Abstract
Objectives:
Amenable mortality is proposed as a health system performance measure, and has been used in comparisons across countries and socio-economic strata. We assess its utility as a health region–level indicator in Canada.
Approach:
We classified all deaths in British Columbia from 2002 to 2009 using two common definitions of amenable mortality. Counts and standardized rates were calculated for 16 health regions. To assess reliability, sensitivity and validity, we compared rates across regions and over time, and examined correlations with premature and all-cause mortality.
Results:
Of the 238,849 deaths in the study period, 6.6% or 13.7% were classified as amenable (depending on the definition used). Rates were stable or falling in more populated regions, but unstable with large confidence intervals elsewhere. Correlation with overall mortality was strong.
Conclusion:
Though amenable mortality is appealing as a feasible, understandable indicator, we question whether it is appropriate for comparisons at a subprovincial level.
Abstract
Objectifs:
La mortalité évitable a été proposée comme mesure du rendement du système de santé, et elle a été utilisée comme moyen de comparaison entre pays ou strates socioéconomiques. Nous évaluons son utilité à titre d'indicateur de la santé à l'échelle des régions sanitaires au Canada.
Démarche:
Nous avons répertorié et classifié toutes les mortalités en Colombie-Britannique, entre 2002 et 2009, selon deux définitions habituelles de la mortalité évitable. Nous avons calculé le nombre et les taux standardisés pour 16 régions sanitaires. Afin d'en évaluer la fiabilité, la sensibilité et la validité, nous avons comparé les taux entre les régions et selon la chronologie, puis nous avons étudié la corrélation entre la mortalité prématurée et la mortalité toutes causes confondues.
Résultats:
Parmi les 238 849 mortalités comptabilisées au cours de la période étudiée, 6,6 % ou 13,7 % ont été classées comme mortalités évitables (dépendamment de la définition utilisée). Les taux étaient stables ou à la baisse dans les régions les plus populeuses, mais instables et à forts intervalles de confiance ailleurs. La corrélation avec la mortalité totale était prononcée.
Conclusion:
Bien que la mortalité évitable semble un indicateur réalisable et compréhensible, nous remettons en question sa pertinence pour les comparaisons à l'échelle infraprovinciale.
There is a clear and ongoing need for better indicators of the effectiveness of healthcare systems. Amenable or avoidable mortality, defined as deaths that, in theory, could be prevented by timely access to good-quality healthcare, is an appealing indicator that bears further empirical scrutiny. It is proposed as a method of measuring the contribution of healthcare to population health, using routinely collected mortality data. It has been used to compare health systems at the levels of nations, provinces or states and across socio-economic strata. We investigate its application at the level of health regions in the Canadian province of British Columbia (BC), where we might expect less dramatic differences in healthcare delivery, and in the context of relatively low mortality.
Background
Health system planners are interested in maximizing the returns on their healthcare investments. Examining geographic and socio-economic variations in healthcare service use and outcomes has the potential to highlight areas where improvements in accessibility, quality or timeliness of care are needed. However, connecting service use to relevant outcomes is easier said than done.
While the use of health services is captured in routinely collected administrative data, corresponding individual- or population-level outcome measures of its effects are harder to come by. Survey data can offer a rich array of potential outcome indicators, but linking these data to actual use of healthcare services is not always possible. In addition, limited numbers, even for large surveys like the Canadian Community Health Survey, can curtail (or eliminate) the ability of survey data to capture small-area variations. Mortality data have the benefit of being routinely collected; as well, they reflect the health status of the entire population. Their chief limitation is that many factors beyond the health system influence mortality rates.
There has been a resurgence in interest in the concept of amenable mortality (CIHI and Statistics Canada 2012; Nolte and McKee 2008, 2011; Tobias and Yeh 2009), defined as deaths that are theoretically preventable with timely access to good-quality healthcare. Classifying a condition as amenable to healthcare is based on a judgment that once the condition has developed, treatment is available that can reasonably be expected to prevent death (Nolte and McKee 2008). This renewed interest in amenable mortality as a healthcare system performance indicator likely comes because such an indicator capitalizes on existing mortality data while appearing to correct for its known limitations.
This concept was first put forth by Rutstein and colleagues (1976), who consulted with an expert panel to compile a list of health conditions from which deaths were considered “untimely and unnecessary.” They describe each death as “a warning signal, a sentinel health event, [indicating] that the quality of care might need to be improved.” This idea of discrete events, each warranting investigation, is not preserved in more recent applications of the concept as a population-level indicator.
