Abstract
The mammalian gut microbiota is essential for normal intestinal development, renewal and repair. Injury to the intestinal mucosa can occur with infection, surgical trauma, and in idiopathic inflammatory bowel disease. Repair of mucosal injury, termed restitution, as well as restoration of intestinal homeostasis involves induced and coordinated proliferation and migration of intestinal epithelial cells. N-formyl peptide receptors (FPRs) are widely expressed pattern recognition receptors that can specifically bind and induce responses to host derived and bacterial peptides and small molecules. Here we report that specific members of the gut microbiota stimulate FPR1 on intestinal epithelial cells to generate reactive oxygen species via enterocyte NADPH oxidase NOX1, causing rapid phosphorylation of Focal Adhesion Kinase (FAK) and ERK MAPK. These events stimulate migration and proliferation of enterocytes adjacent to colonic wounds. Together, these findings identify a novel role of FPR1 as pattern recognition receptors for perceiving the enteric microbiota that promotes repair of mucosal wounds via generation of ROS from the enterocyte NOX1.
Keywords: Epithelia, Formyl peptide receptors, microbiota, lactobacilli, wound healing
INTRODUCTION
The gastrointestinal epithelium acts as a physiologic barrier that separates the underlying systemic tissue compartments from the microbe-rich gut luminal contents. Defects in this barrier occur with inflammatory bowel diseases (IBD) as well as infectious and mechanical injury.1,2 Additionally, intrinsic defects in mucosal barrier homeostasis are likely central to the pathogenesis of IBD and systemic inflammatory syndromes. The mammalian intestinal tract is host to, and coevolved with, a taxonomically diverse and numerically vast prokaryotic microbiota. The resident microbial community in the intestinal lumen is essential for numerous beneficial functions including nutrient extraction, immune development, and competitive exclusion of pathogens.3 In addition, recent data have implicated the microbiota in the mucosal tissue development and renewal. Germ-free mice exhibit slower turnover of the intestinal epithelial cells (IEC)3 and epithelial regenerative responses to mucosal injury are impaired, suggesting a role for the microbiota in stimulation of wound restitution and response to injury.4–6 However, the mechanistic processes by which the host perceives the enteric microbiota to stimulate these beneficial effects is largely unknown.
The formyl peptide receptors (FPRs) are G-protein coupled transmembrane receptors originally characterized in phagocytes, which upon stimulation by microbially derived formylated peptides, induce chemotaxis and reactive oxygen species (ROS) generation in these cells7–10 indicating the role of FPRs as pattern recognition receptors. Functional FPRs are described in the intestinal epithelial cells that serve as receptors for endogenous anti-inflammatory and pro-resolution mediators, including annexin A1 (AnxA1), lipoxin A4, resolving D1.11–14 Recently, Chen et al. utilized FPR2 null mice to demonstrate defective healing in models of chemical colits,15 suggesting functional roles of the FPRs in the intestinal mucosa. Importantly, our prior work showed AnxA1 requires FPR1 and the enterocyte NADPH oxidase, NOX1 for mucosal wound healing13 in a ROS-dependent manner. Physiological levels of cellular ROS function as a signaling molecule and modulate different homeostatic processes, including those implicated in migration and cellular proliferation.16–18 FPRs expressed in IECs are in direct contact with the gut luminal contents11 and thus can also be activated by exogenous ligands, including microbial formyl peptides and certain taxa of the gut microbiota.15,19
We and others reported that specific taxa of enteric bacteria, largely lactobacilli, stimulate ROS production in the gut of animals as disparate as mammals and flies.13,20,21 (Jones et al. unpublished data). Recently, we demonstrated that microbiota induced ROS generation promotes migration of cultured enterocytes by activating phosphorylation of focal adhesion kinase (FAK) in a redox dependent manner.21 FAK is a key regulatory protein of focal adhesion complex – that mediates turnover of cell adhesions, affects cell migration, and thus regulates wound repair.22,23 However, the receptor that recognizes bacterial signals and the cellular source of ROS that promote enterocyte migration, and thus mediate microbiota-induced intestinal wound healing and homeostasis, are unknown.
In this report, we examined the role of FPR1 as pattern recognition receptors in perception of enteric commensal mediated signaling in vivo and demonstrated that FPR1 mediates commensal bacteria-stimulated NOX1-dependent ROS generation in colonic enterocytes, which in turn activates phosphorylation of FAK and ERK in vivo, culminating in migration and proliferation that are required for intestinal homeostasis and wound restitution. Overall, these results identify redox signaling as a key mechanism in the host crosstalk of the microbiota in homeostatic and restitutive processes.
RESULTS
Enteric commensal bacteria-stimulated colonic mucosal wound healing requires FPR1 and NOX1
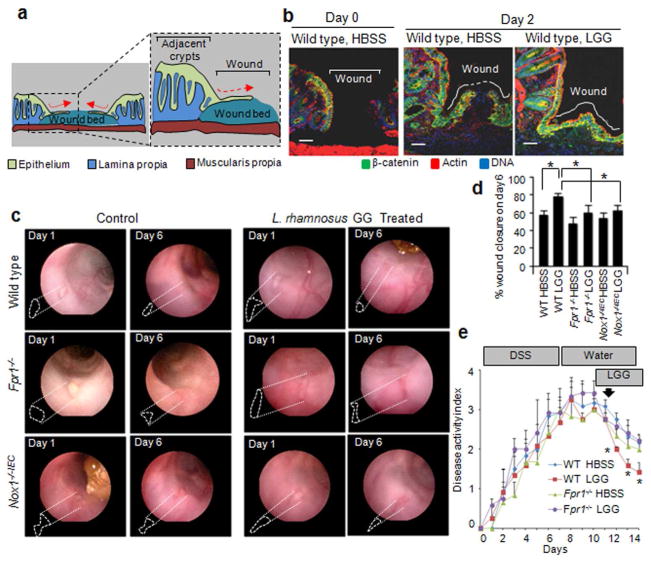
To assess the extent to which FPR1 and NOX1 function in microbiota-induced restitution, discrete and reproducible mechanical wounds (Supplementary Figure S1, and Figure 1a) were inflicted in murine colonic epithelial mucosa with veterinary endoscopic biopsy forceps, followed by intrarectal administration of control (Hank’s buffer; HBSS) or L. rhamnosus GG (LGG), a representative commensal bacterium that activates FPRs in cultured IEC.19 LGG-treated wound beds rapidly re-epithelialized within 2 days, whereas HBSS treated wounds re-epithelialized at a significantly slower rate demonstrated by the monolayer of β-catenin containing epithelial cells (green) covering the wound beds (Figure 1b, and Supplementary Figure S1c). LGG-enhanced wound closure was quantified utilizing the method24 described by Seno et al. in WT mice, in mice with germ line mutations in FPR1 (Fpr1−/−), and in mice harboring an epithelial specific knockout in Nox1 (Noxfl/FL x Villin-Cre, designated Nox1−/−IEC) (Supplementary Figure S1d, and Figure 1c,d). In wild type mice, wounds treated with LGG for 6 days showed enhanced mucosal closure (78.5%) when compared to control treatment (57.4%). However, LGG failed to enhance wound closure in Fpr1−/− and Nox1−/−IEC mice (59.3% and 62.7% respectively) (Figure 1c,d). Untreated Fpr1−/− and Nox1−/−IEC mice did not show significant delays (48.0% and 53.1% respectively) in wound healing when compared to wild type mice. These data demonstrate that commensal bacteria augment repair of mucosal injury that requires FPR1 and NOX1 signaling pathways. In a separate model of epithelial restitution, mice were given 4.0% dextran sodium sulfate (DSS) in drinking water and Disease Activity Index (body weight loss, stool consistency and occult blood; DAI) was recorded. DSS was withdrawn and replaced with water, and animals were subsequently treated with intrarectal administration of LGG suspension or control for 3 days. As previously reported,21 LGG treatment enhanced recovery from DSS-induced injury (Figure 1e). Importantly, the beneficial effects of LGG post-DSS treatment were absent in Fpr1−/− mice. Collectively, these data demonstrate that FPR1 is also necessary in microbiota-induced recovery from intestinal injury induced by DSS treatment.
