Abstract
Background
Sentinel lymph nodes (SLNs) have been used to predict regional lymph node metastasis in patients with melanoma and breast cancer. However, the validity of the SLN hypothesis is still controversial for oesophageal cancer. We performed this meta-analysis to evaluate the feasibility and accuracy of radio-guided SLN mapping for oesophageal cancer.
Methods
A systematic search was conducted using MEDLINE, PubMed, EMBASE, Current Contents Connect, Cochrane library, Google scholar, Science Direct, and Web of Science. Original data was abstracted from each study and used to calculate a pooled event rates and 95% confidence interval (95% CI).
Results
The search identified 23 relevant articles. The overall detection rate was 0.93 (95% CI: 0.894-0.950), sensitivity 0.87 (95% CI: 0.811-0.908), negative predictive value 0.77 (95% CI: 0.568-0.890) and the accuracy was 0.88 (95% CI: 0.817-0.921). In the adenocarcinoma cohort, detection rate was 0.98 (95% CI: 0.923-0.992), sensitivity 0.84 (95% CI: 0.743-0.911) and the accuracy was 0.87(95% CI: 0.796-0.913). In the squamous cell carcinoma group, detection rate was 0.89 (95% CI: 00.792-0.943), sensitivity 0.91 (95% CI: 0.754-0.972) and the accuracy was 0.84 (95% CI: 0.732-0.914).
Conclusions
It is possible to identify and obtain a SLN before neoadjuvant therapy in oesophageal cancer. However, further work is needed to optimize radiocolloid type, refine the technique and develop a quick and accurate way to determine SLN status intraoperatively. This technique has to be further evaluated before it can be applied widely.
Keywords: Sentinel lymph nodes (SLNs), esophageal cancer, esophageal adenocarcinoma
Introduction
The incidence and mortality from cancer of all types in the United States has decreased during the 1991-2006 timeframe (1). However, the opposite is true for oesophageal cancer. Its incidence and mortality continue to rise. In 2010, estimated new cases of oesophageal cancer number 16,640 in the United States, while deaths total 14,500 (1). The United States has seen an average increase of 20.6% per year in the incidence of adenocarcinoma of the oesophagus since that time (2). This translates into a 463% and 335% increased incidence in white males and females, respectively, between 1975 and 2004. Adenocarcinoma now accounts for 58% of all oesophageal cancers in the United States. Total oesophageal cancer incidence and mortality have been increasing among white men, stable among white women, and decreasing in black men and women (3). It is projected that there will be 16,470 new patients diagnosed with oesophageal cancer and 14,280 deaths from it in 2008 (1).
Oesophageal cancer surgery is one of the most invasive types of gastrointestinal (GI) tract surgery. Due to the recent developments in lymph node metastasis diagnosis, endoscopic mucosal resection and less invasive surgery with thoracoscopic and laparoscopic technique has been possible in early-stage disease. However, because the sites of lymph node metastases are distributed extensively, it is sometimes difficult to focus on the removal of specific lymph nodes, even in superficial oesophageal cancer. The “fear” for the invisible micro metastasis prompted surgeons to perform more aggressive resections with lymphadenectomy to control the disease locally. Given this background, the concept of the sentinel lymph node (SLN), intraoperative lymphatic mapping and sentinel lymphadenectomy appears attractive.
Many studies have validated the sentinel node concept for cutaneous melanoma (4) and breast carcinoma (5,6). The dramatic impact of sentinel node biopsy on clinical practice, most notably for breast carcinoma, has led to recent successful attempts to extrapolate these techniques to other solid tumours including those of the GI tract (7,8). The SLN concept has revolutionized the approach to the surgical staging of both melanoma and breast cancer, and these techniques can benefit patients by avoiding various complications that may result from unnecessary prophylactic radical lymph node dissection in cases of negative SLNs for cancer metastasis. The basic technique used for SLN mapping involves injecting a tracer around the tumour and then following it to where it reaches the first drainage lymph node downstream from the tumour. In other words, the method simply entails the use of tracers and their respective detection devices.
Lymph node metastasis is not a rare event in oesophageal cancer, and the incidence of lymph node metastasis, even in pT1b tumours, reaches 45% (9). The other specific characteristics of oesophageal cancer is multidirectional lymphatic flow from the primary lesion, and the wide spread and random patterns of lymph node metastasis from cervical to abdominal areas. Actually, anatomic skip metastases to the second or third compartment of regional lymph nodes were found in 50% to 60% of oesophageal cancer (9). Based on these clinical observations, extended radical oesophagectomy with 3-field lymph node dissection has become recognized as a standard procedure in Japan, even for clinically node-negative cases (9,10). However, the oesophagectomy with 3-field lymph node dissection is one of the most invasive procedures in GI surgeries. A significant increase of morbidity and mortality after the invasive procedures has been reported (11).
The aim of this meta-analysis was to evaluate the feasibility, reliability, sensitivity and accuracy of sentinel node biopsy for adenocarcinoma, squamous cell carcinoma of the oesophagus.
Methods
Study protocol
We followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses PRISMA guidelines where possible in performing our systematic review (12). We performed a systematic search through MEDLINE (from 1950), PubMed (from 1946), EMBASE (from 1949), Current Contents Connect (from 1998), Cochrane library, Google scholar, Science Direct, and Web of Science to August 2013. The search terms included “Oesophageal cancer” AND “Sentinel Lymph Node Biopsy”, which were searched as text word and as exploded medical subject headings where possible. No language restrictions were used in either the search or study selection. The reference lists of relevant articles were also searched for appropriate studies. A search for unpublished literature was not performed.
Study selection
We included studies that met the following inclusion criteria:
Studies identifying the population of patients with oesophageal cancer who underwent SLN biopsy;
Studies that reported sensitivity, negative predictive value and other parameters.
Data extraction
We performed the data extraction using a standardized data extraction form, collecting information on the publication year, study design, number of cases, total sample size, population type, country, continent, mean age and clinical data. The event rate and confidence intervals were calculated.
Statistical analysis
Pooled event rate and 95% confidence intervals were calculated using a random effects model (13). We tested heterogeneity with Cochran’s Q statistic, with P<0.10 indicating heterogeneity, and quantified the degree of heterogeneity using the I2 statistic, which represents the percentage of the total variability across studies which is due to heterogeneity. I2 values of 25%, 50% and 75% corresponded to low, moderate and high degrees of heterogeneity respectively (14). The quantified publication bias using the Egger’s regression model (15), with the effect of bias assessed using the fail-safe number method. The fail-safe number was the number of studies that we would need to have missed for our observed result to be nullified to statistical non-significance at the P<0.05 level. Publication bias is generally regarded as a concern if the fail-safe number is less than 5n+10, with n being the number of studies included in the meta-analysis (16). All analyses were performed with Comprehensive Meta-analysis (version 2.0), Biostat, Englwood, NJ, USA [2005].
Results
The original search strategy retrieved studies (Figure 1). The abstracts were reviewed and after applying the inclusion and exclusion criteria, articles were selected for full-text evaluation. Of the articles selected, only 22 met full criteria for analysis and are summarised in Table 1. The years of publication ranged from 2002 to 2011.
Figure 1.
