Abstract
Purpose
To evaluate the association between outdoor and nearwork activities at baseline and myopia stabilisation by age 15 in the Correction of Myopia Evaluation Trial (COMET).
Methods
COMET enrolled 469 children (ages: six to 11 years) with spherical equivalent myopia between −1.25 and −4.50D, who were randomised to progressive addition or single vision lenses and followed for five years in their original lenses. At baseline, families recorded the child's outdoor and nearwork activities for three days within a week. Weekly hours spent in nearwork and outdoor activities were calculated for each participant. Refractions collected over 11 years were fit using the Gompertz function to determine each participant's myopia stabilisation age. Myopia for each child was then categorized as stable/not stable by age 15.
Results
Half (233/469) of participants had usable baseline activity diaries and refraction data that could be fit with the Gompertz function, 59.7% (139/233) had stable myopia by age 15 and 40.3% had myopia that was not yet stable. The frequency of stable myopia was similar for the two categories (median split) of outdoor activities: 60% (71/118) for ≤9.0 hours/week and 59% (68/115) for >9.0 hours/week. 56% (64/114) of children reporting >21.0 hours of baseline weekly nearwork activity had stable myopia by age 15 compared to 63% (75/119) with ≤21.0 hours of near work (adjusted OR= 0.74; 95% CI: 0.43-1.29). Using baseline nearwork as a continuous variable, the multivariable odds ratio for the association between baseline nearwork hours and stabilisation by age 15 is 0.98: 95% CI: 0.96-1.00, a result trending towards significance.
Conclusion
While time spent in outdoor activities in childhood does not appear to be related to myopia stabilisation by age 15, less near work activity might potentially be associated with myopia stabilisation by that age.
Keywords: myopia, nearwork, outdoor activity, visual activity
Introduction
In recent years there has been a resurgence of interest in investigating treatments for controlling the progression of myopia, as well as identifying risk factors related to myopia and its progression. This renewed interest is likely related to the significant increase in the prevalence of myopia, particularly in Asian populations 1-4, the increase in the prevalence of high myopia 1, 2, and the association between high myopia and chorioretinal disease.5
Most investigators agree that moderate levels of juvenile myopia are due to a combination of genetic and environmental factors.6-8 Results of recent genetic studies of refractive error with very large sample sizes7, 8 suggest that multiple genetic factors are involved in the development of myopia. The Consortium for Refractive Error and Myopia (CREAM)8, which conducted genome-wide meta-analyses based on 37,382 individuals from 27 studies of European ancestry and 8,376 persons from 5 Asian populations, found a tenfold increased risk of myopia for individuals carrying the highest genetic load. Genetics, however, play only a partial role in the development of myopia. With the increasing prevalence of myopia, other investigators have been exploring a wide range of potential environmental risk factors for developing myopia such as the amount of near work 9-12, reading habits (reading distance, frequency of breaks)13, 14, and more recently outdoor activity.12, 15-21 An interesting development in recent years has been reports of the protective role of outdoor activity in myopia development as reported in questionnaires.10, 12, 15, 16, 19-26
Sherwin, et al.25 recently completed a systematic review and meta-analysis, pooling results from seven cross-sectional studies10, 12, 14, 16, 18, 23, 27 to summarise the relevant evidence investigating the association between time spent outdoors and myopia in children and adolescents. The pooled odds ratio indicated a 2% reduced odds of having myopia per additional hour of time spent outdoors per week after adjustment for covariates. They concluded that increasing time spent outdoors might be a simple strategy to reduce the risk of development of myopia in children and adolescents. However, in a recent review of the literature, French, et al.,19 included a number of studies that were not included in the meta-analysis by Sherwin et al These studies reported a more significant effect of time spent outdoors in protecting against myopia. The authors concluded that the effect of time outdoors is robust and seems to reduce or even negate the influence of factors that may be associated with higher prevalence of myopia, such as significant near work, or having myopic parents.19 They also indicated that it is not clear from the limited current literature whether time outdoors also regulates progression in children with established myopia.
Although the majority of studies have reported a potential protective effect of outdoor activities for the development of myopia, two studies did not find such a relationship.12, 14 The first study, the Xichang Pediatric Refractive Error Study (X-Pres)14, included 1892 teenage participants (mean age 14.7 years). The authors found no evidence of greater time spent on outdoor or near activities in children with myopia vs. children without myopia in this cohort. In the only study to investigate visual activities in pre-school children, Low et al12 found that a family history of myopia was the strongest factor associated with pre-school myopia. Neither nearwork nor outdoor activities was found to be associated with early myopia.
A second more recent study reported on the relationship between visual activity and myopia progression28. Activity data were collected by parental survey from 835 myopes in the Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE). The authors found that the number of hours of outdoor/sports activity was not associated with myopia progression following onset.
Another frequently mentioned risk factor for myopia development and progression is near visual activity 29, 30. Studies of near work in which questionnaires were used have provided only weak evidence to support this hypothesis 9, 10. Ip et al suggested that the important factors are reading distance and the amount of continuous reading without a break, rather than the total amount of time spent reading 23. They found that although myopia was not significantly associated with time spent in nearwork after adjustment for other factors, there were significant independent associations with close reading distance and continuous reading. In a study by Williams et al the strongest predictor of myopia developing between the ages of seven and 10 years was a parental report that the child liked reading 31. The recent report by Jones-Jordan et al 28 found that the number of hours of reading for pleasure per week was not significantly associated with annual progression, similar to their finding of no association between outdoor activity and progression.