Figure 1.
Enteric commensal bacteria require FPR1 and NOX1 to enhance colon mucosal healing. (a) Schematic diagram showing a transverse section of a wound bed surrounded by crypts where epithelial cells proliferate in and migrate from to cover the wound bed.24,29 (b) Immunofluorescence staining of wound beds in the colon of wild type mice using antibody against β-catenin (green) and stained with actin (red) and DNA (blue). Mice were treated intrarectally with LGG (2.5×109 cfu) or HBSS for two days. The wound bed center is described in methods and Supplementary Figure S1. Scale bar, 50μm. (c) Endoscopic images of colonic wounds in mice (wild type, Fpr1−/− and Nox1−/−IEC) at day 1 and 6. Bioptic injuries were inflicted following the method24 described by Seno et al. n=5 mice/group. Mice were treated as above for 6 days. Dotted lines outline the depressed area margin of the lesion at each time point. (d) Graph shows percent wound closure on day 6. Results are shown as means ± SD and *P < 0.05, by Student’s t test. (e) Clinical disease activity index of mice subjected to DSS colitis for 7 days followed by recovery from colitis for 7 days. Graph is highlighted for intrarectal administration of LGG or HBSS for 3 days post DSS replacement with water. n=6 mice / group. Data in graph are presented as mean ± SEM. **P < 0.05, WT HBSS vs. WT LGG, and WT LGG vs. Fpr1−/− LGG by ANOVA with Tukey’s multiple comparison post-test.
Enteric commensal bacteria induce FPR1- and NOX1-dependent ROS generation in murine colonic epithelia
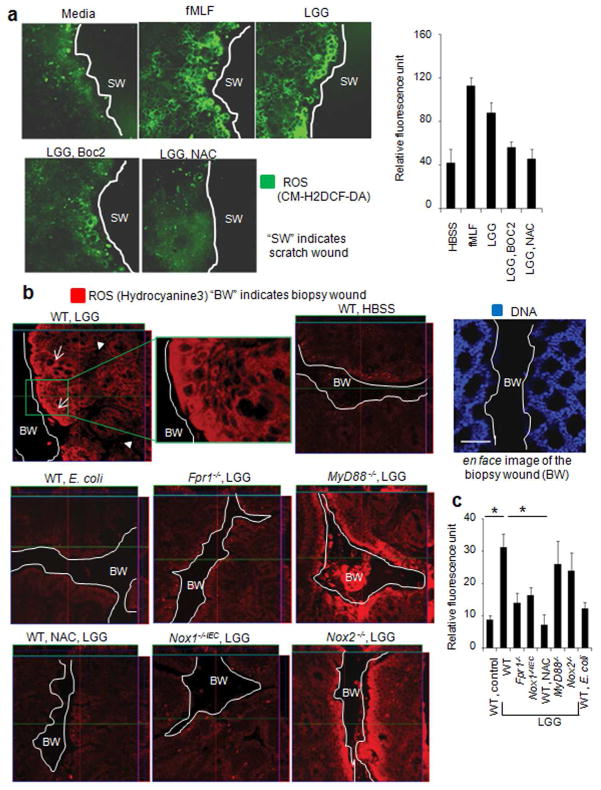
We hypothesized that, similar to AnxA1, products of the resident microbiota recognized by FPR1 require epithelial NOX1 to generate ROS and activate signaling pathways that eventuate in epithelial migration and restitution. Therefore, we investigated the extent to which commensal bacteria or fMLF activated FPRs situated on the apical surface of epithelial cells and mediated ROS response. Cellular ROS was determined in cultured polarized SK-CO15 colonic epithelial cells using redox sensitive CM-H2DCF-DA dye. We demonstrated that both LGG and fMLF stimulated ROS generation within 15 minutes in cultured SK-CO15 epithelial cells in a dose-dependent manner (Supplementary Figure S2a), highlighting the enterocytes’ ability to independently generate cellular ROS following bacterial contact. In addition, these ROS were produced in the cytoplasmic area of the epithelial cells but not in the nucleus (Supplementary Figure S2a, right panel). Next we examined effects of fMLF and LGG to induce ROS generation in wounded model polarized epithelial cells. ROS were rapidly generated in cells within 15 min of application with fMLF and LGG (Figure 2a) Intriguingly, in response to application of fMLF and LGG, cells located in close proximity of the wound edges produced more ROS evident from the stronger fluorescent signals generated from CM-H2DCF-DA. Additionally, LGG-induced ROS generation in wounded cultured enterocytes was abrogated in cells pretreated with Boc2, a specific and competitive inhibitor of fMLF binding to FPRs, and also by NAC, a glutathione (GSH) precursor and ROS scavenger (Figure 2a). These data demonstrate that LGG activated FPR to induce ROS generation in the wounded model polarized epithelial cells.
Figure 2.
Commensal bacteria-induced ROS generation in intestinal epithelia requires FPR1 and NOX1. (a) CM-H2DCF-DA (5 μM)-mediated detection of ROS in scratch-wounded (SW) polarized SK-CO15 cells treated with fMLF or LGG (2.5×107 cfu/ml) over 15 min. White lines depict scratch-wounded area. Quantitative representation (right) of ROS production in a. Fluorescence intensity was measured by ImageJ software and expressed in units of fluorescence. Results are shown as means ± SD. (b) Detection of ROS in vivo. Mice were loaded with hydrocyanine 3 followed by biopsy wounding (BW) of epithelium. Mucosa was luminally treated for 15 min with HBSS or LGG (2.5×109 cfu). Fluorescence was determined from en face wound bed by confocal laser scanning microscopy (Zeiss). Data represents three independent experiments with n=3 mice per group. White lines, white arrows, and white triangles depict biopsy wounds, enterocytes in colonic crypt units, and lamina propria, respectively. DNA was stained with To-pro 3 for tissue orientation. Scale bar, 50μm. (c) Quantitative representation of ROS production in b. Results are shown as means ± SD and *P < 0.001, by Student’s t test. Fluorescence intensity was measured by ImageJ software and expressed in units of fluorescence.