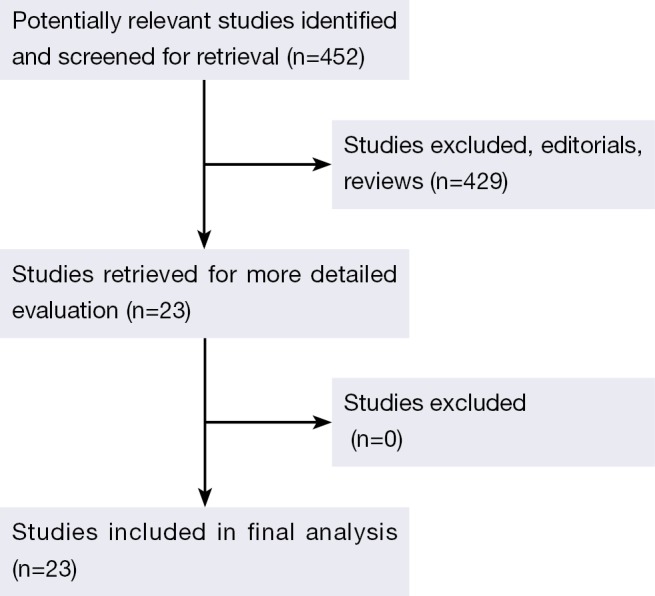
Flow of included studies.
Table 1. Characteristics of the 23 studies included in the systematic review and meta-analysis.
| Author (Ref) | Year | Country | Pathological variant | Radioisotope | Patients |
|---|---|---|---|---|---|
| Bhat et al. (17) | 2010 | India | SCC + ACA | Methylene blue | 32 |
| Yasuda et al. (18) | 2003 | Japan | SCC + ACA | 99m technetium tin colloid | 23 |
| Kato et al. (19) | 2003 | Japan | SCC | 99m technetium rhenium sulphide | 25 |
| Kitagawa et al. (20) | 2002 | Japan | SCC | 99m technetium tin colloid | 27 |
| Burian et al. (21) | 2004 | Germany | ACA | Methylene blue | 20 |
| Hayashi et al. (22) | 2006 | Japan | SCC + ACA | Iopamidol | 12 |
| Takeuchi et al. (23) | 2009 | Japan | SCC + ACA | Technetium-99m tin colloid | 75 |
| Yuasa et al. (24) | 2012 | Japan | ACA | Indocyanine Green Fluorescence | 20 |
| Uenosono et al. (25) | 2011 | Japan | SCC + ACA | 99m technetium tin colloid | 110 |
| Tanaka et al. (26) | 2005 | USA | SCC | Tc-99m tin colloid | 1 |
| Lamb et al. (27) | 2005 | United Kingdom | ACA | 99m technetium Nano colloid | 40 |
| Arima et al. (28) | 2006 | Japan | SCC | 99m technetium tin colloid | 19 |
| Bohanes et al. (29) | 2005 | Czech Republic | SCC | 99mTc-labelled Nano colloid | 1 |
| Kim et al. (30) | 2011 | Korea | SCC | Technetium-99m neomannosyl human serum albumin | 23 |
| Kosugi et al. (31) | 2007 | Japan | SCC + ACA | 99m-Tc tin colloid | 10 |
| Udagawa et al. (32) | 2005 | Japan | NA | 99mTc-Tin and 99mTc-Phytate | 24 |
| Nomura et al. (33) | 2001 | Japan | SCC + ACA | Methylene blue | 41 |
| Thompson et al. (34) | 2011 | Australia | SCC + ACA | 99mTc antimony colloid | 16 |
| Thompson et al. (35) | 2011 | Australia | SCC + ACA | 99mTc antimony colloid | 31 |
| Grotenhuis et al. (36) | 2009 | The Netherlands | ACA | Patent blue V | 40 |
| Terui et al. (37) | 1982 | Japan | SCC + ACA | 99mTc rhenium sulfur colloid | 9 |
| Kitagawa et al. (38) | 2000 | Japan | SCC | 99m technetium tin colloid | 16 |
| Tsai et al. (39) | 2013 | Stockholm | SCC + ACA | 99mTc-nanocoll | 8 |
Event rates
Definitions of various parameters and selection criteria of patients undergoing sentinel node biopsy are listed in Tables 2 and 3 respectively. The overall detection rate was 0.93 (95% CI: 0.894-0.950), sensitivity 0.87 (95% CI: 0.811-0.908), negative predictive value 0.77 (95% CI: 0.568-0.890) and the accuracy was 0.88 (95% CI: 0.817-0.921). In the adenocarcinoma cohort, detection rate was 0.98 (95% CI: 0.923-0.992), sensitivity 0.84 (95% CI: 0.743-0.911) and the accuracy was 0.87 (95% CI: 0.796-0.913). In the squamous cell carcinoma group, detection rate was 0.89 (95% CI: 00.792-0.943), sensitivity 0.91 (95% CI: 0.754-0.972) and the accuracy was 0.84 (95% CI: 0.732-0.914).
Table 2. Definitions of various parameters.
| Parameters (40,41) | Formula |
|---|---|
| Detection rate of SNs | No. of the cases with detectable SNs/No. of the total cases |
| Negative predictive value | No. of patients with true-negative node (SN + NSN)/No. of patients with true-negative node + patients with false-negative SN |
| Accuracy | No. of patients with positive SN + No. of patients with true-negative SN/No. of patients with an identified SN |
| Sensitivity | No. of patients with true-positive SN/No. of patients with true-positive SN + patients with false-negative SN |
Table 3. When was the sentinel node biopsy done and selection criteria of patients?
