Abstract
Background:
Parents of children with developmental problems are always bearing a load of stress. The aim of this study is to compare the stress in mothers of children with different disabilities to each other, considering their demographic background.
Materials and Methods:
This was a cross-sectional study conducted in Isfahan, Iran during 2012 on 285 mothers of 6-12 years old children with chronic physical disease, psychological disorder, and sensory-motor and mental problems. Abedin's parenting stress questionnaire was used and obtained data were analyzed using multivariate analysis of variance or covariance as appropriate.
Results:
Mothers of children with sensory-motor mental and chronic physical problems experience more stress than mothers of children with psychological disorders (P < 0.05). The stress score of mothers of children with psychological disorders was lower than the other two groups. Also there was a significant difference between the score of mothers of children with chronic physical problems and mothers of children with psychological disorders regarding parent-child dysfunctional interaction (P < 0.01). A significant difference was observed in terms of stress among mothers of children with sensory-motor mental problems with different number of children (P < 0.05); also mothers of children with chronic physical problems in different levels of education have experienced different levels of parenting stress (P < 0.05)
Conclusion:
Due to high level of parenting stress among our studied samples, special education and early intervention are needed for parents in our study population in order to deepening their diagnostic knowledge and professional consultation on stress management
Keywords: Developmental disability, mental health, parenting stress, physical chronic problem, psychological disorder
INTRODUCTION
Long-term limitative conditions, especially for children, lead to stress for the individual and particularly for their family. Under difficult circumstances and beyond one's ability of adaptation, stress would be spread to every aspect of life and would lead the person to show an adaptive or nonadaptive response.[1,2]
Having a child with developmental or psychological problems is always stressful for their parents who are taking care of them, even when the child is a grown up person, which would cause a constant incompatibility of parents with their child's disability.[3,4] These parents, other than bearing financial pressures, are always facing emotional pressures such as feeling ashamed or feeling guilty.[4,5]
The relation between stress and parenting has attracted the attention of researchers for a long time. The pressure of raising a child is an important concept in parenting and mostly it has a close relation with parents’ dysfunction[6] One of the factors that would lead to stress in women is their responsibility as a housewife that would be divided to three main classes:
taking care of elderlies,
taking care of children, and c) taking care of children with special needs.[7] It could be said that mothers of children with special needs experience more stress than mothers of normal children. Parents of children with different disorders report higher levels of anxiety and depression, negative parent-child interactions, insecure attachment of the child, physical abuse, and child's behavioral and emotional problems.[8]
Shin and Nhan[9] have mentioned more stress among parents of children with cognitive delay and also has revealed the relation between lower levels of education and low social supports with their stress; Shin and Nhan also added that after controlling all the other demographic and psychological variables, having a child with cognitive delay is the strongest predictor of stress.
Also Mahoney and Perales[10] has mentioned that the severity of child's disability is an important predictor of mother's parenting stress; moreover, diagnosis of pervasive developmental disorders (DDs) in children and the parent-child interactions before any interventions are predictors of changes in parent-child interactions after the treatment. It has been revealed that mothers who experience higher levels of stress have a lower quality of life compared with those who experience less stress.[11]
Having an autistic child has a negative influence on mother's mental and emotional functions. Mothers of autistic children report higher stress and poorer mental health than normal mothers. Social support is a variable that mediate the effects of having an autistic child on the mental health of the mother and family's function.[12] Any defect and delay in a child's social relationships is related to parenting stress, parent-child's relationship problems, and parental distress (PD)[7] Hoffman et al.,[13] has also mentioned higher levels of stress in mothers of autistic children compared with normal mothers, with a significant difference regarding attachment.
Research has showed that even parents of children with attention deficit hyperactive disorder (ADHD) or DDs report higher levels of stress in comparison to parents of human immunodeficiency virus (HIV) positive children, children with asthma, and those who have normal development.[14]
Considering all that has mentioned, the question is what is the difference between three groups of mothers of disabled or sick children regarding their stress and after considering variables like mother's education, duration of illness or disorder, or child's problem in the Iranian population how would that difference stand. By answering this question and also by studying the stress in parents of children with different disabilities. some relevant therapeutic interventions for these parents and through methods of stress management interventions could be adapted to prevent many of these parents’ problems with their children. In this study, it has been assumed that mothers of children with different disabilities experience different levels of stress. In fact, using a representative sample of mothers of children with developmental and mental problems, we study the effect of having a disabled child on mother's physical and mental health, to assess the predictors of well-being of these parents.