We next investigated whether commensal bacteria-induced ROS generation occurs in vivo in biopsy-wounded intestinal epithelia by measuring cellular ROS using hydrocyanine 3, a stable intracellular ROS sensitive fluorophore.21,25 Within 15 minutes of intrarectal administration of LGG suspension (2.5×109 cfu), but not HBSS control, wild type mice showed rapid generation of ROS in the colonic epithelial cells (Supplementary Figure S2b, and Figure 2b,c; white arrows), predominately in close proximity of the wounded area. Furthermore, administration of NAC in the mouse distal colon abrogated LGG-stimulated ROS generation (Figure 2b,c). Importantly, administration of E. coli did not induce ROS generation, consistent with our past data indicating that specific strains of bacteria differ in their capacity to induce ROS generation.20 Minimal ROS generation was detected in IECs of Fpr1−/− mice administered LGG (Figure 2b,c), implicating that this receptor is required for commensal mediated ROS generation. The NADPH oxidase family enzymes are the major sources of cellular ROS generation in non-phagocytic cells,26 with NOX1 abundantly expressed in IECs along the crypt-luminal axis.27 ROS generation was markedly reduced in the IECs of Nox1−/−IEC but remained at wild type levels in the Nox2−/− (the phagocyte NADPH oxidase) mouse treated with LGG. Finally, we found that the TLR signaling adaptor MyD88 was not necessary for LGG-stimulated ROS generation (Figure 2b,c). Together, these data show that recognition of the microbiota by FPR1 induced NOX1-dependant ROS generation within the enterocytes.
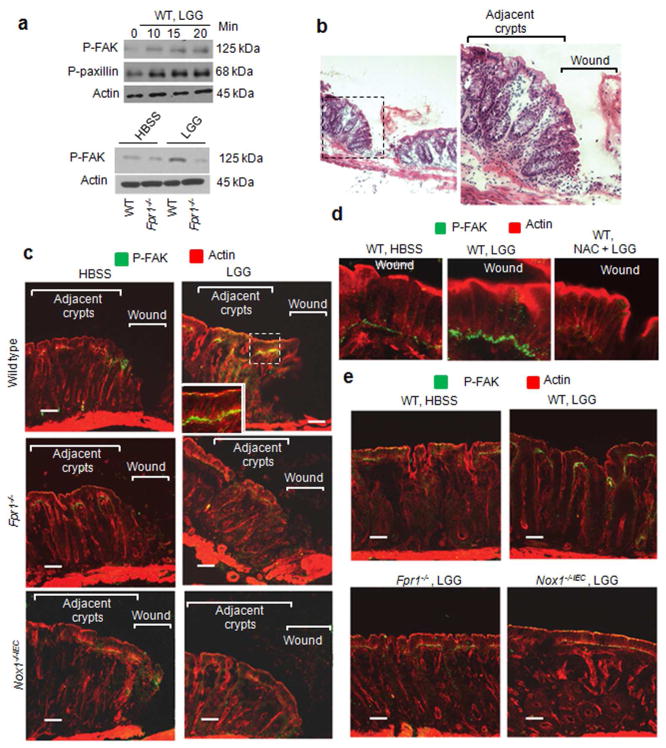
Enteric commensal bacteria-stimulated FAK activation in murine colon depends on FPR1 and NOX1
ROS modulate regulatory pathways important for wound healing18 by reversible oxidative modification of redox sensitive signaling intermediates, often enzymes bearing a low pKa “sensor” cysteines in their active sites, which thereby results in their catalytic inactivation26,28. We recently demonstrated that enteric microbiota-induced ROS generation inactivates LMW_PTP and SHP-2, two related redox sensitive FAK phosphatases, and thereby activates FAK and paxillin phosphorylation in vitro;21 nonetheless, the receptor that recognized microbial signals and the cellular source that generated ROS remained unidentified. Since these proteins are key regulators of epithelial cell migration, in this current study we investigated the role of FPR1 and NOX1 in FAK and paxillin phosphorylation in vivo (Figure 3). Within 15 minutes of the intrarectal administration of LGG suspension, but not HBSS, FAK was rapidly phosphorylated at tyrosine residue 861 (pFAK-Y861) over physiological steady state conditions (control) as detected by immunoblotting ((Supplementary Figure S3a, and Figure 3a) or immunofluorescence microscopy (Figure 3c,d) in wild type mice. Phosphorylated FAK was located at the basal surface of the epithelial cells (Figure 3c,d). Importantly, phosphorylation of FAK was markedly decreased in Fpr1−/− and Nox1−/−IEC mice (Figure 3a and 3c) and in wild type mice pretreated with NAC (Figure 3d). Equal basal levels of unphosphorylated FAK were detected in wild type, Fpr1−/− and Nox1−/−IEC mice (data not shown). Similarly, though much weaker, FPR1 and NOX1 dependent FAK activation was seen in unwounded mucosa (Figure 3e). Together, these data indicate that FPR1 and NOX1 are required for enteric commensal bacteria-stimulated activation of FAK in IECs.
Figure 3.
Enteric commensal bacteria-stimulated FAK activation in murine colon depends on FPR1 and NOX1. (a) Immunoblot analysis of phospho-FAK (pFAK-Y861) in mouse colon at 15 minutes post biopsy injury and treatment with LGG or HBSS. Data are representative of two independent experiments with n=3 mice per group. (b) H&E staining of a biopsy wound bed from wild type mice 15 minutes post injury. (c, d, and e) Immunofluorescence analysis of phospho-FAK in serial sections of colonic tissues harvested from mice treated intrarectally with LGG (2.5×109 cfu) or HBSS for 15 min. (c) Biopsy wounds (n=6 lesions per group). White lines show crypts adjacent to the wound. (d) Biopsy wounds. NAC was instilled 30 min prior to LGG treatment. (e) Intact colonic mucosa. n=5 per group. Scale bar, 50μm. Data are representative of three independent experiments.
