Abstract
Introduction:
Despite the widespread use of physician return-for-service (RFS) programs in Canada, few have been evaluated. We examined two types of RFS agreements (Family Medicine Bursary and Special Funded Residency Position) and (a) describe the proportion of RFS physicians who complete their service obligation and identify the predictors of completion and (b) compare the retention of RFS physicians to that of non-RFS physicians.
Methods:
Using administrative data on physicians with RFS agreements in Newfoundland and Labrador (NL), Memorial University's Postgraduate Medical Education Office and the Physician and Medical Practice Database, we calculated the proportion of RFS physicians (1997–2009) who fulfilled their service obligation and also identified predictors of completion. We then followed to 2010 a cohort of physicians who started practice in NL between 2000 and 2005 to compare the retention of RFS and non-RFS physicians.
Results:
Ninety-six (71.6%) of 134 RFS physicians fulfilled the service obligation in full. Physicians who held Special Funding Residency Position RFS agreements were 11.1 times less likely (95% CI: 4.0–33.3) to complete their service commitment than physicians who held Family Medicine Bursary RFS agreements. In the cohort of 60 RFS and 67 non-RFS physicians, 16.9% of RFS versus 41.8% of non-RFS physicians left NL by 2010 (p=0.004). RFS physicians were 3.22 times less likely (95% CI: 1.41–7.14) than non-RFS physicians to leave the province. Four years after starting practice, roughly 90% of RFS versus 60% of non-RFS physicians remained in NL; after 10 years, 70% of RFS versus 60% of non-RFS physicians remained (p=0.006).
Conclusion:
The RFS program improves the retention of physicians in NL. Using RFS tied to bursaries rather than residency positions may increase service completion and retention rates.
Abstract
Introduction:
Malgré l'usage répandu des programmes canadiens d'obligation de service (OS) pour les médecins, il y a eu peu d'évaluations de ce type de programmes. Nous avons examiné deux types de programmes d'OS (Family Medicine Bursary et Special Funded Residency Position) et (a) nous avons décrit le nombre de médecins qui ont terminé leur service obligatoire et repéré les paramètres de prévision des médecins qui remplissent leur obligation de service, puis (b) nous avons comparé le taux de rétention des médecins provenant de programmes d'OS par rapport aux médecins hors programme.
Méthodes:
Au moyen de données administratives sur les médecins qui participent aux programmes d'OS à Terre-Neuve-et-Labrador (TN), de données sur la formation aux cycles supérieurs ainsi que de la base de données Physician and Medical Practice, nous avons calculé le nombre de médecins issus de programmes d'OS (1997–2009) qui ont rempli leur obligation de service, et nous en avons dégagé les paramètres de prévision. Nous avons ensuite suivi jusqu'en 2010 un groupe de médecins qui ont commencé la pratique à TN entre 2000 et 2005 afin de comparer le taux de rétention des médecins OS par rapport aux médecins non OS.
Résultats:
Quatre-vignt-seize (71,6 %) des 134 médecins des programmes d'OS ont rempli leur obligation de service. Les médecins qui ont bénéficié du financement du programme Special Funding Residency Position étaient 11,1 fois moins susceptibles (95 % IC: 4,0–33,3) de compléter leur obligation de service que les médecins qui bénéficiaient du programme Family Medicine Bursary. Pour le groupe de 60 médecins OS et de 67 médecins non OS, 16,9 % des médecins OS, contre 41,8 % des médecins non OS, avaient quitté TN dès 2010 (p=0,004). Les médecins OS étaient 3,22 fois moins susceptibles (95 % IC: 1,41–7,14) que les médecins non OS de quitter TN. Quatre ans après avoir commencé la pratique, environ 90 % des médecins OS, contre 60 % des médecins non OS, étaient toujours à TN; après 10 ans, 70 % des médecins OS, contre 60 % des médecins non OS, étaient toujours à TN (p=0,006).
Conclusion:
Les programmes d'OS améliorent la rétention de médecins à TN. L'emploi de programmes d'OS pour des postes liés à des bourses plutôt qu'à une résidence, peut augmenter le taux d'achèvement du service et le taux de rétention.
Return-for-service (RFS) programs are a commonly used strategy to attract physicians to practice in rural or underserviced communities with the long-term goal of improving physician retention in these communities (Bärnighausen and Bloom 2009). RFS agreements obligate physicians to work in underserviced communities in exchange for financial support that may be provided in the form of bursaries (for tuition and other education costs), student loan remission, funded training positions or unrestricted funds (Mason 1971; Pathman et al. 2000; Sempowski 2004). RFS programs may target physicians at various stages of undergraduate or postgraduate education (or both) and generally require a one-year service commitment for each year of financial support. RFS agreements generally have a “buy-out option” in which participants can pay back the funding (with minimum penalties or interest) if they are unwilling or unable to work in an underserviced community. Service commitments are usually expected to be fulfilled upon completion of postgraduate training.
