Abstract
Background:
Conducted researches show that psychological factors may have a very important role in the etiology, continuity and consequences of coronary heart diseases. This study has drawn the psychological risk and protective factors and their effects in patients with coronary heart diseases (CHD) in a structural model. It aims to determine the structural relations between psychological risk and protective factors with quality of life in patients with coronary heart disease.
Materials and Methods:
The present cross-sectional and correlational studies were conducted using structural equation modeling. The study sample included 398 patients of coronary heart disease in the university referral Hospital, as well as other city health care centers in Isfahan city. They were selected based on random sampling method. Then, in case, they were executed the following questionnaires: Coping with stressful situations (CISS- 21), life orientation (LOT-10), general self-efficacy (GSE-10), depression, anxiety and stress (DASS-21), perceived stress (PSS-14), multidimensional social support (MSPSS-12), alexithymia (TAS-20), spiritual intelligence (SQ-23) and quality of life (WHOQOL-26).
Results:
The results showed that protective and risk factors could affect the quality of life in patients with CHD with factor loadings of 0.35 and −0.60, respectively. Moreover, based on the values of the framework of the model such as relative chi-square (CMIN/DF = 3.25), the Comparative Fit Index (CFI = 0.93), the Parsimony Comparative Fit Index (PCFI = 0.68), the Root Mean Square Error of Approximation (RMSEA = 0.07) and details of the model (significance of the relationships) it has been confirmed that the psychocardiological structural model of the study is the good fitting model.
Conclusion:
This study was among the first to research the different psychological risk and protective factors of coronary heart diseases in the form of a structural model. The results of this study have emphasized the necessity of noticing the psychological factors in primary prevention by preventive programs and in secondary prevention by rehabilitation centers to improve the quality of life of the people with heart diseases.
Keywords: Coronary heart disease, protective, Psycho-Cardiology, Psychological risk factors, structural model
INTRODUCTION
Coronary heart disease (CHD) is the leading cause of global mortality, which is also responsible for 33% of deaths in people under 65, and 28% of all deaths.[1,2,3] Although previous studies have mostly focused on the role of biological factors in this disease, recent studies suggest a new holistic paradigm[4] (biological, psychological, social and spiritual) in clinical care for patients with coronary heart disease. This has led to greater attention being directed to the role of psychological factors in the etiology, progression, continuity, and consequences of this disease.[5,6,7]
Anxiety, depression, and stress are among the most important psychological risk factors for coronary heart disease.[8,9,10,11,12,13,14] According to epidemiological and research evidence, these risk factors, even after controlling biological risk factors such as cholesterol levels and blood pressure, are the predictors of morbidity, decreased quality of life, and even death in CHD patients.[12,15] Pessimism is also a negative risk factor for CHD; and there is a negative relationship between CHD risk, decreased quality of life, pessimism and negative mood.[16,17] Alexithymia, or inability to express emotions, is another risk factor for CHD. Alexithymic people are usually unable to identify, understand, and describe their emotions.[18,19] The relationship between alexithymia, depression, and anxiety has also been the subject of several studies.[20]
As a defense shield and in parallel with CHD risk factors, protective factors in the field of positive psychology can prevent or moderate the impacts of risk factors on patients’ quality of life through increasing abilities and positive experiences.[21] In this regard, strategies to cope with stress could be mentioned as some examples. The patients who stay active after a heart disease and use problem-focused strategies to deal with problems will get better results on health promotion and improvement of the quality of their life in the long term. Although emotion-focused strategies might be helpful in coping with disease as the effects are short term, they will cause stress, discomfort, and finally anxiety that are long term.[22] As a kind of positive attributional style, optimism is also a dimension of life orientation leading to positive expectations of self, others, and future, which is related to the improvement of the quality of life and reduction of cardiovascular disease symptoms.[23,24] Moreover, there is a relationship between positive and optimistic emotions and reduction in abnormal physiological biomarkers such as reduced activity of autonomic nervous system and reduced inflammation.[25] Self-efficacy is an important protective factor for cardiovascular diseases. It can, on the one hand, enhance people's ability to control and manage their own behaviors,[26,27,28] and on the other hand, prevent the impacts of risk factors such as anxiety, depression, and stress, leading to useful changes and improvements in patients’ lifestyle. In patients with heart disease, studies on self-efficacy are mostly focused on the successful role of cardiac rehabilitation[29,30] in enhancing people's ability to manage stress, do physical activities, and finally improve self-efficacy.[31] As an important aspect of humanistic action related to reliability and health and improvement of the quality of life resulting in less disease and longer lifespan, much attention has been paid to spirituality in recent years.[32,33] The study on the relationship between spirituality and CHD showed that higher and lower levels of spirituality were accompanied by less and more progressions of CHD within 4 years, respectively.[34]
Quality of life is also considered as one of the main objectives in the prevention and treatment of cardiovascular diseases. It is highly important in terms of both the results obtained from the evaluation of medical tests, reviewing and recognizing medical decisions for each individual.[35] Poor quality of life is accompanied by worse disease severity, lower survival rate, increased number of hospitalizations, and decreased activity and function among patients with heart diseases.[36,37] Therefore, quality of life has been considered as an important indicator of health resulting in therapeutic interventions in all these studies. By proposing a biological, psychological, and behavioral model, Wulsin (2012) showed that psychological factors such as depression, anxiety, chronic and acute stress, poverty, hostility, occupational restrictions, and anger could lead to the emergence of behavioral factors such as cigarette smoking, physical inactivity, obesity, lack of social support, and decreased quality of life, which altogether provide the context for CHD.[38] Given that few studies have been conducted in Iran on providing a comprehensive psychological model for risk and protective factors for CHD and its application on the treatment protocol for CHD patients, conducting a study by providing a comprehensive psychological model for primary prevention of CHD for the general public, and secondary prevention of CHD for patients with heart diseases seemed necessary.
