Abstract
Background:
Although giant cell tumor (GCT) is considered to be a primary benign bone tumor, its aggressive behavior makes its diagnosis and treatment, difficult and challenging. This is especially true in distal radius where GCT appears to be more aggressive and difficult to control locally. We report our clinical outcome of en-block resection and reconstruction with non-vascularized fibular autograft in 15 patients with distal radius GCT.
Materials and Methods:
We retrospectively reviewed 15 patients with GCT (Grade 2 and 3) of distal radius who were treated with en-block resection and non-vascularized fibular autograft. Five of 15 were recurrent GCT treated initially with extended curettage; local adjuvant therapy and filling the cavity with cement or bone graft. We followed the patients for mean 7.2 years post operation (range: 4-11 years). Patients were evaluated post operation with clinical examination, plain radiography of distal radius and chest X-ray and/or computed tomography scan. Furthermore pain, function, range of motion and grip strength of the affected limb were evaluated and mMayo wrist score was assessed.
Results:
A total of 11 patients were women and 4 were men. Mean age of patients was 29 years (range: 19-48). We had no lung metastasis and bony recurrence occurred in one patient (6.6%). Nearly 53.3% of patients had excellent or good functional wrist score, 80% of the patients were free of pain or had only occasional pain and 80% of patients returned to work. Mean range of motion of the wrist was 77° of flexion-extension and mean grip strength was 70% of the normal hand.
Conclusion:
En-block resection of distal radius GCT and reconstruction with non-vascularized fibular autograft is an effective technique for treatment in local control of the tumor and preserving function of the limb.
Keywords: Autograft, distal radius, giant cell tumor, outcome, reconstruction, fibular graft
INTRODUCTION
Giant cell tumor (GCT) is a relatively common primary benign bone tumor, which is usually seen at the end of long bones under the age of 40 years.[1] It is a locally potential aggressive lesion with the unique ability to produce lung metastasis. Although metaphyseoepiphyseal region of the distal femur and proximal tibia are more commonly affected, GCT in distal radius is both common and puzzling. Intralesional extended curettage with local adjuvant therapy, is an acceptable method for the treatment of this indistinctive behavior bone tumor with reasonable rate of recurrence.[2,3,4,5,6,7,8,9,10]
The mild symptoms may present for months before becoming severe enough to be visited by the physician. Acute events especially fractures with acute and severe pain, bring the tumor to clinical attention.[11]
GCT in the distal end of the radius is commonly associated with cortical invasion, pathologic fracture and extracompartmental extension, with a high rate of recurrence after extended curettage of the lesion. En-block resection with some kind of reconstruction surgery ranging from arthroplasty to allograft techniques may reduce the recurrence rate.[2,3] Non-vascularized fibular autograft is a method that we present here for reconstruction of the distal part of the radius after en-block resection of the tumor. Therefore, clinical outcome of en-block resection and reconstruction with non-vascularized fibular autograft for the treatment of GCT of distal radius in this study was evaluated.
MATERIALS AND METHODS
This cross-sectional study was approval by the research committee of our institute. We retrospectively reviewed 15 patients with histologically proved distal radius GCT (Grade 2 and 3) treated with en-block resection and non-vascularized fibular autograft from 2001 to 2007 in our referral hospital. Our inclusion criteria consisted of adult patients with definite pathological diagnosis of GCT of distal radius who was treated with resection of distal radius and replacement with a proximal avascular fibular autograft. Patients charts were reviewed, demographics, pre-operative evaluations and contact address were collected. Totally 11 patients were women and 4 men with a mean age of 29 years (range: 19-48). In 12 patients (80%) the lesion was in right radius and in other 3 patients (20%) left radius was involved. All patients were available for follow-up.
All patients had plain radiography as the first step in evaluation and magnetic resonance imaging (MRI) of the distal radius. Chest X-rays and/or chest computed tomography (CT) scan were included in the initial evaluation. All patients histologically proved to be GCT.
In one of recurrent cases, on histological examination, aneurismal bone cyst coexisted in addition to underlying GCT.
Surgery consisted of en-block resection of the tumor and reconstruction with ipsilateral fibular autograft with applying a radiofibular dynamic compression plate (DCP). Routinely, all patients had completed and signed a consent form before surgery.