In summary, the current literature primarily provides data about the association between visual activities and the development of myopia and only preliminary information about myopia progression.19 To our knowledge, there have been no reports about the association between visual activities and myopia stabilisation. In the current study, we report new data about the relationship between visual activities and myopia stabilisation in participants originally enrolled as six to <12-year-old children in the Correction of Myopia Evaluation Trial (COMET).
Methods
Study Population
The tenets of the Declaration of Helsinki were followed throughout the study. The institutional review boards of all participating centres (Optometry Schools and Colleges in Birmingham, AL, Boston, MA, Houston, TX, and Philadelphia, PA) approved the protocol and informed consent forms. Informed consent from the parents was obtained after verbal and written explanation of the study, and assent was obtained from the children.
COMET enrolled 469 ethnically diverse children (6–11 years) with spherical equivalent (SER) myopia between −1.25 and −4.50 D. They were randomised to either progressive addition lenses (PALs) or single vision lenses (SVLs), and followed for five years in their original lens assignment and six additional years wearing either spectacles (PALs or SVLs) or contact lenses. Visual activity diaries were distributed to the families of the 469 COMET children at the start of the study. Study enrolment took place throughout the year, so administration of the diaries could take place any time of the year. The families were asked to record the child's activities for three days (two weekdays and one weekend day), and to specify the type of day (i.e. regular school day or vacation day). Recognizing that visual activities were likely to differ on weekdays and weekend days, in order to obtain a good representation of the number of hours spent per week on visual activities during the school year parents and children were asked to complete the diaries for two weekdays and one weekend day.
Description of Visual Activity Diaries
The visual activity diary was a one-page form that was filled out by either the parent(s) or the child, or the child with the help of a parent when necessary. Parents were instructed to observe the child as well as encourage a detailed hourly recall of events from the child for each day selected. The one-page diary requested tracking of different visual activity categories throughout each day including five near activity categories (reading, writing, desktop computer work/games, hand-held computer games, and other nearwork activities such as board games, colouring, arts and crafts), and one category for outdoor activity. The five nearwork categories were combined into one for the main analyses. In addition, only the near and outdoor activity that occurred before or after school hours were considered for analysis. This approach is consistent with previous studies.10, 18
Participants with useable baseline diaries (defined as having at least one complete weekday and one weekend day) and Gompertz curves that could be fit to their refraction data 32, 33were selected for these analyses. We assessed stabilisation at age 15 based on previous reports 32, 34 that about 90% of myopia progression stops by this age. For these analyses, visual activities were divided into two categories: nearwork and outdoor activities. Hours for each category were based on time spent outside of school hours, i.e. if the form indicated that the child was in school on the day the form was completed, hours from the beginning to the end of the school day were not considered. The number of visual activity hours was summed for each category to determine the total daily number of hours spent for each weekday, weekend day and vacation day. Vacation days were considered equivalent to weekend days. The total daily number of hours was then averaged for similar day types to generate separate averages/day for weekday and weekend days. For estimates of hours per week for each activity, the average weekday hours were multiplied by five, the weekend day hours were multiplied by two, and the two were added together. If more than one category was checked for a specific hour, the time spent in each activity was divided either in half or thirds, as indicated by the number of categories checked.
Myopia Stabilisation
The Gompertz function, a double exponential growth function, was fit to the non-cycloplegic SER measurements for the right eye of each participant who had at least six years and up to 11 years of data. 32 Non-cycloplegic refractions were used as the outcome variable for these analyses because they were measured at six-month intervals for the first four years and annually thereafter, while cycloplegic refraction was only measured annually throughout the study. The use of non-cycloplegic refraction data allowed us to maximize the number of data points available for curve fitting. Comparison of non-cycloplegic and cycloplegic measures in the COMET study showed a mean (SD) difference of 0.19 D (0.22) at baseline and 0.23 D (0.27) on average throughout the 11-year follow-up period, with non-cycloplegic measures more myopic than cycloplegic.
The Gompertz function was used because it was shown to provide good fits to longitudinal refraction data and parameters with biological relevance. 32,30 For each participant, using yij to represent the SER of the right eye at a given age for each individual, the Gompertz function for refractive error was specified as: where for each ith participant: Rei = SER prior to the onset of myopia; Rci = the change in SER from Rei to the final asymptotic myopia level; 0.07295 is a constant, based on an a priori definition of myopia progression onset and the nature of the double exponential function, i.e. peak acceleration into myopia which happens when 7.295% of the myopisation change is achieved; ai = the shape parameter with larger ai (0 < ai < 1) values representing slower myopia progression from the emmetropic phase; t0i = the myopia progression onset age at which there is peak acceleration in myopia; and, εij = residual error at age j. Age of onset was imputed for each curve. Age of myopia stabilisation was defined as the age when myopia reached 0.50D of the asymptote (Rei + Rci) (definition of myopia stabilisation), which was calculated from the parameters of the Gompertz curve as: Agestablei =ln[ln(0.5/Rci + 1)/ln 0.07295]/ln at+t0i. Stabilisation status was classified as either stable or not stable, i.e. that estimated myopia has not yet reached the curve asymptote +0.50D by age 15 (defined as: 15.00 – 15.99 years). Curves were included for analyses unless non-convergence (based on convergence threshold of c=10-5) or a poor model fit (defined as a mean squared residual > 0.40) were observed.