MATERIALS AND METHODS
This was a cross-sectional and correlational study (2013) and has provided a structural model of psychological risk protective factors of coronary heart disease as a psycho-cardiology structural model. The study sample included 398 patients of coronary heart disease in the university referral Hospital, as well as other city health care centers in Isfahan city. The samples were selected randomly. The Satorra-Saris method was used for further accuracy and reliability in the estimation of sample size of the estimated main parameters.[39] CHD patients with medical records fitting the study criteria (including minimum literacy level, age group 30-70, and history of heart disease from 6 months up to 5 years) were selected. Then the selected patients were invited to participate in the study by phone. Moreover, a free blood test was considered for the patients to motivate them and compensate for their cooperation. Some of the patients declared their readiness to participate in the study. Some of the patients were then invited to Isfahan Cardiovascular Research Institute to complete the questionnaire every day for 3 months. Before completing the questionnaires, the patients were told about the necessary points to complete them. They were also assured that the results would not be published individually by their names. The questionnaires were given to the subjects in booklet form and if they had any question or if the questions were ambiguous, the tester was responsible for it. The questions were read and necessary explanations were provided for those who had trouble reading and understanding the questions. After the questionnaires were completed, they were completely checked for unanswered questions. If there were any unanswered questions, the questionnaire was given to the patients to be completed. The patients were not allowed to take the questionnaires home, and the questionnaire was time limited. The inclusion criteria were as follows:
A confirmation by a cardiologist and an angiography test that patients were with coronary disease.
Minimum literacy level.
Age group 30-70
History of heart disease from 6 months up to 5 years.
The exclusion criteria were as follows:
Non-compliance with the inclusion criteria.
Lack of understanding the study questions.
Unwillingness to continue answering the questions.
Flawed or incomplete questionnaire.
Based on this, the patients were asked to complete nine questionnaires. These questionnaires included: Depression, anxiety and stress variables (DASS-21), strategies of coping (CISS-21), alexithymia (TAS-20), life orientation (LOT-10), general self-efficacy (GSE-10), perceived stress (PSS-14), social support (MSPSS-12), quality of life (WHOQOL-26) and spiritual intelligence (SQ-23). The research questionnaires were as follows:
Depression, anxiety and stress scale (DASS-21):[40] The scale is a set of with three sub-scales of self-reporting for the evaluation of negative emotional states of depression, anxiety and stress. The important application of this scale is measuring the intensity of the symptoms of major depression, anxiety and stress. The reliability coefficient of the test was equal to 89 percent by using the Cronbach's alpha coefficient.
Short form questionnaire of coping with stressful situations (CISS-21):[41] This scale was made by Calsbeek and colleagues based on the original questionnaire of coping with stressful situations. This scale is for evaluating the main three coping styles. 1- Task oriented coping, to control the emotions and planning for step-by-step problem solving (7 items), 2- Emotion oriented coping, that is, instead of focusing on the problem, it is focused on its excitements or in other words, reducing the negative emotions instead of solving the problem (7 items) and 3- Avoidance oriented coping style, in that the person avoids ways of dealing with the problem (7 items). Responses adjusted in a Likert type five degrees scale (never = 1 to very often = 5). Reliability of this scale in the present study was 72 percent in terms of Cronbach's alpha coefficient.
Life orientation questionnaire (LOT-10):[42] This test is a 10-item questionnaire. The items of 2, 5, 6 and 8 are misleading without belonging any scores to them. The reliability coefficient of the test by using Cronbach's alpha was 74 percent in the present study.
Perceived stress scale (PSS-14): This questionnaire[43] was provided by Cohen et al., in 1983 in order to measure the perceived general stress during the past one month. The questionnaire measures the thoughts and feelings about stressful life events, controlling, overcome and coping with stress and stressful experience.
Toronto alexithymia questionnaire (TAS-20): This questionnaire was developed by Bagby et al., (1994)[44] and the questionnaire is a survey with 20 questions. It is divided into three dimensions, difficulty in diagnosis and identifying the feelings (7 questions), difficulty in describing the feelings (5 questions) and focus on external experiences (8 questions). The reliability of this test was equal to 74 percent by using Cronbach's alpha coefficient in the present study.
General self-efficacy scale (GSE-10): This scale was built by Schwartzer and Jerusalem (1995)[45] in order to assess general and social self-efficacy. This questionnaire has 10 items for evaluating general self-efficacy. The reliability of the test was 82 percent by using Cronbach's alpha coefficient in the present study.
Multidimensional scale of perceived social support (MSPSS): It is a tool with 12 phrases to assess the perceived social support from three sources of family, friends and the significant people in their lives. It is designed by ZIMET et al., (1988).[46] The reliability of the test was 87 percent by using Cronbach's alpha coefficient in the present study.
WHOQOL-BREF questionnaire:[47] This questionnaire has 26 questions in four domains of physical health, mental health, social relations and environment health (each of the domains has 3, 6, 7 and 8 questions, respectively). The reliability coefficient of the test by using Cronbach's alpha in the present study was 90%.
-
Spiritual intelligence questionnaire (SQ-23): The questionnaire was developed by Yousefy and Khayyam Nekouei[48] (2013) consisting of two subscales:
- Relationship to self
- Relationship to others. The reliability coefficient of the test by using Cronbach's alpha in the present study was 83 percent, which is indicative of high reliability of this test.
