Abstract
Mycophenolate mofetil (MMF) is a commonly used drug in the prevention of allograft rejection in patients with solid organ transplants. Although diffuse colitis has been described in MMF-related colitis, segmental colitis has not been reported. We report the case of a 64-year-old male on MMF therapy who presented for evaluation of afebrile diarrhea and abdominal pain. Flexible sigmoidoscopy revealed a segmental erythematous mucosa with ulceration in the sigmoid colon, descending colon, splenic flexure and proximal transverse colon. Biopsies of these areas showed dilated damaged crypts, eosinophilic epithelial changes and crypt abscesses with apoptotic bodies consistent with MMF-induced injury. MMF was discontinued, leading to a significant improvement of his symptoms.
Key Words: Segmental colitis, Mycophenolate mofetil, Apoptosis, Ischemic colitis
Introduction
The increase in the incidence of solid organ transplantation has led to the need for highly potent immunosuppressive drugs for the prevention of allograft rejection and autoimmune conditions. Mycophenolate mofetil (MMF or CellCept) is commonly used for maintenance of immunosuppression and the treatment of ongoing rejection in organ transplant patients [1]. Its effectiveness is comparable to other immunosuppressive agents such as tacrolimus, cyclosporine and azathioprine, yet it holds a lower toxicity profile, making it an attractive alternative agent in allograft rejection [2]. Gastrointestinal mucosal injuries related to MMF use are common and include those related to suppression of immune function (infectious) and effects due to drug interaction and metabolism (suppression of de novo purine synthesis) [3]. Afebrile diarrhea is the most frequently reported primary manifestation of toxicity related to MMF, with an incidence in renal transplant patients ranging from 12 to 40% [4].
While diffuse colitis has been described as a typical endoscopic feature of MMF use, its presentation as segmental colitis is unknown. We report the rare case of segmental colitis in a patient with autoimmune autonomic dysfunction treated with MMF. Our patient presented unusually with abdominal pain and diarrhea after a recent increase of his MMF dose.
Case Report
A 64-year-old gentleman with a history of autoimmune autonomic dysfunction and gastroparesis on a background of type 2 insulin-dependent diabetes mellitus presented to our hospital with abdominal pain and diarrhea. He did not have any history of coronary artery disease or other cardiovascular comorbidities. The patient was initially started on MMF 1,000 mg twice daily 2 years prior for autoimmune autonomic dysfunction. This was subsequently raised to 1,500 mg twice daily 4 months preceding the patient's presentation. The diarrhea had started 2 months prior to presentation, with up to eight episodes of non-bloody diarrhea per day. Abdominal pain was of recent onset with a 4-day history of lower abdominal stabbing pain most severe in the left lower quadrant and reported as constant and progressive in nature. He also had decreased appetite, weight loss, sensation of bloating and intermittent nausea. He did not have any history of coronary artery disease or other cardiovascular comorbidities. The patient had undergone esophagogastroduodenoscopy within the past year, which had been unremarkable. A colonoscopy 5 years prior had shown diverticulosis, but otherwise been normal.
