βIn f ant. Second, suppose under-reporting is proportional, so that for some proportion γ > 1. In this case, each recorded infant death represents more than 1 infant deaths, so that the estimate of 0.0065 is actually a lower bound of the true equalizing impact of the program. Third, suppose the 30 Baht program increases the reporting of infant mortality deaths, as may be expected because of the increase in hospital utilization and the higher propensity to report infant deaths if they occur in a hospital (Tangcharoensathien et al. (2006)). Since utilization increases were largest amongst the MWS group, this type of measurement error would lead to an increase in reporting of MWS infant deaths under the 30 Baht program. This renders our estimate of 0.0065 a further understatement of the true βIn f ant.
In addition to this theoretical assessment, we also pursue all possible alternative measures of Thai infant mortality. To our knowledge, the only other national dataset containing infant mortality data in Thailand in this time period are the 2000 Census and the 2005–6 Survey of Population Change. Each of these surveys ask summary birth histories: married women are asked (a) how many children they have ever had and (b) how many of these children have died. Because these surveys do not ask about when these deaths occurred, they are not ideal for our analysis of a high-frequency impact of the 30 Baht program. Therefore, we present these results in the Appendix, as opposed to the main text. Despite these concerns, in Appendix C we focus on a sample of women aged 25 and under and show that our results using the vital statistics are consistent with the results from these summary birth history data.
3.3.2 Other Thaksin Programs
A remaining identification concern is that there was something else implemented in 2001, aside from the increased access to care associated with the 30 Baht program, that led to the relative reduction in infant mortality in high MWS versus low MWS provinces. Most notably, Thaksin came to power in 2001 under a populist, pro-poor platform. The 30 Baht program was the cornerstone of the healthcare policy, but Thaksin also implemented various economic policies to promote economic growth for the poor. In particular, the so-called “Million Baht Fund”, analyzed in detail in Kaboski and Townsend (2009, 2011), provided 1 million baht to each village for use in micro-loans. Yet these loan funds were provided uniformly across provinces, in contrast to the 30 Baht program which led to a differential change in funding correlated with the fraction MWS in the province. Other concerns may simply be that Thaksin implemented other policies which led to economic expansion in poorer areas (i.e. with higher MWS). But, as shown in Table 4, our results are quite robust to the inclusion of current and lagged provincial-level GDP variables, suggesting that changing economic conditions does not explain the sharp reduction in infant mortality around the introduction of the 30 Baht program. Thus, our results do not appear to be driven by other contemporaneous factors correlated with the fraction of MWS enrollees in each province.
3.4 Interpretation: Equalization versus Aggregate Reduction
Our results document a sharp equalization of infant mortality rates across provinces between 2000 and 2002, consistent with the increased access to care for the poor leading to a reduction in their infant mortality rates. Our analysis relies on cross-sectional variation, and it allows for time-series changes in the infant mortality rate due to various within country factors, including time-varying changes in aggregate measurement error. As a result, we cannot extrapolate our analysis to an implied aggregate reduction in infant mortality without additional assumptions.
One natural assumption to make is that areas with no MWS (FracMWS = 0) have no change in infant mortality. Since the MWS comprise roughly 30–35% of the population, this implies an aggregate reduction in infant mortality of roughly 2 per 1,000 births (30%*6.5=1.95). This can be compared either to the World Development Indicators estimates of infant mortality rates of 15/1,000 in 2000 (suggesting a national reduction of 13%) or to the vital statistics sample mean of 6.2/1,000 in 2000 (suggesting a national reduction of ~30%).
However, we are cautious to make strong claims about the implied impact on aggregate infant mortality. Indeed, there is no significant drop in the aggregate infant mortality rate in the vital statistics registries. To be sure, the expansion of healthcare access and increase in services associated with the 30 Baht program could be driving an aggregate increase in reported infant mortality. However, our empirical analysis does not rule out the potential that the program led to an increase in infant mortality in richer areas that did not experience the large budgetary windfall from the 30 Baht program. However, there are two reasons to believe the equalization in infant mortality did not come at the expense of infant mortality in richer areas. First, healthcare utilization increased across the country, including in richer areas; this suggests the supply of care did not contract in rich areas. Second, our casual interviews with doctors and hospitals in richer areas of Thailand suggest they do not believe that the program led to a significant decrease in the quality of their care provided or a significant rise in their infant mortality rates. In short, our empirical strategy robustly identifies an equalization of infant mortality rates across Thailand, consistent with the budgetary equalization of resources. This equalization represents suggestive evidence of a large aggregate reduction in infant mortality of 13–30%.
