Abstract
This study examines the impact of fear of past abusive partner(s) on posttraumatic stress among 212 community-recruited women currently exposed to intimate partner violence (IPV). The path analysis model tested explained 60% of the variation in IPV-related posttraumatic stress. Findings revealed that fear of past abusive partner(s) was uniquely associated with the severity of current posttraumatic stress symptoms over and above the impact of current IPV or childhood abuse and neglect. Future research should continue examining women's subjective emotional experience of past and current victimization so as to further inform both clinical practice and intervention planning.
Keywords: intimate partner violence, posttraumatic stress, fear, cumulative abuse
The relationship between intimate partner violence (IPV) and posttraumatic stress is firmly established in the literature. Psychological, physical, and sexual IPV have demonstrated significant relationships to posttraumatic stress symptom severity and posttraumatic stress disorder among a range of populations including community women (Sullivan & Holt, 2008), immigrant women (Yoshihama & Horrocks, 2003), treatment-seeking women (Krause, Kaltman, Goodman, & Dutton, 2006; Krause, Kaltman, Goodman, & Dutton, 2007; Pico-Alfonso, 2005), and sheltered women (Kemp, Green, Hovanitz, & Rawlings, 1995). Further, research on cumulative trauma has evidenced that mental health problems increase through exposure to multiple victimization experiences (Follette, Polusny, Bechtle, & Naugle, 1996; Schumm, Briggs-Phillips, & Hobfoll, 2006; and, for a review, see Scott-Storey, 2011). In particular, women currently exposed to IPV who report past victimization in childhood or adulthood display higher levels of posttraumatic stress than women who did not report past victimization (Banyard, Williams, Saunders, & Fitzgerald, 2008; Becker, Stuewig, & McCloskey, 2010; Follette et al., 1996; Nishith, Mechanic, & Resick, 2000; Sullivan, Cavanaugh, Buckner, & Edmondson, 2009). Though very few studies have examined patterns of past victimization in adulthood, namely past abusive relationships, existing data show that a fairly large proportion of women who experience IPV report more than one abusive relationship – for example an average of two to eight (Golder & Logan, 2011; Levendosky & Graham-Bermann, 2001). Past victimization is an important risk factor for posttraumatic stress; however, it is not sufficient in itself to explain variations in current symptom severity. Despite the salience of past victimization in relation to current functioning in general, mechanisms underlying the association between past victimization and current posttraumatic stress in the context of current IPV remain understudied.
Previous research suggests that the subjective emotional experience of victimization may be an additional risk factor for posttraumatic stress, with one study showing that subjective stress-related factors contributed twice as much as objective factors to the magnitude of psychological distress (Weaver & Clum, 1995). Although few studies have critically examined women's subjective emotional experience of victimization, some researchers have identified that negative emotions associated with IPV and posttraumatic stress, such as shame (Sippel & Marshall, 2011), guilt (Beck et al., 2011), or fear (Scheffer Lindgren & Renck, 2008) impact women's wellbeing. In particular, several studies have demonstrated that women who are fearful of their current abusive partner experience more severe mental health problems, including posttraumatic stress and depression (Brown, McDonald, & Krastev, 2008; Hamberger & Guse, 2002; Hathaway et al., 2000; Lowe, Humphreys, & Williams, 2007). However, to our knowledge, no studies have examined how fear of past abusive partner(s) might affect the association between current IPV and posttraumatic stress.
A better understanding of the underlying mechanisms through which past victimization affects women's current functioning has direct implications for clinical practice and intervention planning. Building upon previous studies that demonstrated that past victimization is associated with an increase of mental health problems subsequent to current victimization (Follette et al., 1996; Schumm et al., 2006; and, for a review, see Scott-Storey, 2011), this retrospective cross-sectional study examines how past and current victimization experiences interplay to impact current posttraumatic stress. Particularly, this study investigates the impact of fear of past abusive partner(s) and childhood abuse and neglect on the association between current IPV and IPV-related posttraumatic stress.
Past Victimization and Posttraumatic Stress
Over past decades, research has demonstrated that IPV has a pervasive impact on women's health in general (Bonomi, Anderson, Rivara, & Thompson, 2007; Campbell, 2002; Ellsberg, Jansen, Heise, Watts, & Garcia-Moreno, 2008; Logan, Walker, Jordan, & Leukefeld, 2006; Pico-Alfonso et al., 2006) and mental health in particular (Bell & Orcutt, 2009; Coker et al., 2002; Ellsberg et al., 2008; Golding, 1999; Mechanic, Weaver, & Resick, 2008; Sullivan et al., 2009). Women's IPV victimization experiences vary in both severity and complexity yet are known to consistently be associated with various short and long-term mental health problems, including posttraumatic stress, depression, dissociation, and suicidal behavior. Particularly, posttraumatic stress affects 31 to 84% of women exposed to IPV depending on the methods and timing of assessment (i.e. lifetime versus current symptoms; Golding, 1999).
Further, extant research suggests that the effect of childhood abuse and neglect combined with subsequent adult victimization increases posttraumatic stress symptomatology (Becker et al., 2010; Nishith et al., 2000; Sullivan et al., 2009), which suggests, in some way, that women do not habituate to victimization (Follette et al., 1996). The fact that past victimization experiences further negatively impact women's mental health is worrisome given that repeat victimization over the lifespan appears to be the norm rather than the exception for women victims of IPV (Scott-Storey, 2011). Women who experienced childhood abuse and neglect are two to ten times more likely to experience adult IPV than women who did not experience childhood abuse and neglect (Becker et al., 2010; Coid et al., 2001; Messman-Moore & Long, 2000). And, although fewer studies have examined the patterns of multiple abusive relationships in adulthood, there is evidence that not only IPV-exposed women are vulnerable to reabuse (e.g., Cattaneo Bennett & Goodman, 2005) but additionally often experience more than one abusive intimate relationship (Bybee & Sullivan, 2005; Cole, Logan, & Shannon, 2008; Golder & Logan, 2011; Krishnan, Hilbert, & Pase, 2001; Levendosky & Graham-Bermann, 2001; Smith, White, & Holland, 2003).
Research on past adult victimization associated to current posttraumatic stress, even though limited, suggests that mental health outcomes related to current victimization are further negatively impacted by past adult victimization (Golding, 1999; Noll, Horowitz, Bonanno, Trickett, & Putnam, 2003; Thompson, Arias, Basile, & Desai, 2002). Most important, adult victimization subsequent to childhood abuse and neglect has been found most significant in predicting lasting symptomatology (Nishith et al., 2000). Surveying a group of community and shelter women, Becker and colleagues (2010) measured the impact of prior childhood and adult victimization on traumatic stress related to current IPV. Physical and sexual childhood victimization showed an independent association with posttraumatic stress symptoms, as did adult psychological, physical, and sexual IPV. Adult IPV mediated the association between childhood physical abuse and the symptom severity of current posttraumatic stress. Further, knowledge about the nature of past abuse remains limited with regard to the underlying mechanisms by which it impacts women's current mental health. Although information regarding the extent and type of violence experienced in abusive relationships is valuable, it tells little about IPV-exposed women's subjective emotional experience of past psychological, physical, and sexual IPV victimization.