Psycho-cardiology structural model
Psycho-cardiology structural model with the variables of (LOT, CISS, TAS, DASS, SQ, PSS, GSE, WHOQOL-Bref, and MSPSS) was plotted by using Asset Management Operating System (AMOS21) SPSS, an IBM Company: Chicago, U.S. Software and the method of maximum likelihood (ML). The assumptions of maximum likelihood method were evaluated with the multivariate normality and adequate sample size for psycho-cardiology structural model. It is presented in Figure 1. In order to achieve the best fit, necessary modifications were applied in the model.
Figure 1.
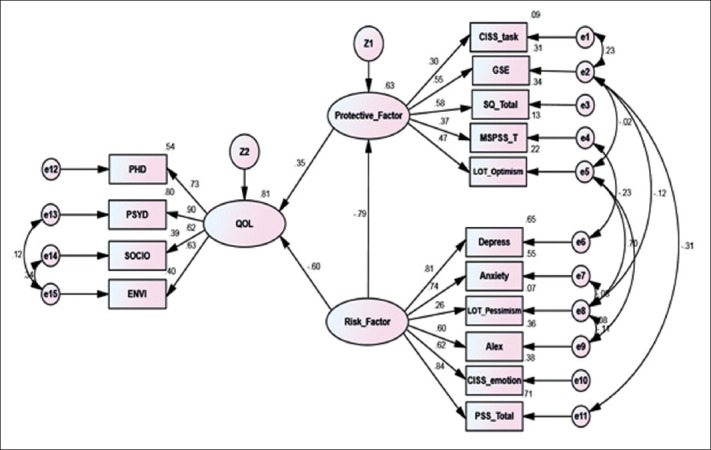
A Psycho-cardiology structural model
Statistical analysis
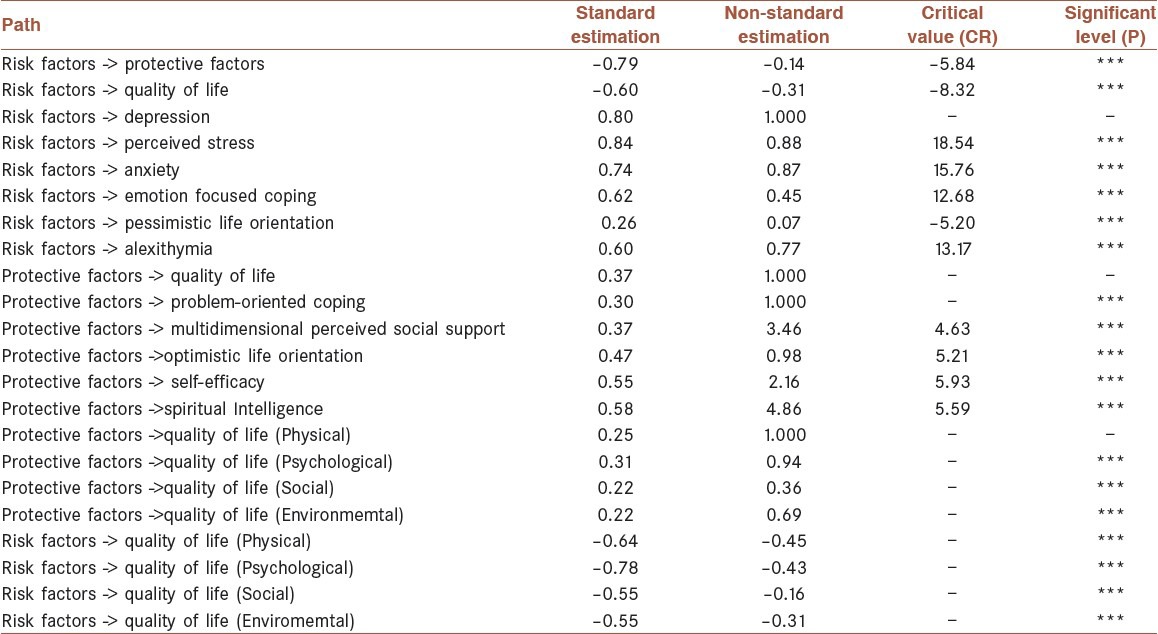
After implementing the questionnaires, the data were entered into SPSS21. Then after the data were completely edited, initial calculations (descriptive statistics) were performed using SPSS21. The structural model of psychocardiology was designed based on a holistic medicine approach (biological, psychological, social and spiritual) and then drawn in AMOS21. Necessary modifications were made on the model to achieve the best fitting. To evaluate the model fit indices, framework and detailed aspects of the model were examined. Tables 1 and 2 present the framework and details of the model, respectively. In reviewing the framework, the most important fit indices are absolute, comparative, and parsimony indices. The relative chi square (CMIN/DF<5), the Comparative Fit Index (CFI>0.90), the Parsimony Comparative Fit Index (PCFI>0.50), and the Root Mean Square Error of Approximation (RMSEA<0.08) indicate that the framework of the model is confirmed. In reviewing the details, significance of the relationships is estimated based on the level of significance.[49] As seen in Table 2, given that P-value is lower than 0.001 (P < 0.001) and less than 0.05, all relationships are significant.
Table 1.
Overall fit indices for the original and the modified models
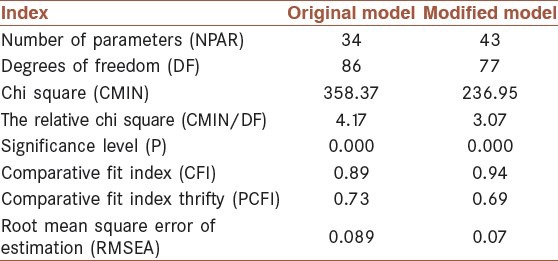
Table 2.
