TO THE EDITOR
Post-traumatic stress disorder (PTSD) is common in primary care patients1 and is associated with psychological distress, suicide risk, and disability. PTSD also increases risk of incident and recurrent cardiovascular events,2 possibly by reducing medication adherence.3 Prior studies showing an association between PTSD and medication non-adherence3 are limited by their use of self-report to measure adherence as PTSD can bias reporting of negative behaviors.4 We evaluated the association between PTSD and antihypertensive medication adherence using electronic monitoring in primary care patients with uncontrolled hypertension.
METHODS
We enrolled a convenience sample of patients with uncontrolled hypertension from an academic hospital-based primary care clinic in New York City. Patients were eligible if they had elevated blood pressure (BP) on two consecutive clinic visits prior to enrollment (BP ≥140/90 mm Hg or ≥130/80 mm Hg if they had diabetes or chronic kidney disease). Patients were ineligible if they had dementia, psychosis, active substance abuse, or resided in an institutional setting. All patients provided written informed consent. The institutional review board of Columbia University Medical Center approved the protocol.
We evaluated PTSD using the 4-item Primary Care PTSD screen (PC-PTSD), which asks patients whether, in response to a traumatic event, they had current PTSD symptoms (re-experiencing, numbing, avoidance, and hyperarousal). A cutpoint of 3 on this screen has good sensitivity and specificity (>80%) for diagnosing PTSD as compared to a clinical interview.5 We assessed medication adherence during the interval between two subsequent clinic visits using an electronic pillbox (MedSignals®). Each BP medication was stored in one of four pillbox compartments. The pillbox records the date and time when each compartment is opened. Regimen adherence was calculated as the mean adherence to monitored medications, with adherence to each medication calculated as the percent of days the prescribed number of doses was taken.
Patients were categorized as non-adherent if regimen adherence was <80%.6 Logistic regression was used to determine whether PTSD symptoms were associated with non-adherence after adjusting for covariates commonly associated with adherence (age, gender, race, ethnicity, number of blood pressure medications, and depressive symptoms measured by the 8-item Patient Health Questionnaire).
RESULTS
Between 2011 and 2013, we identified 123 patients who met eligibility criteria; 114 (92%) consented and 98 (86%) had usable pillbox data. The mean (SD) age was 64 years (9), 76% were women, 81% Hispanic, and 29% white. Fifty-nine percent had no PTSD symptoms, 20% had 1–2 symptoms, and 19% had 3–4 symptoms, consistent with a positive screen for PTSD.
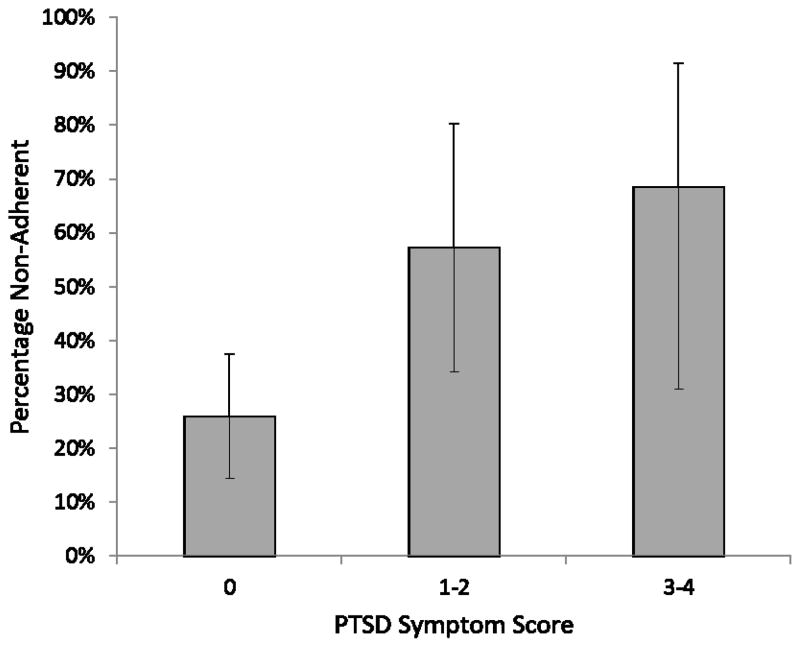
The mean number of prescribed BP medications was 2.6 (0.9). Adherence was monitored for a mean of 56 (43) days. Median regimen adherence was 86% (interquartile range 58%-97%), and 41% of the sample was non-adherent (<80% of days). In unadjusted analysis, there was a graded association between PTSD symptoms and medication non-adherence (Figure). Sixty-eight percent of patients who screened positive for PTSD were non-adherent compared to 26% without any PTSD symptoms (P=0.001). In adjusted analyses, PTSD symptoms continued to be associated with non-adherence; those who screened positive for PTSD had 5.2 (95% CI 1.1–24.4) increased odds of non-adherence compared to those without PTSD symptoms (p=0.04; Table).