RFS programs are widely used in Canada; all provinces and territories except Yukon offer them (Neufeld and Mathews 2012). Few studies in Canada have evaluated such programs, particularly in terms of their impact on retention of physicians after the obligated service period (Sempowski 2004). Simoens (2004) suggests that large numbers of RFS physicians in Canada have opted to repay funding rather than work in an underserviced area and that few physicians remain in these communities after fulfilling their service obligation. However, his study was based on interviews with two representatives of unidentified ministries of health. Periodic internal program evaluations of the RFS component of Ontario's Underserviced Area Program reported that between 50% and 60% of program participants fulfilled their service obligation, and two-thirds of these physicians continued to practise in an underserviced community after completing their obligation (Bass and Copeman 1975; Copeman 1979, 1987). These studies, the most recent dating to the 1980s, found that students who received less than three years of bursary support, and women, were less likely to fulfill their service commitment (compared to students who had three years of bursary support, and men, respectively).
Between 1997 and 2006, the province of Newfoundland and Labrador (NL) offered RFS agreements as part of its Fellowships and Bursaries Program (hereafter, “Bursary RFS agreements”) and through Special Funded Residency Positions (“Special Funded RFS agreements”). Bursary RFS agreements – administered by the Department of Health and Community Services – offers funding to medical students and postgraduate residents training in family medicine, psychiatry and other specialist programs where physician shortages have been identified. Special Funded RFS agreements – administered by the Memorial University of Newfoundland (MUN) Faculty of Medicine Postgraduate Medical Education Office – offer postgraduate training positions (along with the salary and benefits). The Special Funded RFS agreements are largely taken by physicians who were unable to secure a position through the Canadian Residency Matching Service (CaRMS) and would otherwise not be able to meet requirements for full licensure to practise in Canada. Bursary and Special Funded RFS agreements are available to postgraduate residents (the Family Medicine Bursary is also available to third- and fourth- year medical students intending to pursue family medicine) (Neufeld and Mathews 2012). Physicians who opt for either Bursary or Special Funded RFS agreements are expected to work in NL for one year for each year of funding received. Physicians may fulfill their service obligation in any community in NL. Alternatively, physicians may pay back their funding with interest.
How effective are RFS agreements in promoting physician retention in NL? Do RFS physicians fulfill their service obligations? Compared to other physicians, how long do RFS physicians remain in NL? In this study, we (a) describe the proportion of RFS physicians who complete their service obligation and identify the predictors of completion and (b) compare the retention of RFS physicians to non-RFS physicians in NL. We hypothesized that the majority (greater than 50%) of RFS physicians would fulfil their service obligation (rather than buy out their obligation or default) and that RFS physicians would work in NL longer than non-RFS physicians.
Methods
The MUN Human Investigation Committee approved this study (reference 09.127).
We linked administrative data from the Department of Health and Community Services Bursary and Fellowships Program, the MUN Postgraduate Medical Education Office and the Physician and Medical Practice Database. The Department of Health and Community Services and the Postgraduate Medical Office provided data on physicians who held RFS agreements including name, sex, graduation year, medical school, type of bursary provided, the years and number of years a bursary was provided and repayment status as of November 2009. The Postgraduate Medical Education Office also provided a list of all residents who had trained at MUN and the dates they had trained. We retrieved the following data from the Physician and Medical Practice Database, a longitudinal research data set of physicians in NL: sex, medical school, year of graduation from medical school, hometown (for MUN graduates only), specialty certifications (e.g., CCFP, FRCP, FRCSC), current and former addresses and address change dates and start and end dates for licence status (e.g., educational, full-time, leave and so on). The data were linked using names, medical school and year of graduation. Once data were linked, names were removed from the data set.
The analysis was conducted in two parts. In part 1, we described the proportion of RFS physicians who completed their service obligation in full and identified predictors of RFS physicians who did so. The study sample consisted of all physicians who held RFS agreements between 1997 and 2009. We excluded any physician who was still in training or who was in the process of working his or her service commitment.
The outcome variable of interest was whether RFS physicians fulfilled their service obligation in its entirety (yes/no). Repayment status was determined by cross-referencing the status reported by the Department of Health and Community Services with the licensing information in the Physicians and Medical Practice Database and data from the Postgraduate Medical Education Office. For example, licensing data were used to determine the number of months that a physician had worked in the province and whether he or she had left it. Only time worked after completion of postgraduate training was counted towards the service commitment (“moonlighting” was not counted as this was generally not accepted by the RFS program). We used data from the Postgraduate Medical Education Office to verify the date when physicians completed their residency training. We relied upon data from the Department of Health and Community Services to determine whether a physician had repaid some or all of the return commitment, whether the physician had been confirmed to have defaulted and whether he or she had left the province to pursue further training (i.e., was still in training).
We used frequencies to describe the characteristics of the sample and chi-square tests (or Fisher's exact tests, if applicable) to compare those who fulfilled and did not fulfill their service commitment in full. We used multiple logistic regression to identify predictors of physicians who fulfilled their service commitment.