Fear of Past Abusive Partner(s)
Fear of abusive partner(s) has been examined in recent research on IPV, yet it has had various conceptualizations and operationalizations. In the IPV literature, fear has been examined as one means an abusive partner uses to establish control over the victim (Babcock, Miller, & Siard, 2003; Clements & Holtzworth-Munroe, 2009; Miller, 2006; Phelan et al., 2005; Thompson et al., 2006), a victim's emotional response to her partner's victimization (Barnett, Miller-Perrin, & Perrin, 2005; Hathaway et al., 2000; Scheffer Lindgren & Renck, 2008; Vogel & Marshall, 2001), a factor influencing women victims’ decision-making and help-seeking behavior in abusive relationships (Barrett & Pierre, 2011; Dearwater et al., 1998; Fanslow & Robinson, 2010; Watt, Bobrow, & Moracco, 2008), and a criterion to identify the primary aggressor in differentiating male- and female-perpetrated IPV (Cercone, Beach, & Arias, 2005; Houry et al., 2008; Jacobson et al., 1994; Johnson, 2008; Langhinrichsen-Rohling, Neidig, & Thorn, 1995; Morse, 1995). Additionally, several studies have conceptualized and studied fear as perceived life threat in relation to IPV experiences (Kilpatrick et al., 1989; Riggs, Kilpatrick, & Resnick, 1992; Weaver & Clum, 1995). Defined as “women's emotional and cognitive reactions to the environment created by their partner's use of violence” (Smith, Tessaro, & Earp, 1995, p. 175), fear in IPV experience is seen as resulting from both the perceived risk of violence and the uncontrollability of this risk.
Abusive partners’ induction of fear has been investigated as one of the primary mechanisms through which they achieve control over their victims. Women may be fearful of injury, death, or other consequences depending on the nature and targets of their partner's threats and behaviors. Very few studies have specifically examined women's levels of fear in abusive relationships regardless of how fear was operationalized, and most of these studies focused on comparing men's and women's levels of fear in line with Johnson's work on different types of relationships in which IPV occurs (Johnson, 2006, 2008) . Compared to IPV-exposed women, IPV-exposed men have been shown to be less fearful of the violence of their female partner (Cercone et al., 2005; Houry et al., 2008; Jacobson et al., 1994; Langhinrichsen-Rohling et al., 1995; Morse, 1995). For example, using a 5-point Likert scale, Hamberger and Guse (2002) showed that both court-ordered women and women in shelters exposed to IPV exhibited an average of 4.2 fear-related responses to their partners' behaviors as compared to the average of 1.7 fear-related responses exhibited by men and further, women were more likely than men to report intense fear when their partners initiated violence. The question of who is the primary aggressor has been raised consecutive to studies showing that both partners might use violent acts that seem similar (Straus, 1999), which then lead to the use of control, domination and fear induction being utilized to identify a power differential in relationships (Jacobson et al., 1994).
Several studies have underscored that a proportion of women do not report being fearful of their partner's violence (e.g., Bonomi et al., 2006; Brown et al., 2008; Olson et al., 2008). Additionally, fear of current partner has demonstrated a relation to increased mental health problems, including depression and posttraumatic stress (Brown et al., 2008; Hamberger & Guse, 2002; Hathaway et al., 2000; Lowe et al., 2007). No study that we know of however has examined how fear in past abusive relationships impacts current posttraumatic stress symptoms, or how childhood abuse and neglect might impact how fearful women are when they experience adult IPV. Given that fear is a central tenet of the development and diagnosis of posttraumatic stress – and because subjective factors such as fear associated with IPV strongly contribute to mental health outcomes – it appears particularly important to better understand how past and current victimization experiences interplay to affect current posttraumatic stress symptom severity. A better understanding of the underlying mechanisms that link IPV experiences and women's functioning over time has implications for clinical practice and intervention planning.
METHOD
Participants
Two hundred and twelve women were recruited from an urban community in New England. Recruitment flyers were posted in various locations throughout the community, including health clinics, churches, salons, grocery stores, and community agencies. The recruitment material read “Women's Relationship Study” so as not to disclose IPV as the primary focus of the study. Participation in the study was confidential. Women interested to take part in a 2-hour interview about the relationship with their boyfriend or husband were asked to call a local number. To determine if a woman was eligible to participate, she answered questions during a telephone screen. The primary inclusion criterion was that the woman experienced at least one act of physical violence during the prior 6 months perpetrated by her current male partner as measured by selected screening questions from the Conflict Tactics Scale-2 (CTS-2; Straus, Hamby, & Warren, 2003). Eligibility was further determined by the following inclusion criteria: (a) a relationship of at least 6 months duration, (b) contact with current partner at least twice a week; (c) continuous partner contact (i.e., no more than 2 weeks apart); and (d) monthly household income no greater than $4,200 which was determined a priori to methodologically control for differential resources associated with income. Of the 240 women who were found eligible to participate via the phone screen, 28 failed to meet inclusion criteria at the time of the study interview; 212 women composed the final sample.
A 2-hour, semistructured, computer-assisted interview was administered by a trained master or doctoral-level research associate. To protect participants’ safety, all interviews were conducted in private offices. During the process of informed consent, all women were asked if their participation would put them at risk. Interviewers were trained how to respond if the participant answered affirmatively. No participant reported safety concerns. After completion of the interview, all participants were debriefed, remunerated $50, and provided with a list of community resources regarding, for example, domestic violence, counseling, substance abuse treatment, housing, and food. Participants were asked if they wanted assistance accessing resources and assistance was provided when requested.
Among the 212 women participants, 184 reported having been in past abusive relationships as adults. Given that this study is focused on the impact that fear in past abusive relationships has on women's current posttraumatic stress, only the experiences of 183 women were considered for the present analyses (1 of the 184 women did not provide details about her past abuse). Subsequent analyses are presented on these 183 women. Women's average age was 36.7 years (SD = 10.5). Most women were either unemployed (34.4%) or unable to work (32.2%) at the time of the study, with a mean level of education of 12 years (SD = 1.5) and a mean annual household income of $13,121 (SD = $10,273). One hundred and twenty-three women were African American, forty were White, nine were Latina, three were American Indian or Alaska Native, and eight were identified as multiracial or didn't specify their race. Thirteen percent of couples were married, 45% were living together, 33% were dating and 6% said they had “broken up” but were still seeing each other. On average, couples saw each other 6 days a week (M = 6.3, SD = 1.4). Mean years in the current relationship was 5.9 (ranging from six months to 33 years; SD = 68.9 months) and 63.9% of women had children under 18 years old. As stated, all of the 183 women reported at least one past abusive relationship; on average, women reported 2.4 past abusive relationships (actual range 1-15; SD = 1.8).
Measures
Fear
Fear was measured with a scale developed for this study as no measure existed. The Past Abusive Behavior Inventory (Swan & Sullivan, 2004) assesses the total number of past adult relationships in which women experienced psychological, physical or sexual IPV. Various acts of IPV were measured. Physical IPV encompassed hitting, slapping, or punching; sexual IPV encompassed sexual touching or forced sex; and psychological IPV encompassed controlling behaviors, swearing, putting down, or calling names. Women who indicated abuse in one or more past intimate relationships were asked additional questions for each of their three most recent abusive relationships. In particular, women were asked to what extent they feared each of their three last abusive partners on a 4-point scale (i.e., “How afraid of him were you?”; 0 = not frightened, 1 = just a little frightened, 2 = somewhat frightened, and 3 = very frightened). Women's current level of fear of past abusive partners was not assessed. To measure fear of past abusive partner(s), a composite variable was computed according to women's highest level of fear experienced across her three most recent past abusive relationships; this resulted in a 3-level ordinal variable (0 = never frightened, 1= a little or somewhat frightened, and 2 = very frightened).