Statistical Methods
All analyses were conducted using SAS Software, Version 9.3 (SAS Inc.,Cary, NC). Baseline near work and outdoor activity hours were evaluated both as categorical variables, based on a median split, and as continuous variables. Univariate analyses were performed using χ2 tests for categorical variables and t tests for continuous variables. Associations between stabilisation status and visual activities were assessed using odds ratios and 95% confidence intervals. Unadjusted and adjusted results were calculated using logistic regression models, using fewer hours as the reference group for the categorical and the continuous factor analyses. Factors were selected for inclusion as covariates in the multivariable models if they reached a p value of p< 0.05 using stepwise logistic regression with forward selection. Factors considered for inclusion were baseline age (age six to nine vs age 10 to11), ethnicity (African-American, Asian, Hispanic, Mixed and White), gender, treatment group, baseline lag of accommodation, and baseline myopia. Number of myopic parents was also evaluated for possible inclusion in a reduced model (n=121), for the participants with parental myopia data.
Results
Of the 469 COMET participants, 50% (233/469) had useable diaries and valid Gompertz curve fits, and were included in the analyses for this report (Figure 1).
Figure 1.
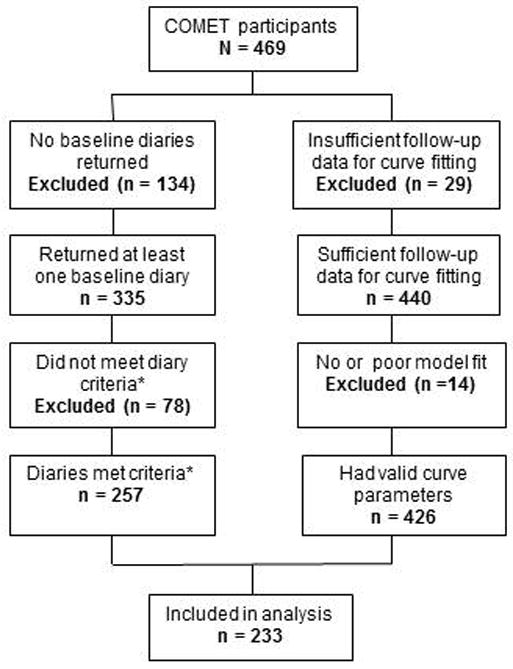
Twenty percent of the diaries were completed by the child only, 53% by the parent/guardian only and 27% by a combination of child and parent/guardian. There were no significant differences in baseline characteristics or stabilisation status between those children included and excluded in these analyses (Table 1). Of the 233 participants included in these analyses at baseline, 139 (59.7%) were classified as having stable myopia by age 15 and 94 (40.3%) were classified as without.
Table 1. Baseline Characteristics.
| Baseline Factors | Eligible1 N=233 | Non-Eligible N=236 | p-value2 | ||
|---|---|---|---|---|---|
|
| |||||
| n | % | n | % | ||
| Age | |||||
| Mean ± SD | 9.34 ± 1.30 | 9.32 ± 1.28 | 0.89 | ||
|
| |||||
| Gender | 0.88 | ||||
| Male | 110 | 47.2 | 113 | 47.9 | |
| Female | 123 | 52.8 | 123 | 52.1 | |
|
| |||||
| Ethnicity | 0.66 | ||||
| African-American | 56 | 24.0 | 67 | 28.4 | |
| Asian | 18 | 7.7 | 18 | 7.6 | |
| Hispanic | 31 | 13.3 | 37 | 15.7 | |
| Mixed | 12 | 5.2 | 12 | 5.1 | |
| White | 116 | 49.8 | 102 | 43.2 | |
|
| |||||
| Myopia3 | |||||
| Mean ± SD | -2.40 ± 0.80 | -2.37 ± 0.80 | 0.7 | ||
|
| |||||
| Center | 0.07 | ||||
| UAB | 63 | 27.0 | 70 | 29.7 | |
| NECO | 46 | 19.7 | 64 | 27.1 | |
| UH | 60 | 25.8 | 58 | 24.6 | |
| PCO | 64 | 27.5 | 44 | 18.6 | |
|
| |||||
| Stabilization Status4 | 0.67 | ||||
| Stable | 139 | 59.7 | 119 | 61.7 | |
| Not Stable | 94 | 40.3 | 74 | 38.3 | |
Eligible: COMET participants with useable (defined as having at least one weekday and one weekend day completed) near work diaries at baseline and an 11-yr Gompertz curve are eligible for the analysis.
based on chi-square tests for categorical variables and t-tests for continuous variables.
Average cycloplegic spherical equivalent refractive error of both eyes.