Potential covariates included sex, medical school, year of graduation from medical school, type of RFS funding, number of years of bursary received, specialty and community where physicians started practice. The type of RFS agreement reflected whether physicians held Bursary or Special Funded RFS agreements. If the former, the type of bursary was also identified (e.g., family medicine, psychiatry, other specialist or travelling). Two physicians had received a combination of bursaries (other specialist and travelling bursary). They were coded as receiving “other specialist” bursaries. The number of years of bursary was coded into two groups (1–3 years and 4 or more years). The three-year cut-off was used based on frequencies.
Specialty was determined based on credentials. Family physicians included only those who had the Certificant of the College of Family Physicians (CCFP) designation. Specialists were physicians who had the designation Fellow of the Royal College of Physicians of Canada (FRCPC) or Fellow of the Royal College of Surgeons of Canada (FRCSC). Physicians with neither of these designations were coded as “other.” Physicians with both the CCFP and either specialist designation were coded as specialists.
The community where physicians started practice was coded as rural, small urban or urban based on its population. Bedroom communities were considered in the population of a larger centre. Rural communities had populations less than 10,000. This definition has been used in our previous studies of the NL physicians' workforce (Mathews et al. 2007). Small urban communities had populations between 10,000 and 99,999. Urban communities had a population of 100,000 or more. Populations were verified using Statistics Canada data (Statistics Canada 2011).
In part 2, we compared the retention of RFS physicians to non-RFS physicians in NL: whether they remained in the province at the end of the follow-up period and how long they worked in it. We examined all physicians who began their first practice in NL between January 1, 2000 and December 31, 2005. We excluded the time when physicians were still in postgraduate training programs (i.e., “moonlighting”). We excluded non-RFS physicians who worked in the province for less than three months (locums). The three-month cut-off was used in previous physician retention studies in NL (Mathews et al. 2008). We excluded locums because they would decrease the average retention time of the non-RFS physician group. Moreover, unlike RFS physicians, locums are not expected to work in NL beyond a short period of time. Because of the small number of physicians who graduated from other Canadian or international universities in the RFS physician group, we limited our analysis to MUN graduates only.
Licence status was used to determine whether and when a physician left the province. To calculate the amount of time a physician worked in NL, we followed each physician from the time he or she began working (after residency) to December 31, 2010 or until the physician terminated his or her licence (and presumably left the province), whichever came first.
We used frequencies to describe the characteristics of the physicians in the study sample and then chi-square tests (or Fisher's exact tests, if applicable) to compare the physicians who left and remained in NL. We used multiple logistic regression to identify predictors of physicians who left the province. Potential covariates included sex, year of graduation from medical school, hometown (rural, small urban or urban based on the same population cut-offs defined above), community where physicians started practice and whether or not physicians held an RFS bursary. Survival analyses (Kaplan-Meier) and the log-rank test were used to compare the retention of RFS and non-RFS physicians.
In both regression models in the analyses, potential predictors were selected on the basis of significant chi-square tests (including potential interactions). To prevent multi-colinearity, correlations between potential predictors were assessed a priori. The final regression model shows only significant predictors.
In supplementary analyses, we used chi-square tests (or Fisher's exact tests, if applicable) to compare the starting and 2010 work locations of RFS and non-RFS physicians. We followed each physician who began work in the province (regardless of whether or not he or she fulfilled the service commitment) until December 31, 2010. The 2010 work locations were coded using the same population cut-offs as the community where physicians started their practice.
Results
Part 1
Between 1997 and 2009, 218 medical trainees (students and postgraduate residents) held RFS agreements in NL. We excluded 31 physicians who were still completing their postgraduate training and the 53 physicians who were in the process of completing their service commitment as of December 31, 2010, leaving a study sample of 134 physicians.
By December 31, 2010, 96 (71.6%) physicians had fulfilled their contract by completing their service commitment in full (Table 1). Eight (6.0%) repaid their funding and another four (3.0%) fulfilled their commitment through a combination of work and repayment. Twenty-six (19.4%) physicians defaulted on some or all of their commitment. Of these 26 physicians, 20 had begun to work in the province but left without completing their service commitment or repaying owed funds.
TABLE 1.
Detailed return status of physicians who received return-for-service agreements in Newfoundland and Labrador
| Return Status | Total (n=134) | RFS Agreement Type | |
|---|---|---|---|
| Bursary (n=107) | Special Funded(n=27) | ||
| Completed Service | 96 (71.6) | 88 (82.2) | 8 (29.6) |
| Repaid | 8 (6.0) | 5 (4.7) | 3 (11.1) |
| Partial Service/Repaid | 4 (3.0) | 4 (3.7) | 0 (0) |
| Confirmed Default | 6 (4.5) | 4 (3.7) | 2 (7.4) |
| Left Province with Incomplete Service | 20 (14.9) | 6 (5.6) | 14 (51.9) |
RFS = Return-for-service; Bursary = Fellowship and Bursary RFS agreement; Special Funded = Special Funded Residency Position RFS agreement
Note: Physicians who completed service, repaid in full or completed partial service/repaid have fulfilled their contract; those that defaulted or left the province without completing service have not fulfilled their contract.