Posttraumatic stress
Intimate partner violence-related posttraumatic stress was measured using the 49-item Posttraumatic Stress Diagnostic Scale (PDS; Foa, 1995). To the extent possible, posttraumatic stress was assessed in relation to current IPV exposure; specifically, women were asked to report on posttraumatic stress symptoms occurring consequent to abuse by their current partner. Five of the six posttraumatic stress diagnostic criteria (American Psychiatric Association, 1994) were considered in these analyses. Specifically, diagnostic criterion A (i.e., exposure to a traumatic stressor) was assessed in relation to IPV by current partner for the duration of the relationship. Diagnostic criteria (B) re-experiencing, (C) avoidance and numbing, (D) arousal symptoms, and (F) the symptoms' impact on daily functioning were assessed over the previous 6 months. Modeled after Sullivan and colleagues (2009), IPV-related posttraumatic stress was included in the analytical model as a latent variable comprised of three indicators: (a) whether the event was considered traumatic according to criterion A (0 = no, 1 = yes), (2) the severity of re-experiencing, avoidance and numbing, and arousal symptoms (i.e., sum score of severity of 17 symptoms), and (3) impairment in functioning (i.e., count of life domains impacted by symptoms, namely household chores and duties, relationships with friends, fun and leisure activities, relationship with family, sex life, and general life satisfaction).
Intimate partner violence
. Psychological, physical, and sexual IPV were measured with the 78-item Conflict Tactics Scale-2 (CTS-2; Straus et al., 2003). To complement the CTS-2, the Sexual Experiences Survey (SES; Koss & Gidycz, 1985) and the Psychological Maltreatment of Women Inventory (PMWI; Tolman, 1989, 1999) were used to measure sexual and psychological IPV, respectively. For the present analyses, a reference period of 6 months was chosen to assess violence perpetrated by the woman's current partner. Physical IPV response categories that comprised a range of values were recoded according to Straus and colleagues (2003) [i.e., never, once, twice, 3-5 times (recoded to 4), 6-10 times (recoded to 8), 11-20 times (recoded to 15), and more than 20 times (recoded to 25)]. The physical IPV score was the sum of the 12 CTS-2 items of the assault subscale, α = .89. The coding scheme for the frequency of the 10 sexual IPV items was identical to the coding scheme of physical IPV; the sexual IPV score was then calculated as the sum of the 10 SES items, α = .89. The psychological IPV score was the sum of the 58 PMWI items with response options from 1 = never to 5 = very often, α = .96.
Childhood abuse and neglect
Childhood physical, sexual, and emotional abuse and physical and emotional neglect were assessed using the 28-item Childhood Trauma Questionnaire (CTQ; Bernstein & Fink, 1998). Items are rated on a 5-point scale from 1 = never true to 5 = very often true, with subscales scores ranging from 5 to 25. Reliability for the five subscales ranged from α = .76 to α = .97. To reduce the number of parameters to be modeled, these five subscales were collapsed into two indicator variables (Kline, 2011). Childhood abuse was computed as the sum score of the CTQ 15 items of the three abuse subscales measuring emotional, physical, and sexual abuse, α = .92. Childhood neglect was computed as the sum score of the 10 CTQ items of the two neglect subscales, emotional and physical neglect1, α = .88.
Data Analysis
Study variables were assessed for assumptions of normality. To produce normal distributions as recommended by Tabachnick and Fidell (2012), variables were transformed using the most conservative transformation. Physical IPV and childhood abuse and neglect subscales were log10 transformed, childhood abuse and childhood neglect indicator variables were square root transformed, and sexual IPV was dichotomized (0 = never; 1 = one experience or more). Transformed scores were analyzed in the structural equation model (raw scores are noted in Table 1). Bivariate methods determined the inclusion of demographic variables in the analytic model (i.e., age, race, education, and household income); only variables correlated at p < .10 with any of the three posttraumatic stress variables were included.
Table 1.
Means, standard deviations and percentages
| Variable | M | SD | Actual range |
|---|---|---|---|
| Fear of past abusive partner(s) | |||
| Never fearful (%) | 23.50 | ||
| A little or somewhat fearful (%) | 39.89 | ||
| Very fearful (%) | 36.61 | ||
| Posttraumatic stress – Traumatic event (% yes) | 44.26 | ||
| Posttraumatic stress – Symptom severity | 19.62 | 11.54 | 0-48 |
| Posttraumatic stress – Domains impacted | 2.91 | 1.98 | 0-6 |
| Childhood emotional abuse | 11.31 | 5.50 | 5-25 |
| Childhood physical abuse | 9.38 | 4.80 | 5-25 |
| Childhood sexual abuse | 10.01 | 7.05 | 5-25 |
| Childhood emotional neglect | 11.53 | 5.33 | 5-24 |
| Childhood physical neglect | 7.30 | 3.27 | 5-20 |
| Psychological intimate partner violence | 128.31 | 34.35 | 53-223 |
| Physical intimate partner violence | 34.92 | 46.82 | 1-209 |
| Sexual intimate partner violence (% yes) | 57.92 | ||
| Age | 36.72 | 10.46 | 18-58 |
| Education | 12.08 | 1.54 | 7-18 |
| Race (%) | |||
| White | 21.86 | ||
| African American | 67.21 | ||
| Hispanic or Latina | 4.92 | ||
| American Indian/Alaska Native | 1.64 | ||
| More than one race | 1.64 | ||
| Unknown/Other | 2.73 | ||
| Income | 13,121.18 | 10,273.91 | 0-48,000 |
Note. Means, standard deviations and percents are untransformed scores.
The hypothesized model was analyzed using structural equation modeling (SEM) techniques (Kline, 2011) in AMOS® 19.0 (Arbuckle, 2010). SEM simultaneously estimates the relationship between observed and latent variables (the measurement model) and among latent variables themselves (the structural model), providing estimates for both direct and indirect, or mediating effects. Confirmatory factor analyses were conducted to confirm relationships between item indicators and latent variables. Scores for all latent variables were calculated using factor score weights provided by AMOS®. These allow for factor scores to be created that reflect the extent to which different indicators load on each of the latent variables. The structural model was then tested using SEM using Kenny's (1999) three-step approach to testing model fit. First, the fit of the theoretical model was tested. Second, “deleted” paths (i.e., paths that were not hypothesized in the theoretical model and thus implicitly set to 0 were tested to guard against specification error). Third, structural paths specified in this revised model were tested, and nonsignificant (p > .05) paths were trimmed to produce a more parsimonious model. Standard measures of model fit [i.e., chi-square, Normed fit index (NFI), Tucker-Lewis index (TLI), comparative fit index (CFI), root mean square error of approximation (RMSEA)] were used to assess model fit. Alternative models were compared based on the Akaike information criterion (AIC); the model with the lower AIC value was chosen as presenting better balance of model fit and parsimony (Akaike, 1974).
Bootstrapping procedures in AMOS were used to estimate the significance of indirect effects. Bootstrapping is a preferred method for estimating and testing hypotheses related to mediation compared to other methods (e.g., the Sobel test) as it does not rely on the assumption that the indirect effect is normally distributed (Kline, 2011; Preacher & Hayes, 2008). Bootstrapping was done with 2,000 random samples generated from the observed covariance matrix to estimate bias-corrected 95% confidence intervals and significance values for the standardized direct, indirect, and total effects in the final model as suggested by Cheung and Lau (2008).
RESULTS
Sample Description
One-hundred and eighty-three women reported they had been in an abusive relationship prior to their current intimate relationship. When asked about their level of fear of their partner(s) while in these past relationships, 23.50% of women said they had never felt fearful, 39.89% said they had been somewhat or a little fearful, and 36.61% said they had been very fearful. As indicated in Table 1, 44.26% of women met criterion A for posttraumatic stress related to current IPV meaning that their IPV met DSM-IV criteria as a traumatic event (American Psychiatric Association, 1994). Mean score for posttraumatic stress symptom severity was 19.62 (SD = 11.54; actual range = 0 – 48). On average, the number of domains across which women's daily functioning was impacted by posttraumatic stress symptoms was 2.91 (SD = 1.98; actual range 0-6).