Surgical technique
The margin of the tumor was determined precisely on plain radiography and MRI. Limits of bony involvement with additional 2.5 cm margin are considered to be safe wide margin and the appropriate length of fibula required for reconstruction is determined accordingly.[12,13]
Via a Henry's posterolateral approach to the ipsilateral proximal fibula, along the posterior margin of the fibular head and the biceps tendon, the common peroneal nerve is isolated and watched carefully.[14] The biceps tendon and lateral collateral ligament are dissected from fibular head and are securely fixed to the lateral aspect of the proximal tibia with a soft-tissue staple and adequate length of the fibula is dissected and ready to transplant. Incision is closed over a suction drain.
The tumor is approached through a Henry volar or dorsolateral. Radius is exposed extraperiosteally and is dissected with an oscillating saw at desired length (with at least 2.5 cm intact bone margin). Any soft-tissue extension of the tumor is removed as well with a reliable margin. Radial collateral ligament is preserved for future attachment to transplanted fibula.
Harvested fibula is fixed to the radius with a 3.5 DCP. Tip of fibula should lie for radial styloid and its articular surface articulates with scaphoid. Radiocarpal ligament is repaired and the transplanted fibula is stabilized to the wrist with two cross pins. A long arm splint in 90° of elbow flexion and 20° of wrist extension is applied. Splint and pins are removed 6 weeks post-operation and gentle range of motion is advised.
Patients were followed for a mean of 7.2 years (include the standard deviation) post-operation (ranging 4-10 years) with the clinical examination, plain radiography of the wrist and chest X-ray and/or CT scan. All patients were assessed for pain, function, range of motion and grip strength. Wrist function was evaluated using Mayo wrist score. Mayo wrist score was developed by Amadio et al. in 1989.[15] Mayo wrist score is a clinician reported questionnaire and includes 4 items of pain intensity, functional status, range of motion and grip strength.
RESULTS
In total, 11 patients were women and 4 men. Mean age of patients was 29 years (range: 19-48).
Five patients were treated before, with extended curettage, local adjuvant therapy and bone graft or bone cement as a cavity filler (bone graft in 2 patients and bone cement in 3 patients) and the tumor had been recurred in mean 18 months (ranging 3 months to 5 years) after initial surgery. No lung metastasis had been detected.
10 patients were not treated before and presented primarily to our institute.
We could achieve solid bony union in all patients. Soft-tissue recurrence occurred in two patients at a mean of 1½ years post-operation that were resected completely and at last follow-up were free of tumor. In one patient bony recurrence occurred in transplanted fibula. En-block resection and reconstruction with contralateral fibular autograft was carried out and the patient remained free of tumor at last follow-up. No lung metastasis has been detected, on the clinical assessment. Recurrence of tumor in carpal bones happened in one patient 2 years after surgery [Figures 1–4].
Figure 1.
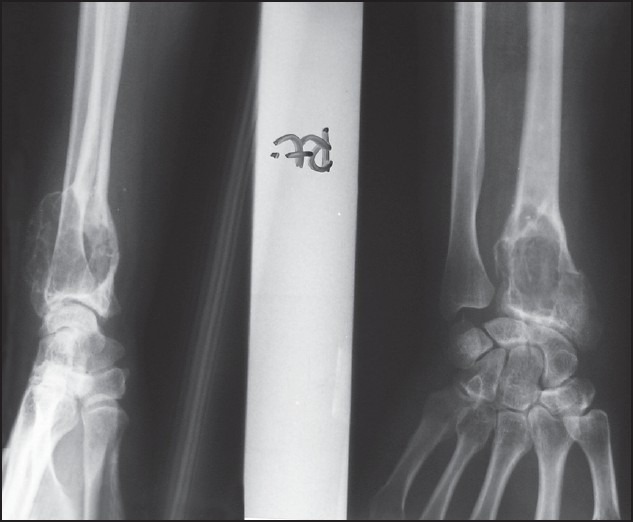
Anteroposterior and lateral X-ray of a 38-year-old woman with giant cell tumor of distal radius
Figure 4.

Anteroposterior and lateral X-ray of the knee of above patient shows proximal fibula has been harvested and lateral collateral ligament is reattached to proximal tibia with screw
Figure 2.