4 Conclusion
Our results suggest that supply-side healthcare financing reforms can increase access to healthcare and combat infant mortality among the poor. Indeed, the sharp equalization in infant mortality observed between 2000 and 2002 is consistent with the fact that the most common causes of infant mortality in the world are from treatable diseases, such as dehydration (associated with diarrhea), pneumonia, and infection (Dupas (2011)). Given the relatively large disparities in infant mortality that were reversed through the program, our results suggest that improved access to medical services could go a long way to improve the large disparities in infant mortality rates both across and within countries.
Supplementary Material
Acknowledgments
We thank the Townsend Thai Family Research Project and the University of Thai Chamber of Commerce for support and research assistance. We also thank the Thai National Statistics Office for data availability. Hendren acknowledges support from the NSF Graduate Research Fellowship and the NBER Health and Aging Fellowship, under NIA grant T32-AG000186. Townsend acknowledges support from the NICHD and the Bill and Melinda Gates Foundation through a grant to the Consortium on Financial Systems and Poverty at the University of Chicago.
Footnotes
An earlier version of this paper relying on a subset of data presented herein was circulated under the title “Demand and Reimbursement Effects of Healthcare Reform: Health Care Utilization and Infant Mortality in Thailand”.
The MWS enrollees were also waived of the 30 Baht fee so that they did not face an increase in the cost of care.
Our finding that the supply-side is important is qualitatively consistent with the depiction of rural health-care provision in India in Banerjee et al. (2004).
It is often doctors, moreso than patients, that choose treatment paths.
Public hospitals in Thailand are managed primarily at the provincial level. Each province has one major hospital, along with numerous smaller hospitals (usually 1 per Amphoe/County) and clinics.
The program also covered the handicapped (all ages) and religious and community leaders. The definition for eligibility based on income (the relevant eligibility criteria for most members) was an income threshold of 2,000 Baht per person or 2,800 Baht per household (~$2.25/day)
In general, individuals were encouraged to go to their geographically local hospitals (to which the capitation funding was provided), and each person’s enrollment card listed the local hospital. However, individuals were allowed to use other hospitals outside their geographic region if they had a legitimate reason to do so (e.g. traveling). In this case, the attended hospital could seek reimbursement from the patient’s home province.
A very small fraction (~1%) of the population, primarily upper class workers in Bangkok, has private insurance coverage. We exclude this group in our healthcare utilization analysis.
Not every service was free under the 500 Baht program or the 30 Baht program (e.g. dialysis was not covered in 2001). The set of covered procedures for 30 Baht was essentially the same set of procedures covered under the 500 Baht and MWS programs.
We thank our partners at the University Thai Chamber of Commerce for compiling and translating this survey into English.
An additional 15 provinces began a pilot study in June of 2001 but before the full implementation in November of 2001. However, the HWS was completed prior to the beginning of this pilot study in these 15 provinces, and thus we include these provinces in our analysis.
The surveys also provide information for outpatient utilization and the presence of sickness, however the recall window changes from 2 weeks in 2001 to 1 month in years 2003–2005. Since this recall window changes over the same time period as the start of the 30 Baht program, we focus our results on inpatient utilization. In Appendix A, we present the results for outpatient utilization.
Although this could be a result of the 30 Baht program, it is also consistent with the general economic growth in Thailand over this time period, as more people enter the formal labor force.
Because we focus on a relatively intensive measure of utilization (inpatient), one may wonder whether our results are picking up switching from less intensive (outpatient) outpatient utilization or a general increase in all forms of utilization. In Appendix A, we present the results for the outpatient utilization, which changes the recall window from 2 weeks to 1 month in the post 30 Baht period. We show that the MWS group experiences a proportionally larger increase in outpatient utilization relative to the control group. Although we are concerned about issues of changing recall bias on the results, and thus do not include them in the main text, the results are consistent with the story that access to both inpatient and outpatient public healthcare was significantly expanded for the MWS.
One concern with including household income is that it may be a causal outcome of an increase in health-care utilization. Our results do not change significantly with or without income controls.
We aggregate these post 30 Baht years for statistical power. Separate estimates by year are very similar but have wider standard errors.