Figure.
Post-traumatic stress disorder (PTSD) symptoms and non-adherence to antihypertensive medications.
Non-adherence was defined as taking less than 80% of the antihypertensive regimen. Error bars represent 95% confidence intervals.
Table.
Unadjusted and Adjusted Association between Post-Traumatic Stress Disorder Symptoms and Non-Adherence to Blood Pressure Medications
| Characteristic | Unadjusted Odds Ratio | 95% Confidence Interval | P-value | Adjusted Odds Ratio | 95% Confidence Interval | P-value |
|---|---|---|---|---|---|---|
| PC-PTSD score | ||||||
| Reference 0 | - | - | - | - | - | - |
| 1–2 | 3.82 | 1.34–10.87 | 0.01 | 4.22 | 1.33–13.51 | 0.02 |
| 3–4 | 6.21 | 2.00–19.23 | 0.002 | 5.18 | 1.10–24.39 | 0.04 |
| Age | 1.10 | 0.91 – 1.00 | 0.05 | 0.96 | 0.91–1.01 | 0.14 |
| Male | 0.76 | 0.30 – 1.93 | 0.57 | 0.76 | 0.26–2.17 | 0.60 |
| Hispanic | 1.39 | 0.51 – 3.82 | 0.52 | 1.62 | 0.50–5.29 | 0.43 |
| White | 0.74 | 0.30 – 1.83 | 0.52 | 1.10 | 0.38–3.22 | 0.86 |
| Number of blood pressure medications | 1.60 | 1.01–2.54 | 0.05 | 1.66 | 0.99–2.78 | 0.06 |
| Depressive symptoms | 1.08 | 1.01 – 1.16 | 0.03 | 1.00 | 0.90–1.10 | 0.90 |
Abbreviations: PC-PTSD, Primary Care Post-Traumatic Stress Disorder screening questionnaire
CONCLUSIONS
This study is the first to demonstrate that PTSD is an independent risk factor for non-adherence among patients with uncontrolled hypertension, and offers a potential mechanism by which PTSD is associated with cardiovascular disease. Limitations include its modest sample size, recruitment from a single urban practice, and brief assessment period. Given the prevalence of PTSD and its strong association with medication non-adherence, our findings provide impetus to evaluate the benefit of enhanced screening and treatment for PTSD in medical settings to improve cardiovascular risk in these patients.
Acknowledgments
Funding Support: The study was supported by the National Heart, Lung, and Blood Institute (NHLBI) (K23 HL098359) and the American Heart Association (10SDG2600321). Dr. Edmondson was supported by NHLBI (HL117832). Drs. Cohen and Voils were supported by resources from the Department of Veterans Affairs (DVA). The views expressed in this article are those of the authors and do not necessarily represent the views of the DVA nor of the other sponsors of the study. The sponsors had no role in the design and conduct of the study, nor in the collection, management, analysis, and interpretation of the data, nor in the preparation, review, approval of the manuscript, and decision to submit the manuscript for publication.
Footnotes
Conflicts of Interest: None
Financial Disclosures: None
References
- 1.Liebschutz J, Saitz R, Brower V, et al. PTSD in urban primary care: high prevalence and low physician recognition. J Gen Intern Med. 2007 Jun;22(6):719–726. doi: 10.1007/s11606-007-0161-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Edmondson D, Cohen BE. Posttraumatic stress disorder and cardiovascular disease. Prog Cardiovasc Dis. 2013 May-Jun;55(6):548–556. doi: 10.1016/j.pcad.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kronish IM, Edmondson D, Li Y, Cohen BE. Post-traumatic stress disorder and medication adherence: results from the Mind Your Heart study. J Psychiatr Res. 2012 Dec;46(12):1595–1599. doi: 10.1016/j.jpsychires.2012.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frueh BC, Hamner MB, Cahill SP, Gold PB, Hamlin KL. Apparent symptom overreporting in combat veterans evaluated for PTSD. Clin Psychol Rev. 2000 Oct;20(7):853–885. doi: 10.1016/s0272-7358(99)00015-x. [DOI] [PubMed] [Google Scholar]
- 5.Freedy JR, Steenkamp MM, Magruder KM, et al. Post-traumatic stress disorder screening test performance in civilian primary care. Fam Pract. 2010 Dec;27(6):615–624. doi: 10.1093/fampra/cmq049. [DOI] [PubMed] [Google Scholar]
- 6.Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009 Jun 16;119(23):3028–3035. doi: 10.1161/CIRCULATIONAHA.108.768986. [DOI] [PubMed] [Google Scholar]