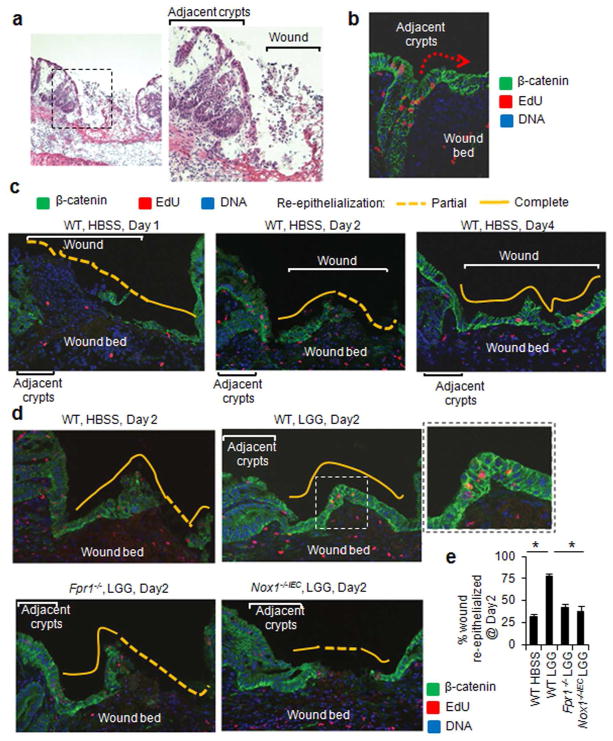
Enteric commensal bacteria-stimulated epithelial cell migration in murine colon requires FPR1 and NOX1
During restitution of colonic wounds, the epithelial cells migrate from the crypts adjacent to the wound site24,29 (Supplementary Figure S3b, left panel). Figure 4a displays crypts adjacent to the wound bed at day 2 in the mouse distal colon. We measured the migration of enterocytes covering the wound bed by a pulse–chase experiment using EdU labeling of crypt epithelial cells following bioptic injury (Supplementary Figure S3b, right panel). EdU is a thymidine analog, which is incorporated in cells only at S-phase. Once labeled, EdU positive cells can be detected after several days. To determine the migration of enterocytes, colonic epithelial wounds were inflicted by biopsy forceps and EdU was injected intraperitonially. Wound bed tissues were subsequently harvested at different days post biopsy injury. Serial sections of wound beds were stained for EdU positive cells (red) as well as immunostained for β-catenin to identify epithelial cells (green). Emigration of EdU labeled enterocytes is seen (red) from the adjacent crypts one day post injury (Figure 4b). In addition, after a four day chase period, we readily found EdU-positive cells in the monolayer of β-catenin containing epithelial cells completely covering the wound beds in wild type control mice (Figure 4c). Interestingly, in the LGG-treated wild type mice, wounds were covered with a monolayer of epithelial cells containing the EdU-marked cells within two days (Figure 4d,e). By comparison, the wound beds in the wild type control or LGG-treated Fpr1−/− and Nox1−/−IEC mice were only partially re-epithelialized at this time point (Figure 4d,e). A similar EdU labeling pulse–chase approach revealed that FPR1 is required in LGG-enhanced crypt-luminal migration of IECs in intact mucosa (Supplementary Figure S3c). Collectively, these data show that LGG-stimulated enterocyte migration is dependent on epithelial FPR1 and NOX1.
Figure 4.
Enteric commensal bacteria-stimulated enterocyte migration in murine colon depends on FPR1 and NOX1. (a) H&E staining of a biopsy wound bed from wild type mice 2 days post injury. (b) EdU stained sections of a WT mouse one day post biopsy injury showing (EdU positive; red) epithelial cells emanating from a crypt. Mice were injected with EdU (I.P.) immediately after endoscopic injury. Wound beds were harvested after one day and serial sections were stained for EdU positive cells and β-catenin. (c) Re-epithelialization of wound beds with EdU labeled enterocytes. Mice were treated as above for 1 – 4 days and injected with EdU (I.P.) immediately after endoscopy. Serial sections of wound beds were stained for EdU positive cells and β-catenin. (d) Re-epithelialization of wound beds with EdU labeled enterocytes in WT, Fpr1−/−, and Nox1−/−IEC mice. Mice were treated as above with HBSS or LGG (2.5×109 cfu) for 2 days and injected with EdU immediately after endoscopy. Sections of wound beds were stained for EdU positive cells and β-catenin. n=5 lesions per group. Data are representative of three independent experiments. White lines show crypts adjacent to the wound. Yellow lines indicate re-epithelialization where the solid yellow lines highlight complete and dotted lines highlight partial re-epithelialization. (e) Quantification of wound re-epithelialization on day 2. Results are shown as means ± SD (n=5) and * P< 0.05 by Student’s t test.
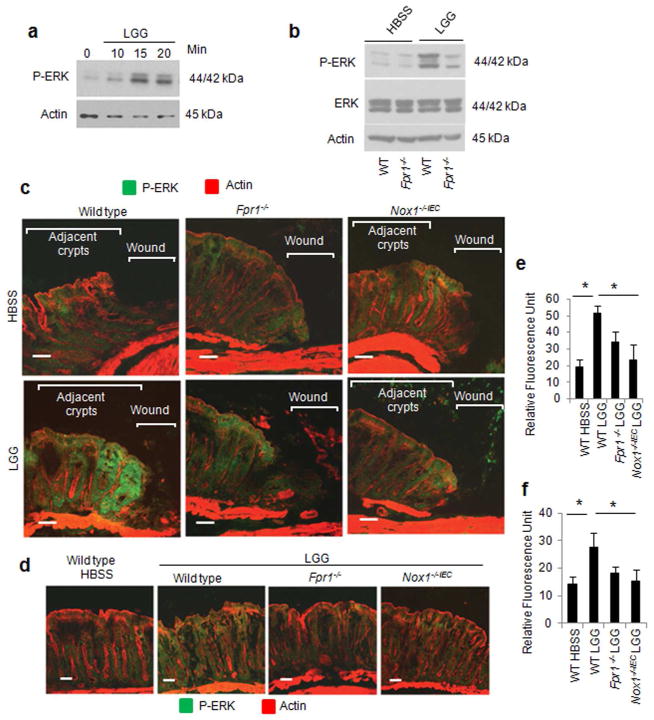
Enteric commensal microbiota-stimulated ERK activation in murine colon requires FPR1 and NOX1
Signaling pathways involved in cellular proliferation, including ERK MAPK pathways, are pivotal components of wound healing. We previously demonstrated that commensal bacteria-induced ROS generation causes oxidative inactivation of the ERK phosphatase DUSP3 and increases ERK phosphorylation;30 however, sources of cellular ROS remained unidentified. In this current study, we thus assessed the role of FPR1 and NOX1 in ERK phosphorylation in vivo by inflicting biopsy injury in the mouse distal colon. Within 15 minutes of the intrarectal administration of LGG suspension, but not HBSS, ERK was rapidly phosphorylated in wild type mice (Supplementary Figure S4, and Figure 5a,b). Interestingly, most phospho-ERK immunolocalized to the 4–5 crypt-villus units adjacent to the biopsy wounds (Figure 5b). Importantly, in response to LGG, markedly reduced levels of ERK phosphorylation was observed in Fpr1−/− and Nox1−/−IEC mice and wild type mice pretreated with NAC (Figure 5a,b,d, and Supplementary Figure S4). Similarly, though much weaker, FPR1 and NOX1 dependent ERK activation was observed in the unwound intact mucosa (Figure 5c,e).
Figure 5.
Commensal bacteria-stimulated ERK activation in crypts adjoining mucosal wounds requires FPR1 and NOX1. (a) Immunoblot analysis for phospho-ERK in colonic epithelial scrapings from harvested biopsy wounds located in the distal colon of wild type and Fpr1−/− mouse after intrarectal administration of HBSS or LGG for 15 min. Data are representative of two independent experiments with n=3 mice per group. (b and c) Immunofluorescence analysis of phospho-ERK in thin sections of colonic tissues from mice treated intrarectally with LGG (2.5×109 cfu) or HBSS for 15 min. (b) Biopsy wounds. n=7 lesions per group. Scale bar, 50μm. (c) Intact colonic mucosa. (d and e) Quantitative representation of immunofluorescence analysis of phospho-ERK in b and c. Results are shown as means ± SD and *P < 0.05 by Student’s t test. Data are representative of three independent experiments with n=3 mice per group.