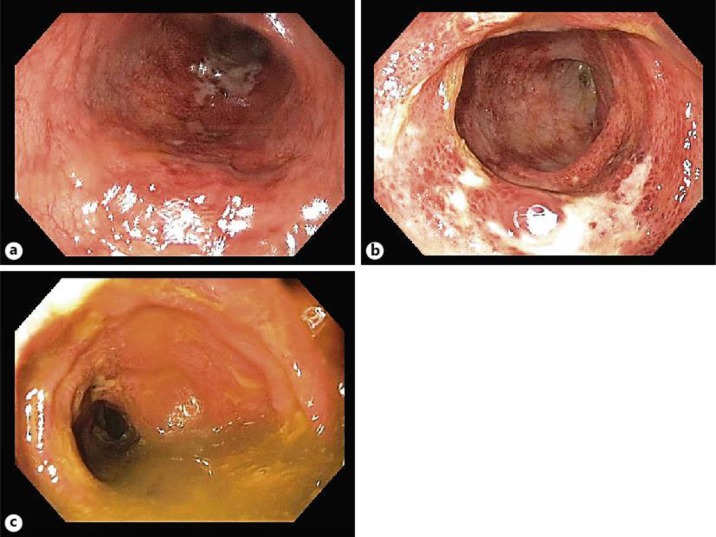
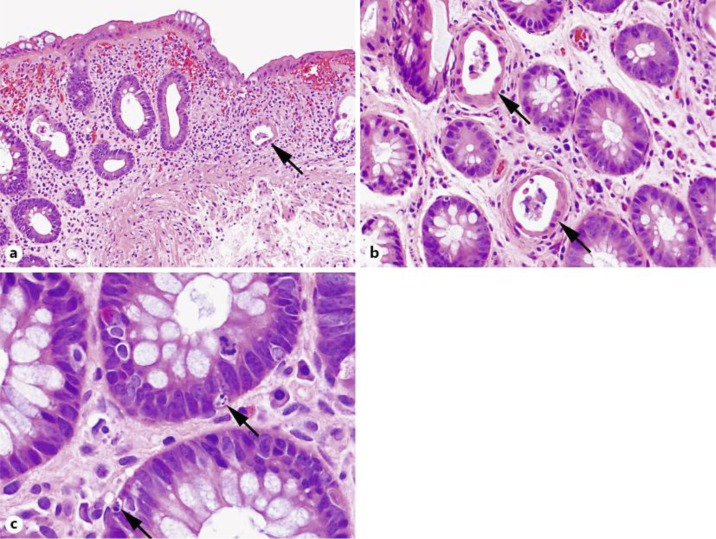
On examination, his vital signs were normal, and he had diffuse abdominal tenderness with increased intensity in the left lower quadrant area. Initial investigations revealed an elevated white blood cell count of 17.9 × 109 cells/l (normal 3.5–10.5 × 109 cells/l) with normal hemoglobin and platelet count. An elevated creatinine of 1.8 mg/dl (normal 0.6–1.2 mg/dl) was also noted. Abdominal X-ray showed no obstruction. Stool examination for microbiology including Clostridium difficile was negative. Initial management included hydration with intravenous fluids, empiric antibiotics and analgesia. Further work-up with CT of the abdomen and pelvis with contrast revealed segmental wall thickening and pericolic inflammation at the splenic flexure and proximal descending colon without evidence of diverticulitis. Flexible sigmoidoscopy revealed a segmental erythematous mucosa and multiple ulcers in the sigmoid colon, descending colon, splenic flexure and proximal transverse colon, suggesting a mucosal injury pattern consistent with ischemic colitis (fig. 1). However, biopsies showed dilated damaged crypts, eosinophilic epithelial changes and crypt abscesses with apoptotic bodies, a pattern of injury highly suggestive of MMF-related colitis (fig. 2). There was no evidence of cytomegalovirus infection.
Fig. 1.
Sigmoidoscopy showing erythematous mucosa with ulceration in the sigmoid (a), descending colon, splenic flexure (b) and proximal transverse colon (c).
Fig. 2.
a The colonic mucosa showed abnormal architecture with unevenly spaced and distorted crypts, features likened to changes seen in inflammatory bowel disease. A withered crypt composed of epithelial cells with eosinophilic change was present (arrow). Hematoxylin and eosin, original magnification 200×. b Individual dilated, damaged crypts were present, scattered throughout the mucosa (arrows). Note the cytoplasmic eosinophilic change and the luminal debris. Hematoxylin and eosin, original magnification 400×. c Subtle background apoptotic bodies (arrows) were present in increased numbers, indicating cellular injury and turnover. Hematoxylin and eosin, original magnification 400×.
MMF therapy was subsequently discontinued and the patient was discharged following improvement of symptoms with follow-up in an outpatient clinic 5 weeks later. During this visit, his abdominal pain and diarrhea had improved rapidly and significantly. He is scheduled for a repeat colonoscopy in 4 months’ time to assess the extent of mucosa recovery.