Stabilization status by age 15 (age 15 includes 15.0-15.99, i.e. <16). Results in the Non-eligible group are based on 193 participants with valid Gompertz curve fits and without useable diaries
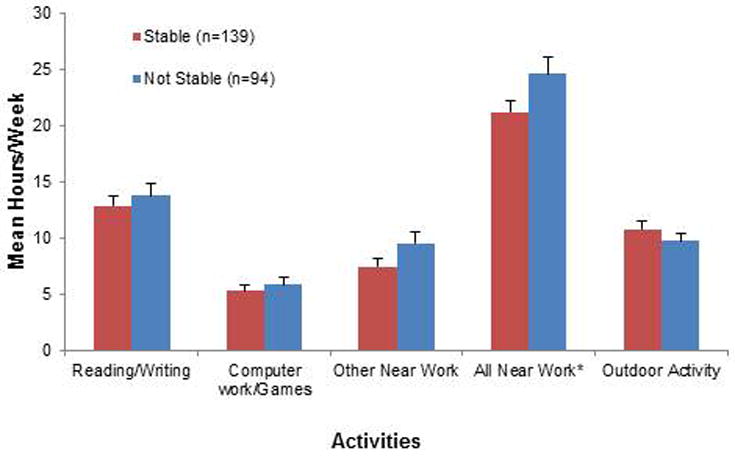
Figure 2 shows the baseline mean hours per week spent on each visual activity by stabilisation status by age 15. The number of weekly hours was not statistically significantly different between the stable and the not stable groups for any visual activity category based on two-sample t-test (all p-values > 0.05). When combining all the nearwork categories of reading/writing, computer/games work and other nearwork, the total number of weekly hours was larger in the not stable group (mean±SD; stable group, 21.2±11.6 hours/week; not stable group, 24.6±14.9 hours/week (p=0.06, t-test).
Figure 2.
Outdoor activity
The relationship between baseline hours/week spent in outdoor activities and stabilisation status by age 15 was analysed considering outdoor activity hours as a categorical variable based on a median split (9.0 hours) of the baseline distribution and as a continuous variable. The proportion of participants with stable myopia by age 15 was similar for the two outdoor activities categories [60.2% (71/118) for <9.0 hours/week and 59.1% (68/115) for >9.0 hours/week]. No association between baseline outdoor activities and stabilisation by age 15 was observed, when evaluated in a multivariable logistic regression model using ≤9 hours/week as the reference group, that included baseline age (age 6 to 9 vs age 10 to11) and ethnicity as covariates chosen by the stepwise logistic regression selection process (adjusted OR=0.93; 95% CI, 0.53-1.65). Results were similar in a separate multivariable analysis including outdoor activity hours as a continuous variable (Adjusted OR=1.02; 95% CI, 0.99-1.06) (Table 2).
Table 2. Stabilization Status by Age 151 Year by Baseline Outdoor Activity2,3.
| Baseline Outdoor Activity (hours/week) | Stabilization Status by Age 15* Years | Univariate† | Multivariable‡ | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Stable | Not Stable | Total | OR (95% CI) | p-value | OR (95% CI) | p-value | ||||
| n | (%) | n | (%) | N | (%) | |||||
| ≤ 9.0* | 71 | (60.2) | 47 | (39.8) | 118 | (100.0) | Reference | - | Reference | - |
| > 9.0 | 68 | (59.1) | 47 | (40.9) | 115 | (100.0) | 0.96 (0.57, 1.62) | 0.87 | 0.93 (0.53, 1.65) | 0.81 |
| Total | 139 | (59.7) | 94 | (40.3) | 233 | (100.0) | - | - | - | - |
| Mean hours/wk ± SD | 10.8 ± 9.3 | 9.8 ± 7.0 | 10.4 ± 8.5 | 1.02 (0.98, 1.05) | 0.36 | 1.02 (0.99, 1.06) | 0.27 | |||
Age 15 years includes 15.0-15.99, i.e. <16.
Outdoor activity is based on time spent in outside activities outside of school hours.
This table is based on all participants with useable (defined as having at least one weekday and one weekend day completed) near work diaries at baseline and an 11-yr Gompertz curve.
Based on a median split of the distribution.
Based on univariate logistic models, with stabilization status by age 15 years as the dependent variable, and baseline near work (median split or as continuous variable separately) as the independent variable.
Based on multivariable logistic models that included covariates of baseline age (6-9 yrs old vs. 10-11 yrs old) and ethnicity chosen by a stepwise logistic regression model with forward selection using p<0.05 as the criterion for selection. Other variables screened for possibe
Nearwork
The association between baseline nearwork activity and myopia stabilisation status by age 15 was evaluated using nearwork activity as both a categorical variable, based on a median split (21.0 hours) of the baseline distributions and as a continuous variable (Table 3). Based on the median split of baseline weekly near work hours, 63.0% (75/119) of children reporting ≤21.0 hours of near work activity reached our definition of myopia stabilisation by age 15 compared to 56.1% (64/114) of children reporting >21.0 hours of near work. Although participants who spent more time on nearwork activities at baseline had a lower odds of having stable myopia by age 15 than those who spent less time, the results are not statistically significant based on a multivariable logistic regression model using ≤21 hours/week as the reference group and adjusting for those variables meeting the selection criteria for inclusion (p<0.05), i.e., baseline age and ethnicity (OR= 0.74; 95% CI, 0.43-1.29; p=0.29) (Table 3).
Table 3. Stabilization Status by Age 151 Years by Baseline Near Work2,3.
| Baseline Near Work2 (hours/week) | Stabilization Status by Age 151 Years | Univariate† | Multivariable ‡ | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Stable | Not Stable | Total | OR (95% CI) | p-value | OR (95% CI) | p-value | ||||
| n | (%) | n | (%) | n | (%) | |||||
| ≤ 21.0* | 75 | (63.0) | 44 | (37.0) | 119 | (100.0) | Reference | - | Reference | - |
| > 21.0 | 64 | (56.1) | 50 | (43.9) | 114 | (100.0) | 0.75 (0.44, 1.27) | 0.28 | 0.74 (0.43, 1.29) | 0.29 |
| Total | 139 | (59.7) | 94 | (40.3) | 233 | (100.0) | - | - | - | - |
| Mean hours/wk ± SD | 21.2 ± 11.6 | 24.6 ± 14.9 | 22.6 ± 13.1 | 0.98 (0.96, 1.00) | 0.05 | 0.98 (0.96, 1.00) | 0.07 | |||
Age 15 years includes 15.0-15.99, i.e. <16.