Charlton and colleagues (1983) were the first to apply this concept at the population level, selecting 14 disease groups from Rutstein's list for which mortality in a high-income country should be avoidable. Since then, studies have modified the list of health conditions to reflect advances in healthcare, increased the upper age limit for deaths to reflect improved life expectancy and, in some cases, extended the concept to include conditions preventable by public health interventions (which may or may not also be amenable to healthcare). A review of this work, entitled Does Health Care Save Lives?, was published by Nolte and McKee (2004) and included an updated definition of amenable mortality. Research comparing amenable mortality across OECD nations drew renewed attention to this measure in the academic literature (Nolte and McKee 2003, 2008). Expanded lists of amenable causes of death were more recently put forth by an Australian team, Tobias and Yeh (2009) and by a European Union–funded group (Plug et al. 2011).
Amenable mortality has been used in recent health atlases to make comparisons by country and state/territory, and between urban and rural areas, but not at smaller units of analysis, analogous to Canadian health regions (Page et al. 2006; Plug et al. 2011). Early work by Charlton and colleagues (1983) examined variations in deaths from individual conditions considered amenable to medical intervention across health regions of England and Wales, but did not apply a combined indicator of amenable mortality. French and Jones (2006) examined two definitions across British electoral districts, focusing on differences in findings based on the definitions used, but did not explore broader questions of sensitivity and validity in regional analysis.
Up to this point, amenable mortality has been used in only a handful of Canadian studies. Only Pampalon (1993) examined variations at the level of health regions in Quebec, but as with Charlton earlier, he examined individual causes of death, not a composite indicator. Comparisons have also been made by provinces or groups of provinces (James et al. 2006), by urban neighbourhood income quintile (James et al. 2007), by socio-economic status (Wood et al. 1999), by occupation group (Mustard et al. 2010) and by national rates between Canada and other countries (Watson and McGrail 2009). There is growing interest in its use as an indicator to compare across health regions (CIHI and Statistics Canada 2012).
An important consideration affecting the classification of deaths as healthcare-amenable is the age limits (if any) that are used for each cause. For most conditions, only deaths from relevant causes occurring before age 75 are included, the rationale being that at older ages the underlying cause of death becomes more difficult to identify, and the contribution of coexisting health conditions and general frailty increases (Nolte and McKee 2004). This rationale parallels the concept of “premature mortality,” which has been defined as all-cause mortality before age 75 (Wells and Gordon 2008). The choice of 75 as the age cut-off is essentially arbitrary and does not imply that some deaths among those aged 75 years and older could not also be avoided. It means, however, that amenable mortality rates by definition are likely to track all-cause premature mortality rates closely, particularly in areas where deaths from injury or violence are not exceptionally high. This prompts the question of whether amenable mortality actually provides more information (or measures something different) than premature all-cause mortality (hereafter called simply “premature mortality”).
Our interest is in assessing whether amenable mortality is a potentially useful indicator of regional health system performance in Canada. In doing so, we pay particular attention to whether rates of amenable mortality are stable over time and across regions, and whether this measure is an improvement over premature mortality in capturing regional health system performance. We apply both the Nolte and McKee (2004) and Tobias and Yeh (2009) definitions.
Approach
We used data on all deaths that occurred in British Columbia, and their underlying causes, from 2002 to 2009, obtained from BC Vital Statistics. We excluded 681 deaths occurring in the study period that were missing patient location information. Each death was classified as amenable or not, using the two definitions of amenable mortality and ICD-10 codes (see Appendix 1). These definitions are largely similar in the conditions they list, though Nolte and McKee (2004) include maternal deaths, misadventures during surgical and medical care, and a wider range of (rare) infectious diseases; they exclude melanoma of the skin, bladder cancer, thyroid cancer and respiratory diseases past age 14. Nolte and McKee also limit deaths from diabetes in patients younger than 50, while Tobias and Yeh (2009) include 50% of deaths under age 75.
Counts and rates were calculated at the level of Health Service Delivery Area (HSDA), the unit at which national health indicators are reported (CIHI and Statistics Canada 2012). British Columbia's 16 HSDAs are nested in five geographic health regions and had populations ranging from 67,962 (Northeast) to 696,896 (Fraser South) in 2009. Rates were standardized to the 2009 age and sex distribution of the province. We used a binomial distribution to estimate standard error and construct 95% confidence intervals.
In planning our analysis, we considered criteria for the evaluation of health indicators put forth by the Institute of Medicine (Field and Gold 1998). These state that a measure is reliable if repeated use under identical circumstances by the same or different users produces the same results. A measure is deemed sensitive or responsive if it can detect differences or changes in population characteristics that are of interest to its users. To assess these criteria, we examined stability of rates in three time periods (2002–5, 2004–7 and 2006–9) within HSDAs and variations in rates across 16 HSDAs, as well as the associated 95% confidence intervals for each estimate.
A measure is valid if it measures the properties, qualities or characteristics it is intended to measure. As amenable mortality is intended to reflect timely access to good-quality healthcare, but not determinants of health outside the health system, patterns should differ from those seen for all-cause and premature mortality. We examined correlations between amenable mortality (using both definitions) and both all-cause premature and overall mortality.