MATERIALS AND METHODS
Study design and participants
This was a cross-sectional (comparative) study that was conducted during 2012. The sample of this study was parents of 6-12 years old children suffering from sensory-motor mental, chronic physical, and psychological disorders. Samples belonged to one these three groups: chronic physical diseases (diabetes, epilepsy, renal problems, and leukemia), difficult sensory-motor conditions (blindness, deafness, mental retardation, cerebral palsy), and psychological problems (scolionophobia, autism, ADHD, conduct disorder, oppositional defiant disorder, and learning disability). A total of 285 mothers of children with one of the above-mentioned problems were selected through conveneive sampling method from those who referred to psychiatric clinics for children, specialists’ offices, and also advisory centers of department of education and training centers–autism rehabilitation and organization for exceptional children of Isfahan city. Inclusion criteria were having a 6-12 years old child, having just one child with one of the above-mentioned problems, having finished middle school, the presence of both parents in the family, employment of the father and not facing any serious financial crisis, not having any other member in the family suffering from chronic physical-mental problems, not having the child admitted to a boarding school, not having serious marital conflicts during the past month, and no record of the death of a loved one during the past 3 months; also they should have been consent to participate in the study and in the case of mothers’ unwillingness to cooperate for completing the questionnaires and giving full answers they would have been excluded from the study. The study was approved by bioethic commity of Isfahan university of medical sciences and a written informed consent was obtained from all study's participants.
Research instrument
For this study, data were gathered using parenting stress index. Parenting stress index is a self-report tool with 36 items in three subscales [PD, parent-child dysfunctional interaction (PCD), difficult child (DC)] that was designed by Abedin in 1990 with a good test-retest reliability result for measuring the stress of the parent-child relationship and defining their psychological sources of stress. In a study by Petch et al.,[15] its α was calculated to be 0.83 for men and women. Researches of Abedin, Silovsky, and Nice have shown that this index can separate the parents of the clinical group and the control group with a really high resolution. In Iran the validity of this index was measured using Cronbach's α for subscales of parental distress, PCD, DC and the total score, and the scores were 0.82, 0.76, 0.89, and 0.93, respectively.[8]
Other variables that were measured for this study included: child's gender, the duration of the child's problem, mother's level of education, number of children, and the birth order of the child with the difficult condition and parenting stress level was compared between them.
Statistical analysis
Data were analyzed using SPSS software version 11.5 (SPSS Inc, Chicago, IL, USA). Quantitative data were expressed as mean (standard deviation) and qualitative as number (percent). Multivariate analysis of variance (MANOVA) (or covariance (MANCOVA) as appropraite) was used for comparing the parenting stress score among studied groups. Bonferroni post hoc test was used for pairwise comparisions. P < 0.05 was considered as statisticaly significant level.
RESULTS
In this study, children were divided into three groups of physical-mental problems, psychological problems, and chronic physical problems; 52.28% of them had physical problems, 22.46% had sensory-motor mental problems, and 25.26% had chronic physical problems. A total of 141 of these children were girls and 144 were boys. Also, almost 62% of the children were the first child of their family, and only the birth order of 38% was second or more. About 80% of the studied mothers were housewife. Studying mothers’ level of education showed that 16.5% of them have finished middle school, 51.2% have finished high school, and 32.3% had college degrees. Also, about 73% of the studied families had up to two children. It was revealed that almost 70% of the children have been suffering from physical and mental problems for at least 4 years [Table 1]. Assessing the total score of parenting stress in parents of children with problems showed that there was a meaningful relationship between the kind of problem that child is suffering from and the score of parenting stress (P < 0.01). As shown in Table 2, parents of children with sensory-motor mental problems, and chronic physical problems, experience more stress than parents of children with psychological problems (P < 0.01). In this study, other than the total score of parenting stress, the scores of three aspects of PD, PCD, and DC were also assessed. The comparative results based on the child's problem are shown in Table 2. Results showed that based on the child's problem, the scores of PD (P < 0.05) and PCD (P < 0.01) have a significant difference. To identify the groups that led to the significant difference the Bonferroni test was used. The results of this test showed regarding the aspect of PD, the scores of mothers of children with physical-mental problems and mothers of children with chronic physical problems are significantly different from the score of mothers of children with psychological problems (P < 0.05). In fact, mothers of children with psychological problems scored less than the other two groups regarding parental distress. This test also showed that the significant difference in the PCD scores is between the scores of mothers of children with chronic physical problems and mothers of children with psychological problems (P < 0.01).