Near work is defined as performing reading, writing, desktop computer work/games, handheld computer games or other near work activities outside of school hours
This table is based on all participants with useable (defined as having at least one weekday and one weekend day completed) near work diaries at baseline and an 11-yr Gompertz curve.
Based on a median split of the distribution.
Based on univariate logistic models, with stabilization status by age 15 years as the dependent variable, and baseline near work (median split or as continuous variable separately) as the independent variable.
Based on multivariable logistic models. Model included covariates of baseline age (6-9 yrs old vs. 10-11 yrs old) and ethnicity chosen by a stepwise logistic regression model with forward selection using p<0.05 as the criterion for selection. Other variables screened for possible inclusion in the model were gender, treatment group, baseline lag of accommodation and baseline myopia. Number of myopic parents was also considered for inclusion in a reduced model (n=121).
Results of a multivariable logistic regression model that defined weekly nearwork hours as a continuous independent variable and also included baseline age and ethnicity as covariates, showed that for each additional hour per week spent on near work activities per week at baseline, the odds of having stable myopia by age 15 decreases by 2% (adjusted OR= 0.98: 95% CI: 0.96-1.00, p=0.07)(Table 3).
Exploratory analysis
An exploratory analysis was conducted in the subset of COMET participants who completed diaries at both the baseline and three-year visits and also remained in the same visual activities category based on median split category at both visits. This analysis was designed to provide a more stable estimate of visual activity hours (i.e. same level of visual activity reported at two visits) and to evaluate the consistency of the baseline findings with visual activity when the visual activity was sustained at the same level for at least three years. Of the 123 participants who had usable visual activity diaries at baseline and three years, 61% (75/123) of participants remained in the same outdoor weekly hours category and 58% (72/123) remained in the same nearwork category. Results remained similar to those based on the full cohort, for both outdoor and nearwork activities, analysed as continuous variables. While no association was found between outdoor activities and stabilisation status by age 15, (adjusted OR: (95% CI) OR=1.06: (0.99, 1.13); p=0.12), the results revealed a significant association between more baseline near work hours, when analysed as a continuous variable, and not having stable myopia by age 15 (adjusted OR (95% CI) OR=0. 96: (0.92, 0.99); p=0.04).
Discussion
While most studies have assessed associations between nearwork or outdoor activities and myopia onset or progression, COMET is the first study to our knowledge to investigate a possible association between visual activities and myopia stabilisation. In this study, we found no relationship with baseline outdoor visual activities and myopia stabilisation by age 15. These data are consistent with a recent publication by Jones-Jordan et al 28 which found no significant association between either outdoor/sports activity or reading with annual myopia progression. We did, however, find a suggestive relationship between baseline nearwork hours and myopia stabilisation by age 15 in children originally enrolled in COMET as six to 11 year-old children. Previous studies have only found a weak relationship between nearwork activity and myopia development and progression 29, 30. However, a study by Williams et al demonstrated that the strongest predictor of myopia developing between the ages of seven7 and 10 years was a parental report that the child liked reading31. Therefore, data from our study provides preliminary information about the relationship between nearwork and myopia stabilisation.
Given the suggested protective effect of outdoor activity on myopia development, it is reasonable to hypothesise that outdoor activity might also slow the progression of myopia and perhaps lead to earlier stabilisation. If that were the case, prescribing/encouraging extensive outdoor activity for myopic children could be a potential future treatment option.19, 35 However, our data do not support this hypothesis.
Our study has some limitations that may have affected our results. First, in this study we used data collected at baseline, when the cohort was on average nine years old to look for a relationship between visual activity and stabilisation of myopia by age 15. The age of the children at baseline ranged from 6 to 11 years, and it is likely that the visual activities reported at age six years may be different from the visual activities that would have been reported at age 11. To this point, Deng et al18 explored the pattern of age dependence of various activities and found an increase in amount of time spent studying with increasing age, but no increase in time outdoors. Recent data from the Sydney Adolescent Vascular and Eye Study20, indicate that irrespective of gender or ethnicity, as children in their cohort became older they spent less time outdoors and more time doing nearwork. To address this potential limitation of different activity hours at different ages in COMET, we conducted exploratory analyses designed to evaluate the consistency of the baseline findings with visual activity when the visual activity was sustained at the same level for at least three years. These results showed that 61% of participants remained in the same outdoor weekly hours category and 58% remained in the same nearwork category. Thus, the association between myopia stabilisation and visual activities was similar whether we used data from the full cohort at baseline or the three-year data. This provides some support for the use of the baseline data to estimate later visual activity levels and their relationship with myopia stabilisation. In addition, most previous studies use activity data collected at one time to assess some aspect of myopia at a later time. Nevertheless, future studies should consider visual activity levels at different ages, to better understand the effect of visual activity on myopia progression and stabilisation during childhood and adolescence.