| Author (Ref) | Selection criteria |
|---|---|
| Bhat et al. (17) | Prior to standard radical oesophagogastrectomy Patients with clinical or radiological evidence of metastasis, T4 tumours, and concomitant co-morbid conditions, such as chronic obstructive pulmonary disease (with VC <1 L, FEVI <50%); chronic renal failure (serum creatinine >3 mg/dL), were excluded from the study. Besides, patients who had undergone neoadjuvant therapy before surgery were excluded from the study |
| Yasuda et al. (18) | Patients who had no apparent signs of LN metastases on preoperative imaging studies and who underwent standard surgeries with extended LN dissections: three field dissection in patients with oesophageal cancer |
| Kato et al. (19) | Thoracic oesophageal SCCs who underwent radical oesophagectomy between January 1999 and December 2001at the Gunma University Faculty of Medicine (Maebashi, Japan). None of these patients had received preoperative treatment |
| Hayashi et al. (22) | All neoplasms were considered cT1-stage without lymph node (cN0) or distant metastasis (cM0). The selection criteria for endoscopic CT lymphography were localized neoplasms without multiple skip tumours, operable superficial neoplasms without extensive neoplastic invasion to surrounding structures such as the heart and trachea/bronchus, and no evidence of distant metastasis or lymph node metastases on preoperative imaging studies including endoscopic ultrasonography and CT |
| Takeuchi et al. (23) | Neoadjuvant therapy was given in Chemotherapy (Y/N) 4/71, Radiotherapy (Y/N) 0/75 |
| Yuasa et al. (24) | Patients who had been administered preoperative chemo radiotherapy or had comorbidity with other malignancies were excluded |
| Uenosono et al. (25) | Based on the TNM classification, cT1 tumours were found in 60 patients, cT2 in 31, and cT3 in 32. Apart from these patients, neoadjuvant chemo radiation therapy (CRT) was given to 11 patients |
| Arima et al. (28) | No patients received radio- or chemotherapy before surgery |
| Bohanes et al. (29) | Before neoadjuvant therapy |
| Kim et al. (30) | Candidates for oesophagectomy with conventional lymph node dissection for thoracic oesophageal cancer were consecutively enrolled. Preoperative concurrent chemo radiation therapy was given in Yes 4 (17.4), No 19 (82.6) |
| Kosugi et al. (31) | cT1N0 carcinoma of the thoracic oesophagus that underwent radical oesophagectomy between March 2002 and November 2003 at the Niigata University Medical and Dental Hospital. None of these patients had received preoperative treatment |
| Thompson et al. (34) | Selected patients (T2 or greater) were treated with neoadjuvant therapy according to protocol |
| Thompson et al. (35) | Preoperative clinical staging included upper gastrointestinal endoscopy, computed tomography scans (chest, abdomen, and pelvis), PET/CT scans, endoscopic ultrasonography (if minimal stricturing), and diagnostic laparoscopy (for gastroesophageal junction tumours). Selected patients (T2 or greater) were treated with neoadjuvant therapy according to protocol. This consisted of two cycles of cisplatin (80 mg/m2 on day 1) and 5-FU (800 mg/m2 continuous infusion for five days) during weeks 1 and 5 of radiotherapy, plus 25 fractions of radiotherapy (over five weeks) to a total of 45 Gy. Patients underwent surgical resection 5 to 6 weeks after completion of neoadjuvant therapy |
| Grotenhuis et al. (36) | Histologically proven adenocarcinoma of the distal oesophagus or GEJ preoperatively (Siewert type I or II, respectively) and no application of neoadjuvant chemotherapy or radiotherapy. Induction chemotherapy or radiotherapy was given in patients with a cT4-tumor without distant metastases or in patients with involvement of celiac trunk lymph nodes (M1a), who were not considered eligible for primary surgical therapy. Chemotherapy or radiotherapy was performed before surgery in 30 patients; histologic examination confirmed a squamous cell carcinoma in 20 patients; surgery for high-grade dysplasia was performed in two patients; and a double tumour of the oesophagus led to exclusion in one patient |
| Terui et al. (37) | Five patients underwent preoperative radiotherapy |
Heterogeneity and publication bias
The heterogeneity of outcomes has been summarized in Tables 4 and 5. The reason for significant heterogeneity may be attributed to different population groups and the variable type of SLN tracer legislated for clinical use in each country. No publication bias was detected using the Egger’s regression model.
Table 4. Pooled event rate and 95% CI.
| Parameter | Sub groups | Pooled event rate | 95% CI | I2 | P value |
|---|---|---|---|---|---|
| Accuracy | Overall | 0.88 | 0.817-0.921 | 56.28 | 0.01 |
| ACA | 0.87 | 0.796-0.913 | 25.19 | 0.25 | |
| SCC | 0.84 | 0.732-0.914 | 36.62 | 0.19 | |
| Detection rate | Overall | 0.93 | 0.894-0.950 | 0.07 | 0.44 |
| ACA | 0.98 | 0.923-0.992 | 0.00 | 0.73 | |
| SCC | 0.89 | 0.792-0.943 | 23.66 | 0.26 | |
| Sensitivity | Overall | 0.87 | 0.811-0.908 | 39.90 | 0.08 |
| ACA | 0.84 | 0.743-0.911 | 0.00 | 0.82 | |
| SCC | 0.91 | 0.754-0.972 | 61.09 | 0.05 | |
| Negative Predictive value | Overall | 0.77 | 0.568-0.890 | 77.44 | 0.00 |
Table 5. Subgroup analysis for various radioisotopes used for lymphoscintigraphy.
| Radioisotopes | Parameter | Pooled event rate | Lower limit | Upper limit |
|---|---|---|---|---|
| 99m technetium Nano colloid | Accuracy | 0.99 | 0.88 | 1.00 |
| 99m technetium Nano colloid | Detection rate | 0.94 | 0.90 | 0.97 |
| 99m technetium Nano colloid | Sensitivity | 0.81 | 0.64 | 0.91 |
| 99m technetium rhenium sulphide | Accuracy | 0.95 | 0.85 | 0.98 |
| 99m technetium rhenium sulphide | Detection rate | 0.86 | 0.80 | 0.90 |
| 99m technetium rhenium sulphide | Sensitivity | 0.93 | 0.81 | 0.97 |
| 99m technetium tin colloid | Accuracy | 0.96 | 0.86 | 0.99 |
| 99m technetium tin colloid | Detection rate | 0.90 | 0.81 | 0.95 |
| 99m technetium tin colloid | Sensitivity | 0.75 | 0.66 | 0.83 |
| 99mTc antimony colloid | Accuracy | 0.92 | 0.73 | 0.98 |
| 99mTc antimony colloid | Detection rate | 0.94 | 0.78 | 0.99 |
| 99mTc antimony colloid | Sensitivity | 0.98 | 0.84 | 1.00 |
| Indocyanine Green Fluorescence | Detection rate | 0.90 | 0.74 | 0.97 |
| Methylene blue | Accuracy | 0.86 | 0.66 | 0.95 |
| Methylene blue | Detection rate | 0.96 | 0.80 | 0.99 |
| Methylene blue | Sensitivity | 0.91 | 0.71 | 0.98 |
| Patent blue V | Accuracy | 0.92 | 0.73 | 0.98 |
| Patent blue V | Detection rate | 0.69 | 0.48 | 0.84 |
| Technetium-99m neomannosyl human serum albumin | Detection rate | 0.98 | 0.71 | 1.00 |
Discussion
SLN mapping and biopsy was first applied to melanoma, and was subsequently extended to breast cancer and, more recently, to many other solid tumours including oesophageal cancer (5,6,34,35,42-47). The SLN concept has revolutionized the approach to the surgical staging of both melanoma and breast cancer, and these techniques can benefit patients by avoiding various complications that may result from unnecessary prophylactic radical lymph node dissection in cases of negative SLNs for cancer metastasis. New developments in determining the sentinel node for especially early oesophageal tumours will probably influence operative strategies in the future.
Kuge et al. found direct lymphatic drainage from the submucosal plexus of the oesophagus to the thoracic duct in cadavers. Moreover, they found a long longitudinal extension of the drainage networks of the submucosal plexus suggesting that this is the explanation for skip metastases to cervical nodes (48). Especially early intramural tumours (T1 and T2) probably tend to drain lymph fluid into the longitudinal networks. Therefore, isolated distant lymph node involvement is not necessarily a sign of advanced disease. Regional lymph nodes, on the other hand are connected with tumours invading the extramural layers (T3 and T4) through lymph vessels piercing through the oesophageal wall. In this concept regional lymph nodes would be a sign of more advanced oesophageal cancer. This was confirmed in a retrospective study by Matsubara et al. (49) In order to predict possible sites of sentinel nodes they analysed the location of initial lymph node metastasis in 329 patients after extended oesophagectomy for squamous cell carcinoma. Of the solely positive lymph nodes 82% was located in the relatively distant cervico-thoracic junction or perigastric region. When two or three positive lymph nodes were identified they were rarely confined to the intrathoracic lymph nodes. The authors reasoned that a cervical and abdominal lymph node dissection prior to a thoracotomy can predict intrathoracic node involvement and could be a treatment strategy to prevent a thoracotomy in poor-risk patients (49).
