Abstract
Chronic pain is a debilitating condition that can impact various facets of interpersonal functioning. Although some studies have examined the extent to which family members are affected by an individual’s chronic pain, none have examined patients’ perceptions of feeling that they have become a burden to others. Research on self-perceived burden in different medical populations, such as cancer, amyotrophic lateral sclerosis, and stroke, has shown that it is associated with physical symptoms and, more robustly, with psychological difficulties and concerns. The present study examined the prevalence and predictors of self-perceived burden in a tertiary chronic pain sample. Participants were consecutive patients (N=238) admitted to an outpatient, interdisciplinary, chronic pain management program at a rehabilitation hospital. At admission, participants completed a battery of psychometric questionnaires assessing self-perceived burden, as well as a number of clinically-relevant constructs. Their significant others (n=80) also completed a measure of caregiver burden. Self-perceived burden was a commonly reported experience among chronic pain patients, with over 70% of participants endorsing clinically-elevated levels. It was significantly correlated with pain intensity ratings, functional limitations, depressive symptoms, attachment anxiety, pain self-efficacy, and caregiver burden. Self-perceived burden was also correlated with an item assessing suicidal ideation. In a hierarchical regression model, depressive symptoms, pain self-efficacy, and adult attachment significantly predicted self-perceived burden after controlling for demographic and pain-related variables. In conclusion, self-perceived burden is a clinically-relevant and commonly reported interpersonal experience in patients with longstanding pain.
1. Introduction
Chronic pain can impact various facets of interpersonal and family functioning [15,48]. Although some studies have examined the extent to which caregivers feel burdened by the provision of emotional and instrumental support to a family member with chronic pain [19,23], none have focused on self-perceived burden (SPB) among patients themselves.
SPB is defined as “empathic concern engendered from the impact on others of one’s illness and care needs, resulting in guilt, distress, feelings of responsibility and diminished sense of self” [32]. It encompasses aspects of self-identity, as well as cognitive, emotional, and interpersonal dimensions. SPB is comparable to the construct of perceived burdensomeness, that is, the perception that one is a burden to loved ones [50]. Both SPB [51] and perceived burdensomeness [21,49] have been identified as putative causes of the desire for suicide. Given the high rates of depression in chronic pain, including suicidality [17,41,54,55], SPB may be relevant to this association.
To date, research on SPB has focused largely on terminally ill patients [33], with 19%–38% of participants reporting significant concern about having become a burden to others [2,12,31,51,53]. SPB may be higher among those with other disabling, but non-fatal conditions, such as stroke [30]. SPB is associated with physical symptoms (e.g., pain and physical weakness) and, more robustly, with psychological difficulties (e.g., depression, anxiety, and decreased quality of life) [8,30,31,46,51], all of which are pertinent to the experience of chronic pain.
In this study, we evaluated the extent to which SPB is relevant to individuals with chronic pain. Because these patients often report being limited functionally in ways that place support requirements on others [45], we hypothesized that many patients would report a heightened level of SPB. Among stroke survivors, for example, SPB has been related to performing family and work roles [30].
A second objective was to identify predictors of SPB. Relationships with pain intensity and functional limitations were explored. Based on previous research [30,31,32,46,51], depressive symptoms were expected to be positively associated with SPB. We also examined, in a preliminary way, the association between SPB and suicidal ideation. Self-efficacy beliefs might influence the degree to which individuals rely on their significant others for support. As such, pain self-efficacy was hypothesized to be negatively associated with SPB. Adult romantic attachment characteristics were also considered because they have received increasing attention in relation to interpersonal aspects of chronic pain [34,37] and are associated with support seeking behaviors [35]. Attachment anxiety involves a fear of rejection and preoccupation with affection and esteem, and is positively associated with support received [11]. It was hypothesized to be positively related to SPB. Attachment avoidance involves discomfort with closeness [35]. Highly avoidant individuals would be expected to seek minimal support, although they may still experience a sense of burden.
A third objective was to evaluate the association between SPB and significant others’ perceptions of caregiver burden. Consistent with research on amyotrophic lateral sclerosis (ALS) and stroke [5,30], a positive, albeit modest, correlation was hypothesized.
2. Method
2.1. Participants and procedure
The data presented here are part of an ongoing program of research examining clinical and interpersonal aspects of chronic pain. Participants were consecutive patients admitted to an outpatient, group-based, interdisciplinary chronic pain self-management program at a rehabilitation hospital. They completed a battery of psychometric questionnaires at admission. The main inclusion criteria were the ability to speak and write in English or French and medical, psychological, and physical appropriateness (i.e., patients had medically stable musculoskeletal pain, were open to the self-management approach, did not have major psychological difficulties that would preclude participation, and were deemed to have the physical tolerance necessary to engage in the physiotherapy component of the program). Patients were excluded if they were medically unstable, they had a primary substance abuse problem, their pain symptoms were limited to headaches or gynecological/urinary, pelvic, or gastro-intestinal issues, and/or they were actively seeking a cure for their pain (i.e., seeking pain medications and/or interventions to eliminate their pain symptoms).
A total of 272 patients were recruited at study baseline. Seventeen participants were excluded because they indicated that they did not have a significant other and, as such, could not complete the primary measures. Additionally, 12 cases were excluded due to missing data, and 5 cases were excluded because participants indicated, in a feedback session, that their questionnaire results were inaccurate with respect to their current level of functioning. The final sample consisted of 238 individuals (141 women; 97 men), ranging in age from 21 to 73 years (M = 47.1 years, SD = 9.8). Based on Cohen’s [7] recommendations, this sample size provides adequate statistical power for detecting small-to-medium effects using correlational and multiple regression analyses.