A second potential limitation is the low percentage of 50.3% (233/469) of participants with useable diaries and valid Gompertz curves and whether this low completion rate may have influenced the results. The fact that the participants included in these analyses were similar to non-eligible participants regarding age, gender, ethnicity, amount of myopia, clinical centre, and stabilisation status by age 15 lessens the likelihood that the low completion rate influenced the results. Another possible limitation is to be considered is limited sample size and reduced power. However, the multivariate odds ratio for the association between baseline nearwork hours and stabilisation by age 15 is 0.98, and the upper bound of the 95% confidence interval is 1.0, a result trending towards significance. This association is also supported by the results of the exploratory analyses, which are statistically significant. Since the power to detect a statistically significant odds ratio of 0.98 for the association between baseline nearwork hours and stabilisation by 15 of age is limited (0.45), a larger sample size is needed to confirm this observation.
The strengths of the COMET study are its ethnically diverse group of children from four different geographic locations with standardised measurements of refractive error, and its outstanding retention suggesting generalisability of the results to other groups of children with juvenile onset myopia in the United States. Because we had very few children of East Asian ethnicity, it may be difficult to generalise our findings to this population. French et al20 recently reported that patterns of visual activity vary significantly between ethnic groups. They found that children of East Asian ethnicity spend significantly less time outdoors and significantly more time on nearwork than European Caucasian children. Another strength of the COMET data is that it represents the longest longitudinal study of myopic children and the first that has included an analysis of factors related to stabilisation of myopia.
Future studies should expand on these results. First, longitudinal cohort studies with an appropriate sample size could be specifically designed to investigate relationships between a range of visual activities and myopia development, progression and stabilisation and include more frequent administration of visual activity questionnaires. In addition, an effort should be made to refine instruments to more accurately measure the level and specific characteristics of visual activity. It also would be useful to evaluate these associations in different populations.
In summary, there is significant evidence from previous studies25 that there is an association between time spent outdoors and myopia development in children and adolescents. When discussing strategies to slow the progression of myopia, clinicians should continue to recommend to parents that increasing time spent outdoors might be a simple approach to reduce the risk of development of myopia in children and adolescents. The results of this study, however, do not support a further suggestion that increasing the amount of outdoor activity will result in an earlier stabilisation of myopia. Rather, our data suggest that spending less time on near work in early childhood may have some role in earlier myopia stabilisation. While it is generally not popular to recommend that children spend less time reading, clinicians could perhaps suggest better near visual hygiene such as longer working distances and more frequent breaks. 23
Conclusions
While time spent in outdoor activities in earlier childhood does not appear to be related to myopia stabilisation by age 15, spending less time on nearwork in earlier childhood may potentially be associated with stabilisation by that same age.
Acknowledgments
This research was supported by National Eye Institute, National Institute of Health, Department of Health and Human Services, NEI/NIH grants EY11756, EY11754, EY11805, EY11752, EY11740, and EY11755.
Footnotes
The members of the COMET study group are as follows:
Study Chair: J Gwiazda (Study Chair/PI); T Norton; K Grice (9/96-7/99); C Fortunato (8/99-9/00); C Weber (10/00-8/03); A Beale (11/03-7/05); D Kern (8/05-8/08); S Bittinger (8/08-4/11); D Ghosh (5/11-present); R Pacella (10/96-10/98).
Coordinating Center: L Hyman (PI); MC Leske (until 9/03); M Hussein (until 10/03); LM Dong (12/03-5/10); M Fazzari (5/11-4/12); E Schoenfeld (until 9/05); L Dias (6/98-present); R Harrison (4/97-3/98); W Zhu (until 12/06); K Zhang (04/06-present); Y Wang (1/00-12/05); A Yassin (1/98-1/99); E Schnall (11/97-11/98); C Rau (2/99-11/00); J Thomas (12/00-04/04); M Wasserman (05/04-07/06); Y Chen (10/06-1/08); S Ahmed (1/09-6/11); L Merill (10/11-present); L Passanant (2/98-12/04); M Rodriguez (10/00-present); A Schmertz (1/98-12/98); A Park (1/99-4/00); P Neuschwender (until 11/99); G Veeraraghavan (12/99-4/01); A Santomarco (7/01-8/04); L Sisti (4/05-10/06); L Seib (6/07-present).
National Eye Institute: D Everett (Project Officer).
Clinical Centres
University of Alabama at Birmingham School of Optometry: W Marsh-Tootle (PI); K Niemann (9/98-present); M Frazier (1/10-present); C Baldwin (10/98-present); C Dillard (10/09-present); K Becker (7/99-3/03); J Raley (9/97-4/99); A Rawden (10/97-9/98); N Harris (3/98-9/99); T Mars (10/97-3/03); R Rutstein (until 8/03).
New England College of Optometry: D Kurtz (PI until 6/07); E Weissberg (6/99-present; PI since 6/07); B Moore (until 6/99); E Harb (8/08-present); R Owens; S Martin (until 9/98); J Bolden (10/98-9/03); J Smith (1/01-8/08); D Kern (8/05-8/08); S Bittinger (8/08-4/11); D Ghosh (5/11-present); B Jaramillo (3/00-6/03); S Hamlett (6/98-5/00); L Vasilakos (2/02-12/05); S Gladstone (6/04-3/07); C Owens (6/06-9/09); P Kowalski (until 6/01); J Hazelwood (7/01-803).