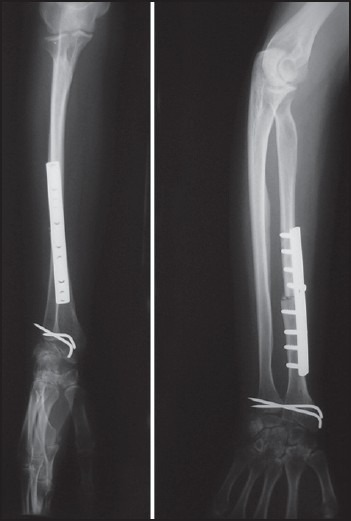
Post-operative anteroposterior and lateral X-ray of the patient who undergone wide resection of the tumor and proximal fibular autograft transplantation
Figure 3.
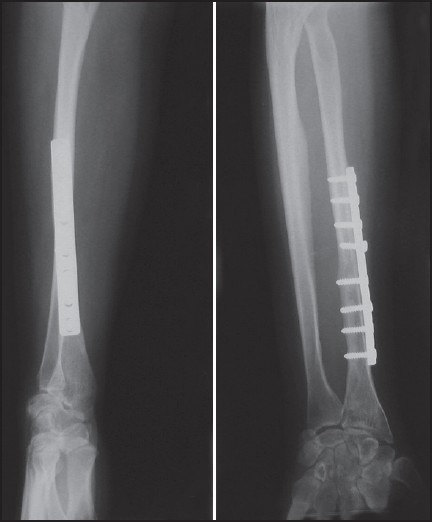
Anteroposterior and lateral of the above patient 48 months after primary en-block resection of distal radius giant cell tumor shows union of the fixation site, remodeling of the proximal fibula and recurrence of tumor in the carpal bones
Eight patients had no pain (53.3%), 4 had mild occasional pain (26.7%), 3 suffered of moderate tolerable pain (20%) and no one had sever intolerable pain.
Four patients returned to previous work with no limitation (26.7%), 8 returned to work but with restricted employment (53.3%), 3 patients were able to work but unemployed (20%) and no one was disabled due to pain.
All patients showed some limitation in the range of motion of the wrist. Five patients (33%) had flexion-extension ranging 20-120°, 6 patients had flexion/extension between 60° and 90° and in 4 patients flexion/extension was limited to 30-60°. However, no patient had flexion/extension <30°. Mean flexion/extension of the wrist was 77° with mean 35° of flexion and 42° of extension while normal wrist extension/flexion range of motion is 70/75.
In 7 patients grip strength was 75-100% of the contralateral normal hand (46.7%), in 5 patients grip strength was 50-75% and in 4 patients it was 25-50% of the normal hand. No patient had 100% grip strength of the normal hand or <25% of it. Mean grip strength of operated limb was 70% of normal hand.
According to the Mayo wrist score system, 3 patients had an excellent result (20%), 5 patients had a good result (33.3%), 5 patients had acceptable result (33.3%) and 2 patients had a poor result (13.4%) and mean wrist score was 64.0.
According the last follow-up visit, no patient complained of any symptom in donor proximal fibula knee and there was not any lateral instability of the knees. In addition, nor post-operative infection or neurovascular complication was reported by patients.
DISCUSSION
GCT of the long bones is known as an aggressive highly recurrent tumor. This is more obvious if the tumor is located at the end of the radius.[16,17,18] it is believed that this aggressive mood also, could be a risk factor for pulmonary metastasis.[19,20]
This tendency to local recurrence may be due to remaining of tumoral cells in soft tissue which act as the host for bone graft.[17,21] The less likely possibility is contamination of surgical site by the instruments.[22]
When treating a primary bone tumor, the first and principal goal should be complete removal of the lesion. Preserving function of the limb and planning for reconstruction procedures is not a priority and should be changed if tumor excision demands otherwise.[23] Prevention of local recurrence precedes maintaining limb function. This principle is still working when treating GCT of distal radius. GCT is a benign aggressive bone tumor and according to Campanacci classification most of these tumors are classified as Stage 2 or 3.[2,3]
It is thought that in GCT of distal radius, cortical invasion and break through with extracompartmental extension of the tumor is common. In addition local control in distal radius is difficult.[23,24,25,26] Local recurrence after extended curettage and cementing of GCT in distal radius has been reported as high as 88% of patients.[3] Considering local control of the lesion, wide resection with some kind of reconstruction, seems to be a more valuable method of treatment. Many reconstruction procedures have been proposed after wide resection of distal radius: Osteoarticular allograft, allograft arthrodesis. Vascularized or non-vascularized fibular autograft with or without arthrodesis are more recently accepted procedures.[23,24,25]