There were nearly equal proportions of male and female RFS physicians (Table 2). Most RFS physicians graduated after 2000 (61.9%) from MUN (73.1%). The largest proportion of physicians received a Family Medicine Bursary agreement (44.5%), received funding for one to three years (91.0%) and became family physicians (45.2%). Of the 122 physicians who worked in the province, most (60.5%) worked in the greater St. John's area. Fewer than one in five physicians (18.0%) started their practice in a rural community.
TABLE 2.
Characteristics of physicians who received return-for-service bursaries who completed and did not complete service commitment in full
| All RFS Physicians (n=134) n (%) |
Completed Service | p-Value* | ||
|---|---|---|---|---|
| No (n=38) n (%) | No (n=38) n (%) | |||
| Sex | 0.583 | |||
| Male | 69 (51.5) | 21 (55.3) | 48 (50.0) | |
| Female | 65 (48.5) | 17 (44.7) | 48 (50.0) | |
| Graduation Year | 0.082 | |||
| Before 1990 | 9 (6.7) | 5 (13.2) | 4 (4.2) | |
| 1990–1999 | 42 (31.3) | 14 (36.8) | 28 (29.2) | |
| After 2000 | 83 (61.9) | 19 (20.0) | 64 (66.7) | |
| Type of RFS Agreement | <0.000 | |||
| Family Bursary | 59 (44.0) | 10 (26.3) | 49 (51.0) | |
| Psychiatry Bursary | 10 (7.5) | 2 (5.3) | 8 (8.3) | |
| Other Specialist Bursary | 26 (19.4) | 4 (10.5) | 22 (22.9) | |
| Travelling Bursary | 12 (9.0) | 3 (7.9) | 9 (9.4) | |
| Special Funded | 27 (20.1) | 19 (50.0) | 8 (8.3) | |
| Number of Years of Bursary | 0.002 | |||
| 1–3 | 122 (91.0) | 30 (78.9) | 92 (95.8) | |
| 4 or more | 12 (9.0) | 8 (21.1) | 4 (4.2) | |
| Medical School | <0.000 | |||
| Memorial University | 98 (73.1) | 18 (47.4) | 80 (83.3) | |
| Other Canadian University | 9 (6.7) | 2 (5.3) | 7 (7.3) | |
| International University | 27 (20.1) | 18 (47.4) | 9 (9.4) | |
| Specialty | <0.000 | |||
| Family Physician | 52 (45.2) | 8 (28.6) | 44 (50.6) | |
| Specialist | 54 (47.0) | 13 (46.4) | 41 (47.1) | |
| Other | 9 (7.8) | 7 (25.0) | 2 (2.3) | |
| Starting Practice Community | 0.378 | |||
| Urban | 75 (61.5) | 15 (57.7) | 60 (62.5) | |
| Small Urban | 25 (20.5) | 4 (15.4) | 21 (21.9) | |
| Rural | 22 (18.0) | 7 (26.9) | 15 (15.6) | |
RFS = Return-for-service
Comparison of physicians who completed and did not complete the service obligation in full.
Note: Numbers may add up to less than reported sample size due to missing data.
Compared to physicians who did not complete their service commitment, a smaller proportion of physicians who completed their service held Special Funded Residency RFS agreements received four or more years of funding, graduated from an international medical school and were neither family physicians nor specialists (Table 2).
Trainees who held Special Funded RFS agreements were 0.09 times as likely (11.1 times less likely) to complete their service commitment compared to physicians who had received a Bursary RFS agreement (Table 3). The other types of bursary holders were as likely as family medicine bursary holders to complete their service commitment.
TABLE 3.
Multiple logistic regression models for completing service obligations and leaving Newfoundland and Labrador
| Predictor Variable | Odds Ratio (95% Confidence Interval) | p-Value |
|---|---|---|
| Predictors of RFS physicians who complete service obligation in full | ||
| Type of RFS Agreement | <0.000 | |
| Family Medicine Bursary | 1.00 | – |
| Psychiatry Bursary | 0.82 (0.15–4.43) | 0.814 |
| Other Specialist Bursary | 1.12 (0.32–3.97) | 0.858 |
| Travelling Bursary | 0.61 (0.14–2.67) | 0.514 |
| Special Funded | 0.09 (0.03–0.25) | <0.000 |
| Predictors for leaving NL for physicians who started practice between 2000 and 2005 | ||
| Received RFS Bursary | ||
| No | – | – |
| Yes | 0.31 (0.14–0.71) | .005 |
RFS = Return-for-service; NL = Newfoundland and Labrador
Part 2
In part 2 of the analysis, we compared the retention of RFS and non-RFS physicians who started their first practice in NL between January 1, 2000 and December 31, 2005. Of the 218 RFS physicians who received funding between 1997 and 2009, 104 had started practice after 2005 and 39 were still in training. These 143 physicians were excluded from the sample. Of the 75 remaining RFS physicians, 60 graduated from medical school from MUN, three from other Canadian universities and 12 from universities outside Canada. Medical school was not known for two physicians. Because of their small numbers, we excluded other Canadian and international medical graduates and “unknowns” from the analysis, leaving 60 MUN RFS physicians.