Discussion
While the diffuse pattern of mucosal injury with MMF use has been described previously, segmental mucosal injury similar to ischemic colitis has not been reported to date. Our case is interesting due to the fact that despite endoscopic appearance of ischemic colitis in a segmental fashion, histology did not show any changes suggestive of ischemia, but rather suggested MMF-related injury, which was confirmed by resolution of symptoms following discontinuation of the offending agent.
The hallmark for the diagnosis of MMF-related colitis is increased epithelial cell apoptosis, which can be accompanied by an inflammatory bowel disease-like histological pattern [5]. Complicating the diagnosis is the similarity of this pattern to acute intestinal graft-versus-host disease [6] and inflammatory bowel disease, and diagnostic distinction is critical in these patients, as MMF-related colitis is managed with reduction in dosage, while graft-versus-host disease and inflammatory bowel disease should be managed with immunosuppression, such as MMF. Several histological features suggestive of MMF injury include crypt architectural disarray, lamina propria edema, increased lamina propria inflammation, dilated damaged crypts and increased crypt epithelial apoptosis [7].
In addition to preventing allograft rejection, MMF is also used to treat autoimmune conditions, including psoriasis, rheumatoid arthritis and autoimmune uveoretinitis [8]. MMF is converted to mycophenolic acid, which non-competitively inhibits the inosine monophosphate dehydrogenase enzymes required for purine synthesis in B and T lymphocytes. This subsequently causes a reduction in humoral and cytotoxic T cell response to immunogenic stimuli [9].
Although the exact pathogenesis is unknown, gastrointestinal mucosal injury is thought to occur due to insult of enterocytes and the formation of toxic immunogenic reactions in the bowel [10]. Enterocyte damage arises as 50% of these cells use the inosine monophosphate dehydrogenase pathway for de novo purine metabolism [11]. Increased incidence of duodenal villous atrophy [12] has been reported with chronic MMF use, and injury via infective etiologies due to immunosuppression may also occur in addition to MMF-related colitis. However, the mechanism for segmental mucosal injury, as seen in our case, is not clear. We speculate that the disease process begins as a segmental colitis, as seen in our case, and then progresses to diffuse colitis, as reported in previous studies.
Clinically, MMF-related colitis commonly manifests as chronic diarrhea unresponsive to antibiotics or steroid therapy, with improvement of symptoms following reduction or cessation of MMF [13]. Other presenting symptoms may include nausea, vomiting, abdominal colic, gastritis, gastric ulcers and intestinal perforation [14]. Symptoms may require 1– 6 months for resolution following cessation of MMF [15]. Patients with poor responses 6 months following discontinuation of therapy may require other alternative strategies, including surgical intervention for curative treatment [15].
Conclusion
In summary, MMF-induced segmental colitis is an uncommon but important clinical condition in patients presenting with chronic diarrhea. Clinical features and histology are helpful in differentiating this condition from ischemic colitis. Early recognition of this entity along with discontinuation of MMF may result in improved clinical outcome.
Disclosure Statement
There are no conflicts of interest to disclose and no funding sources to report.