University of Houston College of Optometry: R Manny (PI); C Crossnoe (until 5/03); K Fern; S Deatherage (until 3/07); C Dudonis (until 1/07); S Henry (until 8/98); J McLeod (9/98-8/04; 2/07-5/08); M Batres (8/04-1/06); J Quiralte (1/98-7/05); G Garza (8/05-1/07); G Solis (3/07-8/11); A Ketcham (6/07-9/11).
Pennsylvania College of Optometry: M Scheiman (PI); K Zinzer (until 4/04); K Pollack (11/03-present); T Lancaster (until 6/99); T Elliott (until 8/01); M Bernhardt (6/99-5/00); D Ferrara (7/00-7/01); J Miles (8/01-12/04); S Wilkins (9/01-8/03); R Wilkins (01/02-8/03); J N Smith (10/03-9/05); D D'Antonio (2/05-5/08); L Lear (5/06-1/08); S Dang (1/08-2/10); C Sporer ( 3/10-10/11); M Jameson (10/11-present); A Grossman (8/01-11/03); M Torres (7/97-6/00); H Jones (8/00-7/01); M Madigan-Carr (7/01-3/03); T Sanogo (7/99-3/03); J Bailey (until 8/03).
Data and Safety Monitoring Committee: R Hardy (Chair); A Hillis; D Mutti; R Stone; Sr. C Taylor.
References
- 1.Lin LL, Shih YF, Hsiao CK, Chen CJ. Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann Acad Med Singapore. 2004;33:27–33. [PubMed] [Google Scholar]
- 2.Vitale S, Sperduto RD, Ferris FL., 3rd Increased prevalence of myopia in the United States between 1971-1972 and 1999-2004. Arch Ophthalmol. 2009;127:1632–1639. doi: 10.1001/archophthalmol.2009.303. [DOI] [PubMed] [Google Scholar]
- 3.Fan DS, Lam DS, Lam RF, et al. Prevalence, incidence, and progression of myopia of school children in Hong Kong. Invest Ophthalmol Vis Sci. 2004;45:1071–1075. doi: 10.1167/iovs.03-1151. [DOI] [PubMed] [Google Scholar]
- 4.Saw SM, Goh PP, Cheng A, Shankar A, Tan DT, Ellwein LB. Ethnicity-specific prevalences of refractive errors vary in Asian children in neighbouring Malaysia and Singapore. Br J Ophthalmol. 2006;90:1230–1235. doi: 10.1136/bjo.2006.093450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saw SM, Gazzard G, Shih-Yen EC, Chua WH. Myopia and associated pathological complications. Ophthalmic Physiol Opt. 2005;25:381–391. doi: 10.1111/j.1475-1313.2005.00298.x. [DOI] [PubMed] [Google Scholar]
- 6.Morgan I, Rose K. How genetic is school myopia? Prog Retin Eye Res. 2005;24:1–38. doi: 10.1016/j.preteyeres.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 7.Kiefer AK, Tung JY, Do CB, et al. Genome-wide analysis points to roles for extracellular matrix remodeling, the visual cycle, and neuronal development in myopia. PLoS Genet. 2013;9:e1003299. doi: 10.1371/journal.pgen.1003299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Verhoeven VJ, Hysi PG, Wojciechowski R, et al. Genome-wide meta-analyses of multiancestry cohorts identify multiple new susceptibility loci for refractive error and myopia. Nat Genet. 2013;45:314–318. doi: 10.1038/ng.2554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saw SM, Chua WH, Hong CY, et al. Nearwork in early-onset myopia. Invest Ophthalmol Vis Sci. 2002;43:332–339. [PubMed] [Google Scholar]
- 10.Mutti DO, Mitchell GL, Moeschberger ML, Jones LA, Zadnik K. Parental myopia, near work, school achievement, and children's refractive error. Invest Ophthalmol Vis Sci. 2002;43:3633–3640. [PubMed] [Google Scholar]
- 11.Saw SM, Nieto FJ, Katz J, Schein OD, Levy B, Chew SJ. Factors related to the progression of myopia in Singaporean children. Optom Vis Sci. 2000;77:549–554. doi: 10.1097/00006324-200010000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Low W, Dirani M, Gazzard G, et al. Family history, near work, outdoor activity, and myopia in Singapore Chinese preschool children. Br J Ophthalmol. 2010;94:1012–1016. doi: 10.1136/bjo.2009.173187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gwiazda JE, Hyman L, Norton TT, et al. Accommodation and related risk factors associated with myopia progression and their interaction with treatment in COMET children. Invest Ophthalmol Vis Sci. 2004;45:2143–2151. doi: 10.1167/iovs.03-1306. [DOI] [PubMed] [Google Scholar]
- 14.Lu B, Congdon N, Liu X, et al. Associations between near work, outdoor activity, and myopia among adolescent students in rural China: the Xichang Pediatric Refractive Error Study report no. 2. Arch Ophthalmol. 2009;127:769–775. doi: 10.1001/archophthalmol.2009.105. [DOI] [PubMed] [Google Scholar]
- 15.Rose KA, Morgan IG, Ip J, et al. Outdoor activity reduces the prevalence of myopia in c hildren. Ophthalmology. 2008;115:1279–1285. doi: 10.1016/j.ophtha.2007.12.019. [DOI] [PubMed] [Google Scholar]