Patients’ significant others were also recruited. As part of the consenting process, patients were asked if their significant others would be willing to complete a brief questionnaire. Willing patients were given a questionnaire package to distribute to their significant others. Those individuals identified as a significant other completed the package and returned it to the treatment centre in a sealed envelope. In total, 80 significant others were recruited. They ranged in age from 22 to 75 years (M=48.7; SD=10.9) and the majority were men (60%). Most were identified as spouses (85%). This sample provides adequate statistical power for detecting correlations of a medium-to-large effect size [7].
All study participants provided written informed consent. The study was approved by the institution’s research ethics board.
2.2. Socio-demographic characteristics and clinical information
Patients’ socio-demographic characteristics (e.g., age, sex, ethnic background, education level, and employment status) and clinical information (e.g., duration of pain and primary pain site) were collected using a patient history questionnaire administered as part of the initial screening process.
2.3. Self-report measures
At admission, all patients completed a battery of self-report measures. Their significant others, where applicable, completed a measure of caregiver burden at the same time point.
2.3.1. Self-perceived burden
SPB, the primary variable of interest, was evaluated using the 10-item Self-Perceived Burden Scale (SPBS) [8]. Respondents rated items on a 5-point Likert-type scale, ranging from 1 (none of the time) to 5 (all of the time). Scores range from 10 to 50, with higher scores indicating greater SPB. Example items were: “I feel guilty about the demands that I make on my caregiver” and “I feel I am a burden to my caregiver.” The SPBS was developed with patients undergoing hemodialysis [8] and further validation research has been conducted with cancer patients [43]. These studies demonstrate that the SPBS has high levels of convergent validity, discriminant validity, and internal consistency (i.e., coefficient alphas > .85). A clinically-relevant cut-off score of 20 has been established based on comparisons with semi-structured interviews conducted with palliative care patients [31].
2.3.2. Pain intensity ratings
Participants rated their current, average, least, and worst pain intensity over the past two weeks on a scale anchored by 0 (no pain) and 10 (as intense as you can imagine) [20]. These scores were summed to derive a total score, with higher totals denoting greater pain intensity.
2.3.3. Functional limitations
Functional limitations were assessed using a scale recommended by the Task Force on Records and Data Retrieval of the International Association for the Study of Pain [18]. The degree to which participants had difficulty performing 16 activities of daily living (e.g., making meals, getting in and out of bed, and participating in social activities) were evaluated on a 5-point scale anchored by 1 (no difficulty) and 5 (unable to do). Total scores range from 0 to 64, with higher scores indicating greater functional limitations. Previous research with chronic pain patients has indicated that this scale is internally consistent and sensitive to treatment effects [25].
2.3.4. Depressive symptoms
The Patient Health Questionnaire-9 (PHQ-9) [24,44] was used to evaluate depressive symptoms. This 9-item scale assesses the severity of depressive symptoms over the past two weeks and is based on DSM-IV diagnostic criteria for major depression. Responses are recorded on a scale ranging from 0 (not at all) to 3 (nearly every day). Total scores range from 0 to 27. The PHQ-9 has been widely used in medical and hospital-based populations [26,39,40].
2.3.5. Pain self-efficacy
Pain self-efficacy reflects an individual’s confidence in his/her ability to enjoy life and participate in various activities despite pain. It was measured using the Pain Self-Efficacy Questionnaire (PSEQ) [36]. Higher scores on this 10-item scale reflect greater confidence in participants’ ability to engage in these activities even though they have pain. Total scale scores range from 0 to 60. Research with chronic pain patients supports the high degree of internal consistency, test-retest reliability, and validity of this instrument [36].
2.3.6. Adult attachment dimensions
Adult attachment dimensions were evaluated using the Experiences in Close Relationships-Revised (ECR-R) questionnaire [14]. This 36-item measure assesses attachment anxiety (18 items) and attachment avoidance (18 items) on a 7-point scale anchored by 1 (strongly disagree) and 7 (strongly agree). Several studies support the excellent psychometric properties of the ECR-R (e.g., validity, factor structure, and reliability) [13,14,42]. In a recent investigation of pain appraisal and illness behavior, the two ECR-R scales demonstrated satisfactory levels of internal consistency [29].
2.3.7. Caregiver burden
Patients’ significant others completed the revised Bakas Caregiving Outcomes Scale (BCOS) [3], a 15-item questionnaire assessing caregiver burden. Items focus on changes in multiple domains (e.g., social and physical functioning) as a result of caregiving activities. Responses are recorded on a 7-point scale, ranging from −3 (changed for the worst) to +3 (changed for the best). Items are recoded such that higher scores reflect greater caregiver burden. This measure has excellent psychometric properties, including reliability and validity, in medical conditions, such as stroke [3].