The use of radioactive agents and lymphoscintigraphy to determine the lymphatic spread of oesophageal and gastric cardia cancers is not new (37,50). In 1982 Terui et al. already reported a series of nine patients with oesophageal cancer in whom radioactive sulfur colloid was injected endoscopically around the tumour to visualize mediastinal lymph nodes (37). A total of 106 nodes were removed from the mediastinum and nine of the 12 positive lymph nodes were visualized on the preoperative lymphoscintigram. Of the visualized (hot) nodes, 34.6% was positive while only 3.8% of the nonvisualized (cold) nodes were positive for metastasis. The authors concluded that hot nodes indicate a high percentage probability of metastatic nodes (37). To clarify the lymphatic pathways of the (mainly lower) oesophagus Aikou et al. injected radioactive colloid in the oesophageal submucosa in 19 patients with oesophageal cancer (50). A lymphoscintigraphy was made afterwards. Because they could not find a difference between the radioisotopic uptake by cancer free and metastatic nodes the authors argued that the technique would not have any future role for the diagnosis of lymph node metastases (50). The feasibility of lymphoscintigraphy of the oesophagus was also studied in a canine model (51). After submucosal injection of radiolabeled technetium-99m antimony sulfide colloid in six dogs lymph nodes were identified on nuclear scans. The expected position of lymph nodes based on the scans correlated with the location of the radiolabeled nodes at anatomic dissection (51).
In a study of 16 patients with oesophageal cancer Kitagawa et al. found that the frequency of metastatic involvement in SLNs was significantly higher than in non-sentinel nodes (38). Lymph node involvement was found in only 2% of the non-sentinel nodes. These results were confirmed in a larger study by Yasuda et al. (18). In that study, however, more than 50% of the radioactive nodes were missed by the handheld gamma probe. Lamb et al. who investigated the feasibility and accuracy of the sentinel node concept in 40 patients with oesophageal cancer (27). After routine haematoxylin-eosin and immunohistochemical examination of each lymph node the accuracy was 96% and only two false negative sentinel nodes were identified. Half of the sentinel nodes for lower oesophageal tumours were located in the mediastinum, whereas nearly 75% of the SLNs for gastric cardia cancers were within the abdomen (27). Although less favourable results have been reported as well (32), this study by Lamb et al. has cleared the way for the first clinical applications of the sentinel node concept in oesophageal cancer which hopefully in the future will lead to less extensive lymphadenectomies for patients with negative SLNs.
Instead of lymphoscintigraphy and intra-operative use of a gamma probe after injection of a radioactive colloid other techniques for identifying sentinel nodes have recently been reported (52,53). Near-infrared fluorescent lymph tracers have been tested in a pig model (53). Moreover, the feasibility of an endoscopic computed tomography (CT) lymphography with a new CT contrast agent (iopamidol®) was shown in a canine model and in nine patients with oesophageal squamous cell cancer (52). After contrast injection into the oesophageal submucosa a CT scan was made. With guidance of the CT lymphography all 18 preoperatively identified sentinel nodes in the patients could be resected. Five SLNs in five different patients contained metastases while in those patients no metastases were found in other lymph nodes after formal two- or three-field lymph node dissections. The technique could also visualize lymphatic vessels connecting the tumour sites directly to lymph nodes (52).
Kagoshima University (25) has been the largest cohort published so far and their detection rates of SLNs were 93.3% in cT1, 100% in cT2, 87.5% in cT3, and 45.5% in CRT patients. In the 120 cases where SLNs were identified, lymph node metastases were found in 12 patients with cT1, 18 with cT2, 24 with cT3 tumours, and 3 with CRT. Accuracy rate of SLN mapping was 98.2% in cT1, 80.6% in cT2, 60.7% in cT3, and 40% in CRT patients. Although one false-negative case had cT1 tumour, the lymph node metastasis was detected preoperatively. Multiple studies using a radio-guided approach to find SLNs in oesophageal cancer have reported success rates of 85% to 100%, and accuracy rates of 88% to 96% (19,21,23,27). Grotenhuis et al. (36) recognized a SLN in 98% of patients, nevertheless had an excessively high false negative rate of 15% and an accuracy rate of only 85%. Likewise, Bhat et al. (17) detected a SLN in 81% of patients with an accuracy rate of only 75%. SLN had a sensitivity of 85.71% in mid oesophageal tumours and 93.33% in lower oesophageal tumours. The SLN biopsy had sensitivity of 87.5% in the case of squamous cell carcinoma and 92.86% in the cases of adenocarcinoma of the oesophagus. The accuracy of the procedure for squamous cell carcinoma and adenocarcinoma was 60% and 76.47%, respectively. In our analysis, the overall detection rate was 0.93 (95% CI: 0.894-0.950), sensitivity 0.87 (95% CI: 0.811-0.908), negative predictive value 0.77 (95% CI: 0.568-0.890) and the accuracy was 0.88 (95% CI: 0.817-0.921). In the adenocarcinoma cohort, detection rate was 0.98 (95% CI: 0.923-0.992), sensitivity 0.84 (95% CI: 0.743-0.911) and the accuracy was 0.87 (95% CI: 0.796-0.913). In the squamous cell carcinoma group, detection rate was 0.89 (95% CI: 00.792-0.943), sensitivity 0.91 (95% CI: 0.754-0.972) and the accuracy was 0.84 (95% CI: 0.732-0.914).
Practical problems
Obesity contributes to bigger difficulty in patients with surgical resection and identification of SLNs. The oesophagus is in the posterior mediastinum, it is difficult to recognize lymph node with dye until the mediastinal pleura is opened. Also, in many patients with oesophageal cancer, mediastinal lymph nodes are black due to anthracosis. Therefore, dye method alone may not be suitable for SLN mapping in oesophageal cancer (35). With the use of three serial sections and immunohistochemistry on negative SLNs, 14% (3/22) of patients were upstaged (35) and Lamb et al. also found that 12% (3/25) of pN0 patients were upstaged following immunohistochemistry analysis (27).
The routine use of SLN biopsy in oesophageal cancer cannot alter or limit the extent of lymphadenectomy in the same way as is seen in breast cancer and melanoma. And in oesophageal cancer, preoperative access to sentinel nodes may be as invasive, and as morbid, as the operation itself. But, if one agrees that isolated tumour cells have prognostic significance in oesophageal cancer and are detected in 12-14% of node-negative patients using serial sections and immunohistochemistry, then the SLN concept becomes the only practical method of improving pathological staging (35). So, although sentinel node biopsy has not yet been shown to minimize the extent of lymphadenectomy, it may influence postoperative therapy for a substantial number of patients.