As physical IPV by current partner was an inclusion criterion of the study, all women experienced at least one act of physical violence by their current partner over the past 6 months. Among these women, 61.20% were injured consequent to IPV and of those, 40.18% sustained severe injuries. All women reported experiences of psychological abuse and controlling behaviors with an average psychological IPV score of 128.31 (SD = 34.35). The mean for the dominance and isolation subscale was 60.31 (SD = 18.74) and for the emotional and verbal abuse subscale was 68.01 (SD = 17.73). More than half of the women reported at least one experience of sexual coercion (e.g., forced rape using threat, force, or alcohol) by their current partner (57.92%). Prevalence of childhood abuse and neglect was high in this sample. According to the CTQ scoring categories, 61.2% of women experienced low to severe emotional abuse, 49.7% low to severe physical abuse, and 46.4% low to severe sexual abuse; 55.7% of women experienced low to severe emotional neglect and 35.5% low to severe physical neglect.
Correlations among study variables are reported in Table 2. Fear of past abusive partner(s) was significantly correlated with two of the posttraumatic stress outcome variables (r = .37 [p < .01] with symptom severity; and r =.16 [p < .05] with number of domains impacted). Fear of past abusive partner(s) was not significantly correlated with posttraumatic stress criterion A related to current IPV (r = .14, p > .10), suggesting an absence of overlap between the two constructs. Fear of past abusive partner(s) was significantly correlated with childhood abuse and neglect and current psychological IPV. Current psychological, physical and sexual IPV were significantly correlated with each of the posttraumatic stress outcome variables. With the exception of participants’ education, demographics were not correlated with the posttraumatic stress variables. Therefore, participants’ education was the only demographic included in the structural model.
Table 2.
Parametric and nonparametric correlations
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Fear of past abusive partner(s) | - | ||||||||||||||
| 2. Posttraumatic stress – Traumatic event | .14† | ||||||||||||||
| 3. Posttraumatic stress – Symptom severity | .37*** | .39*** | |||||||||||||
| 4. Posttraumatic stress – Domains impacted | .15* | .33*** | .60*** | ||||||||||||
| 5. Childhood emotional abuse | .23** | .25*** | .46*** | .39*** | |||||||||||
| 6. Childhood physical abuse | .13† | .23** | .42*** | .21** | .48*** | ||||||||||
| 7. Childhood sexual abuse | .10 | .14† | .24** | .27*** | .27*** | .20*** | |||||||||
| 8. Childhood emotional neglect | .18* | .18* | .42*** | .36*** | .22** | .17* | .06 | ||||||||
| 9. Childhood physical neglect | .18* | .25*** | .26*** | .23** | .13† | .20** | .06 | .62*** | |||||||
| 10. Psychological intimate partner violence | .15* | .16* | .21** | .14† | .16* | .11 | .16* | .43*** | .35*** | ||||||
| 11. Physical intimate partner violence | .16* | .10 | .28*** | .20** | .09 | .07 | .07 | .71*** | .42*** | .28*** | |||||
| 12. Sexual intimate partner violence | .15* | .15* | .25*** | .23** | .14† | .09 | .07 | .56*** | .40*** | .27*** | .67*** | ||||
| 13. Age | .17* | .10 | .09 | .08 | .18* | −.03 | .15* | −.05 | .05 | .12 | −.13† | −.08 | |||
| 14. Education | −.18* | .05 | .02 | .13† | −.07 | .03 | .12 | .06 | .00 | −.09 | .00 | −.14† | −.07 | ||
| 15. Race | −.12 | −.06 | −.05 | −.06 | −.11 | −.01 | .10 | −.16* | −.02 | .10 | −.14† | −.06 | −.02 | .04 | |
| 16. Household income | −.03 | −.01 | −.03 | .06 | .03 | −.17* | .05 | .04 | .00 | −.11 | .08 | .05 | −.05 | .30*** | −.14† |
Note. Correlations are based on transformed scores.
p <.10.
p < .05.
p < .01
Model Testing
The first step in model testing was to fit the measurement model that included the latent variables child abuse and neglect, current IPV and IPV-related posttraumatic stress. Factor loadings were statistically significant and of substantive magnitude (0.66-0.88), with the exception of the factor loadings of the two dichotomous indicators, namely sexual IPV and posttraumatic stress criterion A, whose loadings were statistically significant but of lower magnitude, 0.36 and 0.47 respectively. No unreasonable parameter estimates such as negative variances or correlation greater than one were observed, and all were in the expected range of values. An examination of parameter estimates provided support for the hypothesized structure of the measurement model. The measurement model was an excellent fit to the data, χ2 (17) = 15.90, p = .53, χ2 / df = 0.94, NFI=.96; TFI = 1.00, CFI = 1.00, and RMSEA = .00 (CI = .00-.06).
Next, the overall model was respecified following Kenny's (1999) three-step approach. The only “deleted” path (i.e., fear of past abusive partner(s) to current IPV) was tested, found significant, and therefore, added to the model. Second, all paths included in the respecified model were tested for significance. Participants’ education was no longer significantly related to posttraumatic stress and was considered for deletion. Given that participants’ education was still significantly related to fear of past abusive partner(s), two alternative models were tested, i.e., with and without participants’ education as a predictor. Education was eventually removed from the model given that the alternative model had a lower AIC value and therefore, possessed better balance of model fit and parsimony. All other paths were significant (p < .05 or p < .01) in the final model.
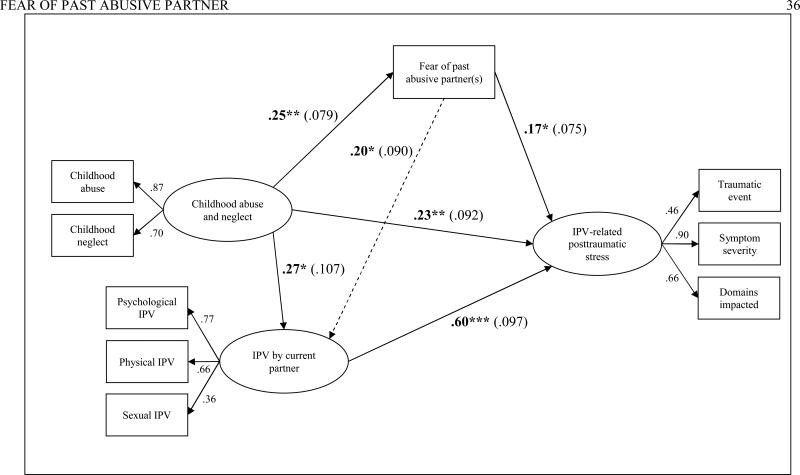
Final Model
The final model provided excellent fit to the data, χ2 (22) = 25.10, p = .29, χ2 / df = 1.14, NFI = .94, TFI = .99; CFI = .99, RMSEA = .03 (CI = .00-.07). Factor loadings are in line with those of the measurement model. The final model explains 60% of the variance in IPV-related posttraumatic stress (see Figure 1). Greater fear of past abusive partner(s) was significantly related to greater IPV-related posttraumatic stress (β = .17, p <.05). As expected, current IPV (β = .60, p <.01) and childhood abuse and neglect (β = .23, p <.01) were significantly and positively related to greater IPV-related posttraumatic stress. Unexpectedly, fear of past abusive partner(s) was also significantly and positively related to the severity of current IPV (β = .20, p <.05).
Figure 1. Final model for fear of past abusive partner(s), childhood abuse and neglect, IPV by current partner and IPV-related posttraumatic stress.
Note. Estimates are standardized and bootstrapped standard errors are presented in parenthesis. Dashed line indicates the significant path that was added through model testing. IPV = intimate partner violence. *p < .05 **p < .01 *** p ≤ .001.
To assess whether indirect pathways included in the final model were significant, AMOS® bootstrapping procedures were used. Results show that both fear of past abusive partner(s) and the severity of current IPV partially mediated the impact of childhood abuse and neglect on posttraumatic stress (Table 3). The impact of fear of past abusive partner(s) on posttraumatic stress was significantly and partially mediated by current IPV.