Total effects Standard and Non-standard
RESULTS
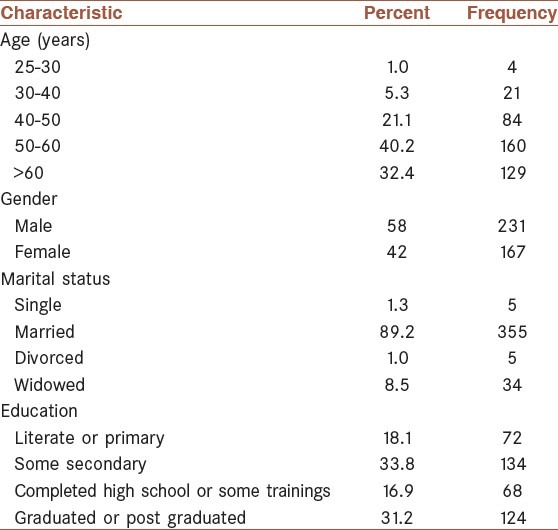
The present study was carried out based on a holistic approach (biological, psychological, social and spiritual). The study samples included 398 CHD patients in Isfahan Cardiovascular Research Institute. Table 3 shows the sample descriptive indices such as frequency, and valid percent and the socio-demographic characteristics based on age, gender, marital status and education. Table 3 shows that from ‘among the 5 age groups’, the 50-60 age group had the highest frequency (160 individuals), which was 40.2% of the whole sample (398 individuals). From ‘among male and female groups’, males had the highest frequency (231 individuals) in the gender group (58%). From ‘among the 4 groups of married, single, divorced, and widowed’, the married had the highest frequency (355 individuals) in the marital status groups (89.2%). From ‘among the 4 education groups’, the secondary education group (134 individuals) had the highest frequency (33.8%).
Table 3.
Patients’ socio-demographic characteristics (n = 398)
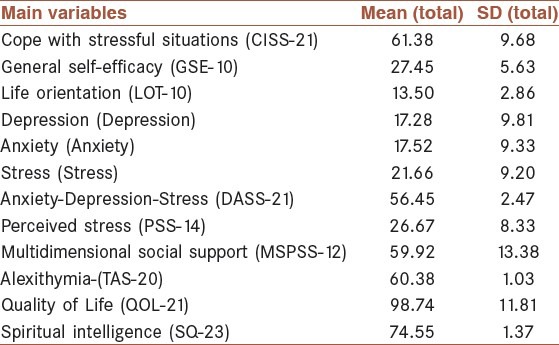
The descriptive indicators of the main variables of the study, the mean and standard deviation have been reported in Table 4.
Table 4.
Mean and standard deviation of the study main variables
To investigate the significance or insignificance of the structural relationships, Tables 1 and 2 show the framework and details of the model, respectively. The summary of the results for the two original and modified models are shown in Table 2. The table reports some of the most important overall fit indices so that the model could be assessed by different values.
It was reported in this table about some of the most important indicators of overall fitness to assess its different amounts of the model. The summary of the results for the two original and modified models are shown in Table 2. The table reports some of the most important overall fit indices so that the model could be assessed by different values.
As it was shown in Table 1, due to the relative chi square of the final modified model equal to 3.25, which is less than 5, Comparative Fit Index (CFI) as 0.93 and greater than 9.0, Parsimony Comparative Fit Index (PCFI) of 0.68 and greater than 0.50, the Root Mean Square Error of Approximation than 0.08 (RMSEA = 0.07), thus the model of psychological risk and protective factors for Coronary heart diseases had a good fit. The results of standard and non-standard estimated factor loadings for the psycho-cardiology model, which was reported in Table 2.
The partial fit indices [critical ratio (CR) and level of significance (P)] showed that all the factor loadings were significant. In Table 2, variables of perceived stress, depression and anxiety with the values of 0.84, 0.80 and 0.74, respectively had the highest factor loadings on risk factors. The lowest factor loading was related to pessimistic life orientation with the value of 0.26. In addition, among the protective factors of coronary heart disease, spiritual intelligence with a factor loading of 0.58 had the maximum value and the lowest factor loading was related to problem-focused coping with the value of 0.30. By referring to Table 2, the details of the model are also approved. The results obtained from the details of the model also showed that psychological risk and protective factors affect CHD patients’ quality of life with factor loadings of −0.60 and 0.35, respectively. As a result, protective factors (0.35) could improve CHD patients’ quality of life, and risk factors (0.60) could decrease their quality of life. Therefore, given that the details (significance of the relationships) and framework (fit indices within the acceptable range) of the model have been confirmed, the psychocardiology model of the study is good fitting model.
Tables 5 and 6 show the standardized direct and indirect effects of the variables.
Table 5.
Standardized Direct Effects
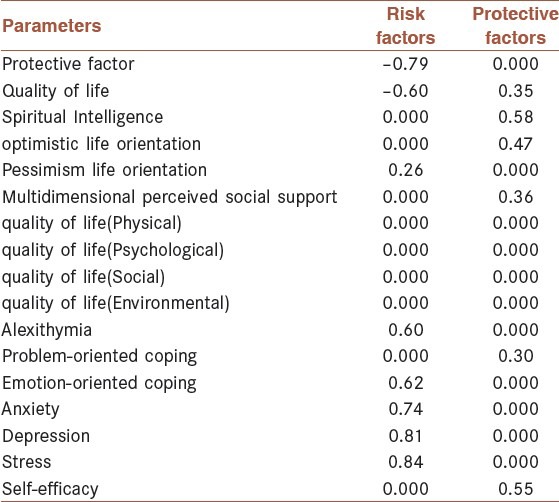
Table 6.