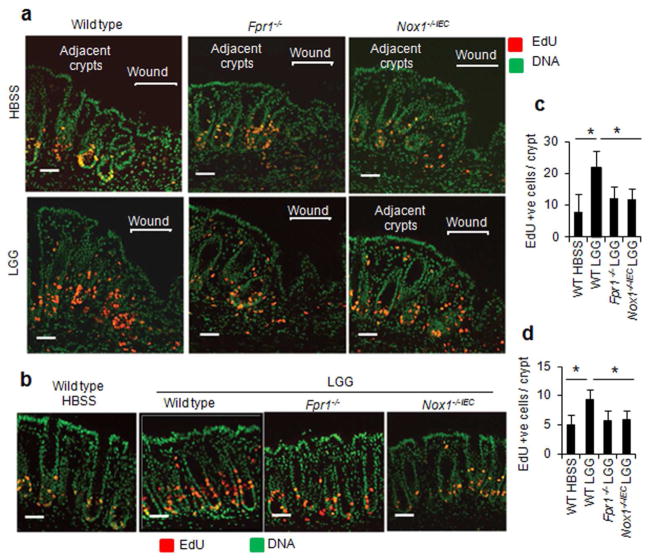
FPR1 and NOX1 are required for enteric commensal bacteria-stimulated proliferation of wound associated colonic epithelial cells
Next, we examined IEC proliferation in crypts adjacent to the biopsy wound bed by EdU incorporation assay (Supplementary Figure S5a). Colonic epithelial wounds were inflicted by biopsy forceps and tissues were collected at different days post biopsy injury. EdU was injected I.P. 2 hours prior to harvesting the wound beds to label proliferating cells at S-phase. As described before,24 4–5 crypts adjacent to wound bed showed increase in IEC proliferation (EdU positive; red) within two days of inflicting biopsy injury in wild type control mice (Supplementary Figure S5b, and Figure 6a). To investigate the role of FPR1 and NOX1 in commensal microbiota-induced IEC proliferation, wounds were treated intrarectally with HBSS or LGG for 2 days and proliferation was assessed by EdU incorporation and immunostaining with anti-Ki67 (Supplementary Figure S5c,d, and Figure 6a,c). Treatment of wounds with LGG significantly increased number of EdU positive cells (red) in the 4–5 colonic crypts adjacent to wounds in wild type mice. However, no significant increase in proliferation was detected in wound associated colonic crypts of Fpr1−/− and Nox1−/−IEC mice (Figure 6a,c). Similarly, though much weaker, FPR1 and NOX1 dependent LGG-stimulated proliferative response was detected in the unwounded mucosa (Figure 6b,d). Together, these data indicate that FPR1 and NOX1 are required for enteric commensal bacteria-stimulated activation of ERK and induction of proliferation of IECs, cellular processes important for mucosal wound healing and homeostasis.
Figure 6.
Commensal bacteria-stimulated enterocyte proliferation in crypts adjoining mucosal wounds requires FPR1 and NOX1. (a and b) Determination of enterocyte proliferation on day two. Mice were treated intrarectally with HBSS or LGG for 2 days. EdU was injected I.P. for a pulse of 2 hours before harvesting of colonic tissues. Thin serial sections of colonic tissues were stained for EdU in cells at S-phase. (a) Biopsy wounds. n=6 lesions per group. White lines show crypts adjacent to the wound. (b) Intact colonic mucosa. Scale bar, 50μm. Data are representative of three independent experiments with n=3 mice per group. (c and d) Quantification of EdU positive cells. (c) Edu positive cells in five crypts adjacent to the biopsy wounds were counted and expressed as Edu positive cells / crypt (d) Intact mucosa. Results are shown as means ± SD (n=6) and *P < 0.05 by Student’s t test.
DISCUSSION
Repair of mucosal injury, termed restitution, requires induced and coordinated proliferation and migration of intestinal epithelial cells. Based on our past demonstration of functional FPR on the apical surface of gut epithelia and our findings showing pro-restitutive effects of FPR ligand annexin A1, we sought to investigate the role of FPR in host-commensal interactions that promote mucosal wound healing. FPRs represent an important class of pattern recognition receptor that can bind an array of exogenous bacterial peptides as well as endogenous mediators including annexin A1, lipoxin A4 and resolving D1.13,14,31 Neutrophils and monocytes perceive bacterial products via the FPRs which elicit key innate immune processes in phagocytes, including onset of motility (chemotaxis), NOX2 catalyzed ROS generation and regulation of signaling pathways.7
While the role of FPRs in microbial perception and effector function in phagocytes goes back decades, only recently have they been detected in non-hematopoietic tissues including colonic and gastric epithelia, lung and nasal epithelia, as well as lens and retinal pigment epithelia,32,33 FPRs mediate migration of cultured intestinal epithelial cells and enhance wound gap closure in response to bacterial formyl peptides.11,12 FPR ligands also promote wound closure in lung epithelial cells32 and human retinal pigment epithelial cell.33 Recently, FPR2 null mice have been reported to be involved in repair of chemically induced mucosal injury.15 In addition, during the resolution phase of inflammation, there is a temporal increase in pro-resolving mediators including resolvin D1 and lipoxin A4, which stimulate resolution via FPR2 receptor.14 Our laboratory previously demonstrated that the commensal microbiota enhance migration of intestinal epithelial cells by modulating cell adhesion complexes,21 called focal adhesions (FAs) that stabilize migrating cells to the underlying matrix. One of the key regulatory proteins of FA complex is FAK, a cytoplasmic protein tyrosine kinase, which is under the regulation of ROS-sensitive phosphatases including PTPs, PTEN and SHP2.17,34,35 We specifically demonstrated that enteric microbiota-induced ROS generation inactivates redox sensitive tyrosine phosphatases towards FAK, and thereby upregulating its phosphorylation in vitro.21 By making endoscopic bioptic mucosal wounds in murine model, in this current report, we specifically show that commensal activate rapid phosphorylation of FAK and paxillin in a FPR1-dependent manner. Importantly, these events were also abolished in Fpr1−/−, Nox1−/−IEC and wild type mice pretreated with NAC, strongly implicating involvement of FPR1 dependent redox signaling. These present findings are consistent with our recent report that Annexin A1, an endogenous FPR ligand, induces NOX1-dependent ROS generation via FPR1 leading to the oxidative inactivation of regulatory phosphatases including PTP-PEST and PTEN resulting in upregulation of FAK phosphorylation and subsequent wound gap closure.13
A number of studies implicated FPRs in epithelial cell proliferation,36,37 a critical component of wound restitution. Intriguingly, Helicobacter pylori Hp (2–20) peptide, an exogenous ligand derived from gastric epithelial microbiota, can also promote proliferation of gastric epithelial cells by interacting with FPRs;8 however, the molecular mechanism of microbiota-induced epithelial proliferation during wound repair via FPRs remained poorly understood. Cellular ROS generated from NOX enzymes mediate intracellular signaling important in wound repair and homeostasis, including cell cycle regulation, proliferation and differentiation.18,26 Nox1 is abundantly transcribed in intestinal epithelial cells located both in the colonic crypts as well as luminal tips.27 Recently, Coant et al. showed that mice with a germline deletion in Nox1 demonstrated defective intestinal epithelial differentiation.38 In this current study, our findings specifically established that microbiota-induced ERK phosphorylation and subsequent IEC proliferation in wound associated enterocytes were dependent on ROS generation mediated by FPR1 and NOX1.