Table 3.
Direct, indirect, and total standardized effects
| Predictor | Criterion | Direct | Indirect | Total |
|---|---|---|---|---|
| Childhood trauma | Fear of past abusive partner(s) | .25** | – | .25** |
| IPV by current partner | .27* | .049* | .32** | |
| Posttraumatic stress | .23* | .24** | .47*** | |
| Fear of past abusive partner(s) | IPV by current partner | .20* | – | .20* |
| Posttraumatic stress | .17* | .12* | .28** | |
| IPV by current partner | Posttraumatic stress | .60*** | – | .60*** |
Note: Effects are standardized. Tests of effects are based on bootstrapped standard errors; 2,000 bootstrap samples. IPV = intimate partner violence.
p < .05.
p < .01
p ≤ .001
DISCUSSION
Findings of this study highlight the critical need to examine current and past victimization experiences to more comprehensively understand women's current posttraumatic stress severity. Consistent with results from other research (Bybee & Sullivan, 2005; Cole et al., 2008; Golder & Logan, 2011; Krishnan et al., 2001; Levendosky & Graham-Bermann, 2001; Smith et al., 2003), results of this study demonstrate that past abusive relationships among IPV-exposed women are common, with 86% of the 212 women in our study reporting at least one past abusive relationship and as many as fifteen. Past victimization in the form of past abusive relationships and childhood abuse and neglect, though important risk factors for posttraumatic stress, are not sufficient to explain variation in the severity of posttraumatic stress symptoms. This study is unique in that it fills a gap in the existing literature: Going beyond the assumption that ‘more is worse’ in regard to victimization (Scott-Storey, 2011, p. 135), this study illustrates that women's fear of past abusive partner(s) – a subjective emotional experience of victimization – plays a central role in explaining variation in the severity of current posttraumatic stress symptoms. The final model, which included fear of past abusive partner(s), current IPV, and childhood abuse and neglect, explained 60% of the variance in current IPV-related posttraumatic stress.
In the present study, fear of past abusive partner(s) influenced current posttraumatic stress over and above the impact of the severity of current IPV and childhood abuse and neglect. In other words, fear of past abusive partner(s) contributed uniquely to current posttraumatic stress symptoms, further negatively impacting posttraumatic stress symptoms related to IPV by a current partner. Women who had feared past abusive partner(s) display more severe posttraumatic stress symptoms than women who did not report fear as indicated by the direct positive relationship between fear of past abusive partner(s) and current posttraumatic stress symptoms. Childhood abuse and neglect significantly impacted fear of past abusive partner(s); women who experienced childhood abuse or neglected indicated greater fear compared to women who did not. Childhood abuse and neglect significantly impacted current posttraumatic stress directly, as well as indirectly through both fear of past abusive partner(s) and IPV by current partner. Of note, fear of past abusive partner(s) also was directly related to IPV by women's current partners. As evidenced in previous research, findings of this study suggest that women do not habituate to being victimized (Follette et al., 1996) meaning that mental health problems increase through exposure to multiple victimization experiences. These findings are of further interest as women who are not fearful are less likely to seek help or terminate an abusive relationship (Barrett & Pierre, 2011; Dearwater et al., 1998; Fanslow & Robinson, 2010; Watt et al., 2008), which puts them at greater risk for revictimization given the chronic nature of IPV.
A few study limitations are worthy of note. Given the cross-sectional study design and the self-report nature of these data, findings are subject to biases inherent in these methods. Further, it is likely that the most severely abused women were not able to participate in this study. Though the sample size is adequate to test the hypothesized model, a larger sample would have allowed the inclusion of a larger number of predictors. For example, future research should also examine how women's subjective emotional experience of victimization impacts mental health problems other than posttraumatic stress, such as depression or anxiety. Last, we did not assess women's subjective emotional experience of childhood abuse and neglect which might also contribute to further understanding variations in current posttraumatic stress.
Findings of the present study clearly suggest variations across women's subjective emotional experience of IPV, in particular with some women reporting being fearful and others not. To further advance knowledge on the interplay between past and current victimization, future studies should examine additional characteristics of women's subjective emotional experience of victimization – including fear of past abusive partner(s) – and how these experiences further impact women's psychological, physical, and reproductive health problems. Mixed-method study designs might be particularly relevant to better understand women's cognitive and emotional appraisals of their victimization (e.g., Testa, Livingston, & VanZile-Tamsen, 2011). Taking into account women's subjective experiences likely will contribute to a more realistic picture of IPV-exposed women and thus contribute to better tailoring interventions to women's specific needs.
The burden of victimization on women's psychological, physical, and reproductive health is evident today in both research findings and clinical practice. Progress has been made in developing our understanding of the cumulative impact of multiple victimization experiences, yet there is much still to learn. Like the complexity of human life, women's victimization experiences are multifaceted phenomenons that vary from one person to another and change over time. Research protocols need to explore how antecedents and correlates impact not only the risk of victimization but also its health consequences. In clinical practice, health screeners might include additional questions on fear and other dimensions of women's subjective emotional experience of IPV to better identify women's needs and thus inform intervention planning. While women who express being fearful of their partner(s) might be responsive to interventions discussing safety strategies, women who are not fearful are likely to find such interventions irrelevant. It is critical to examine the cumulative impact of multiple victimization experiences over time on current mental health symptomatology and take into account women's subjective emotional experiences to adequately identify targets for intervention.
Acknowledgments
Funding
The research described here was supported, in part, by grants from the National Institute on Drug Abuse (R03 DA17668) and the Swiss National Science Foundation (PBLAP1-131842 and PBLAP1-140055).
Biography
Véronique Jaquier, PhD, is a postdoctoral fellow in the Division of Prevention and Community Research, Department of Psychiatry, Yale School of Medicine, and a Part-Time Lecturer at the University of Lausanne. Trained in social psychology and criminology in Switzerland and the United States, she has taught classes in gender and crime, violence against women, victims’ rights and counseling. Dr Jaquier's program of research focuses on the interrelations of women's and girls' victimization and their use of aggression as it impacts mental health, substance use and risk behaviors, with emphasis on understanding how the criminal justice response impacts these different life trajectories.
Tami P. Sullivan, PhD, is an Assistant Professor and Director, Family Violence Research and Programs, Yale University School of Medicine. Her research centers on individual- and system-level factors that affect the wellbeing of women victims of IPV. At the individual level, she conducts risk and protective factor research and is particularly interested in applying micro-longitudinal designs and conducting research that informs the development of community-based interventions. Dr. Sullivan focuses on advancing knowledge of IPV, posttraumatic stress, substance use, and HIV/sexual risk. At the system-level, she focuses on understanding the capacity of systems to meet the unique needs of IPV-exposed women.
Footnotes
Of note, physical neglect has at times been found to overlap with poverty. Readers can refer to the following authors for further discussion, e.g., Carter and Myers (2007), McSherry (2004), or Slack, Holl, McDabiel, Yoo, and Bolger (2004).
Contributor Information
Véronique Jaquier, Yale University, School of Medicine, Department of Psychiatry The Consultation Center, 389 Whitney Avenue, New Haven, CT 06511 veronique.jaquier@yale.edu.
Tami P. Sullivan, Yale University, School of Medicine, Department of Psychiatry The Consultation Center, 389 Whitney Avenue, New Haven, CT 06511.