Standardized Indirect Effects
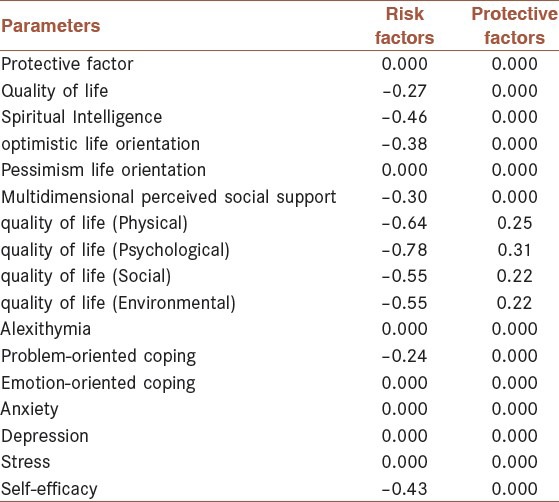
Table 5 shows the direct standard effects of the variables. As seen in Table 5, the direct minimum factor loading on risk factors is 0.26, which is related to pessimistic life orientation, and the direct highest factor loading is 0.84, which is related to stress. Moreover, the minimum factor loading on protective factors is 0.30, which is associated with problem-focused coping and the maximum factor loading is 0.58, which is related to spiritual intelligence.
Table 6 shows the indirect standard effects of the variables. As seen in Table 6, the indirect minimum factor loading on risk factors is −0.24, which is related to problem-focused coping, and the indirect highest factor loading is −0.46, which is related to spiritual intelligence. Most of the indirect effects on protective factors is also zero except the indirect effects of various dimensions of quality of life, including physical, psychological, social and environmental dimensions, which are 0.25, 0.31, 0.22, 0.22, respectively.
DISCUSSION
The results of this study, after a thorough analysis of the obtained data from 398 patients (2013) with coronary heart diseases demonstrated that the hypothetical psycho-cardiology model was a good fit. The results of this model suggested that psychological risk factors and protective with a load factor of −0.60 and 0.35 had a very important role on the quality of life of the patients with coronary heart disease. Quality of life, from long time ago, in clinical trials has been raised as the result and outcome of the treatment interventions. Thus, the quality of life is an important indicator in evaluating the health of patients.[50,51] Keeping up the quality of life has an important role on the fast recovery of the patients to normal life, reducing the complications and preventing the recurrences of heart diseases. Therefore, it is necessary to pay more attention to risk factors and protective factors for quality of life in CHD patients. Citing numerous studies, risk factors and protection play a very important role in chronic diseases and especially the heart disease.[7] In this regard, the present study by providing a psycho-cardiology structural model it has investigated the risk factors and protective factors of coronary artery disease. As it might be expected, in the clustering of risk factors and consistent with previous research, it was revealed the role of anxiety, depression and perceived stress with factor loadings of 0.74, 0.80 and 0.84, respectively had played important role on risk factors. These results were consistent with those studies, which pose anxiety, depression and stress as the three most important risk factors for coronary artery disease that can reduce the quality of life of the patients.[8,9,10,11,12,13,14,15] Other findings showed that pessimistic orientation had factor load of 0.26 on the risk factors. This finding was consistent with the findings of Murphy study (2000),[52] which reported the risk of coronary artery disease in the pessimists as nine times. Alexithymia has also been discussed as a relatively strong risk factor with the factor loading of 0.60 on risk factors. Several other studies have mentioned about alexithymia as a risk factor for psychosomatic diseases. In recent years, the relationship between alexithymia with anxiety and depression has been shown in many studies.[53,54] Alexithymia is an emotional-cognitive characteristic trait. People with alexithymia in facing with a stressful and traumatic event have limited ability to cope with stressful situations, non-compliance with conditions and disability to express emotions lead to experiencing negative emotions such as depression and anxiety, which will consequently result in decreased quality of life among patients.
Among other risk factors for coronary artery disease are emotion-focused strategies in facing with stress. In this regard, the results of the present study have demonstrated the relationship of emotion-focused coping in the reduction of quality of life of coronary heart disease patients. The factor loading of this variable on the risk factors was 0.62. These results were consistent with the previous studies.[55] Much research has shown the role of social support on the etiology and prognosis of coronary artery disease. Barth et al., research (2010)[9] emphasized that not just the lack of social support played a role in the etiology and prognosis of coronary artery disease, but also low social support, even in healthy people, affecting the incidence of myocardial infarction and in general, on all types of deaths. Social support and lack of social support as important variables have been discussed in the role of protective factor and risk factor in coronary artery disease. In this regard, the present study also showed that social support with a causal relationship of 0.37 had an important role in the protective factors for coronary heart diseases. The results also were consistent with the research of Kawachi et al., (1996).[56] Lofvenmark and colleagues (2009)[57] and Barth et al.,(2010)[58] about the role of social support in the etiology and prognosis of coronary heart disease and the relationship of social support with myocardial infarction and mortality. These results were probably due to the golden role of social support from the positive perception about available community resources and as a protective factor in dealing with stress in terms of therapeutic interventions and improving the individuals’ beliefs and feelings.[56,57,58] Among the other results of the study was the significant relationship 0.47 of optimism with protective factors for coronary heart diseases. Many studies have discussed about the role of optimism as a positive factor, which is associated with the reduction of autonomic system activity and ultimately reducing the cardiovascular symptoms. It appears that the role of optimism can be explained by increasing the positive expectations of people, paying more attention to lifestyle modification and medical care for coronary artery disease. This study showed that the total of factor loadings of protective factors for coronary artery disease was 0.35 on the quality of life.