In the Appendix, we present the summary statistics for the mean infant mortality rate in our sample for each year. These are fluctuating and slightly increasing over time and range from 6 and 7.3; in contrast, the World Bank Development Indicators which suggest infant mortality rates closer to 15/1,000 in 2001 and 12/1,000 in 2007 (World Bank (2001,2007)). We discuss the potential impact of time-varying measurement error in Section 3.3.1.
We also constructed a measure of the fraction in each province that falls in the UNINS category, FracUNINS; however, there is very little variation in the size of the control group across provinces; thus the correlation between FracUNINSp and FracMWSp is −0.85. Since we only have 76 provinces, we do not have enough power to separate effects on the uninsured and MWS. We therefore analyze the relationship between the infant mortality rate and the fraction enrolled in the MWS program, FracMWSp, but will discuss the impact of not including FracUNINSp on the interpretation of the results.
A joint test for all post 30 Baht coefficients equal to zero cannot be rejected at p = 0.10.
If there is a positive effect of the program on the UNINS as well, then βVital is an under-estimate of the impact of the program on infant mortality of the MWS (because of the negative correlation between fracMWS and fracUNINS). Conversely, if there are spillovers onto the uninsured and control groups in areas with high MWS, then the coefficient captures the total average effect on all groups, but does not isolate the effect on the MWS group.
Our mean infant mortality rate in our sample is 6.5/1000 births, which is less than imputed estimates used in the World Bank Development Indicators.
References
- Banerjee A, Deaton A, Duflo E. Health, health care, and economic development. The American economic review. 2004 May;94(2):326–330. doi: 10.1257/0002828041301902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damrongplasit K, Melnick GA. Early results from thailand’s 30 baht health reform: something to smile about. Health Affairs. 2009;28(3) doi: 10.1377/hlthaff.28.3.w457. [DOI] [PubMed] [Google Scholar]
- Donaldson D, Pannarunothai S, Tangcharoensathien V. Health financing in thailand technical report. Health Management and Financing Study Project, ADB 1999 [Google Scholar]
- Dow W, Gertler P, Schoeni RF, Strauss J, Thomas D. Health care prices, health and labor outcomes: Experimental evidence. Paper, RAND - Labor and Population Program 1997 [Google Scholar]
- Dow WH, Scmeer KK. Health insurance and child mortality in costa rica. Social Science and Medicine. 2003 Sep;57(6):975–986. doi: 10.1016/s0277-9536(02)00464-1. [DOI] [PubMed] [Google Scholar]
- Dupas P. Health behavior in developing countries. Annual Review of Economics 2011 Jan; [Google Scholar]
- Gertler P. On the road to social health insurance: the asian experience. World Development. 1998;26:717–732. [Google Scholar]
- Kaboski J, Townsend R. The impacts of credit on village economies. MIT Department of Economics Working Paper No 09-13. 2009 doi: 10.1257/app.4.2.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaboski J, Townsend R. A structural evaluation of a large-scale quasi-experimental microfinance initiative. Econometrica, Forthcoming. 2011 doi: 10.3982/ECTA7079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porapakkham Y, Rao C, Pattaraarchachai J, Polprasert W, Vos T, Adair T, Lopez A. Estimated causes of death in thailand, 2005: implications for health policy. Population Health Metrics. 2010 May;8(1):14. doi: 10.1186/1478-7954-8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setel PW, Macfarlane SB, Szreter S, Mikkelsen L, Jha P, Stout S, AbouZahr C. Who counts? (1): A scandal of invisibility: Making everyone count by counting everyone. The Lancet. 2007 doi: 10.1016/S0140-6736(07)61307-5. [DOI] [PubMed] [Google Scholar]
- Tangcharoensathien V, Faramnuayphol P, Teokul W, Bundhamcharoen K, Wibulpholprasert S. A critical assessment of mortality statistics in thailand: potential for improvements. Bulletin of the World Health Organization. 2006;84(3):233–238. doi: 10.2471/blt.05.026310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornton RL, Hatt LE, Field EM, Islam M, Solis Diaz F, Gonzalez MA. Social security health insurance for the informal sector in nicaragua: a randomized evaluation. Health Economics. 2010;19(S1):181–206. doi: 10.1002/hec.1635. [DOI] [PubMed] [Google Scholar]
- Vapattanawong P, Hogan MC, Hanvoravongchai P, Gakidou E, Vos T, Lopez AD, Lim SS. Reductions in child mortality levels and inequalities in thailand: analysis of two censuses. The Lancet. 2007;369(9564):850–855. doi: 10.1016/S0140-6736(07)60413-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.