- 16.Dirani M, Tong L, Gazzard G, et al. Outdoor activity and myopia in Singapore teenage children. Br J Ophthalmol. 2009;93:997–1000. doi: 10.1136/bjo.2008.150979. [DOI] [PubMed] [Google Scholar]
- 17.Rose KA, Morgan IG, Smith W, Burlutsky G, Mitchell P, Saw SM. Myopia, lifestyle, and schooling in students of Chinese ethnicity in Singapore and Sydney. Arch Ophthalmol. 2008;126:527–530. doi: 10.1001/archopht.126.4.527. [DOI] [PubMed] [Google Scholar]
- 18.Deng L, Gwiazda J, Thorn F. Children's refractions and visual activities in the school year and summer. Optom Vis Sci. 2010;87:406–413. doi: 10.1097/OPX.0b013e3181da8a85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.French AN, Ashby RS, Morgan IG, Rose KA. Time outdoors and the prevention of myopia. Exp Eye Res. 2013;114:58–68. doi: 10.1016/j.exer.2013.04.018. [DOI] [PubMed] [Google Scholar]
- 20.French AN, Morgan IG, Mitchell P, Rose KA. Patterns of myopigenic activities with age, gender and ethnicity in Sydney schoolchildren. Ophthalmic Physiol Opt. 2013;33:318–328. doi: 10.1111/opo.12045. [DOI] [PubMed] [Google Scholar]
- 21.French AN, Morgan IG, Mitchell P, Rose KA. Risk factors for incident myopia in Australian schoolchildren: the sydney adolescent vascular and eye study. Ophthalmology. 2013;120:2100–2108. doi: 10.1016/j.ophtha.2013.02.035. [DOI] [PubMed] [Google Scholar]
- 22.Jones LA, Sinnott LT, Mutti DO, Mitchell GL, Moeschberger ML, Zadnik K. Parental history of myopia, sports and outdoor activities, and future myopia. Invest Ophthalmol Vis Sci. 2007;48:3524–3532. doi: 10.1167/iovs.06-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ip JM, Saw SM, Rose KA, et al. Role of near work in myopia: findings in a sample of Australian school children. Invest Ophthalmol Vis Sci. 2008;49:2903–2910. doi: 10.1167/iovs.07-0804. [DOI] [PubMed] [Google Scholar]
- 24.Wu PC, Tsai CL, Hu CH, Yang YH. Effects of outdoor activities on myopia among rural school children in Taiwan. Ophthalmic Epidemiol. 2010;17:338–342. doi: 10.3109/09286586.2010.508347. [DOI] [PubMed] [Google Scholar]
- 25.Sherwin JC, Reacher MH, Keogh RH, Khawaja AP, Mackey DA, Foster PJ. The Association between Time Spent Outdoors and Myopia in Children and Adolescents: A Systematic Review and Meta-analysis. Ophthalmology. 2012;119:2141–2151. doi: 10.1016/j.ophtha.2012.04.020. [DOI] [PubMed] [Google Scholar]
- 26.Wu PC, Tsai CL, Wu HL, Yang YH, Kuo HK. Outdoor Activity during Class Recess Reduces Myopia Onset and Progression in School Children. Ophthalmology. 2013;120:1080–1085. doi: 10.1016/j.ophtha.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 27.Khader YSBW, Abdul-Aziz SM, Al-Shiekh-Khalil MI. Prevalence and risk indicators of myopia among schoolchildren in Amman, Jordan. East Mediterr Health J. 2006;12:434–439. [PubMed] [Google Scholar]
- 28.Jones-Jordan LA, Sinnott LT, Cotter SA, et al. Time outdoors, visual activity, and myopia progression in juvenile-onset myopes. Invest Ophthalmol Vis Sci. 2012;53:7169–7175. doi: 10.1167/iovs.11-8336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goss DA. Nearwork and myopia. Lancet. 2000;356:1456–1457. doi: 10.1016/S0140-6736(00)02864-6. [DOI] [PubMed] [Google Scholar]
- 30.Goldschmidt E. The importance of heredity and environment in the etiology of low myopia. Acta Ophthalmol (Copenh) 1981;59:759–762. doi: 10.1111/j.1755-3768.1981.tb08743.x. [DOI] [PubMed] [Google Scholar]
- 31.Williams C, Miller LL, Gazzard G, Saw SM. A comparison of measures of reading and intelligence as risk factors for the development of myopia in a UK cohort of children. Br J Ophthalmol. 2008;92:1117–1121. doi: 10.1136/bjo.2007.128256. [DOI] [PubMed] [Google Scholar]
- 32.Thorn F, Gwiazda J, Held R. Myopia progression is specified by a double exponential growth function. Optom Vis Sci. 2005;82:286–297. doi: 10.1097/01.opx.0000159370.66540.34. [DOI] [PubMed] [Google Scholar]
- 33.Dong Li Ming, Thorn F, Gwiazda J, Hyman L, Norton TT. American Academy of Optometry. Denver, CO: 2006. Use of the Gompertz function to describe the course of myopia progression and stabilization in the correction of myopia evaluation trial (COMET) [Google Scholar]
- 34.Goss DA, Winkler RL. Progression of myopia in youth: age of cessation. Am J Optom Physiol Opt. 1983;60:651–658. doi: 10.1097/00006324-198308000-00002. [DOI] [PubMed] [Google Scholar]
- 35.Gwiazda J. Treatment options for myopia. Optom Vis Sci. 2009;86:624–628. doi: 10.1097/OPX.0b013e3181a6a225. [DOI] [PMC free article] [PubMed] [Google Scholar]