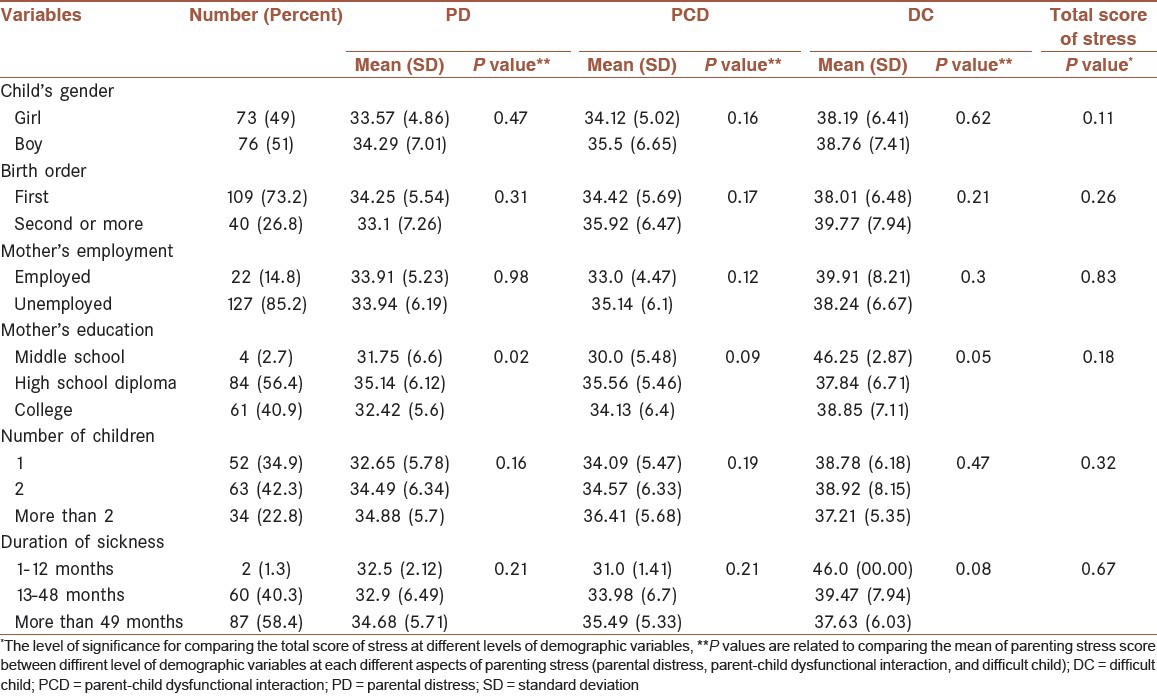
Table 1.
The scores of parenting stress at different levels of demographic variables for three groups of mothers with difficult children
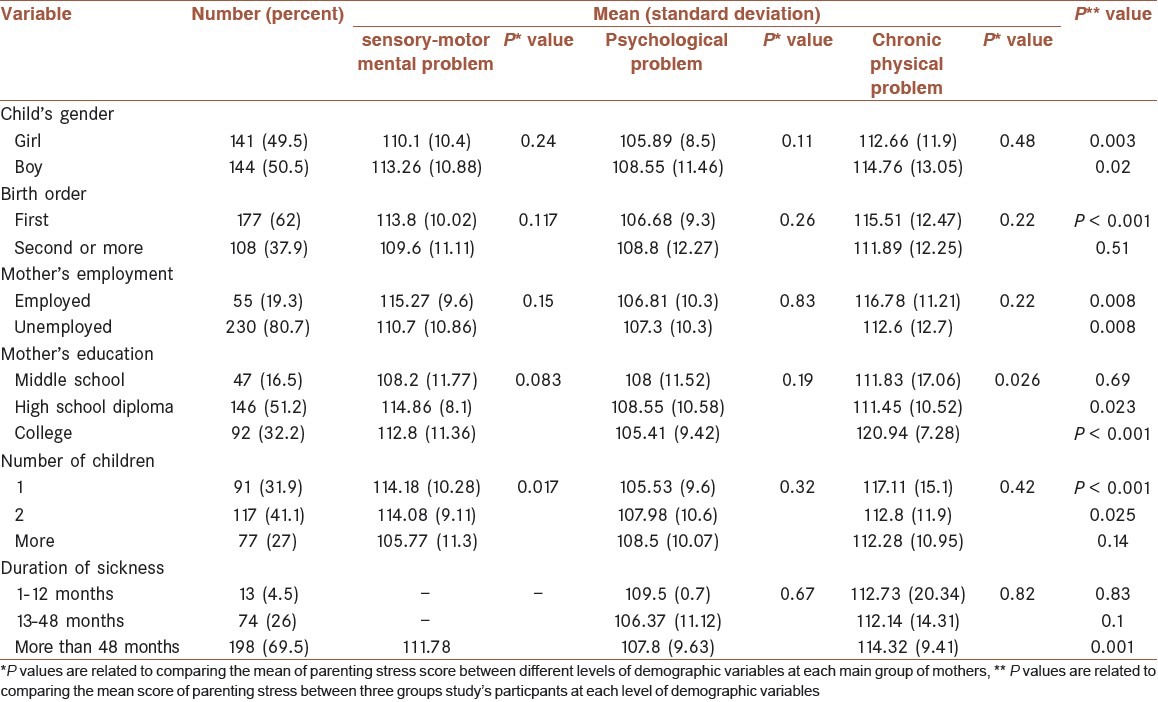
Table 2.