Moreover, problem-focused coping with a factor loading of 0.30 belongs to the cluster of protective factors. This result was consistent with the results of earlier research, which demonstrated that the patients using problem-oriented approaches experienced better results in long-term for their health promotion and the quality of their lives.[22,55] Efficacy is also among the important variables of protective factors. In the present study, it had a 0.55 relationship with protective factors for coronary heart diseases. This result was also consistent with earlier findings.[28,29,30,31] These results have been probably due to the very important role of self-efficacy on the management and control of behaviors, physical activities and drug use and in general, adopting a healthy lifestyle in the heart patients. Spiritual Intelligence with a correlation of 0.58 with protective factors had an important role on the quality of life of coronary heart disease too. This result was also consistent with the research results of Macdonald (2002), Emmons (2000) regarding the role of spirituality on one's health and Morris (2001) about the relationship between spirituality and coronary heart disease.[32,33,34]
CONCLUSIONS
The psychocardiology structural model in the present study showed that psychological factors had a very important role on the quality of life of the coronary heart disease (CHD). The results of this study emphasized on the necessity of paying more attention to psychological factors in primary prevention level in reference to the public welfare and quality of life in general. In the secondary prevention level, it should be noticed that the aspects are related tohealth promotion in particular and based on a holistic view, setting up a comprehensive bio-psycho-social-spiritual treatment protocol in the health centers of CHD and application of this ideal features.
ACKNOWLEDGMENT
The authors’ deepest gratitude goes to all the patients who participated in the study and the authorities of the Isfahan Cardiovascular Research Institute, Chamran Heart Hospital, Noor and Ali Asghar Hospitals, and other Medical Centers that helped in the process of this research. The present paper is adapted from a Ph.D thesis in Isfahan Sciences and Research Branch, Islamic Azad University, supported by Isfahan Cardiovascular Research Institute.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
REFERENCES
- 1.Ko M, Kim MT, Nam JJ. Assessing risk factors of coronary heart disease and its risk prediction among Korean adults: The 2001 Korea National Health and Nutrition Examination Survey. Int J Cardiol. 2006;110:184–90. doi: 10.1016/j.ijcard.2005.07.030. [DOI] [PubMed] [Google Scholar]
- 2.Ingelsson E, Schaefer EJ, Contois JH. Clinical utility of different lipid measures for prediction of coronary heart disease in men and women. JAMA. 2007;298:776–85. doi: 10.1001/jama.298.7.776. [DOI] [PubMed] [Google Scholar]
- 3.Baruah DK. What is the cardiac disease. 2010. [Last accessed on 2010 Aug 29]. Available from: http://www.dkbaruah-cardiology.com .
- 4.Barnes J, Abbot NC, Harkness EF, Ernest E. Articles on complementary medicine in the mainstream medical literature: An investigation of Medline, 1966 through 1996. Arch Intern Med. 1999;159:1721–5. doi: 10.1001/archinte.159.15.1721. [DOI] [PubMed] [Google Scholar]
- 5.Kaplan JR, Manuck SB. Using ethological principles to study psychosocial influences on coronary atherosclerosis in monkeys. Acta Physiol Scand Suppl. 1997;640:96–9. [PubMed] [Google Scholar]
- 6.Ketterera MW, Mahra G, Goldbergb AD. Psychological factors affecting a medical condition ischemic coronary heart disease. J Psychosom Res. 2000;48:357–67. doi: 10.1016/s0022-3999(00)00099-4. [DOI] [PubMed] [Google Scholar]
- 7.Vitaliano PP, Scanlan JM, Zhang J, Sarage MV, Hirsch IB, Siegler IC. Path model of chronic Stress, the metabolic syndrome and coronary heart disease. Psychosom Med. 2002;64:418–35. doi: 10.1097/00006842-200205000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Rumfeld JS, Harranek E, Masoudi FA, Petrson ED, Jones P, Tooley JF, et al. Cardiovascular Outcomes Research Consortium. Depressive symptoms are the strongest predictors of short-term declines in health status with heart failare. J Am Coll Cardiol. 2003;42:1811–7. doi: 10.1016/j.jacc.2003.07.013. [DOI] [PubMed] [Google Scholar]
- 9.Barth J, Sheneider S, Kanel R. Lack of Social Support in the Etiology and the Prognosis of Coronary Heart Disease: A Systematic Review and Meta-Analysis. Psychosom Med. 2010;72:229–38. doi: 10.1097/PSY.0b013e3181d01611. [DOI] [PubMed] [Google Scholar]
- 10.Denollet J, Freedland KE, Carney RM, de Jonge P, Roest AM. Cognitive-affective symptoms of depression after myocardial infarction: Different prognostic importance across age groups. Psychosom Med. 2013;75:701–8. doi: 10.1097/PSY.0b013e31829dbd36. [DOI] [PubMed] [Google Scholar]
- 11.Khayyam Nekouei Z, Yousefy A. Application of cognitive - behavioral therapy for reducing anxiety in cardiac patients. Arya Atherosclerosis J. 2007;3:69–71. [Google Scholar]