Perhaps the key drawback with SLN biopsy in oesophageal cancer is the variety of SLN tracer authorized for clinical use in each nation (54). The vastly diverse particle sizes hinder wide application of the model and design of a uniform practice. For instance, Japan’s 99mTc-tin colloid (100 nm in size) allows for lymphoscintigraphy 24 h before surgical resection (23), while other smaller radio colloids (like Australia’s 99mTc-antimony trisulphide colloid) have much shorter transit periods in the sentinel nodes (54,55). We observed that the parameters like sensitivity, accuracy and detection rates were higher in radioisotopes when compared to methylene blue or patent blue dyes (Table 6). Facilitating preoperative lymphoscintigraphy in between endoscopic peritumoural injection and same-day surgery is often not practical.
Table 6. Information about the particle property, injection technique and pathological analysis.
| Author (Ref) | Properties of the particles | Type of injection | Time between injection and examination | Histopathology |
|---|---|---|---|---|
| Bhat et al. (17) | 0.5 mL of 1% Methylene Blue (2 mL) at four points at the periphery of the tumour before mobilization | |||
| Yasuda et al. (18) | The amount injected into each patient was 184 MBq (5 mCi). On the day before surgery, 0.5 mL (46 MBq, 1.25 mCi) of Tc-99m tin colloids was injected endoscopically into four submucosal sites surrounding the tumor. Injections were performed with 23-gauge endoscopic injection sclerotherapy needles | Metastatic status was determined for each LN by routine hematoxylin and eosin (H&E) preparations | ||
| Kato et al. (19) | The day before surgery, 0.5 mL (0.5 millicuries) of technetium-99m colloidal rhenium sulfide (NANOCIS, CIS Bio-international, Gif sur Yvette, France) was injected into the submucosa at four sites around the primary tumor using esophagoscopy. Before the surgery, anterior and posterior lymphoscintigraphy from the neck to the upper abdomen was performed with a large-field scintillation camera. Sentinel lymph nodes were defined as hot lymph nodes identified by two surgeons at the time of lymphoscintigraphy. Because esophageal SCC can show unidirectional or bidirectional lymphatic spread, the sentinel lymph node was assigned to assess the distribution of spread. These lymph nodes were defined as above (I) if the radiocolloid was localized at a site above the injection site or below (II) if it was localized at a site below the injection site | 17 hours | Two pathologists evaluated one crosssection stained with HE. The extent of lymph node metastasis and the localization of the lymph nodes were documented.Two extra cross-sections were cut in all dissected lymph nodes. One section was stained with HE, and the other was used for immunohistochemical detection of CK. Sections that were 4 mm thick were cut from each paraffin block of the 1,406 lymph nodes and then deparaffinized and treated with 0.3% H2O2-methanol solution for 30 minutes at room temperature to block endogenous peroxidase activity. After rehydration through a graded ethanol series, we incubated each slide for 30 minutes in 0.1% trypsin solution in CaCl2/phosphate-buffered saline (PBS). After the slide had been rinsed in 0.1 M PBS (pH 7.4), nonspecific binding sites were blocked by incubation with 10% normal horse serum for 30 minutes. The sections were then incubated with primary antibody overnight at 4 °C. The monoclonal antibody cocktail AE1/AE3 (Boehringer-Mannheim, Mannheim, Germany) was diluted by a ratio of 1:1,000. Immunohistochemistry was performed using the ABC system (Vectastatin, Burlingame, CA). Incubation with the secondary antibody, biotinylated anti-mouse IgG, was carried out for 30 minutes. The chromogen used was 3,3-diaminobenzidine tetrahydrochloride, applied as a 0.02% solution containing 0.005% H2O2 in 50 mM ammonium acetate–citric acid buffer (pH 6.0). The sections were counterstained lightly with hematoxylin. Negative controls were established by replacing the antibody with PBS or normal mouse serum | |
| Hayashi et al. (22) | Iopamidol a molecular weight of 777 daltons, iodine concentration of 370 mg/mL, osmolarity of 780 mOsm/kg, viscosity of 9.1 mPa/s, and a pH level of 6.5 to 7.5 | A total of 2 to 3 mL of iopamidol was injected into the submucosal layer at four different areas surrounding the primary neoplasms (0.5- to 0.75-mL dose each) | All dissected lymph nodes and esophagogastric tissues were fixed in 10% buffered formalin, processed overnight, and embedded in paraffin | |
| Takeuchi et al. (23) | In brief, one day (within 16 hours) before the surgery, a 2.0-mL volume of technetium-99m tin colloid solution (150 MBq) was injected at four quadrants into the submucosal layer around the primary tumor using an endoscopic puncture needle. Preoperative lymphoscintigraphy was usually obtained 3 to 4 hours after the tracer injection. For abdominal esophageal cancer or adenocarcinoma of gastroesophageal junction, a dual tracer method of the radioactive tracer and blue dye (1% isosulfan blue) was principally used for SLN detection. The blue-dye was injected into the submucosal layer of the primary lesion endoscopically right after surgery began. | 3-4 hours | ||
| Yuasa et al. (24) | Iopamidol (Iopamiron 370; Nihon Schering, Osaka, Japan) is a commercially available water-soluble monometric iodine CT contrast medium for intravenous use, with a molecular weight of 777.09 Da, and the solute has an iodine concentration of 370 mg/mL and an osmolality of 780 mOsm/kg (<3 times the osmolality of physiological saline (~300 mOsm/kg), viscosity of 9.1 mPa/s, and pH of 6.5-7.5 | First, iopamidol was injected endoscopically into the four submucosal regions around the tumor tissues at high pressure with a 23-gauge needle. The injection was performed until swelling was confirmed with every 0.5-mL administration | Biopsy samples of SLN tissue were stored in 10% buffered formalin, processed overnight, and sectioned in serial 2.0-mm-thick slices. All slices were embedded in paraffin and examined by hematoxylin and eosin staining. Another dissected LN was also cut in half along the long axis, and one section from each tissue slice was examined after hematoxylin and eosin staining | |
| Uenosono et al. (25) | 99mTechnetium-Tin colloid that was 100 nm in size was used as a tracer | One day before surgery, approximately 222 MBq (2 mL) of 99mTc-tin colloid (1 mM anhydrous stannous chloride solution, Nihon Medi-physics Co. Ltd., Nishinomiya, Japan) was injected under endoscopic guidance into the submucosa of the esophagus at four sites (0.5 mL each) around the tumor using a disposable 23-gauge needle (MAJ-75, Olympus, Japan) | All dissected lymph nodes, including SNs, were examined by hematoxylin and eosin staining (H&E) and immunohistochemical staining (IHC). After each lymph node was cut in the plane of largest dimension, it was fixed in 10% formaldehyde and embedded in paraffin. Paraffin sections (3 mL each) were stained with H&E, and additional sections were used for IHC using a monoclonal anticytokeratin (CK) antibody cocktail (AE1/AE3, DAKO Corporation, CA, USA) that reacts with a broad spectrum of human CKs. Three sections in each node were used to detect lymph node micrometastasis in IHC. The sections were deparaffinized in xylene, rehydrated with a graded series of ethanol, and then endogenous peroxidase activity was blocked by 5-min incubation in 3% hydrogen peroxide in methanol. The sections were then immersed in proteinase K (DAKO Corporation) to activate the antigen and incubated with CK monoclonal antibody diluted 1:200 for 30 min. After two 5-min washes with phosphate-buffered saline, the avidin-biotin complex and immunoperoxidase were applied (ABC method; VECTASTAIN ABC Kit, Vector Laboratories, Inc., Burlingame, CA, USA). Cells positive for CK were visualized using diaminobenzidine tetrahydrochloride, and the sections were lightly counterstained with hematoxylin. The negative controls consisted of sections processed in the same manner but without the primary antibody. Consistently CK-positive normal esophageal mucosa and primary tumor specimens were used as positive controls | |