2.4. Data analyses
Data were analyzed using SPSS, version 18. Data were initially screened using established procedures [47]. Gender differences on all study variables were evaluated using independent samples t-tests. Differences between patients whose significant others completed a questionnaire and all other patients were also compared. Internal consistency was evaluated using coefficient alpha. Descriptive statistics were used to summarize the SPBS. Associations among SPB and other study variables were examined using Pearson correlations. Predictors of SPBS scores were examined in a hierarchical multiple regression (HMR) analysis. In the first step, age and gender were entered. In the second step, the predictors were pain intensity ratings and functional limitations. In the third and final step, the predictors were depressive symptoms, pain self-efficacy, attachment anxiety, attachment avoidance, and the attachment anxiety by attachment avoidance interaction. The interaction term was created to examine different attachment categories (viz. secure, dismissing, preoccupied, and fearful) based on a theoretical model of adult attachment [4]. It was derived by multiplying attachment anxiety and attachment avoidance. The HMR analysis allowed for the relative contribution of variables entered in each step to be evaluated after controlling for all other variables already entered in the model. It specifically allowed for an examination of the relationships among the SPBS and other psychological variables after controlling for demographic and pain-related variables. The coefficient of determination was calculated for each step. To test the interaction effect and to reduce multicollinearity, all continuous variables were initially centered (i.e., re-scaled so the mean of each scale was zero) based on established procedures [1]. The criterion for statistical significance for all analyses was set at p<.05.
3. Results
3.1. Sample characteristics
Of the final sample (N = 238), the primary sites of pain were back, generalized, and neck. The majority of participants were Caucasian (86.5%), not working, and had attended at least some college or university. Additional patient characteristics are presented in Table 1.
Table 1.
Participant characteristics (N = 238)
| Variable | Descriptive Statistics |
|---|---|
| Mean age ± SD (yrs.) | 47.08 ± 9.81 |
| Range (yrs.) | 21–73 |
| Sex | |
| Female | 59.2% |
| Male | 40.8% |
| Mean duration of pain symptoms ± SD (yrs.) | 6.80 ± 7.63 |
| Range | 5 months–53 yrs |
| Primary pain location | |
| Head, face, mouth | 3.4% |
| Neck (cervical) | 8.8% |
| Shoulders, arms, hands | 6.7% |
| Back | 33.6% |
| Legs, feet | 6.7% |
| Pelvic region | 2.5% |
| Generalized | 29.0% |
| Other | 8.0% |
| Education level | |
| Primary or secondary | 23.5% |
| Some college or university | 21.0% |
| College or university graduate | 43.4% |
| Trade certificate | 12.2% |
| Employment status | |
| Full- or part- time | 17.6% |
| Unemployed | 18.5% |
| Student | 1.3% |
| Disability | 41.6% |
| Sick Leave | 7.1% |
| Retired | 5.5% |
| Other | 8.4% |
| Marital Status | |
| Single | 12.6% |
| Married/common-law | 69.7% |
| Divorced/separated | 15.9% |
| Widowed | 1.7% |
Note. Percentages may not sum to 100 due to rounding.
3.2. Preliminary analyses
All scales had good or excellent levels of internal consistency, with coefficient alphas ranging from .81 to .95 (Table 2). No differences between men and women were obtained on any study measure. Participants’ SPBS scores were unrelated to their employment status. Compared to all other patients, those whose significant others completed a questionnaire (n = 80) endorsed lower levels of both attachment anxiety [t(236) = 2.64, p < .01] and attachment avoidance [t(236) = 2.85, p < .01]. These two groups did not differ on any other variable.
Table 2.
Cronbach’s alphas, descriptive statistics, and inter-correlations for study self-report measures (N = 238)
| Measure | α | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) Self-perceived burden | .91 | 27.42 | 10.02 | -- | .21** | .32*** | .41*** | −.38*** | .23*** | .12 | .34** |
| (2) Pain intensity | .87 | 26.00 | 5.81 | -- | .46*** | .23*** | −.28*** | −.03 | .07 | .05 | |
| (3) Functional limitations | .92 | 42.26 | 10.45 | -- | .29*** | −.41*** | .01 | .05 | .12 | ||
| (4) Depressive symptoms | .81 | 14.03 | 5.65 | -- | −.43*** | .38*** | .26*** | .23* | |||
| (5) Pain self-efficacy | .90 | 24.17 | 12.02 | -- | −.14* | −.12 | −.14 | ||||
| (6) Attachment anxiety | .93 | 3.06 | 1.36 | -- | .64*** | .23* | |||||
| (7) Attachment avoidance | .91 | 3.10 | 1.17 | -- | .18 | ||||||
| (8) Caregiver burden | .95 | 66.69 | 14.64 | -- |
Note. Correlations among caregiver burden and all other variables are based on a sample of 80 significant others.
p< .05.
p< .01.
p< .001.
3.3. Prevalence of SPB
SPBS scores ranged from 10 to 50, with a median of 27.0. The item with the highest mean score was “I feel guilty about the demands that I make on my caregiver,” whereas the item with the lowest mean score was “I am concerned that my caregiver is helping me beyond their capacity” (Table 3). Seventy-three percent of the sample (n = 174) endorsed an elevated level of SPB based on a SPBS clinical cut-off of 20 [31].
Table 3.