A measure is acceptable if its intended users find it understandable, credible and useful for their purposes. Provided it meets the other criteria, amenable mortality is readily understandable and responds to a clear need for indicators of health system performance, and would therefore be acceptable. A measure is feasible if users can collect the necessary data and perform the required analyses without imposing excessive burdens. As amenable mortality is based on routinely collected mortality data, it is very feasible. Finally, a measure is universal or flexible if it is adaptable to the variability of problems, populations, settings or purposes that face potential users. Because it uses ICD-10 codes, and is based on only “widely available treatments,” amenable mortality should be adaptable to multiple settings. No analyses were undertaken to assess these latter criteria.
Results and Discussion
Of the 238,849 deaths occurring in British Columbia in the study period with known location of death, 89,707, or 37.6%, occurred before age 75. The proportion of deaths considered
amenable varies by definition used, with Tobias and Yeh's definition classifying 13.7% of all deaths and 36.7% of premature deaths as amenable, and Nolte and McKee classifying only 6.6% of all deaths and 17.6% of premature deaths as amenable (Table 1). The larger number of deaths included in Tobias and Yeh's definition was driven by wider age ranges for diabetes, respiratory disease and uterine cancers (see Appendix 1). Rates were markedly higher for men than for women, a finding that is consistent across studies (James et al. 2006, 2007; Mustard et al. 2010; Nolte and McKee 2008; Tobias and Yeh 2009).
TABLE 1A.
Counts of all-cause, premature and amenable mortality, using definitions from Nolte and McKee 2004 (N&M) and Tobias and Yeh 2009 (T&Y), British Columbia, 2002–9
| Health Service Delivery Area | 2009 | Average Annual Number of Deaths | |||
|---|---|---|---|---|---|
| Females | Population | All causes | Premature | N&M | T&Y |
| East Kootenay | 39,996 | 274 | 87 | 16 | 39 |
| Kootenay Boundary | 39,775 | 348 | 103 | 16 | 42 |
| Okanagan | 179,430 | 1,533 | 408 | 81 | 182 |
| Thompson Cariboo | 111,678 | 788 | 299 | 56 | 112 |
| Fraser East | 139,748 | 949 | 294 | 63 | 132 |
| Fraser North | 300,530 | 1,658 | 489 | 113 | 221 |
| Fraser South | 350,060 | 1,948 | 602 | 142 | 274 |
| Richmond | 99,046 | 443 | 122 | 30 | 58 |
| Vancouver | 323,836 | 1,812 | 479 | 105 | 205 |
| North Shore/Coast Garibaldi | 141,671 | 956 | 248 | 56 | 113 |
| South Vancouver Island | 190,157 | 1,678 | 384 | 83 | 189 |
| Central Vancouver Island | 132,621 | 1,104 | 347 | 74 | 151 |
| North Vancouver Island | 60,371 | 396 | 141 | 27 | 58 |
| Northwest | 36,610 | 180 | 88 | 18 | 30 |
| Northern Interior | 70,006 | 368 | 167 | 31 | 60 |
| Northeast | 32,658 | 133 | 59 | 13 | 23 |
| British Columbia | 2,248,193 | 14,567 | 4,317 | 923 | 1,889 |
| Males | Population | All causes | Premature | N&M | T&Y |
| East Kootenay | 40,118 | 309 | 146 | 19 | 46 |
| Kootenay Boundary | 39,633 | 374 | 171 | 25 | 56 |
| Okanagan | 172,008 | 1,677 | 655 | 92 | 230 |