| Thompson et al. (35) | Peritumoral injection of four, 1-mL aliquots of 40 MBq 99mTc antimony colloid (Lymphflo) was undertaken once the patient was under general anesthetic immediately before surgery. At endoscopy, the peritumoral injections were performed into the submucosal layer at both the proximal and distal margins of the tumor | Sentinel lymph nodes were bisected along their longitudinal axis, or cut into 2- or 3-mm slices if thicker than 5 mm. On the first section, one slide was stained with H&E, and the other with the monoclonal epithelial antibody AE1/AE3 (DAKO, Carpinteria, CA) for immunohistochemistry (IHC). The monoclonal antibody AE1/AE3 is widely used because it recognizes a broad range of keratin subtypes expressed in esophageal carcinomas [21]. Sections of primary tumors were used as positive controls with each run, and a negative control (primary antibody omitted) was also included. Sentinel lymph nodes that remained tumor free on both H&E and IHC on the first section had a minimum of two further serial step sections performed [22-24]. Lymph node metastases were defined as metastasis >2 mm in size. Micrometastases were defined as metastasis >0.2 mm and <2 mm, while isolated tumor cells were defined as a single tumor cell or a cluster of tumor cells <0.2 mm in size. Strict criteria were used to designate a positive cell(s) as an isolated tumor cell(s). Cells had to demonstrate cytologic and microanatomic features of a tumor cell, including increased cell size, enlarged nuclear size, and increased nuclear-to-cytoplasmic ratio | ||
| Tanaka et al. (26) | Lymphoscintigrams were obtained three hours after administration of 148 MBq (4 mCi) Tc-99m tin colloid into the sub-mucosal layer of 2 points each in oral and anal sides of lesion (totally 4 points) using an endoscopic procedure | |||
| Lamb et al. (27) | The half-life of 99mTc is 6 h and the γ counter had a sensitivity of 6.55×104 c.p.s. per MBq. | Using an endoscopic injection needle, 2 mL 99mTcradiolabelled nanocolloid (NanocollTM; Amersham Health, Little Chalfont, UK), containing 20 MBq radioactivity, was injected into the submucosa at the tumour margins. Aliquots of 0.25-0.50 mL were used to completely surround small lesions, and to mark the proximal and distal margins of larger tumours | A 3-μm section taken through the centre of each lymph node was fixed, embedded, and stained with haematoxylin and eosin for examination by an experienced upper gastrointestinal pathologist. Immunohistochemical staining was performed on an adjacent 3-μm section from all sentinel and non-sentinel lymph nodes. A streptavidin-biotin immunoperoxidase method was used with a combination of anticytokeratin antibody 5D3 (Novocastra, Newcastle, UK) and LP34 (DakoCytomation, Ely, UK) as the primary antiserum. These are known to react with human cytokeratin proteins 5, 6, 8 and 18. Sections of skin were used as positive controls and a negative control (omission of the primary antibody) was included with each set of immunohistochemical reactions | |
| Arima et al. (28) | Solutions of 99mTc and tin were mixed at a ratio of 1:2 to make a particle size of approximately 100 nm. At 1 d before surgery, 0.5 mL (0.75 mCi) of 99mTc-tin colloid was endoscopically injected into the submucosa at four sites around the tumor using a MAJ-75 disposable 23-gauge needle | Each lymph node was cut at the plane of largest dimension, then fixed in 10% formaldehyde and embedded in paraffin. Paraffin sections (3-m thick) were stained using hematoxylin and eosin. Presence or absence of metastasis was then examined microscopically in one representative section including the node hilus. Total area of the lymph node and area comprising metastatic cancer cells were measured using NCC Volumetrer version 2.03 area calculation software. Metastatic area was then calculated using the following formula: metastatic area (%) (area of metastasis/total area of lymph node) 100 | ||
| Bohanes et al. (29) | 99mTc-labelled nanocolloid (Nanocoll®) was applied 2 h before the surgery via endoscopy to the borders of the tumor | |||
| Kim et al. (30) | A total dose of 1mCi of 99mTc-MSA in 0.2 mL was administered at four quadrants into the submucosal layer around the primary tumor under esophagoscopic guidance approximately 1 to 3 hours before surgery | All harvested lymph nodes including SLNs identified during the operation were examined by frozen sections. They were cut into 2-mm slices and ultimately diagnosed by using formalin-fixed and paraffin-embedded sections with hematoxylin and eosin staining | ||
| Kosugi et al. (31) | On the day before surgery, 3.99 to 7.03 mCi (average: 5.03 mCi) of Tc-99m tin colloids in a volume of 2.0 to 6.0 mL was injected endoscopically into the submucosal layer at four sites around the primary tumor, using a 23-gauge endoscopic puncture needle | 23 hours | The surgical specimens were fixed, embedded, stained with hematoxylin and eosin (HE), and evaluated microscopically | |
| Grotenhuis et al. (36) | At three different sites in the vicinity of the tumor, 1 to 2 mL Patent Blue V (Guerbet-Laboratories, Issy les Moulineaux, France) was injected into the submucosal layer. Within the next five minutes, the sentinel node(s) were identified by following the blue-stained lymphatic vessels | Pathologic evaluation of all lymph nodes consisted of conventional hematoxylin-eosin (H&E) staining. If no tumor cells were identified in the sentinel node(s), multilevel serial sectioning was performed. These lymph nodes were cut at 10 levels of approximately 100 mm (dependent in lymph nodes’ size). Subsequently, sections were cut with a thickness of 4 mm and examined for tumor cells with H&E staining and immunohistochemistry to reveal micrometastases (metastatic lesions >0.2 mm in dimension but <2.0 mm) and isolated tumor cells (metastatic lesions <0.2 mm in dimension). The mouse-monoclonal antibody CAM 5.2 (NCL5D3, Novo Castra, Wetzlar, Germany), which is specific for intracellular cytokeratin-8 and 18, was used for this experiment | ||
| Tsai et al. (39) | On the afternoon the day before surgery, the patients underwent endoscopic submucosal injection of 4×0.5 mL in total 60 MBq 99mTc-nanocoll (GE Healthcare Srl., Milan, Italy) proximal to the tumor | All tissue received as sentinel node was paraffin embedded and sectioned in four levels where each first level was stained with hematoxylin-eosin staining and each second level was stained with immunohistochemical staining with a pan-cytokeratin antibody (CK MNF), for the detection of micro metastases analogous to the Swedish standard for processing of breast cancer sentinel nodes. Non-sentinel nodes were sectioned once and analyzed after hematoxylineosin staining. All slides were assessed by the same pathologist (EL) using light microscopy |
Skip metastases
Another criticism in the literature about SLN biopsy in oesophageal cancer is the described high frequency of skip metastases, although most of these outcomes have been in patients with squamous cell carcinomas (27,35). If SLNs without metastasis are identified only in abdominal lymph nodes, especially in the tumours limited to the lower third of the oesophagus, cervical lymph nodes dissection may be omitted, such as left thoracotomy or trans-hiatal approach. SLN navigation surgery also is unacceptable for patients who have had neoadjuvant therapy (25).