Mean Self-Perceived Burden Scale item scores (N = 238)
| Self-Perceived Burden Scale Item | M | SD |
|---|---|---|
| 1. I worry that the health of my caregiver could suffer as a result of caring for me. | 2.87 | 1.33 |
| 2. I worry that my caregiver is overextending himself/herself in helping me. | 2.63 | 1.35 |
| 3. I am concerned that it costs my caregiver a lot of money to care for me. | 2.02 | 1.41 |
| 4. I feel guilty about the demands that I make on my caregiver. | 3.06 | 1.36 |
| 5. I am concerned that I am “too much trouble” to my caregiver. | 2.89 | 1.36 |
| 6. I am concerned that because of my illness, my caregiver is having to do too many things at once. | 2.83 | 1.36 |
| 7. I am confident that my caregiver can handle the demands of caring for me (reversed scored). | 2.94 | 1.27 |
| 8. I think that I make things hard on my caregiver. | 2.82 | 1.29 |
| 9. I feel I am a burden to my caregiver. | 3.01 | 1.39 |
| 10. I am concerned that my caregiver is helping me beyond their capacity. | 2.35 | 1.37 |
Note. Each item was rated on a 5-point scale, ranging from 1 (none of the time) to 5 (all of the time).
3.4. Correlates of SPB
SPBS scores were positively and significantly associated with pain intensity, functional limitations, depressive symptoms, attachment anxiety, and caregiver burden, whereas they were negatively and significantly correlated with pain self-efficacy (Table 2). They were also negatively associated with age (r = −.19, p < .01). Of note, caregiver burden was positively and significantly associated with both patients’ attachment anxiety and depressive symptoms. In the majority of cases, the above noted correlations were at least moderate in size (i.e., r ≥ .30) [7]. As is common in attachment research, the correlation between the attachment dimensions was positive and large (i.e., r > .50).
Given past research and theory linking perceived burdensomeness to both depression and suicidality [21,50,54], associations between individual items on the PHQ-9 and the SPBS were examined. All depression items correlated positively and significantly with SPB. In most cases, the magnitude of the correlations was small-to-moderate (i.e., rs between .10 and .30). The highest correlations were with the worthlessness (r = .44, p < .001) and suicidal ideation (r = .46 p < .001) items.
3.5. Hierarchical regression analysis predicting SPB
The HMR analysis predicting the SPBS total score is summarized in Table 4. On the first step, age and gender accounted for 5% (p < .01) of the variance in SPB. On the second step, pain intensity ratings and functional limitations uniquely explained an additional 10% (p < .001) of the variance in SPBS scores. In the third and final step, depressive symptoms, pain self-efficacy, and the attachment variables uniquely accounted for a further 14% (p < .001) of the variance in the criterion measure. In the final model (i.e., when all variables were entered together), functional limitations, depressive symptoms, pain self-efficacy, and the attachment anxiety by attachment avoidance interaction significantly predicted SPB. Together, all variables accounted for 29% of the variance in SPBS scores.
Table 4.
Final model for the hierarchical multiple regression predicting self-perceived burden (N = 238)
| Step | Independent variable | β | ΔF | ΔR2 | R2 |
|---|---|---|---|---|---|
| 1 | Age | −.11 | 5.83** | .05** | 05 |
| Gender (Male = 0, Female = 1) | −.10 | ||||
|
| |||||
| 2 | Pain intensity | .03 | 14.02*** | .10*** | .15 |
| Functional limitations | .17* | ||||
|
| |||||
| 3 | Depressive symptoms | .20** | 8.90*** | .14*** | .29 |
| Pain self-efficacy | −.20** | ||||
| Attachment anxiety | .15 | ||||
| Attachment avoidance | −.05 | ||||
| Attachment anxiety X avoidance | −.13* | ||||
p< .05.
p< .01.
p< .001.
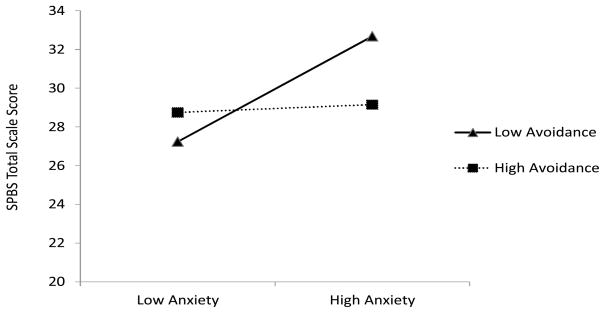
The regression equation from the final model was used to determine plot points for illustrating the interaction effect. Low and high levels of the attachment variables (i.e., 1 SD below and above the mean) were used for this purpose. Attachment avoidance was treated as the moderator and attachment anxiety was treated as the focal predictor. As is standard practice, zeros (i.e., the means of the centered continuous variables and the value for males based on the dichotomous gender variable) were entered for other variables in the regression. The obtained values are illustrated in Figure 1. Inferential statistical procedures were used to assess the statistical significance of the relationships illustrated in Figure 1 [38]. Among those high in attachment avoidance, there was a slight positive association between attachment anxiety and the total SPBS score; however, this relationship was not statistically significant (b = .14, p = .83). Amongst those low in attachment avoidance, there was a significant and positive association between attachment anxiety and the total SPBS score (b = 2.01, p = .009).
Fig. 1.
Graph depicting attachment avoidance moderating the relationship between attachment anxiety and self-perceived burden (N = 238). Regression analyses were used to plot predicted Self-Perceived Burden Scale (SPBS) scores based on high and low levels (i.e., 1 SD above and below the mean) of attachment anxiety and attachment avoidance. The points on the graph illustrate predicted SPBS values at specific values of the two attachment dimensions.