REFERENCES
- Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;19:716–723. doi: 10.1109/TAC.1974.1100705. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. APA; Washington D.C.: 1994. [Google Scholar]
- Arbuckle JL. Amos (Version 19.0) [Computer program] SPSS Inc.; Chicago, IL: 2010. [Google Scholar]
- Babcock JC, Miller SA, Siard C. Toward a typology of abusive women: Differences between partner-only and generally violent women in the use of violence. Psychology of Women Quarterly. 2003;27(2):153–161. doi: 10.1111/1471-6402.00095. [Google Scholar]
- Banyard VL, Williams LM, Saunders BE, Fitzgerald MM. The Complexity of Trauma Types in the Lives of Women in Families Referred for Family Violence: Multiple Mediators of Mental Health. American Journal of Orthopsychiatry. 2008;78(4):394–404. doi: 10.1037/a0014314. doi: 10.1037/a0014314. [DOI] [PubMed] [Google Scholar]
- Barnett O, Miller-Perrin CL, Perrin RD, editors. Family violence across the lifespan. An Introduction. 2nd ed. Sage; Thousand Oaks, CA: 2005. [Google Scholar]
- Barrett BJ, Pierre MS. Variations in Women's Help Seeking in Response to Intimate Partner Violence: Findings From a Canadian Population-Based Study. Violence Against Women. 2011;17(1):47–70. doi: 10.1177/1077801210394273. doi: 10.1177/1077801210394273. [DOI] [PubMed] [Google Scholar]
- Beck JG, McNiff J, Clapp JD, Olsen SA, Avery ML, Hagewood JH. Exploring Negative Emotion in Women Experiencing Intimate Partner Violence: Shame, Guilt, and PTSD. Behavior Therapy. 2011;42(4):740–750. doi: 10.1016/j.beth.2011.04.001. doi: 10.1016/j.beth.2011.04.001. [DOI] [PubMed] [Google Scholar]
- Becker KD, Stuewig J, McCloskey LA. Traumatic Stress Symptoms of Women Exposed to Different Forms of Childhood Victimization and Intimate Partner Violence. Journal of Interpersonal Violence. 2010;25(9):1699–1715. doi: 10.1177/0886260509354578. doi: 10.1177/0886260509354578. [DOI] [PubMed] [Google Scholar]
- Bell KM, Orcutt HK. Posttraumatic Stress Disorder and Male-Perpetrated Intimate Partner Violence. JAMA: The Journal of the American Medical Association. 2009;302(5):562–564. doi: 10.1001/jama.2009.1126. doi: 10.1001/jama.2009.1126. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L. Childhood trauma questionnaire: A retrospective self-report questionnaire and manual. The Psychological Corporation; San Antonio, TX: 1998. [Google Scholar]
- Bonomi AE, Anderson ML, Rivara FP, Thompson RS. Health Outcomes in Women with Physical and Sexual Intimate Partner Violence Exposure. Journal of Women's Health. 2007;16(7):987–997. doi: 10.1089/jwh.2006.0239. doi: doi:10.1089/jwh.2006.0239. [DOI] [PubMed] [Google Scholar]
- Bonomi AE, Thompson RS, Anderson M, Rivara FP, Holt VL, Carrell D, Martin DP. Ascertainment of intimate partner violence using two abuse measurement frameworks. Injury Prevention. 2006;12(2):121–124. doi: 10.1136/ip.2005.009563. doi: 10.1136/ip.2005.009563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SJ, McDonald EA, Krastev AH. Fear of an intimate partner and women's health in early pregnancy: findings from the Maternal Health Study. Birth. 2008;35(4):293–302. doi: 10.1111/j.1523-536X.2008.00256.x. doi: 10.1111/j.1523-536X.2008.00256.x. [DOI] [PubMed] [Google Scholar]
- Bybee D, Sullivan CM. Predicting re-victimization of battered women 3 years after exiting a shelter program. American Journal of Community Psychology. 2005;36(1):85–96. doi: 10.1007/s10464-005-6234-5. doi: 10.1007/s10464-005-6234-5. [DOI] [PubMed] [Google Scholar]
- Campbell JC. Health consequences of intimate partner violence. The Lancet. 2002;359(9314):1331–1336. doi: 10.1016/S0140-6736(02)08336-8. doi: 10.1016/S0140-6736(02)08336-8. [DOI] [PubMed] [Google Scholar]
- Carter V, Myers MR. Exploring the risks of substantiated physical neglect related to poverty and parental characteristics: A national sample. Children and Youth Services Review. 2007;29(1):110–121. [Google Scholar]
- Cattaneo Bennett L, Goodman L. Risk factors for reabuse in intimate partner violence: A cross-disciplinary critical review. Trauma, Violence & Abuse. 2005;6(2):141–175. doi: 10.1177/1524838005275088. doi: 10.1177/1524838005275088. [DOI] [PubMed] [Google Scholar]
- Cercone JJ, Beach SR, Arias I. Gender Symmetry in Dating Intimate Partner Violence: Does Similar Behavior Imply Similar Constructs? Violence and Victims. 2005;20(2):207–218. doi: 10.1891/vivi.2005.20.2.207. [PubMed] [Google Scholar]
- Cheung GW, Lau RS. Testing Mediation and Suppression Effects of Latent Variables. Organizational Research Methods. 2008;11(2):296–325. doi: 10.1177/1094428107300343. [Google Scholar]
- Clements K, Holtzworth-Munroe A. Participation in laboratory research result in emotional distress with one's partner: Comparing violent and nonviolent couples. Journal of Family Violence. 2009;24(5):283–295. doi: 10.1007/s10896-009-9229-4. [Google Scholar]
- Coid J, Petruckevitch A, Feder G, Chung W-S, Richardson J, Moorey S. Relation between childhood sexual and physical abuse and risk of revictimisation in women: a cross-sectional survey. The Lancet. 2001;358(9280):450–454. doi: 10.1016/s0140-6736(01)05622-7. doi: 10.1016/S0140-6736(01)05622-7. [DOI] [PubMed] [Google Scholar]
- Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, Hall Smith P. Physical and Mental Health Effects of Intimate Partner Violence for Men and Women. American Journal of Preventive Medicine. 2002;23(4):260–268. doi: 10.1016/s0749-3797(02)00514-7. doi: 10.1016/S0749-3797(02)00514-7. [DOI] [PubMed] [Google Scholar]
- Cole J, Logan TK, Shannon L. Women's risk for revictimization by a new abusive partner: For what should we be looking? Violence and Victims. 2008;23(3):315–330. doi: 10.1891/0886-6708.23.3.315. doi: 10.1891/0886-6708.23.3.315. [DOI] [PubMed] [Google Scholar]
- Dearwater SR, Coben JH, Campbell JC, Nah G, Glass N, McLoughlin E, Bekemeier B. Prevalence of Intimate Partner Abuse in Women Treated at Community Hospital Emergency Departments. JAMA: The Journal of the American Medical Association. 1998;280(5):433–438. doi: 10.1001/jama.280.5.433. doi: 10.1001/jama.280.5.433. [DOI] [PubMed] [Google Scholar]
- Ellsberg M, Jansen HAFM, Heise L, Watts CH, Garcia-Moreno C. Intimate partner violence and women's physical and mental health in the WHO multi-country study on women's health and domestic violence: An observational study. The Lancet. 2008;371(9619):1165–1172. doi: 10.1016/S0140-6736(08)60522-X. [DOI] [PubMed] [Google Scholar]
- Fanslow JL, Robinson EM. Help-Seeking Behaviors and Reasons for Help Seeking Reported by a Representative Sample of Women Victims of Intimate Partner Violence in New Zealand. Journal of Interpersonal Violence. 2010;25(5):929–951. doi: 10.1177/0886260509336963. doi: 10.1177/0886260509336963. [DOI] [PubMed] [Google Scholar]
- Foa EB. Posttraumatic Stress Diagnostic Scale manual. National Computer Systems Pearson, Inc; Minneapolis, MN: 1995. [Google Scholar]