Comparison of the total score of stress and its different aspects in children with different problems
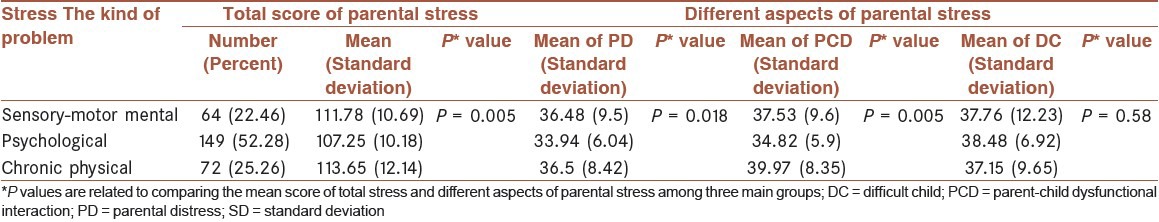
Table 1 shows the comparison of the score of parenting stress for different levels of demographic variables (gender, birth order, mother's employment, mother's education, number of children, and the duration of the sickness). It could be noticed that mother's education for children with chronic physical problem (P < 0.05) and number of children for children with sensory-motor mental problems are of significant importance. In fact, mothers of children with chronic physical problems who have college degrees experience more stress than mothers of the same groups with lower levels of education. On the contrary, parenting stress in mothers of girls (P < 0.05) or mothers of boys (P < 0.01) showed a significant difference in terms of kinds of problems and mothers of children with chronic physical problems show more parenting stress than other two groups. Based on different kinds of problems, there was also a significant difference between the score of parenting stress of mothers that their first child had problem, mothers with high school or college degrees, mothers with one or two children, and mothers who their child has been sick for more than 48 months [Table 1].
The results of comparing the score of different aspects of parenting stress (PD, PCD, and DC) at different levels of demographic variables for each group of mothers are shown in Tables 3–5.
Table 3.
The scores of different aspects of parenting stress (parental distress, parent-child dysfunctional interaction, and difficult child) at different levels of demographic variables for mothers of children with sensory-motor mental problems
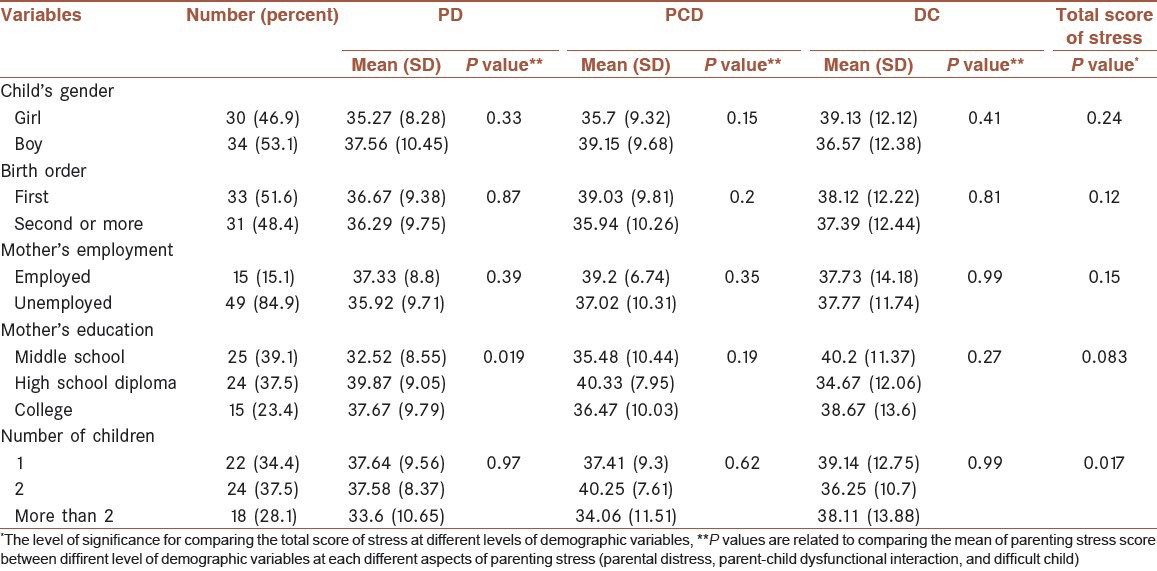
Table 5.