4. Discussion
This study examined SPB in a tertiary sample of chronic pain patients. Overall, results indicated that SPB is a common interpersonal experience reported by patients with longstanding pain, which is associated with several clinically-relevant variables. The majority of participants endorsed an elevated level of SPB, suggesting a high degree of concern about the impact of their condition on significant others. Hence, this investigation makes an important contribution to a growing body of literature examining interpersonal dimensions of chronic pain [15,27,34,37,48].
The 73% of chronic pain patients with elevated SPB is higher than the proportions reported in studies of patients with advanced cancer [31,43], although it is comparable to the 70% reported among stroke survivors [30]. Some of the enduring changes associated with chronic pain (e.g., changes in emotional, vocational, and interpersonal functioning) [15,48], as well as other chronic illnesses and disabilities, are likely different from end-of-life issues faced by the terminally ill, which could explain why chronic pain patients endorse higher levels of SPB than patients with advanced cancer. As well, there is some evidence to suggest that, compared to other chronic conditions, painful rheumatic diseases are associated with greater functional impairment and diminished health-related quality of life [28]. It may be that declines in both functional ability and health-related quality of life contribute to SPB among individuals with chronic pain.
Interpersonally, SPB may arise, at least in part, from a sense of perceived inequity. According to social exchange theory [16], individuals in social relationships weigh benefits (i.e., what they receive) and costs (i.e., what they provide). This analysis results in a series of “negotiated” exchanges between individuals. Successful relationships are based on give-and-take, with both parties contributing and receiving in approximately equal proportions. Dissatisfaction and distress are hypothesized to result when there is a perceived imbalance between benefits and costs. Indeed, research with stroke survivors indicated that those who perceived that they were over-benefiting from relationships experienced greater levels of SPB than those who perceived that they were under-benefiting or those who perceived that their relationships were equitable [30].
In chronic pain, SPB could result when patients perceive that what they receive from significant others is greater than what they provide. Many chronic pain patients depend on others, at least to some degree, for instrumental, emotional, and social support, which could result in a sense of inequity or imbalance. This disparity could result in feelings of dependence and loss, as well as a decreased sense of autonomy and/or self-confidence. Similarly, significant others could experience a sense of inequity when they perceive that what they provide outweighs what they receive. This discrepancy is especially salient when one considers changes in roles and responsibilities that can result from chronic pain [45]. From an applied perspective, restoring a sense of equity and, potentially reducing SPB, could be achieved by changing one’s contributions (e.g. by doing more or doing differently), reducing one’s benefits (e.g., by relying less on others and, perhaps, fostering a sense of independence), and/or by changing one’s perception of the situation (e.g., by redefining or renegotiating roles and/or expectations). Within the context of pain management, this could be accomplished through the use of cognitive, behavioral, and interpersonal techniques, as well as by involving patients’ significant others in treatment. Furthermore, as patients become more active functionally through the course of pain management, relationship equity could be restored by facilitating greater participation in social roles.
The significant, positive association between SPB and depressive symptoms is in line with hypotheses and replicates a basic finding obtained in other populations, including cancer [43], hemodialysis [46], and stroke [30] patients. Arguably, one of the more important aspects of SPB reported to date is its association with suicidal ideation and behavior. This is integral to the Interpersonal Theory of Suicide [21,50], which holds that two factors, namely, perceived burdensomeness and thwarted belongingness, are causally related to suicidal behavior. Several recent studies have linked perceived burdensomeness or SPB to suicide-related behaviors in the general population [10,22], as well as in medical [32,52] and psychiatric patients [9,22]. Interestingly, of the items comprising the PHQ-9 [24,44], the suicidal ideation item was correlated most strongly with SPB, which further supports this conceptualization. The link between suicidal ideation and SPB is particularly important because suicide attempts and completed suicides are known to be elevated among people with chronic pain [17,41,54,55]. Nevertheless, the role of SPB as a contributing factor to this elevation remains to be determined.
The results pertaining to romantic attachment suggest that attachment anxiety is associated with higher SPB. They also suggest that attachment avoidance is a moderator of this relationship. The four points illustrating the interaction effect in Figure 1 correspond to the four attachment categories in Batholomew and Horowitz’s model of attachment [4]. Relative to the other attachment groups (secure, dismissing, and fearful), individuals with a preoccupied attachment style (i.e., high anxiety and low avoidance) are especially likely to experience a sense of burden. Preoccupied individuals see themselves negatively and worry that their partners will reject and leave them [35]. As such, they may be highly sensitive to the impact of their pain-related disability on others, and worry that their functional limitations might cause them to be abandoned. Concomitantly, they may have doubts about being worthy of affection, esteem, and love, which could increase their feeling of SPB. Individuals with high attachment avoidance (i.e., those with dismissing and fearful attachment), on the other hand, rarely allow themselves to depend on others for help [11] and do not expect others to provide assistance and care. Accordingly, they may be less prone to experience SPB regardless of their level of anxiety.
Two recent reviews highlight that attachment-anxious pain patients tend to present more pain symptoms, perceive the pain as more severe, experience low pain self-efficacy, and report more symptoms of depression, stress, and anxiety [34,37]. Accordingly, they may be more demanding toward their caregivers, which may contribute to caregiver burden as well as to feelings of SPB. It could be that for some patients with chronic pain, addressing interpersonal issues, including attachment anxiety and SPB, might actually contribute to improvements in pain symptoms, as well as to better emotional and social functioning.