To create the non-RFS physician comparison group, we identified 625 physicians who began their first practice between January 1, 2000 and December 31, 2005 and had not received an RFS bursary. We excluded 121 physicians who graduated from other Canadian medical schools and 413 physicians who graduated from international medical schools, leaving 91 MUN medical graduates. We excluded 24 locum physicians, leaving 67 non-RFS physicians.
There were nearly equal proportions of male and female physicians, and family physicians and specialists, in the study sample (Table 4). More than half the physicians in the study sample had graduated from medical school after 2000 (55.9%), came from urban hometowns (53.3%), started practice in an urban community (71.0%), did not have an RFS agreement (52.8%) and had not left the province at the end of the follow-up period (69.3%).
TABLE 4.
Characteristics of Memorial University RFS and non-RFS physicians who began practice in Newfoundland and Labrador between 2000 and 2005 and who left and stayed in the province
| Study Sample (n=127) n (%) |
Left Province | p-Value* | ||
|---|---|---|---|---|
| No (n=88) n (%) | Yes (n=39) n (%) | |||
| Sex | 0.698 | |||
| Male | 62 (48.8) | 44 (50.0) | 18 (46.2) | |
| Female | 65 (51.2) | 44 (50.0) | 21 (53.8) | |
| Graduation Year | 0.884 | |||
| Before 1990 | 5 (3.9) | 3 (3.4) | 2 (5.1) | |
| 1990–1999 | 51 (40.2) | 36 (40.9) | 15 (38.5) | |
| After 2000 | 71 (55.9) | 49 (55.7) | 22 (56.4) | |
| Hometown | 0.749 | |||
| Urban | 65 (53.3) | 43 (51.2) | 22 (57.9) | |
| Small Urban | 16 (13.1) | 11 (13.1) | 5 (13.2) | |
| Rural | 41 (33.6) | 30 (35.7) | 11 (28.9) | |
| Specialty | 0.619 | |||
| Family Physician | 58 (46.0) | 38 (43.2) | 20 (52.6) | |
| Specialist | 57 (45.2) | 42 (47.7) | 15 (39.5) | |
| Other | 11 (8.7) | 8 (9.1) | 3 (7.9) | |
| Starting Practice Community | 0.749 | |||
| Urban | 88 (71.0) | 62 (70.5) | 26 (72.2) | |
| Small Urban | 18 (14.5) | 12 (13.6) | 6 (16.7) | |
| Rural | 18 (14.5) | 14 (15.9) | 4 (11.1) | |
| Received RFS Bursary | 0.004 | |||
| No | 67 (52.8) | 39 (44.3) | 28 (71.8) | |
| Yes | 60 (47.2) | 49 (55.7) | 11 (28.2) | |
RFS = Return-for-service
Comparison of physicians who left and did not leave the province.
Note: Numbers may add up to less than reported sample size due to missing data.
Compared to physicians who stayed in NL, a larger proportion of non-RFS physicians than RFS physicians left the province (Table 4). There were no other significant differences in the characteristics of physicians who stayed and left the province.
The only significant predictor of leaving the province was whether or not a physician received an RFS bursary (Table 3). RFS physicians were 0.31 times as likely (or 3.2 times less likely) compared to non-RFS physicians to leave the province.
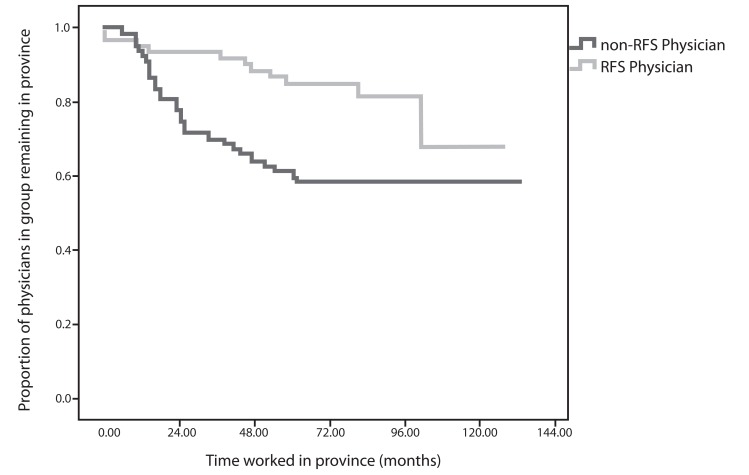
Figure 1 shows the Kaplan-Meier survival curves of RFS and non-RFS physicians. Four years after starting practice, roughly 90% of RFS physicians remained in the province, compared to roughly 60% of non-RFS physicians. After 10 years, roughly 70% of RFS physicians remain in the province, compared to roughly 60% of non-RFS physicians. The log-rank test (chi-square=7.678, degrees of freedom=1, p value=0.006) confirmed that RFS physicians worked longer in the province than non-RFS physicians.