The scores of different aspects of parenting stress (parental distress, parent-child dysfunctional interaction, and difficult child) at different levels of demographic variables for mothers of children with chronic physical problems
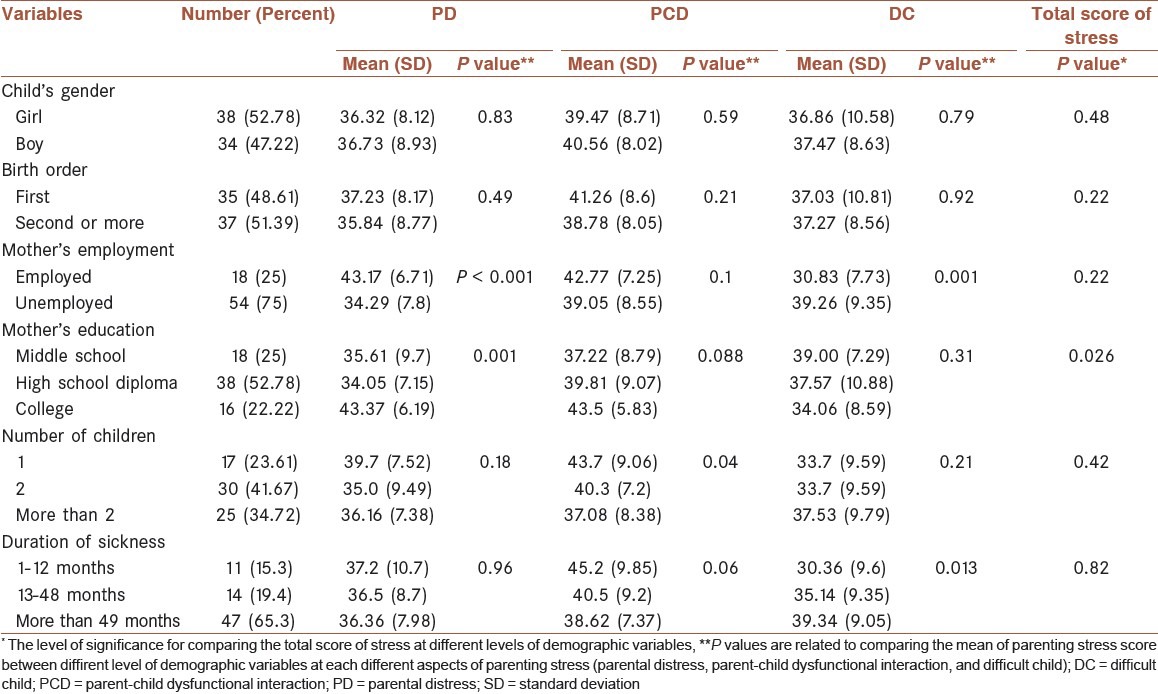
Table 3 shows the score of different aspects of parenting stress (PD, PCD, and DC) at different levels of demographic variables for mothers of children with sensory-motor mental problems. Results revealed a significant difference in terms of PD score of at different levels of mother's education; also, mothers of children with sensory-motor mental problems who have a high school diploma experienced more distress (PD) than other mothers of the same group. Also, the total score of parental stress only has a significant difference at different levels of the number of children t. Considering Table 4, it could be inferedthat the score of PD and DC aspects have significant difference at different levels of mother's education and mothers of children with psychological problems and a high school diploma have higher scores of PD and DC. Table 5, like both previous Tables, contains the scores of different aspects of parenting stress at different levels of demographic variables. The score of PD for mothers of children with chronic physical problems showed significant differences at different levels of mother's education and mother's employment; this difference is in mothers who are employed and those who have a college degree. Also, the score of PCD for mothers of children with chronic physical problems showed a significant difference for those who had different number of children; families with one child had a higher score than others. Regarding the aspect of DC, it could be mentioned that mother's employment and the duration of sickness were the demographic variables that made significant differences (P = 0.013). In this case, mothers who are employed and those who are dealing with their child's condition for more than 48 months made higher scores. And finally, the total score of parenting stress was higher for mothers of children with chronic physical who have not finished the middle school.
Table 4.