Limitations
The studies included in the meta-analysis are predominantly from Japan and hence generalization of such results cannot be made. Prospective analysis and long-term follow-up studies of the sentinel node concept are needed before these techniques can be applied widely in different stages, pre or post neoadjuvant chemoradiotherapy, tumour sites and histology. There are considerable variations between particle sizes and particle composition, time between injection and examination. The lack of standardization of technique is a major setback for challenging procedure to gain popularity across the globe. Another important of the studies is lack of uniformity reporting data. Measures are needed to enhance radioisotope develop a swift and precise technique to localise the SLN. In the relative absence of hard facts and in the presence of debatable evidence this procedure cannot be recommended as standard of care at present. More additional, definitive, adequately powered studies with a virtuous selection criteria, predefined surgical technique and that takes into consideration the existing shortcomings of the procedure would be ideal to evaluate the role of SLN biopsy in oesophageal cancers.
Conclusions
SLN biopsy is feasible in oesophageal resections with conservative lymphadenectomy and, when successful, initial results suggest it is very accurate in predicting overall nodal status. However, further work is needed to optimize radiocolloid type, refine the technique and develop a quick and accurate way to determine SLN status intraoperatively. SLN biopsy may become standard of care in oesophageal cancer in the near future, especially in the setting of minimally invasive surgery. Whether it will ever be useful as a tool for tailoring a lymphadenectomy is a question for the future.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Jemal A, Siegel R, Xu J, et al. Cancer statistics, 2010. CA Cancer J Clin 2010;60:277-300 [DOI] [PubMed] [Google Scholar]
- 2.Bollschweiler E, Wolfgarten E, Gutschow C, et al. Demographic variations in the rising incidence of esophageal adenocarcinoma in white males. Cancer 2001;92:549-55 [DOI] [PubMed] [Google Scholar]
- 3.Ries LAG, Melbert D, Krapcho M, et al. eds. SEER Cancer Statistics Review, 1975-2004, National Cancer Institute, Bethesda, MD 2007. [Google Scholar]
- 4.Morton DL, Thompson JF, Essner R, et al. Validation of the accuracy of intraoperative lymphatic mapping and sentinel lymphadenectomy for early-stage melanoma: a multicenter trial. Multicenter Selective Lymphadenectomy Trial Group. Ann Surg 1999;230:453-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giuliano AE, Jones RC, Brennan M, et al. Sentinel lymphadenectomy in breast cancer. J Clin Oncol 1997;15:2345-50 [DOI] [PubMed] [Google Scholar]
- 6.Turner RR, Ollila DW, Krasne DL, et al. Histopathologic validation of the sentinel lymph node hypothesis for breast carcinoma. Ann Surg 1997;226:271-6; discussion 276-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aikou T, Kitagawa Y, Kitajima M, et al. Sentinel lymph node mapping with GI cancer. Cancer Metastasis Rev 2006;25:269-77 [DOI] [PubMed] [Google Scholar]
- 8.Kitagawa Y, Ohgami M, Fujii H, et al. Laparoscopic detection of sentinel lymph nodes in gastrointestinal cancer: a novel and minimally invasive approach. Ann Surg Oncol 2001;8:86S-9S [PubMed] [Google Scholar]
- 9.Ando N, Ozawa S, Kitagawa Y, et al. Improvement in the results of surgical treatment of advanced squamous esophageal carcinoma during 15 consecutive years. Ann Surg 2000;232:225-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Akiyama H, Tsurumaru M, et al. Radical lymph node dissection for cancer of the thoracic esophagus. Ann Surg 1994;220:364-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fujita H, Kakegawa T, Yamana H, et al. Mortality and morbidity rates, postoperative course, quality of life, and prognosis after extended radical lymphadenectomy for esophageal cancer. Comparison of three-field lymphadenectomy with two-field lymphadenectomy. Ann Surg 1995;222:654-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006-12 [DOI] [PubMed] [Google Scholar]
- 13.DerSimonian R, Laird N.Meta-analysis in clinical trials. Controlled Clinical Trials. 1986;7:177-88 [DOI] [PubMed] [Google Scholar]
- 14.Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Egger M, Smith GD, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Orwin R.A fail-safe N for effect size in meta-analysis. Journal of educational statistics 1983;8:157-159 1983 [Google Scholar]
- 17.Bhat MA, Naikoo ZA, Dass TA, et al. Role of intraoperative sentinel lymph node mapping in the management of carcinoma of the esophagus. Saudi J Gastroenterol 2010;16:168-73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yasuda S, Shimada H, Chino O, et al. Sentinel lymph node detection with Tc-99m tin colloids in patients with esophagogastric cancer. Jpn J Clin Oncol 2003;33:68-72 [DOI] [PubMed] [Google Scholar]
- 19.Kato H, Miyazaki T, Nakajima M, et al. Sentinel lymph nodes with technetium-99m colloidal rhenium sulfide in patients with esophageal carcinoma. Cancer 2003;98:932-9 [DOI] [PubMed] [Google Scholar]
- 20.Kitagawa Y, Fujii H, Mukai M, et al. Intraoperative lymphatic mapping and sentinel lymph node sampling in esophageal and gastric cancer. Surg Oncol Clin N Am 2002;11:293-304 [DOI] [PubMed] [Google Scholar]
- 21.Burian M, Stein HJ, Sendler A, et al. Sentinel node detection in Barrett’s and cardia cancer. Ann Surg Oncol 2004;11:255S-8S [DOI] [PubMed] [Google Scholar]
- 22.Hayashi H, Tangoku A, Suga K, et al. CT lymphography-navigated sentinel lymph node biopsy in patients with superficial esophageal cancer. Surgery 2006;139:224-35 [DOI] [PubMed] [Google Scholar]
- 23.Takeuchi H, Fujii H, Ando N, et al. Validation study of radio-guided sentinel lymph node navigation in esophageal cancer. Ann Surg 2009;249:757-63 [DOI] [PubMed] [Google Scholar]
- 24.Yuasa Y, Seike J, Yoshida T, et al. Sentinel lymph node biopsy using intraoperative indocyanine green fluorescence imaging navigated with preoperative CT lymphography for superficial esophageal cancer. Ann Surg Oncol 2012;19:486-93 [DOI] [PubMed] [Google Scholar]