Non-vascular fibular autograft preserves wrist function and maintains anatomy of the carpus. In addition, there is no risk of viral transmissions. As mentioned before most GCTs of distal radius are Companacci Stage 2 and 3. In these stages of tumor, cortical thinning, cortical expansion or breakthrough with extracompartmental extension make complete removal of the tumor very difficult if not impossible.[2,3,23,24,26] The surgeon never can be sure of adequate curettage and almost always leave the surgery with a sense of uncertainty. Subchondral bone near the joint, cortical thinning and expansions are regions that never one can be sure of adequate curettage. We believe that wide margin en-block excision of the tumor is a better choice than extended curettage in the treatment of GCT of distal radius, unless in rare cases of Stage 1 Companacci with definite sclerotic margins. After excision, there are many reconstruction choices. Osteoarticular allograft and proximal fibula autograft are more desirable for preserving function and motion of the wrist.[2,23,24,27]
The study by Kocher et al. reported low recurrence rate, good function, moderate range of motion of the wrist, little pain and relatively high rate of revision after excision and reconstruction with osteoarticular allograft of 24 distal radius tumors, most of them GCT (20 of tumors). They proposed osteoarticular allograft as an acceptable option for reconstruction of distal radius benign aggressive and malignant tumors.[23]
In an article in 2005, Bianchi et al. reported results of osteoarticular allograft after resection of distal radius in 12 patients, 9 of them GCT and concluded that good functional outcome can be achieved with this technique and in spite of radiological signs of degenerative changes, function was acceptable. They reported 3 recurrence in these 12 patients, all of them GCT but all were free of disease at last follow-up.[24]
Szabo et al. in 2006 reported reasonable functional outcome after en-block excision and reconstruction with osteoarticular allograft and Sauve-kapandji procedure of 9 distal radius GCTs.[28]
Koul et al. in 2007 reported excellent and good functional results in two patients with distal radius GCT after excision of distal radius and reconstruction with free vascularized fibular autograft.[29]
In 2002, Maruthainar et al. reported their result of treating 13 patients with malignant and benign aggressive GCT) tumors of distal radius with wide excision and non-vascularized fibular autograft reconstruction. They proposed this technique as an acceptable option with satisfactory functional results without compromising the prognosis.[30]
In our study, we had only one bony recurrence (6.6% of patients) which is an acceptable result, considering local control of the tumor. When patients were assessed with Mayo Wrist Score, 53.3% hands excellent or good results, 80% had no pain or only occasional pain, 80% returned to work. Although all patients had some limitation in wrist range of motion, mean range of motion was 77° which is quite satisfactory. And mean grip strength was 70% of normal contralateral hand.
Although GCT is commonly considered benign, malignant cases can arise de-novo or transform from a benign lesion.[31] In this study, no lung metastasis has been detected, on clinical assessment.
Some limitations exist in the current study; we didn’t assess radiographic changes and the study did not compare the results of this technique to alternative techniques.
Another deficiency was that there was not a pre-operative wrist function and quality of life measurement in patients’ hospital charts to compare them to follow-up results. We believe that as long as functional outcomes are acceptable, radiographic changes are not important and that the pain and function, make surgical intervention necessary not radiographic changes. After a period of time, proximal fibula form to distal radius and may be indistinguishable from it. This means that the bone accommodates with forces exerted at the region and shape to the original bone. Finally, we would recommend wide margin en-block resection of distal radius GCT (Grade 2 and 3) and reconstruction with non-vascularized fibular autograft as an effective technique in long-term.
With this technique we can maintain acceptable function while preventing local recurrence. It has no risk of viral transmission with low complications and morbidity rate.
ACKNOWLEDGMENT
This research was done with support of Orthopedic Research Center, Mashhad University of Medical Sciences. Project number was 2405 in MUMS research affairs.
We also would like to thank Dr. Husain Ahmadzadeh and Dr. Reza Eshraghi for their assistance in drafting this manuscript.
Footnotes
Source of Support: This research was done with support of Orthopedic Research Center, Mashhad University of Medical
Conflict of Interest: None declared.