| Thompson Cariboo | 111,653 | 937 | 496 | 71 | 154 |
| Fraser East | 140,612 | 1,033 | 472 | 70 | 162 |
| Fraser North | 296,897 | 1,646 | 742 | 119 | 247 |
| Fraser South | 346,836 | 1,960 | 880 | 149 | 288 |
| Richmond | 94,459 | 422 | 180 | 30 | 60 |
| Vancouver | 319,425 | 1,881 | 903 | 142 | 274 |
| North Shore/Coast Garibaldi | 136,667 | 909 | 370 | 60 | 123 |
| South Vancouver Island | 177,888 | 1,544 | 548 | 79 | 193 |
| Central Vancouver Island | 129,190 | 1,205 | 526 | 77 | 168 |
| North Vancouver Island | 60,104 | 467 | 244 | 33 | 72 |
| Northwest | 38,548 | 257 | 158 | 23 | 41 |
| Northern Interior | 72,757 | 485 | 293 | 42 | 83 |
| Northeast | 35,304 | 184 | 113 | 17 | 32 |
| British Columbia | 2,212,099 | 15,289 | 6,896 | 1,047 | 2,230 |
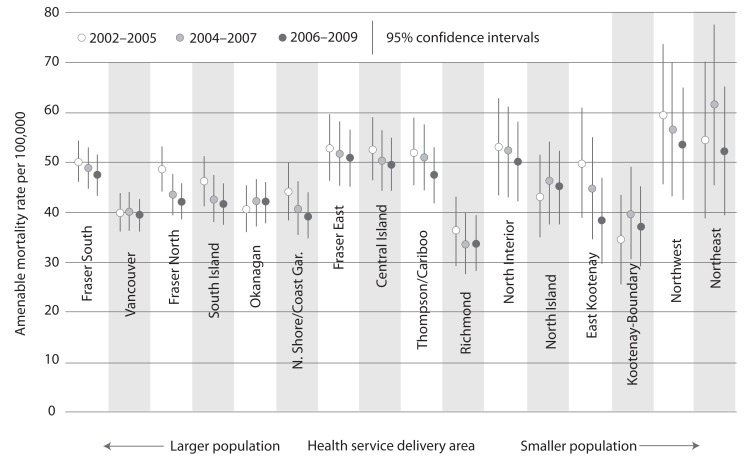
Examining counts by HSDA and year reveals that for all but three HSDAs, sex-specific rates for the Nolte and McKee definitions are based on fewer than 100 deaths (Table 1). These small numbers are reflected in very large confidence intervals (Table 1 and Figure 1). When four years of data are pooled (2002–5, 2004–7, 2006–9), rates are stable or trend downward in more populated regions (Vancouver, Richmond, Fraser North and South, South Vancouver Island), but have large confidence intervals and fluctuate considerably in more remote regions (East Kootenay, North Vancouver Island and the northern HSDAs) (Figure 1). Only rates for females are graphed, but findings were similar for males. These results suggest that for smaller health regions, amenable mortality would be reliable only if several years of data were pooled, and is therefore sensitive only to changes over long time periods.
TABLE 1B.
Rates of all-cause, premature and amenable mortality, using definitions from Nolte and McKee 2004 (N&M) and Tobias and Yeh 2009 (T&Y), British Columbia, 2002–9
| Health Service Delivery Area | Deaths per 100,000, Age Standardized to the 2009 BC Population | |||
|---|---|---|---|---|
| Females | All causes | Premature | N&M | T&Y |
| East Kootenay | 655 (628, 681) | 233 (216, 250) | 43 (35, 50) | 72 (63, 82) |
| Kootenay Boundary | 697 (672, 722) | 256 (238, 273) | 39 (32, 46) | 69 (60, 79) |
| Okanagan | 640 (629, 651) | 229 (221, 237) | 46 (42, 49) | 69 (65, 73) |
| Thompson Cariboo | 730 (712, 747) | 281 (270, 292) | 52 (48, 57) | 81 (75, 87) |
| Fraser East | 676 (661, 691) | 259 (248, 269) | 56 (51, 61) | 85 (79, 91) |
| Fraser North | 622 (612, 632) | 214 (207, 220) | 49 (45, 52) | 71 (67, 75) |
| Fraser South | 634 (624, 644) | 221 (215, 227) | 52 (49, 55) | 76 (72, 80) |
| Richmond | 491 (475, 507) | 153 (143, 163) | 37 (32, 42) | 50 (45, 56) |
| Vancouver | 551 (542, 560) | 191 (185, 197) | 42 (39, 45) | 59 (56, 63) |
| North Shore/Coast Garibaldi | 596 (583, 609) | 193 (185, 202) | 44 (40, 48) | 63 (58, 68) |
| South Vancouver Island | 602 (591, 612) | 221 (214, 229) | 48 (44, 51) | 70 (66, 75) |
| Central Vancouver Island | 674 (660, 688) | 260 (250, 270) | 55 (50, 59) | 79 (74, 84) |
| North Vancouver Island | 676 (653, 698) | 248 (233, 262) | 48 (41, 54) | 73 (65, 80) |