The mechanisms by which the host perceives prokaryotic contact and transduces this into physiological, rather than pathological, results are largely unknown. We identify a central role of FPR1 and NOX1 in mediating the commensal microbiota stimulated pro-proliferative and pro-migratory effects on enterocytes that facilitate mucosal repair and homeostasis (Figure 7). Identification of the optimal commensal species and/or microbial products as well as indigenous host molecules that modulate the physiological ROS generation through epithelial FPR1-NOX1 signaling pathways will be crucial for developing future therapeutic approaches for a range of mucosal disorders.
Figure 7.
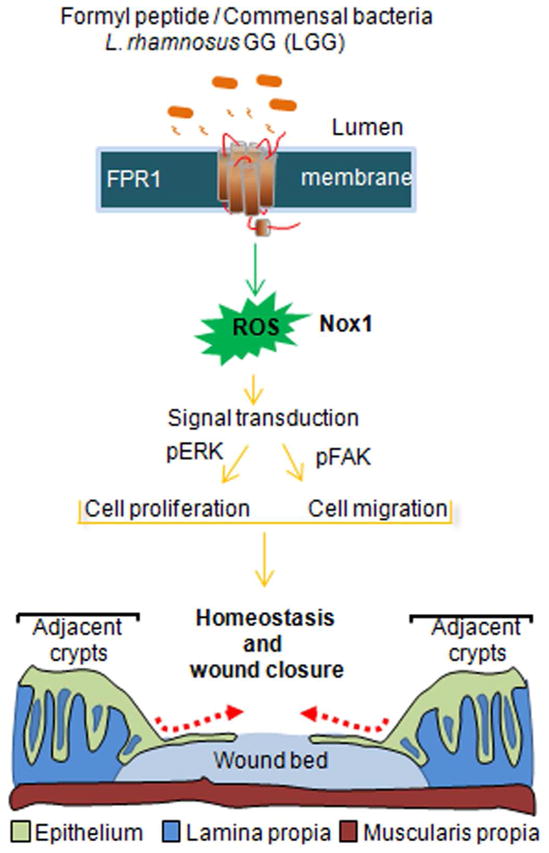
Model depicts the effects of commensal bacteria on restitution of colonic epithelial wounds. FPR1 receptors are expressed on the apical surface of colonic enterocytes. The FPR1 receptor perceives signals from commensal bacteria to elicit ROS via activation of NOX1. ROS mediates activation/phosphorylation of ERK and FAK with resultant effects on proliferation and also turnover of focal adhesions. Overall enhancement of cell proliferation and migration promotes wound closure and contributes to overall homeostasis.
MATERIALS AND METHODS
Mouse models
All animal experiments were approved by the Institutional Animal Care and Use Committee at Emory University and performed according to the National Institutes of Health guidelines. The mice had ad libitum access to a standard diet and water until reaching the desired age and/or weight. Animals were maintained on a 12-h light/12-h dark cycle under pathogen free conditions. Fpr1 −/− mouse were purchased from Taconic. Colonies of Fpr1−/−, Nox1−/−IEC, and MyD88−/− mice were established and maintained in our research facility. Nox1−/−IEC mice24 were described by Leoni et al. Nox2 null mice were purchased from the Jackson Laboratory. Genotyping was accomplished by PCR of the wild type mFpr1 allele or mutated gene carrying the neomycin resistance gene (neor).
Endoscope used in live mice
To create discrete mucosal injuries in the mouse colon and to monitor their regeneration, we used a high-resolution miniaturized colonoscope system (Coloview Veterinary Endoscope, Karl Stortz). This system consisted of a miniature rigid endoscope (1.9-mm outer diameter), a xenon light source, a triple chip high resolution CCD camera, and an operating sheath with instrument channels and an air / water injection bulb to regulate inflation of the mouse colon (all from Karl Storz). The endoscope with outer operating sheath was inserted into the mid-descending colon and the mucosa was surveyed to the ano-rectal junction. Then, the flexible biopsy forceps with a diameter of 3 French were inserted to remove single full thickness areas of the entire mucosa and submucosa. Endoscopic procedures were viewed with high resolution (1024 × 768 pixels) images on a flat panel color monitor. This enabled us to take both video and still images of the endoscopic procedures.24 The Image J software (National Institutes of Health, Bethesda, MD) was used to analyze the wound sizes. The night before the initial biopsy injury, food was removed from the mouse cages. The following morning, mice were anesthetized using ketamine and xylazine. We took particular care to avoid penetration of the muscularis propria.
Wound bed tissue preparation
Wound bed gross morphology was studied with a dissection microscope. Mucosal tissues with the wound bed were preserved in OCT media and frozen to perform immunofluorescence microscopy and histopathologic analysis. For histological analysis, wounds were oriented and cut in a proximal to distal manner and sections were prepared in 7-μm increments.24,39 The sections with the largest area of the wound bed (highlighted by dashed lines in Supplementary Figure S1a and with asterisk in Supplementary Figure S1b) were considered the center of the wound24, 39 and used for immunofluorescence staining.
Cell migration in vivo
To assess for epithelial migration to cover a wound bed, mice were injected I.P. with EdU (100 μg/g body weight) at the time of biopsy injury and were euthanized two - four days later (chase: 2–4 days). Immunohistochemical localization of EdU labeled cells were done by Click-iT® EdU Alexa Fluor® Imaging Kit. Nuclei were stained with the To-pro 3 (Molecular Probes). Sections were also immunostained for β-catenin to identify enterocytes.
To assess for epithelial migration in intact colonic tissue, mice were injected I.P. with EdU. Migration of enterocytes was measured by determining locations of the foremost EdU-labeled enterocytes colonic crypt and were recorded as the percent of epithelial cell positions along the crypt-luminal axis of well-oriented crypt units.
Cell proliferation in vivo
After inflicting biopsy injury in mice, EdU was administered I.P. at different time points (day 0, 1 and 2). Mice were euthanized 2 hours post EdU administration (pulse: 2 hr); tissue sections containing wound beds were collected in OCT medium and were frozen. S-phase cells were detected with procedure described above. Proliferating cells were also determined by immunofluorescence using anti-Ki67 antibody.