FIGURE 1.
Kaplan-Meier survival curves for RFS and non-RFS physicians
In supplementary analyses, we examined the locations where RFS and non-RFS physicians worked when they started practice and at the end of the follow-up period in 2010. There was no difference in the starting locations of RFS and non-RFS physicians; however, in 2010, at the end of the follow-up period, a greater proportion of non-RFS than RFS physicians had left the province (Table 5). Of the 50 non-RFS physicians who started practice in an urban community (St. John's), most (60.0%) remained in St. John's in 2010 (Table 6). Most (83.3%) of the non-RFS physicians who started practice in a small urban community had left the province by 2010. The majority (55.5%) of non-RFS physicians who started in a rural community remained in a rural community in 2010. Most RFS physicians continued to work in the same size community in 2010 as when they started practice.
TABLE 5.
Summary of the locations of RFS and non-RFS physicians at the start of their practice and in 2010
| Had RFS Bursary | p-Value* | ||
|---|---|---|---|
| No (n=65)* n (%) | Yes (n=59)* n (%) | ||
| Starting Practice Community | 0.187 | ||
| Urban | 50 (76.9) | 38 (64.4) | |
| Small Urban | 6 (9.2) | 12 (20.3) | |
| Rural | 9 (13.8) | 9 (15.3) | |
| 2010 Practice Community | 0.006 | ||
| Urban | 5 (7.6) | 7 (11.9) | |
| Small Urban | 4 (6.2) | 12 (20.3) | |
| Rural | 30 (46.2) | 30 (50.8) | |
| Left the Province | 26 (40.0) | 10 (16.9) | |
RFS = Return-for-service
Starting practice community was not available for two non-RFS physicians; one RFS physician defaulted.
TABLE 6.
Location of RFS and non-RFS physicians at the start of their practice and in 2010
| Starting Practice Community | 2010 Practice Community n (%) | ||||||
|---|---|---|---|---|---|---|---|
| Same Rural | New Rural | Same Small Urban | New Small Urban | Same Urban | New Urban | Left Province | |
| Non-RFS Physicians (n=65)* | |||||||
| Urban n=50 | – | – | – | 2 (4.0) | 30 (60.0) | – | 18 (36.0) |
| Small Urban n=6 | – | – | 1 (16.7) | – | – | – | 5 (83.3) |
| Rural n=9 | 2 (22.2) | 3 (33.3) | – | 1 (11.1) | – | – | 3 (33.3) |
| RFS Physicians (n=59)* | |||||||
| Urban n=38 | – | – | – | 2 (5.3) | 28 (73.5) | – | 8 (21.0) |
| Small Urban n=12 | – | – | 10 (83.3) | – | – | 1 (8.3) | 1 (8.3) |
| Rural n=9 | 4 (44.4) | 3 (33.3) | – | – | – | 1 (11.1) | 1 (11.1) |
RFS = Return-for-service
Starting and 2010 practice community was not available for two non-RFS physicians; one RFS physician defaulted.
Discussion
Over 80% of RFS physicians in NL fulfill their RFS contract (through either work or repayment). The vast majority of RFS physicians who do so (96 of 108, 89.0%) complete their service commitment in its entirety. These findings support our hypothesis that the majority of RFS physicians fulfill their service obligation (rather than buy out their obligation or default). The 80.6% RFS fulfillment rate is lower than rates cited by RFS program managers in Nova Scotia (89%) and Quebec (90%–95%), but these programs had not been formally evaluated at the time of this study (Neufeld and Mathews 2012). The 89% service completion rate in NL is higher than the 50%–60% found in the 1980s-era evaluations of Ontario's Underserviced Area Program – Rural (Copeman 1979, 1987). A meta-analysis found that 71% of RFS participants completed service obligations in full or were in the process of completing obligations (Bärnighausen and Bloom 2009). If we calculated completion rates using the methods applied in these studies (including the 53 RFS physicians who are in the process of working their service commitment), the completion rate for NL is 86.1% (161 of 187 RFS physicians).
Almost one in five RFS physicians in NL defaulted on some or all of their RFS contract. The majority of physicians left the province before completing their service commitment and had not repaid their remaining obligation. The default rate (i.e., failed to fulfill service requirements or pay back funding) among NL RFS physicians is within the range (2%–23%) cited in other studies (Copeman 1987; Jackson et al. 2003; Mason 1971; Navin and Nichols 1977; Pathman et al. 2000). A survey of West Virginia RFS program defaulters reported that unavailability of locations suitable to family members, low bursary amounts, poor recruitment from sites and changes in personal priorities were frequently cited reasons for defaulting (Jackson et al. 2003).