The scores of different aspects of parenting stress (parental distress, parent-child dysfunctional interaction, and difficult child) at different levels of demographic variables for mothers of children with psychological problems
DISCUSSION
As the aim of this study was to study the differences between three groups of mothers of disabled or sick children regarding their parenting stress and also to investigate the potential effects of variables such as mother's education, the duration of sickness, or child's problems in the Iranian society on these differences, results revealed that parents of children with sensory-motor mental problems and chronic physical problems experience higher levels of parenting stress and higher scores of PD and PCD in comparison with parents of children with psychological problems. Similar studies have also revealed that parents of disabled children, in comparison with parents of normal children, experience higher levels of negative effects, less social and mental welfare, and significantly more physical problems; parents would never totally accept their child's disability.[4] Results of Habibi's study (2009) showed that mothers of exceptional children report more parental stress. In this study, assessing the effect on each subscale showed that the score of stress in mothers of exceptional children was higher than mothers of normal children in subscales of parental distress, parent-child dysfunctional interaction, and DC.[8]
Also, research results have reported that parents of children with developmental problems and children with mental health problems both suffer from negative agitations and physical problems more than parents of normal children. In the study of Ha et al.,[16] parents of children with developmental problems had less social and mental welfare in comparison to the control group, although in the same study the social and mental welfare of the parents of children with mental health issues had no significant difference with the control group. Based on the multivariable analysis conducted in the study of Ha et al., parents of children with developmental or mental health problems experienced higher levels of negative agitation, less social and mental welfare and more physical problems in comparison with parents with no disabled child; these results show that having a disabled child is just one of the reasons, among so many other reasons, that could affect the social and mental welfare of parents.[16]
In the study of Hung et al.,[17] a significant difference was observed between different diagnostic groups regarding each parenting stress subscale. Parents of children diagnosed with cancer showed significantly higher levels of stress comparing to parents of disabled children. In the study of Colletti et al.,[18] it was revealed that higher levels of parental stress, but not parents’ obsessive protection or child's perceived vulnerability, had a significant relation with lower levels of social and behavioral adjustment. Higher levels of children's perceived vulnerability and parental stress, but not parents’ obsessive protection, had an independent relation with lower levels of emotional adjustment.
Seltzer et al.,[4] also found that parents of children with developmental problems in comparison to parents of children with psychological problems had more physical complaints and experienced higher levels of depression; the depression level in both of these groups were higher than parents of normal children, and lack of mental health, having signs of stress, depression, or anxiety could disturb the accountability and effectiveness of the parenting style.[19] It has been reported that parents of children with ADHD and developmental problems show higher levels of stress in comparison to parents of children suffering from HIV and asthma and normal children.
Regarding sensory deficits, studies have shown that people suffering from sensory deficits would gradually develop a kind of depression and isolation due to their deficits and this isolation would lead to dysfunctional interactions with others including their mothers.[21] Mothers of these patients also in comparison with mothers of normal children show higher levels of stress and depression.[22] It seems that not only the future of children with chronic physical problems and sensory-motor mental problems would lean on their dependence to others more than children with hyperactivity and scolionophobia, but also their current condition requires special care, follow-ups, rehabilitation, and special education. Moreover, parents’ interpretation of their child's problem and their coping style with that problem are also effective factors, like mother's education, that could play a mediator role and explain the observed significance in differences.
Among all the observed loads of parenting, parents believe that management of their child's troubling behaviors is the most pressuring challenge.[23] There is also an emotional load related to being ashamed of their child's disability, being sorrowful to confirm that their child can never experience a normal adolescence, and being worried about who's going to take care of their child after their death.[4] As a result of these kinds of long-term chronic pressures on the parents of disabled children, parents of disabled children experience more physical problems and higher levels of depression compared with the parents of normal children.[24,25]
Results also revealed that dealing with the problem for a longer amount of time would lead to more stress especially regarding the aspect of DC. Cumulative stress model claims that weariness and exhaustion due to the stress caused by taking care would add up during time and people who deal with stressful chronic conditions for longer amounts of time would be more vulnerable compared to those who had a short time stressful experience.[16]
On the contrary, the transactional model (Lazarus and Folkman, 1984) suggests that the longer someone spends trying to cope with a stressful condition, the better they would be able to adjust with that challenge. During time, parents would adjust with the stress caused by their child's disability; hence, they will learn new skills to have better reacts and responds toward their life conditions.
Overall, it could be said that psychological acceptance and empowerment have a significant relation with the severity of the parents’ mental health issues. Psychological acceptance as a minor mediator influences the path between child's difficult behavior and parents’ mental issues. As the difficult behavior of the child increases, parents’ psychological acceptance lowers and therefore their mental health issues increases. These results show that for chronic problems psychological acceptance could be an important confronting factor for parents of children with difficult physical and mental conditions.