| Northwest | 742 (704, 781) | 302 (280, 325) | 61 (51, 71) | 89 (77, 101) |
| Northern Interior | 781 (753, 809) | 297 (281, 313) | 56 (49, 63) | 84 (76, 93) |
| Northeast | 740 (696, 784) | 268 (244, 293) | 58 (46, 69) | 84 (70, 98) |
| British Columbia | 648 | 192 | 41 | 84 |
| Males | All causes | Premature | N&M | T&Y |
| East Kootenay | 930 (893, 966) | 383 (361, 405) | 49 (41, 57) | 85 (74, 95) |
| Kootenay Boundary | 1,014 (978, 1,049) | 429 (406, 452) | 62 (54, 71) | 100 (89, 111) |
| Okanagan | 943 (928, 959) | 395 (384, 406) | 54 (50, 57) | 88 (83, 93) |
| Thompson Cariboo | 1,024 (1,001, 1,048) | 458 (444, 472) | 65 (59, 70) | 104 (98, 111) |
| Fraser East | 971 (951, 991) | 428 (414, 441) | 64 (59, 69) | 108 (101, 115) |
| Fraser North | 908 (892, 923) | 335 (327, 344) | 55 (51, 58) | 86 (82, 91) |
| Fraser South | 886 (872, 899) | 333 (325, 341) | 57 (54, 60) | 85 (81, 89) |
| Richmond | 669 (646, 691) | 241 (229, 254) | 41 (36, 46) | 63 (57, 70) |
| Vancouver | 841 (828, 854) | 369 (360, 377) | 59 (56, 63) | 91 (87, 95) |
| North Shore/Coast Garibaldi | 819 (801, 838) | 303 (292, 314) | 49 (45, 54) | 75 (69, 80) |
| South Vancouver Island | 875 (860, 890) | 344 (334, 354) | 49 (46, 53) | 81 (76, 86) |
| Central Vancouver Island | 945 (927, 964) | 404 (391, 416) | 57 (53, 62) | 92 (86, 98) |
| North Vancouver Island | 979 (947, 1,011) | 420 (401, 438) | 56 (50, 63) | 89 (81, 98) |
| Northwest | 1,098 (1,046, 1,149) | 485 (458, 512) | 72 (61, 82) | 107 (94, 120) |
| Northern Interior | 1,097 (1,060, 1,133) | 482 (463, 502) | 70 (62, 77) | 116 (106, 126) |
| Northeast | 1,087 (1,027, 1,147) | 472 (441, 503) | 72 (60, 85) | 114 (98, 130) |
| British Columbia | 691 | 312 | 47 | 101 |
FIGURE 1.
Amenable mortality rates (Nolte and McKee) among females, by Health Service Delivery Areas, 2002–9, age-standardized to the 2009 BC population
Differences were observed between mortality rates for urban and suburban areas of the lower mainland (e.g., Richmond, Vancouver, Fraser North) and the much higher rates in the HSDAs of Northern Health Region. Beyond these differences between north–south and urban–rural, differences were not apparent among HSDAs within health regions or with similar geographic and socio-economic characteristics.
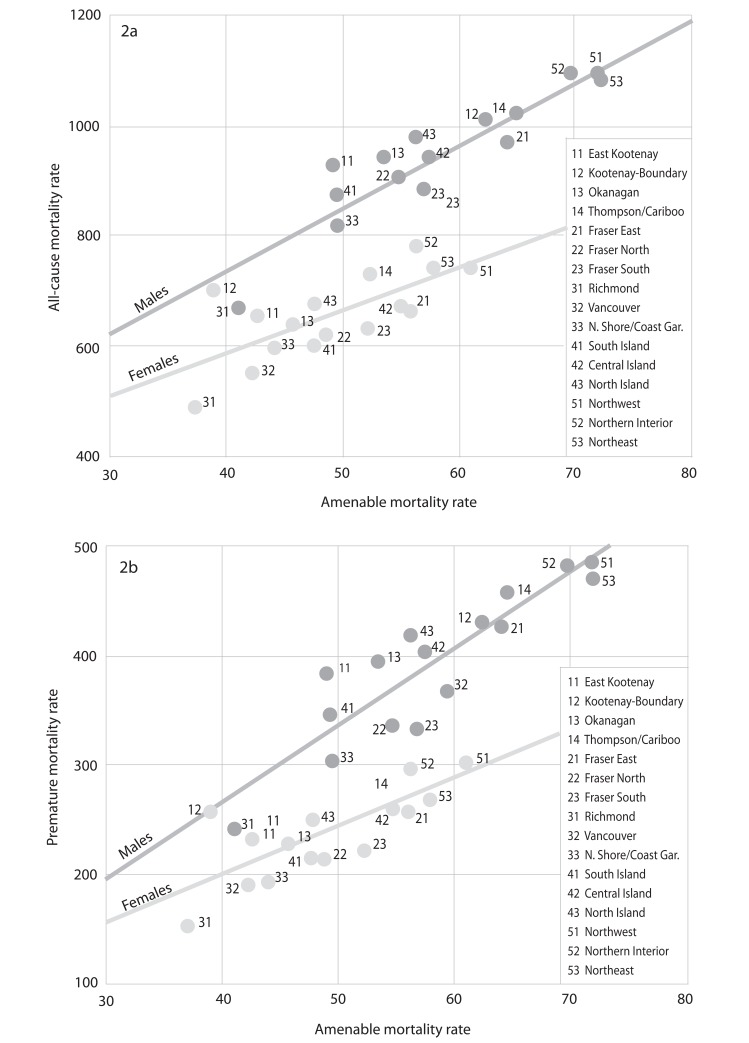
Figure 2 depicts the relationship between Nolte and McKee's definition of amenable mortality and both all-cause and premature mortality by sex, using age-standardized rates for all study years combined (2002–9). Correlation coefficients with all-cause mortality are 0.73 (females) and 0.89 (males), rising to 0.77 and 0.90, respectively, for premature mortality. When Tobias and Yeh's definition was used, correlations were even stronger for both all-cause (0.09 female, 0.92 male) and premature mortality (0.93 female, 0.94 male), consistent with the fact that a higher proportion of deaths were classified as amenable. The results of correlations using Tobias and Yeh's definition are not graphed, but show even fewer off-diagonal points. Correlations were generally stronger for men than for women, and were highly significant in all cases (p<0.0001).