REFERENCES
- 1.Kulenovic E. Giant cell tumor. Appl Radiol. 2008;37:37–9. [Google Scholar]
- 2.Turcotte RE. Giant cell tumor of bone. Orthop Clin North Am. 2006;37:35–51. doi: 10.1016/j.ocl.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 3.Balke M, Schremper L, Gebert C, Ahrens H, Streitbuerger A, Koehler G, et al. Giant cell tumor of bone: Treatment and outcome of 214 cases. J Cancer Res Clin Oncol. 2008;134:969–78. doi: 10.1007/s00432-008-0370-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morii T, Yabe H, Morioka H, Suzuki Y, Anazawa U, Toyama Y. Curettage and allograft reconstruction for giant cell tumours. J Orthop Surg (Hong Kong) 2008;16:75–9. doi: 10.1177/230949900801600117. [DOI] [PubMed] [Google Scholar]
- 5.Zhen W, Yaotian H, Songjian L, Ge L, Qingliang W. Giant-cell tumour of bone. The long-term results of treatment by curettage and bone graft. J Bone Joint Surg Br. 2004;86:212–6. doi: 10.1302/0301-620x.86b2.14362. [DOI] [PubMed] [Google Scholar]
- 6.von Steyern FV, Kristiansson I, Jonsson K, Mannfolk P, Heinegård D, Rydholm A. Giant-cell tumour of the knee: The condition of the cartilage after treatment by curettage and cementing. J Bone Joint Surg Br. 2007;89:361–5. doi: 10.1302/0301-620X.89B3.18604. [DOI] [PubMed] [Google Scholar]
- 7.Siebenrock KA, Unni KK, Rock MG. Giant-cell tumour of bone metastasising to the lungs. A long-term follow-up. J Bone Joint Surg Br. 1998;80:43–7. doi: 10.1302/0301-620x.80b1.7875. [DOI] [PubMed] [Google Scholar]
- 8.Vult von Steyern F, Bauer HC, Trovik C, Kivioja A, Bergh P, Holmberg Jörgensen P, et al. Treatment of local recurrences of giant cell tumour in long bones after curettage and cementing. A Scandinavian Sarcoma Group study. J Bone Joint Surg Br. 2006;88:531–5. doi: 10.1302/0301-620X.88B4.17407. [DOI] [PubMed] [Google Scholar]
- 9.Malek F, Krueger P, Hatmi ZN, Malayeri AA, Faezipour H, O’Donnell RJ. Local control of long bone giant cell tumour using curettage, burring and bone grafting without adjuvant therapy. Int Orthop. 2006;30:495–8. doi: 10.1007/s00264-006-0146-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu YP, Li KH, Sun BH. Which treatment is the best for giant cell tumors of the distal radius? A meta-analysis. Clin Orthop Relat Res. 2012;470:2886–94. doi: 10.1007/s11999-012-2464-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murphey MD, Nomikos GC, Flemming DJ, Gannon FH, Temple HT, Kransdorf MJ. From the archives of AFIP. Imaging of giant cell tumor and giant cell reparative granuloma of bone: Radiologic-pathologic correlation. Radiographics. 2001;21:1283–309. doi: 10.1148/radiographics.21.5.g01se251283. [DOI] [PubMed] [Google Scholar]
- 12.Oliveira VC, van der Heijden L, van der Geest IC, Campanacci DA, Gibbons CL, van de Sande MA, et al. Giant cell tumours of the small bones of the hands and feet: Long-term results of 30 patients and a systematic literature review. Bone Joint J. 2013;95-B:838–45. doi: 10.1302/0301-620X.95B6.30876. [DOI] [PubMed] [Google Scholar]
- 13.Pazionis TJ, Alradwan H, Deheshi BM, Turcotte R, Farrokhyar F, Ghert M. A systematic review and meta-analysis of En-Bloc vs intralesional resection for giant cell tumor of bone of the distal radius. Open Orthop J. 2013;7:103–8. doi: 10.2174/1874325001307010103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Canale ST, Beaty JH. Mosby; 2012. Campbell's Operative Orthopaedics. [Google Scholar]
- 15.Amadio PC, Berquist TH, Smith DK, Ilstrup DM, Cooney WP, 3rd, Linscheid RL. Scaphoid malunion. J Hand Surg [Am] 1989 Jul;14:679–87. doi: 10.1016/0363-5023(89)90191-3. [DOI] [PubMed] [Google Scholar]
- 16.Harris WR, Lehmann EC. Recurrent giant-cell tumour after en bloc excision of the distal radius and fibular autograft replacement. J Bone Joint Surg Br. 1983;65:618–20. doi: 10.1302/0301-620X.65B5.6643568. [DOI] [PubMed] [Google Scholar]