We found a number of discrepancies between the RFS status reported in Department of Health and Community Services and Postgraduate Medical Education Office records and the RFS status indicated by the licensing records. More and regular communication between the Department and RFS physicians, and verification of return status using billing and/or licensing data, may reduce the number of RFS physicians who default.
Physicians with Bursary RFS agreements (88 of 107; 82.2%) had a higher service completion rate than physicians with Special Funded RFS agreements (8 of 27; 29.6%). Although physicians with Special Funded RFS agreements comprise 20% of the study sample, they accounted for half of all the physicians (19 of 38; 50%) who did not complete the service commitment in full. The default rate may be related to the large proportion (20 or 27; 74.1%) of international medical graduates who participate in Special Funded RFS agreements. A previous study of postgraduate residents had found that few international medical graduates who had done residency training in NL remained in the province after their training (Mathews et al. 2007).
MUN-graduated RFS physicians remained in NL longer than their non-RFS counterparts. The majority of RFS physicians remained in the practice setting (i.e., rural, small urban or urban) after they completed their service obligation. These findings support our hypothesis that RFS physicians work in NL longer than non-RFS physicians. It is difficult to compare retention across studies because few studies consider the same outcome (e.g., retention in service community, in rural community, in any rural or underserved community), examine similar physicians (e.g., primary care and specialist physicians) or have similar follow-up periods (Bärnighausen and Bloom 2009).
Our evaluation examines the RFS agreement initiatives available in NL between 1997 and 2006. In 2007, RFS agreements were required for physicians who had been matched through the CaRMS international medical graduate stream. Physicians who are matched through this stream are required to accept an RFS agreement. The results from this study suggest that RFS agreements wherein physicians have little choice but to accept have higher default rates than RFS agreements chosen by physicians.
RFS programs should ideally balance the province's need to fill vacancies in specific communities with individual physician preference (whether in terms of accepting an RFS agreement or determining where to work) (Neufeld and Mathews 2012). RFS agreements that provide provinces with little say in where physicians work may do little to address physician mal-distribution. In 2013, the federal government will also launch its RFS program to encourage physicians to practise in rural communities (generally, communities with populations of 50,000 or less that are not near larger urban centres (Government of Canada 2012). However, RFS-eligible communities under the federal RFS program may not necessarily be RFS-eligible communities under provincial RFS programs; coordination between programs is needed to encourage physicians to work in underserved communities. Further research should assess the federal program's impact on provincial RFS programs and the retention and distribution of physicians within each province.
Limitations
Given our reliance on administrative data, we were able to consider only a handful of covariates in our analyses. While survey data would allow us to gather information on a greater number of variables, administrative data allowed us to verify reported RFS repayment status against licensing data. It is possible, however, that despite holding NL licences, physicians did not actually work in the province. We were unable to examine the retention patterns of RFS physicians who graduated from international or other Canadian medical schools. We also cannot conclude that RFS agreements cause higher retention of physicians. Self-selection of RFS program participants limits the ability to assess causality (Grobler et al. 2009). Surveys of health professionals (including medical students and physicians) have found that most individuals who took an RFS bursary were predisposed to working in the region, regardless of the RFS bursary program (Neufeld and Mathews 2012; Renner et al. 2010).
The NL RFS agreements require physicians to return service anywhere in the province (with provincial approval), regardless of whether they are family or specialist physicians. Most other programs in Canada require physicians to return service in specific, usually rural, communities (Neufeld and Mathews 2012); as a result, our findings may not be generalizable to other RFS programs in Canada. Further research is needed to evaluate service fulfillment rates and retention patterns in other Canadian RFS programs.
Conclusion
The RFS program improves the retention of physicians in NL. Most (71.9%) RFS physicians fulfill their service commitments. Another 9% fulfill their contractual obligations either by repaying their funding in full (with applicable penalties/interest) or through a combination of work and repayment. RFS agreements linked to bursary funding were more effective than RFS agreements linked to residency position funding. Physicians Special Funded RFS agreements were more than 11 times less likely than those physicians with Family Medicine Bursary RFS agreements to complete their service commitments. RFS physicians were more likely to remain in the province than non-RFS physicians. More than half of RFS physicians remained in their starting practice setting. Based on this study, we recommend limiting RFS agreements to optional, bursary-type incentives and improving the tracking of RFS physicians to increase service completion and retention rates.
Acknowledgements
This study was funded by the Newfoundland and Labrador Centre for Applied Health Research. The Physician and Medical Practice Database used in this study was funded by the Canada Foundation for Innovation and the Newfoundland and Labrador Industrial Research and Innovation Fund. We thank Dr. Larry Alteen and Mr. Daniel Fitzgerald, Department of Health and Community Medical Services Division, Department of Health and Community Services for their assistance with this project and their feedback on an earlier draft of this paper.