FIGURE 2.
Correlation between amenable mortality rates (Nolte and McKee) and all-cause mortality (F=0.73, M=0.89) (2a), premature mortality (F=0.77, M=0.90), age-standardized to the 2009 BC population (2b)
These very strong correlations call into question the validity of amenable mortality as a measure of regional health system performance. More importantly, it does not appear that the points that fall farthest from the line of best fit provide additional useful information. For example, in the plots for amenable mortality and all-cause mortality for both definitions, Vancouver falls off the diagonal line, indicating higher than expected amenable mortality relative to overall mortality. Vancouver has a high physician-to-population ratio and is a tertiary care centre. At the same time, Vancouver's Downtown Eastside is well known to have a very high incidence of poverty, drug use, crime and violence. It is far more likely that Vancouver's off-diagonal position is driven by these social determinants of health than by any (relative) difference in performance of the healthcare system.
While intended as an improvement over all-cause and premature mortality, which are limited in their ability to attribute deaths to the failure of healthcare systems, it seems unlikely that amenable mortality is capturing something fundamentally different, regardless of the definition used. While there is some promise that this indicator is sensitive to broad system changes (Desai et al. 2011; Lee et al. 2010), questions remain related to confounding by concurrent socio-economic changes. Our analysis suggests that, at the very least, amenable mortality is not sensitive to more subtle regional variations in health services, a finding that is perhaps not surprising in a Canadian provincial health system.
Nolte and McKee emphasize that amenable mortality is proposed only as an initial screen of health system performance, ideally in combination with other indicators. It may identify possible health system problems, but more detailed investigation is needed to understand their source (i.e., examining the conditions included to determine which may be responsible for observed high rates). Unfortunately (or fortunately), at the level of health region, numbers are insufficient, for many causes of death, to delve into this analysis. National-level analysis has paid particular attention to outliers, or has compared countries with similar rates of all-cause, premature or potential life years lost, but these differ in terms of amenable mortality. However, apart from the Vancouver example, there are no HSDAs that are consistently off-diagonal, and therefore no opportunities for such investigation. And as discussed, the identification of Vancouver is not a surprise, is unlikely to be related to health system performance and, thus, provides no new information.
In addition to the above-mentioned limitations, and despite the widespread (and still growing) interest, only a small subset of research has examined the association between amenable mortality and health services supply or use. These studies show weak or inconsistent associations (Mackenbach et al. 1990; Pampalon 1993) and in some cases fail to control appropriately for confounding by socio-economic factors (Buck and Bull 1986). Importantly, these studies examined quantity, not quality, of health services used. If regional variation in amenable mortality appears to be more closely related to socio-economic rather than health system factors, this may still suggest barriers to timely access to care, independent of available supply (Nolte and McKee 2004). To fully assess the validity of this measure, further research must examine the extent to which deaths classified as amenable actually reflect the absence of timely access to good-quality healthcare.
Conclusion
Though amenable mortality is appealing as a feasible, easily understandable indicator of health system performance, we question whether it is an appropriate indicator for comparing health system performance across regions in a single province or country. Its exceptionally strong correlation with broader mortality measures suggests that it is not, in fact, specifically capturing health system performance. If amenable mortality and premature mortality are effectively measuring the same thing, researchers and decision-makers interested in regional analyses will be better off using premature mortality, which has a higher rate and is more stable over time. If misapplied and misinterpreted, the use of amenable mortality has the potential to focus unwarranted attention on places that may in fact be providing high-quality care, while distracting from factors outside the healthcare system that contribute to marked and persistent health inequities.
Appendix
APPENDIX 1.