- 12.Janszky I, Ahnve S, Landberg I, Hemmingsson T. Early onset depression, anxiety, and risk of subsequent coronary heart disease. J Am Coll Cardiol. 2010;56:31–7. doi: 10.1016/j.jacc.2010.03.033. [DOI] [PubMed] [Google Scholar]
- 13.Bortman D, Golden SH, Wittstein IS. The cardiovascular toll of stress. Lancet. 2007;370:1089–100. doi: 10.1016/S0140-6736(07)61305-1. [DOI] [PubMed] [Google Scholar]
- 14.Kurd BJ, Dar MI, Shoaib M, Malik L, Aijaz Z, Asif I. Relationship between stress and coronary heart disease. Asian Cardiovasc Thorac Ann. 2014;22:142–47. doi: 10.1177/0218492312469803. [DOI] [PubMed] [Google Scholar]
- 15.Khayyam-Nekouei Z, Neshatdoost H, Yousefy A, Sadeghi M, Manshaee G. Psychological factors and coronary heart disease. ARYA Atheroscler. 2013;9:102–11. [PMC free article] [PubMed] [Google Scholar]
- 16.Asimakopoulou K, Skinner TC, Spimpolo J, Marsh S, Fox C. Unrealistic pessimism about risk of coronary heart disease and stroke in patients with type 2 diabetes. Patient Educ Couns. 2008;71:95–101. doi: 10.1016/j.pec.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 17.Cohen BE, Panguluri P, Na B, Whooley MA. Psychological risk factors and the metabolic syndrome in patients with coronary heart disease. Psychiatry Res. 2008;175:133–72010. doi: 10.1016/j.psychres.2009.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Valkamo M, Hintikka J, Honkalampi K, Nikanen L, Koviumaa - Honkanen L, viinamaki H. Alexithymia in patients with coronary heart disease. J Psychosom Res. 2001;50:125–30. doi: 10.1016/s0022-3999(00)00209-9. [DOI] [PubMed] [Google Scholar]
- 19.Lumley MA, Neely LC, Burger AJ. The assessment of Alexithymia in medical settings: implications for understanding and treating health problems. J Pers Assess. 2007;89:230–46. doi: 10.1080/00223890701629698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berthoz S, Consoli S, Perez-Diaz F, Jouvent R. Alexithymia and anxiety: Compounded relationships? A psychometric study. Eur Psychiatry. 1999;14:372–8. doi: 10.1016/s0924-9338(99)00233-3. [DOI] [PubMed] [Google Scholar]
- 21.Linley AP, Joseph S, Harrington S, Wood AM. Positive psychology: Past, present, and (possible) future. J Posit Psychol. 2006;1:3–16. [Google Scholar]
- 22.Sheen BJ, Mayers HF, Mccrae CP. Psycho - Social Predictors of cardiac Qol Outcomes. J Psychosomatic. 2006;6:3–11. [Google Scholar]
- 23.Tindle H, Davis E, Kuller L. Attitudes and cardiovascular disease. Maturitas. 2010;67:108–13. doi: 10.1016/j.maturitas.2010.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tindle HA, Chang YF, Kuller LH, Manson JE, Robinson JG, Rosal MC, et al. Optimism, cynical hostility and incident coronary heart disease and mortality in women's health initative. Circulation. 2009;120:656–62. doi: 10.1161/CIRCULATIONAHA.108.827642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Steptoe A, Wright C, Kunz-Ebrecht SR, Iliffe S. Dispositional optimism and health behaviour in community-dwelling older people: Associations with healthy ageing. Br J Health Psychol. 2006;11(Pt1):71–84. doi: 10.1348/135910705X42850. [DOI] [PubMed] [Google Scholar]
- 26.Grossarth R, Eysenk HJ. Self-regulation and mortality from cancer, coronary heart disease, and other causes: A prospective study. Person in divid. 1995;19(6):781–95. [Google Scholar]
- 27.Kara M, Astil T. Effect of education on self-efficacy of Turkish patients with chronic obstructive pulmony disease. Patient Educ Couns. 2004;55:114–20. doi: 10.1016/j.pec.2003.08.006. [DOI] [PubMed] [Google Scholar]
- 28.Sol GM, van der Graaf Y, van Petersen R, Visseren LJ. The effect of self efficacy on Cardiovascular lifestyle. Eur J Cardiovasc Nurs. 2011;10:180–6. doi: 10.1016/j.ejcnurse.2010.06.005. Available from: http://www.elsevier.com/locate/ejcnurse . [DOI] [PubMed] [Google Scholar]
- 29.Gardner JK, Mcconnell T, kinger T, Herman CP, Hauck CA, Laubach CA. Quality of life and self efficancy: Gender and diagnosis consideration for management during cardiac rehabilitation. J Cardiopulm Rehabil. 2003;23:299–306. doi: 10.1097/00008483-200307000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Izawa KP, Watanabe S, Omiya K, Hirano Y, Oka K, Osada N. Effect of the self-monitoring approach on exercise maintenance during cardiac rehabilitation: A randomized, controlled trial. Am J Phys Med Rehabil. 2005;84:313–21. doi: 10.1097/01.phm.0000156901.95289.09. [DOI] [PubMed] [Google Scholar]
- 31.Berkhuysen MA, Nieuwland W, Buunk BP, Sanderman R, Rispens P. Change in self-efficacy during cardiac rehabilitation and the role of perceived overpretectiveness. Patient Educ Couns. 1999;38:21–32. doi: 10.1016/s0738-3991(98)00115-3. [DOI] [PubMed] [Google Scholar]
- 32.Macdonald JJ. Torento, Canada: 2002. Spiritual Health in older men. Proceeding of the 1th on Seminar Older men and Community. [Google Scholar]
- 33.Emmons AR. Spirituality and intelligence: Problems and prospects. Int Psychol Relig. 2000;10:57–64. [Google Scholar]