Immunoblotting and immunofluorescence
To collect epithelial cells, intrarectal administrations of HBSS (Hank’s buffer), LGG, or fMLF for the indicated times were performed in anesthetized mice. Mice were euthanized, colons were opened along the mesenteric border, epithelial tissues were scrapped and lysed in radioimmunoprecipitation assay (RIPA) buffer (100 mg tissue/ml of buffer) followed by centrifugation at 16000 r.p.m. for 20 min at 4°C. Antibodies were obtained as follows: anti ERK, phospho-ERK, (Cell Signaling), β-actin (Sigma-Aldrich), phospho-FAK (Sigma), phospho-paxillin (AbCam), fluorescein (FITC)-conjugated goat anti-rabbit IgG (Jackson ImmunoResearch), and HRP-conjugated donkey anti-rabbit or sheep anti-mouse secondary antibody (GE Healthcare). Immunoblot and immunofluorescent labeling slips were performed as previously described.13 Nuclei were stained with To-Pro-3 iodide (Molecular Probes). Fluorescent images acquired by laser confocal microscopy
ROS assay in vivo
For detection of ROS in the murine biopsy injury model, a nontoxic ROS sensitive dye hydrocyanine 3 was used.25 Mice were anesthetized, followed by intrarectal injection with nontoxic ROS sensitive dye hydrocyanine 3 that fluoresces when oxidized. After 30 min of Hydro-Cy3 injection, biopsy injuries were made, and administration of HBSS, LGG (2.5×109 cfu), or fMLF for different time points were performed. Mice were euthanized, the colons were opened along the mesenteric border, and tissues were collected. After mounting on slides, samples were examined by Confocal laser scanning microscopy. Images were captured using 535 nM laser extinction and 560 nM emission filter. ImageJ software (National Institutes of Health, Bethesda, MD) was used to analyze fluorescence intensity.
ROS assay in vitro
Cell Culture
Human intestinal epithelial cell line SK-CO15 was grown on membrane inserts in high glucose (4.5 g/liter) DMEM supplemented with 10% FBS, 100 units/ml penicillin, 100 μg/ml streptomycin, 15mM HEPES (pH 7.4), 2mML-glutamine, and 1% nonessential amino acids at 37 °C in a 4% CO2 incubator.
ROS Detection
Scratch wounds were performed with plastic micropipette tips on polarized SK-CO15 cells grown on membrane inserts. Epithelial cells were treated with L. rhamnosus GG (LGG; 5×107 cfu/ml) (ATCC 53103) or fMLF (500 nM) (Sigma-Aldrich) for the indicated times were washed with HBSS and incubated in the dark with CM-H2DCF-DA (Molecular Probes) for an additional 5 min as described previously by Wentworth et. al.30 All images were acquired using a confocal laser scanning microscope (Zeiss LSM 510) at ×40 magnification. Images were captured using 488 nM laser for excitation and a 515–540 nM emission filter. Quantification of fluorescence intensity was determined using ImageJ (National Institutes of Health, Bethesda, MD).
Induction of colitis
4% (wt/vol) Dextran sodium sulfate (DSS, molecular mass, 36–50 kDa) was dissolved in purified water and orally administered to mice as previously described13,21. Mice were allowed free access to food and water containing 4% DSS from day 0 until day 7 and DSS was withdrawn to allow recovery from colitis for additional 4 days. Mice were administered with intrarectal injections of LGG suspension in HBSS buffer for additional 3 days. Mice were sacrificed on day 14. Daily clinical assessment of DSS-treated animals included evaluation of stool consistency, detection of blood in stool, and body weight loss measurements. An individual score (ranging from 0 to 4) was attributed for each one of these parameters, and a disease activity index (DAI) ranging from 0 to 4 was calculated by combining all three scores.
Statistics
Quantitative data are expressed as mean ±S.E.M. or S.D. for each treatment group. Statistical comparisons were performed by 2-tailed Student’s t-test or ANOVA with Tukey’s multiple comparison post-test (GraphPad Prism; GraphPad Software). P values less than 0.05 were considered significant.
Supplementary Material
Acknowledgments
We thank Dr. Charles Parkos for critically reviewing the manuscript. Supported by grants RO1DK089763, RO1DK055679 to ASN; RO1AI64462 to A.N. and the Emory Digestive Diseases Research Development Center Core Grant (DK 064399). A.A. is supported by a Research Fellowship from Crohn’s and Colitis Foundation of America
Footnotes
Competing Financial Interests: The authors declare no competing financial interests.
References
- 1.Loftus EV., Jr Clinical epidemiology of inflammatory bowel disease: Incidence prevalence and environmental influences. Gastroenterology. 2004;126:1504–1517. doi: 10.1053/j.gastro.2004.01.063. [DOI] [PubMed] [Google Scholar]
- 2.Bewtra M, Su C, Lewis JD. Trends in hospitalization rates for inflammatory bowel disease in the United States. Clin Gastroenterol Hepatol. 2007;5:597–601. doi: 10.1016/j.cgh.2007.01.015. [DOI] [PubMed] [Google Scholar]
- 3.Pull SL, Doherty JM, Mills JC, Gordon JI, Stappenbeck TS. Activated macrophages are an adaptive element of the colonic epithelial progenitor niche necessary for regenerative responses to injury. Proceedings of the National Academy of Sciences. 2005;102:99–104. doi: 10.1073/pnas.0405979102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Neish AS. Microbes in gastrointestinal health and disease. Gastroenterology. 2009;136:65–80. doi: 10.1053/j.gastro.2008.10.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hooper LV, et al. Molecular analysis of commensal host-microbial relationships in the intestine. Science. 2001;291:881–884. doi: 10.1126/science.291.5505.881. [DOI] [PubMed] [Google Scholar]
- 6.Rakoff-Nahoum S, Paglino J, Eslami-Varzaneh F, Edberg S, Medzhitov R. Recognition of commensal microflora by toll-like receptors is required for intestinal homeostasis. Cell. 2004;118:229–241. doi: 10.1016/j.cell.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 7.Ye RD, et al. International Union of Basic and Clinical Pharmacology. LXXIII. Nomenclature for the formyl peptide receptor (FPR) family. Pharmacol Rev. 2009;61:119–161. doi: 10.1124/pr.109.001578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Paulis A, et al. Helicobacter pylori Hp(2–20) promotes migration and proliferation of gastric epithelial cells by interacting with formyl peptide receptors in vitro and accelerates gastric mucosal healing in vivo. J Immunol. 2009;183:3761–3769. doi: 10.4049/jimmunol.0900863. [DOI] [PubMed] [Google Scholar]
- 9.Southgate EL, et al. Identification of formyl peptides from Listeria monocytogenes and Staphylococcus aureus as potent chemoattractants for mouse neutrophils. J Immunol. 2008;181:1429–1437. doi: 10.4049/jimmunol.181.2.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bylund J, Samuelsson M, Collins LV, Karlsson A. NADPH-oxidase activation in murine neutrophils via formyl peptide receptors. Exp Cell Res. 2003;282:70–77. doi: 10.1016/s0014-4827(02)00010-1. [DOI] [PubMed] [Google Scholar]