Definitions of amenable mortality from Nolte and McKee 2004, Tobias and Yeh 2009
| Cause of Death | Nolte and McKee | Tobias and Yeh | ||
|---|---|---|---|---|
| Age | ICD-10 Codes | Age | ICD-10 Codes | |
| Intestinal infection | 0–14 | A00–A09 | ||
| Tuberculosis | 0–74 | A15–9, B90 | 0–74 | A15–9, B90 |
| Diphtheria | 0–74 | A36 | ||
| Whooping cough | 0–14 | A37 | ||
| Tetanus | 0–74 | A35 | ||
| Septicemia | 0–74 | A40–A41 | 0–74 | A40–A41 |
| Poliomyelitis | 0–74 | A80 | ||
| Measles | 1–14 | B05 | ||
| Other infections | 0–74 | A38, A39, A46, A48.1, B50–54, G00, G03, L03 | ||
| Melanoma of skin | 0–74 | C43 | ||
| Non-melanomic skin cancer | 0–74 | C44 | 0–74 | C44 |
| Breast cancer | 0–74 | C50 | 0–74 | C50 |
| Cervical cancer | 0–74 | C53 | 0–74 | C53 |
| Uterine cancer | 0–44 | C54, C55 | 0–74 | C54, C55 |
| Colorectal cancer | 0–74 | C18–21 | 0–74 | C18–21 |
| Testicular cancer | 0–74 | C62 | ||
| Bladder cancer | 0–74 | C67 | ||
| Thyroid cancer | 0–74 | C73 | ||
| Hodgkins' disease | 0–74 | C81 | 0–74 | C81 |
| Leukaemia | 0–44 | C91–C95 | 0–44 | C91–C95 |
| Benign tumours | 0–74 | D10–D36 | ||
| Thyroid disorders | 0–74 | E00–E07 | 0–74 | E00–E07 |
| Diabetes mellitus | 0–49 | E10–E14 | 0–74 | E10–E14 (50% of cases) |
| Epilepsy | 0–74 | G40–G41 | 0–74 | G40–G41 |
| Rheumatic fever and chorea | 0–74 | I01–I04 | ||
| Chronic rheumatic heart disease | 0–74 | I05–I09 | 0–74 | I05–I09 |
| Hypertensive disease | 0–74 | I10–I13, I15 | 0–74 | I11–I13 |
| Ischaemic heart disease | 0–74 | I20–I25 (50% of cases) | 0–74 | I20–I25 (50% of cases) |
| Cerebrovascular disease | 0–74 | I60–I69 | 0–74 | I60–I69 (50% of cases) |
| All other respiratory diseases | 1–14 | J00–J09, J20–J39, J47–J99 | 0–74 | J02.00 |
| COPD | 1–14 | J40–J44 | 44+ | J40–J44 |
| Asthma | 1–14 | J45–J46 | 0–44 | J45–J46 |
| Influenza | 0–74 | J10–J11 | ||
| Pneumonia | 0–74 | J12–J18 | 0–74 | J13–15, J18 |
| Peptic ulcer | 0–74 | K25–K27 | 0–74 | K25–K28 |
| Appendicitis | 0–74 | K35–K38 | 0–74 | K35–K38 |
| Abdominal hernia | 0–74 | K40–K46 | 0–74 | K40–K46 |
| Cholelithiasis, cholecystitis (and cholangitis) | 0–74 | K80–K81 | 0–74 | K80–K81 |
| Pancreatitis, hernia | 0–74 | K82–K83, K85–K86, K91.5 | ||
| Nephritis and nephrosis | 0–74 | N00–N07, N17–N19, N25–N27 | 0–74 | N00–N09, N17–N19 |
| Benign hyperplasia of the prostate | 0–74 | N40 | 0–74 | N40 |
| Obstructive uropathy | 0–74 | N13, N20–N21, N35, N99.1 | ||
| Maternal death (all causes) | All | O00–O99 | ||
| Congenital anomalies | 0–74 | Q20–Q28 | 0–74 | Q00–Q99, H31.1 |
| Perinatal conditions | All | P00–P96, A33, A34 | 0–74 | P00, P03–P95 |
| Misadventures to patients during surgical and medical care | All | Y60–Y69, Y83–Y84 | ||
Contributor Information
M. Ruth Lavergne, Doctoral Candidate, Centre for Health Services and Policy Research, School of Population and Public Health, University of British Columbia, Vancouver, BC.
Kimberlyn McGrail, Assistant Professor, Centre for Health Services and Policy Research, School of Population and Public Health, University of British Columbia, Vancouver, BC.