- Follette VM, Polusny MA, Bechtle AE, Naugle AE. Cumulative trauma: The impact of child sexual abuse, adult sexual assault, and spouse abuse. Journal of Traumatic Stress. 1996;9(1):25–35. doi: 10.1007/BF02116831. doi: 10.1007/bf02116831. [DOI] [PubMed] [Google Scholar]
- Golder S, Logan TK. Cumulative Victimization, Psychological Distress, and High- Risk Behavior Among Substance-Involved Women. Violence and Victims. 2011;26(4):477–495. doi: 10.1891/0886-6708.26.4.477. doi: 10.1891/0886-6708.26.4.477. [DOI] [PubMed] [Google Scholar]
- Golding JM. Intimate partner violence as a risk factor for mental disorders: A meta-analysis. Journal of Family Violence. 1999;14(2):99–132. doi: 10.1023/A:1022079418229. [Google Scholar]
- Hamberger LK, Guse CE. Men's and Women's Use of Intimate Partner Violence in Clinical Samples: Toward a gender-sensitive analysis. Violence Against Women. 2002;8(11):1301–1331. doi: 10.1177/107780102762478028. [PubMed] [Google Scholar]
- Hathaway JE, Mucci LA, Silverman JG, Brooks DR, Mathews R, Pavlos CA. Health status and health care use of Massachusetts women reporting partner abuse. American Journal of Preventive Medicine. 2000;19(4):302–307. doi: 10.1016/s0749-3797(00)00236-1. doi: 10.1016/S0749-3797(00)00236-1. [DOI] [PubMed] [Google Scholar]
- Houry D, Rhodes KV, Kemball RS, Click L, Cerulli C, McNutt LA, Kaslow NJ. Differences in Female and Male Victims and Perpetrators of Partner Violence With Respect to WEB Scores. Journal of Interpersonal Violence. 2008;23(8):1041–1055. doi: 10.1177/0886260507313969. doi: 10.1177/0886260507313969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, Gottman JM, Waltz J, Rushe R, Babcock J, Holtzworth-Munroe A. Affect, Verbal Content, and Psychophysiology in the Arguments of Couples With a Violent Husband. Journal of Consulting and Clinical Psychology. 1994;62(5):982–988. doi: 10.1037//0022-006x.62.5.982. doi: 10.1037//0022-006X.62.5.982. [DOI] [PubMed] [Google Scholar]
- Johnson MP. Conflict and Control: Gender Symmetry and Asymmetry in Domestic Violence. Violence Against Women. 2006;12(11):1003–1018. doi: 10.1177/1077801206293328. doi: 10.1177/1077801206293328. [DOI] [PubMed] [Google Scholar]
- Johnson MP. A typology of domestic violence: Intimate terrorism, violent resistance, and situational couple violence. Northeastern University; Lebanon, NH: 2008. [Google Scholar]
- Kemp A, Green BL, Hovanitz C, Rawlings EI. Incidence and Correlates of Posttraumatic Stress Disorder in Battered Women. Journal of Interpersonal Violence. 1995;10(1):43–55. doi: 10.1177/088626095010001003. [Google Scholar]
- Kenny DA. [May 16, 2011];Respecification of latent variable models. 1999 from http://davidakenny.net/cm/respec.htm.
- Kilpatrick DG, Saunders BE, Amick-McMullan A, Best CL, Veronen LJ, Resnick HS. Victim and crime factors associated with the development of crime-related post-traumatic stress disorder. Behavior Therapy. 1989;20(2):199–214. doi: 10.1016/s0005-7894(89)80069-3. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 3rd ed. The Guilford Press; New York: 2011. [Google Scholar]
- Koss MP, Gidycz CA. The Sexual Experiences Survey: Reliability and validity. Journal of Consulting and Clinical Psychology. 1985;53(3):442–443. doi: 10.1037//0022-006x.53.3.422. doi: 10.1037//0022-006X.53.3.422. [DOI] [PubMed] [Google Scholar]
- Krause ED, Kaltman S, Goodman L, Dutton MA. Role of distinct PTSD symptoms in intimate partner reabuse: A prospective study. Journal of Traumatic Stress. 2006;19(4):507–516. doi: 10.1002/jts.20136. doi: 10.1002/jts.20136. [DOI] [PubMed] [Google Scholar]
- Krause ED, Kaltman S, Goodman LA, Dutton MA. Longitudinal Factor Structure of Posttraumatic Stress Symptoms Related to Intimate Partner Violence. Psychological Assessment. 2007;19(2):165–175. doi: 10.1037/1040-3590.19.2.165. doi: 10.1037/1040-3590.19.2.165. [DOI] [PubMed] [Google Scholar]
- Krishnan SP, Hilbert JC, Pase M. An Examination of Intimate Partner Violence in Rural Communities: Results from a Hospital Emergency Department Study from Southwest United States. Family & Community Health. 2001;24(1):1–14. doi: 10.1097/00003727-200104000-00004. [DOI] [PubMed] [Google Scholar]
- Langhinrichsen-Rohling J, Neidig P, Thorn G. Violent marriages: Gender differences in levels of current violence and past abuse. Journal of Family Violence. 1995;10(2):159–176. doi: 10.1007/bf02110598. [Google Scholar]
- Levendosky AA, Graham-Bermann SA. Parenting in Battered Women: The Effects of Domestic Violence on Women and Their Children. Journal of Family Violence. 2001;16(2):171–192. doi: 10.1023/a:1011111003373. [Google Scholar]
- Logan TK, Walker R, Jordan CE, Leukefeld CG. Women and victimization: Contributing factors, interventions, and implications. American Psychological Association; Washington, DC: 2006. [Google Scholar]
- Lowe P, Humphreys C, Williams SJ. Night Terrors: Women's Experiences of (Not) Sleeping Where There Is Domestic Violence. Violence Against Women. 2007;13(6):549–561. doi: 10.1177/1077801207301556. doi: 10.1177/1077801207301556. [DOI] [PubMed] [Google Scholar]
- McSherry D. Which Came First, the Chicken or the Egg? Examining the Relationship between Child Neglect and Poverty. British Journal of Social Work. 2004;34(5):727–733. [Google Scholar]
- Mechanic MB, Weaver TL, Resick PA. Mental Health Consequences of Intimate Partner Abuse: A Multidimensional Assessment of Four Different Forms of Abuse. Violence Against Women. 2008;14(6):634–654. doi: 10.1177/1077801208319283. doi: 10.1177/1077801208319283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messman-Moore TL, Long PJ. Child sexual abuse and revictimization in the form of adult sexual abuse, adult physical abuse, and adult psychological maltreatment. Journal of Interpersonal Violence. 2000;15(5):489–502. doi: 10.1177/088626000015005003. [Google Scholar]
- Miller J. A Specification of the Types of Intimate Partner Violence Experienced by Women in the General Population. Violence Against Women. 2006;12(12):1105–1131. doi: 10.1177/1077801206293501. doi: 10.1177/1077801206293501. [DOI] [PubMed] [Google Scholar]
- Morse BJ. Beyond the Conflict Tactics Scale: Assessing Gender Differences in Partner Violence. Violence and Victims. 1995;10:251–272. [PubMed] [Google Scholar]
- Nishith P, Mechanic MB, Resick PA. Prior Interpersonal Trauma: The Contribution to Current PTSD Symptoms in Female Rape Victims. Journal of Abnormal Psychology. 2000;109(1):20–25. doi: 10.1037//0021-843X.109.1.20. [PMC free article] [PubMed] [Google Scholar]
- Noll JG, Horowitz LA, Bonanno GA, Trickett PK, Putnam FW. Revictimization and self-harm in females who experienced childhood sexual abuse: Results from a prospective study. Journal of Interpersonal Violence. 2003;18(12):1452–1471. doi: 10.1177/0886260503258035. doi: 10.1177/0886260503258035. [DOI] [PubMed] [Google Scholar]
- Olson EC, Kerker BD, McVeigh KH, Stayton C, Wye GV, Thorpe L. Profiling risk of fear of an intimate partner among men and women. Preventive Medicine. 2008;47(5):559–564. doi: 10.1016/j.ypmed.2008.08.005. doi: 10.1016/j.ypmed.2008.08.005. [DOI] [PubMed] [Google Scholar]