- 25.Uenosono Y, Arigami T, Yanagita S, et al. Sentinel node navigation surgery is acceptable for clinical T1 and N0 esophageal cancer. Ann Surg Oncol 2011;18:2003-9 [DOI] [PubMed] [Google Scholar]
- 26.Tanaka C, Fujii H, Kitagawa Y, et al. Oblique view of preoperative lymphoscintigraphy improves detection of sentinel lymph nodes in esophageal cancer. Ann Nucl Med 2005;19:719-23 [DOI] [PubMed] [Google Scholar]
- 27.Lamb PJ, Griffin SM, Burt AD, et al. Sentinel node biopsy to evaluate the metastatic dissemination of oesophageal adenocarcinoma. Br J Surg 2005;92:60-7 [DOI] [PubMed] [Google Scholar]
- 28.Arima H, Natsugoe S, Uenosono Y, et al. Area of nodal metastasis and radioisotope uptake in sentinel nodes of upper gastrointestinal cancer. J Surg Res 2006;135:250-4 [DOI] [PubMed] [Google Scholar]
- 29.Bohanes T, Neoral C, Aujesky R, et al. Sentinel lymph node in esophageal cancer before neoadjuvant therapy. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 2005;149:145-7 [DOI] [PubMed] [Google Scholar]
- 30.Kim HK, Kim S, Park JJ, et al. Sentinel node identification using technetium-99m neomannosyl human serum albumin in esophageal cancer. Ann Thorac Surg 2011;91:1517-22 [DOI] [PubMed] [Google Scholar]
- 31.Kosugi S, Nakagawa S, Kanda T, et al. Radio-guided sentinel node mapping in patients with superficial esophageal carcinoma: feasibility study. Minim Invasive Ther Allied Technol 2007;16:181-6 [DOI] [PubMed] [Google Scholar]
- 32.Udagawa H.Sentinel node concept in esophageal surgery: an elegant strategy. Ann Thorac Cardiovasc Surg 2005;11:1-3 [PubMed] [Google Scholar]
- 33.Nomura T, Onda M, Miyashita M, et al. Wide-spread distribution of sentinel lymph nodes in esophageal cancer. J Nippon Med Sch 2001;68:393-6 [DOI] [PubMed] [Google Scholar]
- 34.Thompson SK, Bartholomeusz D, Devitt PG, et al. Feasibility study of sentinel lymph node biopsy in esophageal cancer with conservative lymphadenectomy. Surg Endosc 2011;25:817-25 [DOI] [PubMed] [Google Scholar]
- 35.hompson SK, Bartholomeusz D, Jamieson GG. Sentinel lymph node biopsy in esophageal cancer: should it be standard of care? J Gastrointest Surg 2011;15:1762-8 [DOI] [PubMed] [Google Scholar]
- 36.Grotenhuis BA, Wijnhoven BP, van Marion R, et al. The sentinel node concept in adenocarcinomas of the distal esophagus and gastroesophageal junction. J Thorac Cardiovasc Surg 2009;138:608-12 [DOI] [PubMed] [Google Scholar]
- 37.Terui S, Kato H, Hirashima T, et al. An evaluation of the mediastinal lymphoscintigram for carcinoma of the esophagus studied with 99mTc rhenium sulfur colloid. Eur J Nucl Med 1982;7:99-101 [DOI] [PubMed] [Google Scholar]
- 38.Kitagawa Y, Fujii H, Mukai M, et al. The role of the sentinel lymph node in gastrointestinal cancer. Surg Clin North Am 2000;80:1799-809 [DOI] [PubMed] [Google Scholar]
- 39.Tsai JA, Celebioglu F, Lindblad M, et al. Hybrid SPECT/CT imaging of sentinel nodes in esophageal cancer: first results. Acta Radiol. 2013 doi: 10.1177/0284185113475924. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 40.Grotenhuis BA, van Hagen P, Wijnhoven BP, et al. Delay in diagnostic workup and treatment of esophageal cancer. J Gastrointest Surg 2010;14:476-83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fujii H, Kitagawa Y, Kitajima M, et al. Sentinel nodes of malignancies originating in the alimentary tract. Ann Nucl Med 2004;18:1-12 [DOI] [PubMed] [Google Scholar]
- 42.Morton DL, Wen DR, Wong JH, et al. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg 1992;127:392-9 [DOI] [PubMed] [Google Scholar]
- 43.Alex JC, Sasaki CT, Krag DN, et al. Sentinel lymph node radiolocalization in head and neck squamous cell carcinoma. Laryngoscope 2000;110:198-203 [DOI] [PubMed] [Google Scholar]
- 44.Ueda K, Suga K, Kaneda Y, et al. Radioisotope lymph node mapping in nonsmall cell lung cancer: can it be applicable for sentinel node biopsy? Ann Thorac Surg 2004;77:426-30 [DOI] [PubMed] [Google Scholar]
- 45.Viehl CT, Guller U, Cecini R, et al. Sentinel lymph node procedure leads to upstaging of patients with resectable colon cancer: results of the Swiss prospective, multicenter study sentinel lymph node procedure in colon cancer. Ann Surg Oncol 2012;19:1959-65 [DOI] [PubMed] [Google Scholar]
- 46.Orsenigo E, Tomajer V, Di Palo S, et al. Sentinel node mapping during laparoscopic distal gastrectomy for gastric cancer. Surg Endosc 2008;22:118-21 [DOI] [PubMed] [Google Scholar]
- 47.McMasters KM. Sentinel-node biopsy in breast cancer. N Engl J Med 2003;349:1968-71; author reply 1968-71. [PubMed]
- 48.Kuge K, Murakami G, Mizobuchi S, et al. Submucosal territory of the direct lymphatic drainage system to the thoracic duct in the human esophagus. J Thorac Cardiovasc Surg 2003;125:1343-9 [DOI] [PubMed] [Google Scholar]
- 49.Matsubara T, Ueda M, Kaisaki S, et al. Localization of initial lymph node metastasis from carcinoma of the thoracic esophagus. Cancer 2000;89:1869-73 [DOI] [PubMed] [Google Scholar]
- 50.Aikou T, Natugoe S, Tenabe G, et al. Lymph drainage originating from the lower esophagus and gastric cardia as measured by radioisotope uptake in the regional lymph nodes following lymphoscintigraphy. Lymphology 1987;20:145-51 [PubMed] [Google Scholar]
- 51.Baciewicz FA, Jr, McNevin MS, Farris RH, et al. Lymphoscintigraphic technique to image canine esophageal lymph nodes. J Invest Surg 2000;13:265-71 [DOI] [PubMed] [Google Scholar]
- 52.Suga K, Shimizu K, Kawakami Y, et al. Lymphatic drainage from esophagogastric tract: feasibility of endoscopic CT lymphography for direct visualization of pathways. Radiology 2005;237:952-60 [DOI] [PubMed] [Google Scholar]
- 53.Parungo CP, Ohnishi S, Kim SW, et al. Intraoperative identification of esophageal sentinel lymph nodes with near-infrared fluorescence imaging. J Thorac Cardiovasc Surg 2005;129:844-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mariani G, Erba P, Manca G, et al. Radioguided sentinel lymph node biopsy in patients with malignant cutaneous melanoma: the nuclear medicine contribution. J Surg Oncol 2004;85:141-51 [DOI] [PubMed] [Google Scholar]
- 55.Chakera AH, Hesse B, Burak Z, et al. EANM-EORTC general recommendations for sentinel node diagnostics in melanoma. Eur J Nucl Med Mol Imaging 2009;36:1713-42 [DOI] [PubMed] [Google Scholar]