REFERENCES
- Buck C., Bull S. 1986. “Preventable Causes of Death versus Infant Mortality as an Indicator of the Quality of Health Services.” International Journal of Health Services: Planning, Administration, Evaluation 16(4): 553–63 [DOI] [PubMed] [Google Scholar]
- Canadian Institute for Health Information (CIHI) and Statistics Canada. 2012. Health Indicators 2012. Ottawa: CIHI [Google Scholar]
- Charlton J., Silver R., Hartley R., Holland W.W. 1983. “Geographical Variation in Mortality from Conditions Amenable to Medical Intervention in England and Wales.” Lancet 321(8326): 691–96 [DOI] [PubMed] [Google Scholar]
- Desai M., Nolte E., Karanikolos M., Khoshaba B., McKee M. 2011. “Measuring NHS Performance 1990–2009 Using Amenable Mortality: Interpret with Care.” Journal of the Royal Society of Medicine 104(9): 370–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field M.J., Gold M.R. 1998. Summarizing Population Health: Directions for the Development and Application of Population Metrics. Washington, DC: National Academy Press; Retrieved December 17, 2012 <http://faculty.washington.edu/samclark/CSDE555/Syllabus/Readings/all/field%20and%20gold_summarizing%20population%20health.pdf>. [PubMed] [Google Scholar]
- French K.M., Jones K. 2006. “Impact of Definition on the Study of Avoidable Mortality: Geographical Trends in British Deaths 1981–1998 Using Charlton and Holland's Definitions.” Social Science and Medicine 62(6): 1443–56 [DOI] [PubMed] [Google Scholar]
- James P.D., Manuel D.G., Mao Y. 2006. “Avoidable Mortality across Canada from 1975 to 1999.” BMC Public Health 6: 137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James P.D., Wilkins R., Detsky A.S., Tugwell P., Manuel D.G. 2007. “Avoidable Mortality by Neighbourhood Income in Canada: 25 Years After the Establishment of Universal Health Insurance.” Journal of Epidemiology and Community Health 61(4): 287–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y.C., Huang Y.T., Tsai Y.W., Huang S.M., Kuo K.N., McKee M., et al. 2010. “The Impact of Universal National Health Insurance on Population Health: The Experience of Taiwan.” BMC Health Services Research 10: 225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenbach J.P., Bouvier-Colle M.H., Jougla E. 1990. “Avoidable Mortality and Health Services: A Review of Aggregate Data Studies.” Journal of Epidemiology and Community Health 44(2): 106–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustard C.A., Bielecky A., Etches J., Wilkins R., Tjepkema M., Amick B.C., et al. 2010. “Avoidable Mortality for Causes Amenable to Medical Care by Occupation in Canada, 1991–2001.” Canadian Journal of Public Health 101(6): 500–06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolte E., McKee M. 2003. “Measuring the Health of Nations: Analysis of Mortality Amenable to Health Care.” British Medical Journal 327(7424): 1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolte E., McKee M. 2004. Does Health Care Save Lives? Avoidable Mortality Revisited. London: Nuffield Trust London; Retrieved December 17, 2012 <http://www.nuffieldtrust.org.uk/sites/files/nuffield/publication/does-healthcare-save-lives-mar04.pdf>. [Google Scholar]
- Nolte E., McKee M. 2008. “Measuring the Health of Nations: Updating an Earlier Analysis.” Health Affairs 27(1): 58–71 [DOI] [PubMed] [Google Scholar]
- Nolte E., McKee M. 2011. “Variations in Amenable Mortality Trends in 16 High-Income Nations.” Health Policy 103(1): 47–52 [DOI] [PubMed] [Google Scholar]
- Page A., Tobias M., Glover J.D., Wright C., Hetzel D.M., Fisher E.J. 2006. “Australian and New Zealand Atlas of Avoidable Mortality.” Adelaide: Public Health Information Development Unit and New Zealand Ministry of Health; Retrieved December 17, 2012 <http://www.publichealth.gov.au/pdf/atlases/avoid_mortality_aust_2006/avoid_mortality_ch1_intro.pdf>. [Google Scholar]
- Pampalon R. 1993. “Avoidable Mortality in Québec and Its Regions.” Social Science and Medicine 37(6): 823–31 [DOI] [PubMed] [Google Scholar]
- Plug I., Hoffmann R., Mackenbach J. 2011. Avoidable Mortality in the European Union: Volume 1: Final Report. EU Public Health Program. Retrieved December 17, 2012 <http://amiehs.lshtm.ac.uk/publications/reports/AMIEHS%20final%20report%20VOL%20I.pdf>.
- Rutstein D.D., Berenberg W., Chalmers T.C., Child C.G., Fishman A.P., Perrin E.B. 1976. “Measuring the Quality of Medical Care. A Clinical Method.” New England Journal of Medicine 294(11): 582–88 [DOI] [PubMed] [Google Scholar]
- Tobias M., Yeh L.C. 2009. “How Much Does Health Care Contribute to Health Gain and to Health Inequality? Trends in Amenable Mortality in New Zealand 1981–2004.” Australian and New Zealand Journal of Public Health 33(1): 70–78 [DOI] [PubMed] [Google Scholar]
- Watson D., McGrail K.M. 2009. “More Doctors or Better Care?” Healthcare Quarterly 12(4): 101–04 [DOI] [PubMed] [Google Scholar]
- Wells C., Gordon E. 2008. “Geographical Variations in Premature Mortality in England and Wales, 1981–2006.” Health Statistics Quarterly 38: 6–18 [PubMed] [Google Scholar]
- Wood E., Sallar A.M., Schechter M.T., Hogg R.S. 1999. “Social Inequalities in Male Mortality Amenable to Medical Intervention in British Columbia.” Social Science and Medicine 48(12): 1751–58 [DOI] [PubMed] [Google Scholar]