- 17.Sheth DS, Healey JH, Sobel M, Lane JM, Marcove RC. Giant cell tumor of the distal radius. J Hand Surg Am. 1995;20:432–40. doi: 10.1016/S0363-5023(05)80102-9. [DOI] [PubMed] [Google Scholar]
- 18.O’Donnell RJ, Springfield DS, Motwani HK, Ready JE, Gebhardt MC, Mankin HJ. Recurrence of giant-cell tumors of the long bones after curettage and packing with cement. J Bone Joint Surg Am. 1994;76:1827–33. doi: 10.2106/00004623-199412000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Cheng JC, Johnston JO. Giant cell tumor of bone. Prognosis and treatment of pulmonary metastases. Clin Orthop Relat Res. 1997;338:205–14. doi: 10.1097/00003086-199705000-00027. [DOI] [PubMed] [Google Scholar]
- 20.Maloney WJ, Vaughan LM, Jones HH, Ross J, Nagel DA. Benign metastasizing giant-cell tumor of bone. Report of three cases and review of the literature. Clin Orthop Relat Res. 1989;243:208–15. [PubMed] [Google Scholar]
- 21.Saiz P, Virkus W, Piasecki P, Templeton A, Shott S, Gitelis S. Results of giant cell tumor of bone treated with intralesional excision. Clin Orthop Relat Res. 2004;424:221–6. doi: 10.1097/01.blo.0000128280.59965.e3. [DOI] [PubMed] [Google Scholar]
- 22.Gursu S, Demir B, Yildirim T, Er T, Oke R, Sahin V. Reconstruction of the wrist using fibular autograft after excision of a giant cell tumor of the distal radius: Report of an unexpected outcome. Eur Orthop Traumatol. 2011;1:203–6. [Google Scholar]
- 23.Kocher MS, Gebhardt MC, Mankin HJ. Reconstruction of the distal aspect of the radius with use of an osteoarticular allograft after excision of a skeletal tumor. J Bone Joint Surg Am. 1998;80:407–19. doi: 10.2106/00004623-199803000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Bianchi G, Donati D, Staals EL, Mercuri M. Osteoarticular allograft reconstruction of the distal radius after bone tumour resection. J Hand Surg Br. 2005;30:369–73. doi: 10.1016/j.jhsb.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 25.Duan H, Zhang B, Yang HS, Liu YH, Zhang WL, Min L, et al. Functional outcome of en bloc resection and osteoarticular allograft reconstruction with locking compression plate for giant cell tumor of the distal radius. J Orthop Sci. 2013;18:599–604. doi: 10.1007/s00776-013-0394-1. [DOI] [PubMed] [Google Scholar]
- 26.Trieb K, Bitzan P, Lang S, Dominkus M, Kotz R. Recurrence of curetted and bone-grafted giant-cell tumours with and without adjuvant phenol therapy. Eur J Surg Oncol. 2001;27:200–2. doi: 10.1053/ejso.2000.1086. [DOI] [PubMed] [Google Scholar]
- 27.Rabitsch K, Maurer-Ertl W, Pirker-Frühauf U, Lovse T, Windhager R, Leithner A. Reconstruction of the distal radius following tumour resection using an osteoarticular allograft. Sarcoma 2013. 2013 doi: 10.1155/2013/318767. 318767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Szabo RM, Anderson KA, Chen JL. Functional outcome of en bloc excision and osteoarticular allograft replacement with the Sauve-Kapandji procedure for Campanacci grade 3 giant-cell tumor of the distal radius. J Hand Surg Am. 2006;31:1340–8. doi: 10.1016/j.jhsa.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 29.Koul A, Patil R, Philip V, Kale S. Reconstruction of lower end of radius using vascularized upper end of fibula. Indian J Plast Surg. 2007;40:61–6. [Google Scholar]
- 30.Maruthainar N, Zambakidis C, Harper G, Calder D, Cannon SR, Briggs TW. Functional outcome following excision of tumours of the distal radius and reconstruction by autologous non-vascularized osteoarticular fibula grafting. J Hand Surg Br. 2002;27:171–4. doi: 10.1054/jhsb.2001.0707. [DOI] [PubMed] [Google Scholar]
- 31.Riddle ND, Yamauchi H, Caracciolo JT, Cheong D, Khakpour N, Bui MM. Giant cell tumor of the anterior rib masquerading as a breast mass: A case report and review of current literature. Cases J. 2010;3:51. doi: 10.1186/1757-1626-3-51. [DOI] [PMC free article] [PubMed] [Google Scholar]