- Phelan MB, Hamberger LK, Guse CE, Edwards S, Walczak S, Zosel A. Domestic Violence Among Male and Female Patients Seeking Emergency Medical Services. Violence and Victims. 2005;20:187–206. doi: 10.1891/vivi.2005.20.2.187. [PubMed] [Google Scholar]
- Pico-Alfonso MA. Psychological intimate partner violence: the major predictor of posttraumatic stress disorder in abused women. Neuroscience & Biobehavioral Reviews. 2005;29(1):181–193. doi: 10.1016/j.neubiorev.2004.08.010. doi: 10.1016/j.neubiorev.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Pico-Alfonso MA, Garcia-Linares MI, Celda-Navarro N, Blasco-Ros C, Echeburúa E, Martinez M. The Impact of Physical, Psychological, and Sexual Intimate Male Partner Violence on Women's Mental Health: Depressive Symptoms, Posttraumatic Stress Disorder, State Anxiety, and Suicide. Journal of Women's Health. 2006;15(5):599–611. doi: 10.1089/jwh.2006.15.599. doi: 10.1089/jwh.2006.15.599. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. doi: 10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- Riggs DS, Kilpatrick DG, Resnick HS. Long-term psychological distress associated with marital rape and aggravated assault: A comparison to other crime victims. Journal of Family Violence. 1992;7(4):283–296. doi: 10.1007/bf00994619. [Google Scholar]
- Scheffer Lindgren M, Renck B. ‘It is still so deep-seated, the fear’: psychological stress reactions as consequences of intimate partner violence. Journal of Psychiatric and Mental Health Nursing. 2008;15(3):219–228. doi: 10.1111/j.1365-2850.2007.01215.x. doi: 10.1111/j.1365-2850.2007.01215.x. [DOI] [PubMed] [Google Scholar]
- Schumm JA, Briggs-Phillips M, Hobfoll SE. Cumulative interpersonal traumas and social support as risk and resiliency factors in predicting PTSD and depression among inner-city women. Journal of Traumatic Stress. 2006;19(6):825–836. doi: 10.1002/jts.20159. doi: 10.1002/jts.20159. [DOI] [PubMed] [Google Scholar]
- Scott-Storey K. Cumulative Abuse: Do Things Add Up? An Evaluation of the Conceptualization, Operationalization, and Methodological Approaches in the Study of the Phenomenon of Cumulative Abuse. Trauma, Violence, & Abuse. 2011;12(3):135–150. doi: 10.1177/1524838011404253. doi: 10.1177/1524838011404253. [DOI] [PubMed] [Google Scholar]
- Sippel LM, Marshall AD. Posttraumatic stress disorder symptoms, intimate partner violence perpetration, and the mediating role of shame processing bias. Journal of Anxiety Disorders. 2011;25(7):903–910. doi: 10.1016/j.janxdis.2011.05.002. doi: 10.1016/j.janxdis.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slack KS, Holl JL, McDaniel M, Yoo J, Bolger K. Understanding the Risks of Child Neglect: An Exploration of Poverty and Parenting Characteristics. Child Maltreatment. 2004;9(4):395–408. doi: 10.1177/1077559504269193. [DOI] [PubMed] [Google Scholar]
- Smith PH, Tessaro I, Earp JAL. Women's experiences with battering: A conceptualization from qualitative research. Women's Health Issues. 1995;5(4):173–182. doi: 10.1016/1049-3867(95)00615-X. doi: 10.1016/1049-3867(95)00615-x. [DOI] [PubMed] [Google Scholar]
- Smith PH, White JW, Holland LJ. A Longitudinal Perspective on Dating Violence Among Adolescent and College-Age Women. American Journal of Public Health. 2003;93(7):1104–1109. doi: 10.2105/ajph.93.7.1104. doi: 10.2105/ajph.93.7.1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straus MA. The controversy over domestic violence by women: A methodological, theoretical, and sociology of science analysis. In: Arriaga XB, Oskamp S, editors. Violence in intimate relationships. Sage; Thousand Oaks, CA: 1999. pp. 17–44. [Google Scholar]
- Straus MA, Hamby SL, Warren WL. The Conflict Tactics Scales handbook. Western Psychological Services; Los Angeles: 2003. [Google Scholar]
- Sullivan TP, Cavanaugh CE, Buckner JD, Edmondson D. Testing posttraumatic stress as a mediator of physical, sexual, and psychological intimate partner violence and substance problems among women. Journal of Traumatic Stress. 2009;22(6):575–584. doi: 10.1002/jts.20474. doi: 10.1002/jts.20474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan TP, Holt LJ. PTSD symptom clusters are differentially related to substance use among community women exposed to intimate partner violence. Journal of Traumatic Stress. 2008;21(2):173–180. doi: 10.1002/jts.20318. doi: 10.1002/jts.20318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swan SC, Sullivan TP. Past Abusive Behavior Inventory (unpublished measure) Yale University; New Haven, CT: 2004. [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 6th ed. Allyn and Bacon; Boston, MA: 2012. [Google Scholar]
- Testa M, Livingston JA, VanZile-Tamsen C. Advancing the Study of Violence Against Women Using Mixed Methods: Integrating Qualitative Methods Into a Quantitative Research Program. Violence Against Women. 2011;17(2):236–250. doi: 10.1177/1077801210397744. doi: 10.1177/1077801210397744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson MP, Arias I, Basile KC, Desai S. The association between childhood physical and sexual victimization and health problems in adulthood in a nationally representative sample of women. Journal of Interpersonal Violence. 2002;17(10):1115–1129. doi: 10.1177/088626002236663. [Google Scholar]
- Thompson RS, Bonomi AE, Anderson M, Reid RJ, Dimer JA, Carrell D, Rivara FP. Intimate Partner Violence: Prevalence, Types, and Chronicity in Adult Women. American Journal of Preventive Medicine. 2006;30(6):447–457. doi: 10.1016/j.amepre.2006.01.016. doi: 10.1016/j.amepre.2006.01.016. [DOI] [PubMed] [Google Scholar]
- Tolman RM. The development of a measure of psychological maltreatment of women inventory. Violence and Victims. 1989;14:25–38. [PubMed] [Google Scholar]
- Tolman RM. The validation of the psychological maltreatment of women inventory. Violence and Victims. 1999;14(1):25–35. [PubMed] [Google Scholar]
- Vogel L, Marshall L. PTSD Symptoms and Partner Abuse: Low Income Women at Risk. Journal of Traumatic Stress. 2001;14(3):569–584. doi: 10.1023/A:1011116824613. doi: 10.1023/a:1011116824613. [DOI] [PubMed] [Google Scholar]
- Watt MH, Bobrow EA, Moracco KE. Providing Support to IPV Victims in the Emergency Department. Violence Against Women. 2008;14(6):715–726. doi: 10.1177/1077801208317290. doi: 10.1177/1077801208317290. [DOI] [PubMed] [Google Scholar]
- Weaver TL, Clum GA. Psychological distress associated with interpersonal violence: A meta-analysis. Clinical Psychology Review. 1995;15(2):115–140. doi: 10.1016/0272-7358(95)00004-9. [Google Scholar]
- Yoshihama M, Horrocks J. The Relationship Between Intimate Partner Violence and PTSD: An Application of Cox Regression with Time-Varying Covariates. Journal of Traumatic Stress. 2003;16(4):371–380. doi: 10.1023/A:1024418119254. doi: 10.1023/A:1024418119254. [DOI] [PubMed] [Google Scholar]