The significant association between SPB and caregiver reports of feeling burdened is consistent with past research on ALS and stroke [5,30]. It is also in line with end-stage renal disease patients’ perceptions of being a burden to unpaid caregivers [46]. This suggests that patients’ sense of burdening others is founded, at least in part, on an accurate perception of caregiver burden. Interestingly, caregiver burden was associated positively with patients’ attachment anxiety and self-reported depressive symptoms. It may be that patients’ problems in interpersonal and emotional domains contribute to significant others’ distress regarding the provision of support. In turn, significant others’ level of caregiver burden, coupled with patients’ recognition of the hardship that is being caused to caregivers, likely contributes to patients’ feelings of SPB. Although the direction of these relationships was not examined in the current study, future research could explore these possibilities. Moreover, interventions that help couples address issues regarding roles, expectations, preferences for support, and emotional reactions could reduce distress in both patients and significant others.
Several study limitations are acknowledged. Causality cannot be inferred due to the correlational nature of the design. Although SPB could stem from functional and emotional changes associated with chronic pain, reciprocal relationships among variables (e.g., SPB and depression) are possible and likely. In a related vein, the data collected were obtained at a single time point. It remains unclear how SPB and other variables are related to each other over time. As this research is part of a larger longitudinal investigation, prospective relationships are planned. The current sample comprised chronic pain patients recruited from an outpatient, interdisciplinary rehabilitation program, the majority of whom were Caucasian, well-educated, and not working. Data on co-morbid medical conditions, which could be associated with functioning in various domains, were not included. As such, the generalizability of findings may be limited. The focus on pain intensity also limits the extent to which results generalize to other pain dimensions. Future research on SPB could examine other aspects of the pain experience. Patients whose significant others completed a questionnaire endorsed lower levels of both attachment anxiety and avoidance. Accordingly, the degree to which these results apply to patients experiencing a greater degree of attachment insecurity remains unknown. In addition, because significant others were recruited by approaching patients (i.e., participants self-identified their significant others), the external validity of findings may be limited. This issue could be addressed in future research by using alternative recruitment strategies. Finally, most of the significant others in this study were spouses. Differences in SPB are possible, depending on the nature of the relationship (e.g., spouses compared to friends or children), and merit further investigation.
In conclusion, results indicate that SPB is a common and clinically relevant experience among patients with longstanding pain. This interpersonal construct is associated with a number of pain-related and psychological variables, including suicidality, and warrants additional study.
Summary.
Self-perceived burden, that is, patients’ perception of being a burden to others, is a clinically-relevant and commonly reported experience in patients with chronic pain.
Acknowledgments
This research was supported by the Canadian Institutes of Health Research (MOP: 93645) and the Institute for Rehabilitation Research and Development of The Ottawa Hospital Rehabilitation Centre.
Footnotes
The authors declare no conflicts of interest for this study.
References
- 1.Aiken LS, West SG. Multiple regression: testing and interpreting interactions. Thousand Oaks, California: Sage Publications; 1991. [Google Scholar]
- 2.Akazawa T, Akechi A, Morita T, Miyashita M, Sato K, Tsuneto S, Shima Y, Furukawa TA. Self-perceived burden in terminally ill cancer patients: a categorization of care strategies based on bereaved family members’ perspectives. J Pain Symptom Manage. 2010;40:224–34. doi: 10.1016/j.jpainsymman.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 3.Bakas T, Champion V, Perkins SM, Farran CJ, Williams LS. Psychometric testing of the revised 15-item Bakas Caregiving Outcomes Scale. Nurs Res. 2006;55:346–55. doi: 10.1097/00006199-200609000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Bartholomew K, Horowitz LM. Attachment styles among young adults: a test of a four-category model. J Pers Soc Psychol. 1991;61:226–44. doi: 10.1037//0022-3514.61.2.226. [DOI] [PubMed] [Google Scholar]
- 5.Chiò A, Gauthier A, Calvo A, Ghiglione P, Muntani R. Caregiver burden and patients’ perception of being a burden in ALS. Neurology. 2005;64:1780–2. doi: 10.1212/01.WNL.0000162034.06268.37. [DOI] [PubMed] [Google Scholar]