Social and mental welfare of disabled child could be endangered by different factors such as the load of managing the condition, self-concept matters that are related to the guilty feelings, stress-related to the child's behavioral difficulties, anxiety about the future, and feeling of loss for the hopes they had for their children. Through special caring measures (like hours and the intensity of care) and by knowing the child's characteristics and parents’ expectations of their disabled child, it could be possible for us to better realize the mechanism through which having a disabled child could affect the social and mental welfare of the parents.
Limitations
The limitations of this study that worthy of mentioning are
the cross-sectional design of the study have probably caused the effects of age would be twisted with the effects of the group. It means that people with different ages were divided in different groups and these group differences, instead of their age differences, could have led to different results. Moreover, with cross-sectional data, we could not study the interpersonal changes during time. Therefore, we should be careful about interpreting the differences in age as the effects of aging.
Since the sample size of some of the diagnosed problems (blindness, deafness) was small, we were not able to study the effect of different kinds of developmental and psychological problems separately. Further studies should use more refined measurement scales to assess the differential effects of different disabilities and the intensity of their effects on parenting stress. So, this study is one of the few studies using a nationally representative sample and a control group for systematic review of variability caused by having a child with developmental problems and to assess the effect of mental health on parents’ social and mental welfare. It is suggested that further studies should review other known factors explaining the differences in the social caring burdens, such as caregiver's social and economic status, race, health characteristics, and social support and society's resources, that could show how much taking care of a disabled child could affect parents’ physical and mental health.
Special educations and early interventional measures should be more extensive in Iran and it should be available to educate children with cognitive delay and support mothers. The results of this study show that most of the parents in our sample population must be referred to specialists for deepening their diagnostic knowledge and professional consultation on stress management.
ACKNOWLEDGMENT
We must thank here all the centers for education and rehabilitation of children with special needs, especially the center for education of autistic children, specialized medical centers of the Isfahan city, and families of the disabled children which their cooperation has made this research an easy job for us.
Authors contribution: Awat Feizi contributed in study design, data analysis and drafting and finalizing the manuscript, Badroddin Najme contributed in study design, drafting and finalizing the manuscript. Aseih Salesi contributed in data analysis and finalizing the manuscript and other authors contributed in data collection, drafting and finalizing the manuscript.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Davis NO, Carter AS. Parenting stress in mothers and fathers of toddlers with autism spectrum disorders: Associations with child characteristics. J Autism Dev Disord. 2008;38:1278–91. doi: 10.1007/s10803-007-0512-z. [DOI] [PubMed] [Google Scholar]
- 2.Sarafino EP. 4th ed. New York: John wiley&sons Inc; 2002. Health Psychology. [Google Scholar]
- 3.Kling KC, Seltzer MM, Ryff CD. Distinctive late-life challenges: Implications for coping and well-being. Psychol Aging. 1997;12:288–95. doi: 10.1037//0882-7974.12.2.288. [DOI] [PubMed] [Google Scholar]
- 4.Seltzer MM, Greenberg JS, Floyd FJ, Pettee Y, Hong J. Life course impacts of parenting a child with a disability. Am J Ment Retard. 2001;106:265–86. doi: 10.1352/0895-8017(2001)106<0265:LCIOPA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Clark RE, Drake RE. Expenditures of time and money by families of people with severe mental illness and substance use disorders. Community Ment Health J. 1994;30:145–63. doi: 10.1007/BF02188626. [DOI] [PubMed] [Google Scholar]
- 6.Ostberg M, Hagekull B. A structural modeling approach to the understanding of parenting stress. J Clin Child Psychol. 2000;29:615–25. doi: 10.1207/S15374424JCCP2904_13. [DOI] [PubMed] [Google Scholar]