Contributor Information
Maria Mathews, Division of Community Health & Humanities, Faculty of Medicine, Memorial University, St. John's, NL.
Sara Lynn Heath, Division of Community Health & Humanities, Faculty of Medicine, Memorial University, St. John's, NL.
Shelley May Neufeld, Division of Community Health & Humanities, Faculty of Medicine, Memorial University, St. John's, NL.
Asoka Samarasena, Postgraduate Medical Education, Faculty of Medicine, Memorial University, St. John's, NL.
REFERENCES
- Bärnighausen T., Bloom D.E. 2009. “Financial Incentives for Return of Service in Underserved Areas: A Systematic Review.” BMC Health Services Research 8(86): 1–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bass M., Copeman W.J. 1975. “An Ontario Solution to Medically Underserviced Areas: Evaluation of an Ongoing Program.” Canadian Medical Association Journal 113(5): 403–07 [PMC free article] [PubMed] [Google Scholar]
- Copeman W.J. 1979. “Experience with an Undergraduate Medical Bursary Program in Ontario.” Canadian Medical Association Journal 121(9): 1170. [PMC free article] [PubMed] [Google Scholar]
- Copeman W.J. 1987. “The Underserviced Area Program of the Ministry of Health of Ontario.” Canadian Family Physician 33: 1683–85 [PMC free article] [PubMed] [Google Scholar]
- Government of Canada. 2012. “After Post Secondary Education – Family Doctors and Nurses Can Get Canada Student Loan Forgiveness.” Retrieved December 18, 2012 <http://www.canlearn.ca/eng/after/forgiveness/index.shtml>.
- Grobler L., Marais B.J., Mabunda S.A., Marindi P.N., Reuter H., Volmink J. 2009. “Interventions for Increasing the Proportion of Health Professionals Practicing in Rural and Underserved Areas.” Cochrane Database of Systematic Reviews 1: CD005314. [DOI] [PubMed] [Google Scholar]
- Jackson J., Shannon K., Pathman D.E., Mason E., Nermitz J.W. 2003. “A Comparative Assessment of West Virginia's Financial Incentive Programs for Rural Physicians.” Journal of Rural Health 19(Suppl.): 329–39 [DOI] [PubMed] [Google Scholar]
- Mason H.R. 1971. “Effectiveness of Student Aid Programs Tied to a Service Commitment.” Journal of Medical Education 46: 575–83 [DOI] [PubMed] [Google Scholar]
- Mathews M., Edwards A.C., Rourke J.T.B. 2008. “Retention of Provisionally Licensed International Medical Graduates: A Historical Cohort Study of General and Family Physicians in Newfoundland and Labrador.” Open Medicine 2(20): 37–44 [PMC free article] [PubMed] [Google Scholar]
- Mathews M., Park A.D., Rourke J.T.B. 2007. “Retention of International Medical Graduates Following Postgraduate Medical Training in Newfoundland and Labrador.” Healthcare Policy 3(2): 50–57 [PMC free article] [PubMed] [Google Scholar]
- Navin T.R., Nichols A.W. 1977. “Evaluation of the Arizona Medical Student Exchange Program.” Journal of Medical Education 52: 817–23 [DOI] [PubMed] [Google Scholar]
- Neufeld S.M., Mathews M. 2012. “Canadian Return-for-Service Bursary Programs for Medical Trainees.” Healthcare Policy 7(4): 82–94 [PMC free article] [PubMed] [Google Scholar]
- Pathman D.E., Taylor D.H., Konrad T.R., King T.S., Harris T., Henderson T.M., et al. 2000. “State Scholarship, Loan Forgiveness and Related Programs: The Unheralded Safety Net.” Journal of the American Medical Association 284(16): 2084–92 [DOI] [PubMed] [Google Scholar]
- Renner D.M., Westfall J.M., Wilfory L.A., Ginde A.A. 2010. “The Influence of Loan Repayment on Rural Healthcare Provider Recruitment and Retention in Colorado.” Rural and Remote Health 10: 1605–18 [PubMed] [Google Scholar]
- Sempowski I.P. 2004. “Effectiveness of Financial Incentives in Exchange for Rural and Underserviced Area Return-of-Service Commitments: Systematic Review of the Literature.” Canadian Journal of Rural Medicine 9: 82–88 [PubMed] [Google Scholar]
- Simoens S. 2004. “Experiences of Organization for Economic Cooperation and Development Countries with Recruiting and Retaining Physicians in Rural Areas.” Australian Journal of Rural Health 12: 104–11 [DOI] [PubMed] [Google Scholar]
- Statistics Canada. 2011. 2006 Community Profiles. Retrieved December 18, 2012 <http://www12.statcan.gc.ca/census-recensement/2006/dp-pd/prof/92-591/index.cfm?Lang=E>.