- 6.Chochinov HM, Kristjanson LJ, Hack TF, Hassard T, McClement S, Harlos M. Burden to others and the terminally ill. J Pain Symptom Manage. 2007;34:463–71. doi: 10.1016/j.jpainsymman.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 7.Cohen J. Statistical power analysis for the behavioural sciences. 2. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 8.Cousineau N, McDowell I, Hotz S, Hubert P. Measuring chronic patients’ feelings of being a burden to their caregivers: development and preliminary validation of a scale. Med Care. 2003;41:110–8. doi: 10.1097/00005650-200301000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Cox DW, Ghahramanlou-Holloway M, Greene FN, Bakalar JL, Schendel CL, Nademib ME, Jobes DA, Englent DR, Kindt M. Suicide in the United States Air Force: risk factors communicated before and at death. J Affect Disorders. 2011;133:398–405. doi: 10.1016/j.jad.2011.05.011. [DOI] [PubMed] [Google Scholar]
- 10.Cukrowicz KC, Cheavens JS, Van Orden KA, Ragain RM, Cook RL. Perceived burdensomeness and suicide ideation in older adults. Psychol Aging. 2011;26:331–8. doi: 10.1037/a0021836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davila J, Kashy DA. Secure base processes in couples: daily associations between support experiences and attachment security. J Fam Psychol. 2009;23:76–88. doi: 10.1037/a0014353. [DOI] [PubMed] [Google Scholar]
- 12.De Faye BJ, Wilson KG, Chater S, Viola RA, Hall P. Stress and coping with advanced cancer. Palliat Support Care. 2006;4:239–49. doi: 10.1017/s1478951506060317. [DOI] [PubMed] [Google Scholar]
- 13.Fairchild A, Finney SJ. Investigating validity evidence for the Experience in Close Relationships Revised Questionnaire. Educ Psychol Meas. 2006;66:116–35. [Google Scholar]
- 14.Fraley RC, Waller NG, Brennan KA. An item response theory analysis of self-report measures of adult attachment. J Pers Soc Psychol. 2000;78:350–65. doi: 10.1037//0022-3514.78.2.350. [DOI] [PubMed] [Google Scholar]
- 15.Gatchel RJ, Dersh J. Psychological disorders and chronic pain: are there cause-and-effect relationships? In: Turk DC, Gatchel RJ, editors. Psychological approaches to pain management: a practitioner’s handhood. 2. New York: Guilford Press; 2002. pp. 30–51. [Google Scholar]
- 16.Homans GC. Social behavior: its elementary forms. New York: Harcourt; 1961. [Google Scholar]
- 17.Ilgen MA, Zivin K, Austin KL, Bohnert AS, Czyz EK, Valenstein M, Kilbourne AM. Severe pain predicts greater likelihood of subsequent suicide. Suicide Life Threat Behav. 2010;40:597–608. doi: 10.1521/suli.2010.40.6.597. [DOI] [PubMed] [Google Scholar]
- 18.International Association for the Study of Pain. Pain database questionnaire. Seattle: 1995. [Google Scholar]
- 19.Jacobi CE, van den Berg B, Boshuizen HC, Rupp I, Dinant HJ, van den Bos GA. Dimension-specific burden of caregiving among partners of rheumatoid arthritis patients. Rheumatology. 2003;42:1226–33. doi: 10.1093/rheumatology/keg366. [DOI] [PubMed] [Google Scholar]
- 20.Jensen MP, Turner JA, Romano JM, Fisher LD. Comparative reliability and validity of chronic pain intensity measures. J Pain. 1999;83:157–62. doi: 10.1016/s0304-3959(99)00101-3. [DOI] [PubMed] [Google Scholar]
- 21.Joiner TE. Why people die by suicide. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- 22.Joiner TE, Jr, Van Orden KA, Witte TK, Selby EA, Ribeiro JD, Lewis R, Rudd MD. Main predictions of the interpersonal-psychological theory of suicidal behavior: empirical tests in two samples of young adults. J Abnorm Psychol. 2009;118:634–46. doi: 10.1037/a0016500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jones SL, Hadjistavropoulos HD, Janzen JA, Hadjistavropoulos T. The relation of pain and caregiver burden in informal older adult caregivers. Pain Med. 2011;12:51–8. doi: 10.1111/j.1526-4637.2010.01018.x. [DOI] [PubMed] [Google Scholar]
- 24.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kowal J, Wilson KG, Geck CM, Henderson PR, D’Eon JL. Changes in perceived pain severity Following interdisciplinary treatment for chronic pain. Pain Res Manag. 2011;16:451–6. doi: 10.1155/2011/817816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kroenke K, Spitzer RL, Williams JB, Löwe B. The Patient Health Questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. 2010;32:345–59. doi: 10.1016/j.genhosppsych.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 27.Leonard MT, Cano A, Johansen AB. Chronic pain in a couples context: a review and integration of theoretical models and empirical evidence. J Pain. 2006;7:377–90. doi: 10.1016/j.jpain.2006.01.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Loza E, Abásolo L, Angel J, Carmona L. Burden of disease across chronic diseases: a health survey that measured prevalence, function, and quality of life. J Rheumatol. 2008;35:159–65. [PubMed] [Google Scholar]
- 29.Martínez MP, Miró E, Sánchez AI, Mundo A, Martínez E. Understanding the relationship between attachment style, pain appraisal and illness behavior in women. Scand J Psychol. 2012;53:54–63. doi: 10.1111/j.1467-9450.2011.00925.x. [DOI] [PubMed] [Google Scholar]
- 30.McPherson CJ, Wilson KG, Chyurlia L, Leclerc C. The balance of give and take in caregiver-partner relationships: an examination of self-perceived burden, relationship equity, and quality of life from the perspective of care recipients following stroke. Rehabil Psychol. 2010;55:194–203. doi: 10.1037/a0019359. [DOI] [PubMed] [Google Scholar]
- 31.McPherson CJ, Wilson KG, Lobchuk MM, Brajtman S. Self-perceived burden to others: patient and family caregiver correlates. J Palliat Care. 2007;23:135–42. [PubMed] [Google Scholar]