- 34.Morris EL. The relationship of spirituality to coronary heart disease. Altern Ther Health. 2001;1:7:96–8. [PubMed] [Google Scholar]
- 35.Coelho R, Romas S, Prata J, Bettenourt P. Heart failure and health related quality of life. [Last accessed on 2006 Sep 11];Clin Pract Epidemiol Ment Health. 2006 1:1–19. doi: 10.1186/1745-0179-1-19. Available from: http://www.cepementalheath.com/content/1/1/19 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hofer S, Lim L, Guyatt G, Oldridge N. The Macnew Heart disease health -related quality of life instrument. Health Qual Life Outcomes. 2004;2:3. doi: 10.1186/1477-7525-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Havik QE, Sivertsen B, Relbo A, Hellesvik M, Grov I, Geiran O. Depressive symptoms and all-cause mortality after heart transplantation. Transplantation. 2007;84:97–103. doi: 10.1097/01.tp.0000268816.90672.a0. [DOI] [PubMed] [Google Scholar]
- 38.Dornelas EA, editor. Springer Science+Business Media, LLC; 2012. Stress Proof the Heart: Behavioral Interventions for Cardiac Patients, 9. [Google Scholar]
- 39.Ghasemi V. Estimation of optimal sample size in structural equation models and assessment of their adequacy for social researchers. Iran J Sociol. 2011;12:138–61. [Google Scholar]
- 40.Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress cales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33:335–43. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- 41.Endler NS, Parker JD. Multidimensional assessment of coping: A critical evaluation. J Pers Soc Psychol. 1990;58:844–54. doi: 10.1037//0022-3514.58.5.844. [DOI] [PubMed] [Google Scholar]
- 42.Scheier MF, Carver CS. Optimism, coping and health: Assessment and implications of generalized outcome expectancies. Health Psychol. 1985;4:219–47. doi: 10.1037//0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- 43.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 44.Bagby RM, Parker JD, Taylor GJ. The twenty-item Toronto Alexithymia Scale-I. Item selection and cross-validation of the factor structure. J Psychosomatic Res. 1994;38:23–32. doi: 10.1016/0022-3999(94)90005-1. [DOI] [PubMed] [Google Scholar]
- 45.Schwarzer R, Jerusalem M. Wright S, Johnston M, Weinman J, editors. Generalized self-efficacy scale. Measures in Health Psychology: A User's Portfolio. Causal and Control Beliefs. 1995:35–7. [Google Scholar]
- 46.Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of perceived social support. J Pers Assess. 1988;52:30–41. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 47.Yousefy AR, Ghassemi GH, Sarrafzadegan N, Mallik S, Baghaei AM, Rabiei K. Psychometric properties of the WHOQOL-BREF in an Iranian adult sample. Community Ment Health J. 2010;46:139–47. doi: 10.1007/s10597-009-9282-8. [DOI] [PubMed] [Google Scholar]
- 48.Yousefy A, Khayyam Nekouei Z. Developing and validating a questionnaire for measuring the spiritual intelligence in Iran. Isfahan-Karbala Conference on Medical Education. Educational development for better health services. 2013:124. [Google Scholar]
- 49.Ghasemi V. Tehran: Sociologists Publication; 2010. Structural equation modeling in social researches using amos graphics. [Google Scholar]
- 50.Basu D. Quality of life issues in mental health care: Past, present and future. German J Psychiatr. 2004;7:35–430. [Google Scholar]
- 51.Kimberly M, Coracle B, Norman S, Endler M. Psychlogical perdictors of cardiac rehabilitation patient's. Qol J Applied Biobehav Res. 2003;8:26. [Google Scholar]
- 52.Murphy SL. Deaths: Final data for 1998. National Vital Statistics Report. 2000;48:1–106. [PubMed] [Google Scholar]
- 53.Motan I, Gencoz T. The relationship between the dimensions of alexithymia and the intensity of depression and anxiety. Turk Psikiyatri Derg. 2007;18:333–43. [PubMed] [Google Scholar]
- 54.Gallo LC, Shiva GG, Wendy SB. Emotions and cognitions in coronary heart disease: risk, resilience, and social context. Cognit Ther Res. 2004;28:669–94. [Google Scholar]
- 55.Daligtan AS, Dippel DW, Ribbers GM, van Balen R, Passchier J, Bussch bach JJ. Coping strategies as determinats of quality of life in strategies patients: A longitudinal study. Cerebrovasc Dis. 2007;23:401–7. doi: 10.1159/000101463. [DOI] [PubMed] [Google Scholar]
- 56.Kawachi I, Colditz GA, Ascherio AA. Prospective study of social networks in relation to total mortality and cardiovascular disease in men in the USA. J Epidimiol Community Health. 1996;50:245–51. doi: 10.1136/jech.50.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lofvenmark C, Mittiasson AC, Billing E, Edne M. Perceived loneliness and social support in patients with chronic heart failure. Eur J Cardiovasc Nurs. 2009;8:251–8. doi: 10.1016/j.ejcnurse.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 58.Barth J, Sheneider S, Kanel R. Lack of social support in the etiology and the prognosis of coronary heart disease: A systematic review and meta-analysis. Psychosom Med. 2010;72:229–38. doi: 10.1097/PSY.0b013e3181d01611. [DOI] [PubMed] [Google Scholar]