- 11.Babbin BA, et al. Annexin I regulates SKCO-15 cell invasion by signaling through formyl peptide receptors. J Biol Chem. 2006;281:19588–19599. doi: 10.1074/jbc.M513025200. [DOI] [PubMed] [Google Scholar]
- 12.Babbin BA, et al. Formyl peptide receptor-1 activation enhances intestinal epithelial cell restitution through phosphatidylinositol 3-kinase-dependent activation of Rac1 and Cdc42. J Immunol. 2007;179:8112–8121. doi: 10.4049/jimmunol.179.12.8112. [DOI] [PubMed] [Google Scholar]
- 13.Leoni G, et al. Annexin A1, formyl peptide receptor, and NOX1 orchestrate epithelial repair. J Clin Invest. 2013;123:443–454. doi: 10.1172/JCI65831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Norling LV, Dalli J, Flower RJ, Serhan CN, Perretti M. Resolvin D1 limits polymorphonuclear leukocyte recruitment to inflammatory loci: receptor-dependent actions. Arterioscler Thromb Vasc Biol. 2012;32:1970–1978. doi: 10.1161/ATVBAHA.112.249508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen K, et al. Formylpeptide receptor-2 contributes to colonic epithelial homeostasis, inflammation, and tumorigenesis. J Clin Invest. 2013;123:1694–704. doi: 10.1172/JCI65569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tsukagoshi H, Busch W, Benfey PN. Transcriptional regulation of ROS controls transition from proliferation to differentiation in the root. Cell. 2010;143:606–616. doi: 10.1016/j.cell.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 17.Chiarugi P, et al. Reactive oxygen species as essential mediators of cell adhesion: the oxidative inhibition of a FAK tyrosine phosphatase is required for cell adhesion. J Cell Biol. 2003;161:933–944. doi: 10.1083/jcb.200211118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Love NR, et al. Amputation-induced reactive oxygen species are required for successful Xenopus tadpole tail regeneration. Nat Cell Biol. 2012;15:222–228. doi: 10.1038/ncb2659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wentworth CC, Jones RM, Kwon YM, Nusrat A, Neish AS. Commensal-epithelial signaling mediated via formyl peptide receptors. Am J Pathol. 2010;177:2782–2790. doi: 10.2353/ajpath.2010.100529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kumar A, et al. Commensal bacteria modulate cullin-dependent signaling via generation of reactive oxygen species. Embo J. 2007;26:4457–4466. doi: 10.1038/sj.emboj.7601867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Swanson PA, 2nd, et al. Enteric commensal bacteria potentiate epithelial restitution via reactive oxygen species-mediated inactivation of focal adhesion kinase phosphatases. Proc Natl Acad Sci U S A. 2011;108:8803–8808. doi: 10.1073/pnas.1010042108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sieg DJ, Hauck CR, Schlaepfer DD. Required role of focal adhesion kinase (FAK) for integrin-stimulated cell migration. J Cell Sci. 1999;112 ( Pt 16):2677–2691. doi: 10.1242/jcs.112.16.2677. [DOI] [PubMed] [Google Scholar]
- 23.Owen KA, Abshire MY, Tilghman RW, Casanova JE, Bouton AH. FAK regulates intestinal epithelial cell survival and proliferation during mucosal wound healing. PLoS One. 2011;6:e23123. doi: 10.1371/journal.pone.0023123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seno H, et al. Efficient colonic mucosal wound repair requires Trem2 signaling. Proc Natl Acad Sci U S A. 2009;106:256–261. doi: 10.1073/pnas.0803343106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kundu K, et al. Hydrocyanines: a class of fluorescent sensors that can image reactive oxygen species in cell culture, tissue, and in vivo. Angew Chem Int Ed Engl. 2009;48:299–303. doi: 10.1002/anie.200804851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aguirre J, Lambeth JD. Nox enzymes from fungus to fly to fish and what they tell us about Nox function in mammals. Free Radic Biol Med. 2010;49:1342–1353. doi: 10.1016/j.freeradbiomed.2010.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Laurent E, et al. Nox1 is over-expressed in human colon cancers and correlates with activating mutations in K-Ras. Int J Cancer. 2008;123:100–107. doi: 10.1002/ijc.23423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hurd TR, DeGennaro M, Lehmann R. Redox regulation of cell migration and adhesion. Trends Cell Biol. 2012;22:107–115. doi: 10.1016/j.tcb.2011.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Miyoshi H, Ajima R, Luo CT, Yamaguchi TP, Stappenbeck TS. Wnt5a potentiates TGF-beta signaling to promote colonic crypt regeneration after tissue injury. Science. 2012;338:108–113. doi: 10.1126/science.1223821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wentworth CC, Alam A, Jones RM, Nusrat A, Neish AS. Enteric commensal bacteria induce extracellular signal-regulated kinase pathway signaling via formyl peptide receptor-dependent redox modulation of dual specific phosphatase 3. J Biol Chem. 2011;286:38448–38455. doi: 10.1074/jbc.M111.268938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gronert K, et al. A role for the mouse 12/15-lipoxygenase pathway in promoting epithelial wound healing and host defense. J Biol Chem. 2005;280:15267–15278. doi: 10.1074/jbc.M410638200. [DOI] [PubMed] [Google Scholar]
- 32.Shao G, et al. Formyl peptide receptor ligands promote wound closure in lung epithelial cells. Am J Respir Cell Mol Biol. 2011;44:264–269. doi: 10.1165/rcmb.2010-0246RC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang XG, et al. Activation of formyl peptide receptor-1 enhances restitution of human retinal pigment epithelial cell monolayer under electric fields. Invest Ophthalmol Vis Sci. 2011;52:3160–3165. doi: 10.1167/iovs.10-5156. [DOI] [PubMed] [Google Scholar]
- 34.Mitra SK, Hanson DA, Schlaepfer DD. Focal adhesion kinase: in command and control of cell motility. Nat Rev Mol Cell Biol. 2005;6:56–68. doi: 10.1038/nrm1549. [DOI] [PubMed] [Google Scholar]
- 35.Shao D, et al. Redox modification of cell signaling in the cardiovascular system. J Mol Cell Cardiol. 2012;52:550–558. doi: 10.1016/j.yjmcc.2011.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khau T, et al. Annexin-1 signals mitogen-stimulated breast tumor cell proliferation by activation of the formyl peptide receptors (FPRs) 1 and 2. FASEB J. 2011;25:483–496. doi: 10.1096/fj.09-154096. [DOI] [PubMed] [Google Scholar]
- 37.Lee SY, et al. F2L, a peptide derived from heme-binding protein, inhibits LL-37-induced cell proliferation and tube formation in human umbilical vein endothelial cells. FEBS Lett. 2008;582:273–278. doi: 10.1016/j.febslet.2007.12.015. [DOI] [PubMed] [Google Scholar]
- 38.Coant N, et al. NADPH oxidase 1 modulates WNT and NOTCH1 signaling to control the fate of proliferative progenitor cells in the colon. Mol Cell Biol. 2010;30:2636–2650. doi: 10.1128/MCB.01194-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Manieri NA, Drylewicz MR, Miyoshi H, Stappenbeck TS. Igf2bp1 is required for full induction of Ptgs2 mRNA in colonic mesenchymal stem cells in mice. Gastroenterology. 2012;143:110–121. e110. doi: 10.1053/j.gastro.2012.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.