- 7.Waisbren SE, Rones M, Read CY, Marsden D, Levy HL. Brief report: Predictors of parenting stress among parents of children with biochemical genetic disorders. J Pediatr Psychol. 2004;29:565–70. doi: 10.1093/jpepsy/jsh058. [DOI] [PubMed] [Google Scholar]
- 8.Habibi Asgar Abad M, Rashidi A, Motevalipour A. Comparing the parental stress between the mothers of disabled boys and the mothers of normal boys. J Res Behav Sci. 2009;2:175–81. [Google Scholar]
- 9.Shin JY, Nhan NV. Predictors of parenting stress among Vietnamese mothers of young children with and without cognitive delay. J Intellect Dev Disabil. 2009;34:17–26. doi: 10.1080/13668250802690914. [DOI] [PubMed] [Google Scholar]
- 10.Mahoney FP. Case Western Reserve University: AAT; 2009. The relationship between parenting stress and maternal responsiveness among mothers of children with developmental problems. [Google Scholar]
- 11.Armstrong N. TUI University: AAT; 2009. The health-related quality of life in mothers of surviving deaf-blind adult children with congenital rubella syndrome. [Google Scholar]
- 12.Montes G, Halterman JS. Psychological functioning and coping among mothers of children with autism: A population-based study. Pediatrics. 2007;119:e1040–6. doi: 10.1542/peds.2006-2819. [DOI] [PubMed] [Google Scholar]
- 13.Hoffman CD, Sweeney DP, Hodge D, Lopez-Wagner MC, Looney L. Parenting stress and closeness; mothers of typically developing children and mothers of children with Autism. Focus Autism Other Dev Disabl. 2004;24:178–88. [Google Scholar]
- 14.Gupta VB. Comparison of parenting stress in different developmental disabilities. J Dev Phys Disabil. 2007;19:417–25. [Google Scholar]
- 15.Petch JF, Halford WK, Creedy DK, Gamble J. A randomized controlled trial of a couple relationshipe and coparenting program (Couple CARE for Parents) for high-and low-risk new parents. J Consult Clin Psychol. 2012;80:662–73. doi: 10.1037/a0028781. [DOI] [PubMed] [Google Scholar]
- 16.Ha JH, Hong J, Seltzer MM, Greenberg JS. Age and gender differences in the well-being of midlife and aging parents with children with mental health or developmental problems: Report of a National Study. J Health Soc Behav. 2008;49:301–16. doi: 10.1177/002214650804900305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hung JW, Wu YH, Yeh CH. Comparing stress levels of parents of children with cancer and parents of children with physical disabilities. Psychooncology. 2004;13:898–903. doi: 10.1002/pon.868. [DOI] [PubMed] [Google Scholar]
- 18.Colletti CJ, Wolfe-Christensen C, Carpentier MY, Page MC, McNall-Knapp RY, Meyer WH, et al. The relationship of parental overprotection, perceived vulnerability, and parenting stress to behavioral, emotional, and social adjustment in children with cancer. Pediatr Blood Cancer. 2008;51:269–74. doi: 10.1002/pbc.21577. [DOI] [PubMed] [Google Scholar]
- 19.Hurley KM, Black MM, Papas MA, Caulfield LE. Maternal symptoms of stress, depression, and anxiety are related to nonresponsive feeding styles in a statewide sample of WIC participants. J Nutr. 2008;138:799–805. doi: 10.1093/jn/138.4.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shin HS, Kim JM. Analysis of relationships between parenting stress, maternal depression, and behavioral problems in children at risk for Attention Deficit Hyperactive Disorder. J Korean Acad Nurs. 2010;40:453–61. doi: 10.4040/jkan.2010.40.3.453. [DOI] [PubMed] [Google Scholar]
- 21.Herring S, Gray K, Taffe J, Tonge B, Sweeney D, Einfeld S. Behaviour and emotional problems in toddlers with pervasive developmental disorders and developmental delay: Associations with parental mental health and family functioning. J Intellect Disabil Res. 2006;50:874–82. doi: 10.1111/j.1365-2788.2006.00904.x. [DOI] [PubMed] [Google Scholar]
- 22.van der Oord S, Prins PJ, Oosterlaan J, Emmelkamp PM. The association between parenting stress, depressed mood and informant agreement in ADHD and ODD. Behav Res Ther. 2006;44:1585–95. doi: 10.1016/j.brat.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 23.Lecavalier L, Leone S, Wiltz J. The impact of behavior problems on caregiver stress in young people with autism spectrum disorders. J Intellect Disabil Res. 2006;50:172–83. doi: 10.1111/j.1365-2788.2005.00732.x. [DOI] [PubMed] [Google Scholar]
- 24.Seltzer MM, Greenberg JS, Floyd FJ, Hong J. Accommodative coping and well-being of midlife parents of children with mental health problems or developmental disabilities. Am J Orthopsychiatry. 2004;74:187–95. doi: 10.1037/0002-9432.74.2.187. [DOI] [PubMed] [Google Scholar]
- 25.Singer GH. Meta-analysis of comparative studies of depression in mothers of children with and without developmental disabilities. Am J Ment Retard. 2006;111:155–69. doi: 10.1352/0895-8017(2006)111[155:MOCSOD]2.0.CO;2. [DOI] [PubMed] [Google Scholar]