References
- 1.Allison AC, Eugui EM. Purine metabolism and immunosuppressive effects of mycophenolate mofetil (MMF) Clin Transplant. 1996;10:77–84. [PubMed] [Google Scholar]
- 2.Suthanthiran M, Morris RE, Strom TB. Immunosuppressants: cellular and molecular mechanisms of action. Am J Kidney Dis. 1996;28:159–172. doi: 10.1016/s0272-6386(96)90297-8. [DOI] [PubMed] [Google Scholar]
- 3.Behrend M. Adverse gastrointestinal effects of mycophenolate mofetil: aetiology, incidence and management. Drug Saf. 2001;24:645–663. doi: 10.2165/00002018-200124090-00002. [DOI] [PubMed] [Google Scholar]
- 4.de Mattos AM, Olyaei AJ, Bennett WM. Nephrotoxicity of immunosuppressive drugs: long-term consequences and challenges for the future. Am J Kidney Dis. 2000;35:333–346. doi: 10.1016/s0272-6386(00)70348-9. [DOI] [PubMed] [Google Scholar]
- 5.Liapis G, Boletis J, Skalioti C, Bamias G, Tsimaratou K, Patsouris E, Delladetsima I. Histological spectrum of mycophenolate mofetil-related colitis: association with apoptosis. Histopathology. 2013;63:649–658. doi: 10.1111/his.12222. [DOI] [PubMed] [Google Scholar]
- 6.Papadimitriou JC, Cangro CB, Lustberg A, Khaled A, Nogueira J, Wiland A, Ramos E, Klassen DK, Drachenberg CB. Histologic features of mycophenolate mofetil-related colitis: a graft-versus-host disease-like pattern. Int J Surg Pathol. 2003;11:295–302. doi: 10.1177/106689690301100406. [DOI] [PubMed] [Google Scholar]
- 7.Papadimitriou JC, Drachenberg CB, Beskow CO, Cangro C, Wiland A, Klassen D, Weir M, Bartlett S. Graft-versus-host disease-like features in mycophenolate mofetil-related colitis. Transplant Proc. 2001;33:2237–2238. doi: 10.1016/s0041-1345(01)01951-0. [DOI] [PubMed] [Google Scholar]
- 8.Epinette WW, Parker CM, Jones EL, Greist MC. Mycophenolic acid for psoriasis. A review of pharmacology, long-term efficacy, and safety. J Am Acad Dermatol. 1987;17:962–971. doi: 10.1016/s0190-9622(87)70285-0. [DOI] [PubMed] [Google Scholar]
- 9.Olyaei AJ, de Mattos AM, Bennett WM. Pharmacology of immunosuppressive drugs. Drugs Today (Barc) 1998;34:463–479. doi: 10.1358/dot.1998.34.5.485245. [DOI] [PubMed] [Google Scholar]
- 10.Childers R, Chow G, Fraig M, Asamoah V, Wong P. Education and imaging. Gastrointestinal: chronic CellCept-induced colitis. J Gastroenterol Hepatol. 2011;26:1214. doi: 10.1111/j.1440-1746.2011.06673.x. [DOI] [PubMed] [Google Scholar]
- 11.Behling KC, Foster DMJ, Edmonston TB, Witkiewicz AK. Graft-versus-host disease-like pattern in mycophenolate mofetil related colon mucosal injury: role of FISH in establishing the diagnosis. Case Rep Gastroenterol. 2009;3:418–423. doi: 10.1159/000260903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weclawiak H, Ould-Mohamed A, Bournet B, Guilbeau-Frugier C, Fortenfant F, Muscari F, Sallusto F, Dambrin C, Esposito L, Guitard J, Abbal M, Rostaing L, Kamar N. Duodenal villous atrophy: a cause of chronic diarrhea after solid-organ transplantation. Am J Transplant. 2011;11:575–582. doi: 10.1111/j.1600-6143.2010.03423.x. [DOI] [PubMed] [Google Scholar]
- 13.Maes BD, Dalle I, Geboes K, Oellerich M, Armstrong VW, Evenepoel P, Geypens B, Kuypers D, Shipkova M, Geboes K, Vanrenterghem YF. Erosive enterocolitis in mycophenolate mofetil-treated renal-transplant recipients with persistent afebrile diarrhea. Transplantation. 2003;75:665–672. doi: 10.1097/01.TP.0000053753.43268.F0. [DOI] [PubMed] [Google Scholar]
- 14.Khoury N, Ammor M, Durrbach A, Kriaa F, Charpentier B. Diffuse colitis associated with mycophenolate mofetil treatment: apropos of 1 case (in French) Nephrologie. 2000;21:437–439. [PubMed] [Google Scholar]
- 15.Jakes AD, Roy A, Veerasamy M, Bhandari S. Case report: Crohn's-like mycophenolate-induced colitis, a fallout in steroid-free regimens. Transplant Proc. 2013;45:842–844. doi: 10.1016/j.transproceed.2012.11.003. [DOI] [PubMed] [Google Scholar]