- 32.McPherson CJ, Wilson KG, Murray M. Feeling like a burden: exploring the perspectives of patients at the end of life. Soc Sci Med. 2007;64:417–27. doi: 10.1016/j.socscimed.2006.09.013. [DOI] [PubMed] [Google Scholar]
- 33.McPherson CJ, Wilson KG, Murray M. Feeling like a burden to others: a systematic review focusing on the end of life. Palliat Med. 2007;21:115–28. doi: 10.1177/0269216307076345. [DOI] [PubMed] [Google Scholar]
- 34.Meredith P, Ownsworth T, Strong J. A review of the evidence linking adult attachment theory and chronic pain: presenting a conceptual model. Clin Psychol Rev. 2008;28:407–29. doi: 10.1016/j.cpr.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 35.Mikulincer M, Shaver PR. Attachment in adulthood: structure, dynamics, and change. New York: Guilford Press; 2007. [Google Scholar]
- 36.Nicholas MK. The Pain Self-Efficacy Questionnaire: taking pain into account. Eur J Pain. 2007;11:153–63. doi: 10.1016/j.ejpain.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 37.Porter LS, Davis D, Keefe FJ. Attachment and pain: recent findings and future directions. Pain. 2007;128:195–8. doi: 10.1016/j.pain.2007.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interaction effects in multiple linear regression, multilevel modeling, and latent curve analysis. J Educ Behav Stat. 2006;31:437–48. [Google Scholar]
- 39.Rentsch D, Dumont P, Borgacci S, Carballeira Y, deTonnac N, Archinard M, Andreoli A. Prevalence and treatment of depression in a hospital department of internal medicine. Gen Hosp Psychiatry. 2007;29:25–31. doi: 10.1016/j.genhosppsych.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 40.Rosemann T, Backenstrass M, Joest K, Rosemann A, Szecsenyi J, Laux G. Predictors of depression in a sample of 1,021 primary care patients with osteoarthritis. Arthritis Rheum. 2007;57:415–22. doi: 10.1002/art.22624. [DOI] [PubMed] [Google Scholar]
- 41.Scott KM, Hwang I, Chin WT, Kessler RC, Angermeyer M, Beautrais A, Barges G, Bruffaerts R, de Graff R, Florescu S, Fukao A, Hero JM, Hu C, Kovess V, Levinson D, Posada-Villa J, Scocco P, Nock MK. Chronic physical conditions and their association with first onset of suicidal behavior in the World Mental Health Surveys. Psychosom Med. 2010;72:712–9. doi: 10.1097/PSY.0b013e3181e3333d. [DOI] [PubMed] [Google Scholar]
- 42.Sibley CG, Fischer R, Liu JH. Reliability and validity of the revised Experiences in Close Relationships (ECR-R) self-report measure of adult romantic attachment. Pers Soc Psychol Bull. 2005;31:1524–36. doi: 10.1177/0146167205276865. [DOI] [PubMed] [Google Scholar]
- 43.Simmons LA. Self-perceived burden in cancer patients. Cancer Nurs. 2007;30:405–11. doi: 10.1097/01.NCC.0000290816.37442.af. [DOI] [PubMed] [Google Scholar]
- 44.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. J Am Med Assoc. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 45.Strunin L, Boden LI. Family consequences of chronic back pain. Soc Sci Med. 2004;58:1385–93. doi: 10.1016/S0277-9536(03)00333-2. [DOI] [PubMed] [Google Scholar]
- 46.Suri RS, Larive B, Garg AX, Hall YN, Pierratos A, Chertow GM, Gorodetskeya I, Kliger AS FHN Study Group. Burden on caregivers as perceived by hemodialysis patients in Frequent Hemodialysis Network (FHN) trials. Nephrol Dial Transplant. 2011;26:2316–22. doi: 10.1093/ndt/gfr007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tabachnick BG, Fidell LS. Using multivariate statistics. 5. Boston: Allyn & Bacon/Pearson Education; 2007. [Google Scholar]
- 48.Tunks ER, Crook J, Weir R. Epidemiology of chronic pain with psychological comorbidity: prevalence, risk, course, and prognosis. Can J Psychiatry. 2008;53:224–34. doi: 10.1177/070674370805300403. [DOI] [PubMed] [Google Scholar]
- 49.Van Orden KA, Lynam ME, Hollar D, Joiner TE., Jr Perceived burdensomeness as an indicator of suicidal symptoms. Cog Ther Res. 2006;30:457–67. [Google Scholar]
- 50.Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr The interpersonal theory of suicide. Psychol Rev. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wilson KG, Chochinov HM, McPherson CJ, Skirko MG, Allard P, Chary S, Gagnon PR, Macmillan K, De Luca M, O’Shea F, Kuhl D, Fainsinger RL, Karam AM, Clinch JJ. Desire for euthanasia or physician-assisted suicide in palliative cancer care. Health Psychol. 2007;26:314–23. doi: 10.1037/0278-6133.26.3.314. [DOI] [PubMed] [Google Scholar]
- 52.Wilson KG, Chochinov HM, Skirko MG, Allard P, Chary S, Gagnon PR, Macmillan K, De Luca M, O’Shea F, Kuhl D, Fainsinger RL. Depression and anxiety disorders in palliative cancer care. J Pain Symptom Manage. 2007;33:118–29. doi: 10.1016/j.jpainsymman.2006.07.016. [DOI] [PubMed] [Google Scholar]
- 53.Wilson KG, Curran D, McPherson CJ. A burden to others: a common source of distress for the terminally ill. Cogn Behav Ther. 2005;34:115–23. doi: 10.1080/16506070510008461. [DOI] [PubMed] [Google Scholar]
- 54.Wilson KG, Eriksson MY, D’Eon JL, Mikail SF, Emery PC. Major depression and insomnia in chronic pain. Clin J Pain. 2002;18:77–83. doi: 10.1097/00002508-200203000-00002. [DOI] [PubMed] [Google Scholar]
- 55.Worz R. Pain in depression—depression in pain. Pain Clinical Updates (IASP) XI. 2003;1:1–4. [Google Scholar]