Sir,
Hair shaft abnormalities can be congenital or acquired can reflect an isolated disorder or a systemic disease or a part of syndrome. Hair shaft microscopy can provide a clue to diagnose complex syndromes. Netherton syndrome is a rare autosomal recessive genodermatoses characterized by a triad of ichthyosiform dermatosis, atopic diathesis and characteristic hair finding trichorrhexis invaginata (bamboo hair).[1] Rarely trichorrhexis nodosa and pili torti is seen. Seven cases have been reported in the literature of netherton syndrome being associated with pili torti. We report case of a 2-year-old female child diagnosed as netherton syndrome with pili torti as a hair shaft abnormality.
A 2-year-old female child born at term, of second degree consanguineous marriage was referred to pediatric dermatology for evaluation of generalized, pruritic, scaly lesions from 1 month of age. The child had recurrent respiratory and skin infections from infancy. No history of collodion membrane at birth. She had delayed developmental milestones and growth retardation. She was the 7th child to her parents. First four siblings had died, 1st child died in utero at 8 months, 2nd and 3rd child died at 1 month and 11 days after birth but the cause of death was unknown. There were no records available. 4th child died at 6 months of age due to similar skin symptoms. Among the other two living siblings, 6th child aged 4 years had similar skin symptoms, which improved spontaneously.
On physical examination, height and weight was below 3rd percentile. Cutaneous examination showed diffuse erythema and fine to thick adherent scaling all over the body including scalp, palms and soles [Figure 1]. Scalp hair, eyebrows, and eyelashes were sparse, rough and brittle. Systemic examination was normal. Investigations revealed peripheral eosinophilia and increased serum immunoglobulin E (IgE) levels (1276 IU/ml). Skin biopsy showed acanthosis, mild spongiosis, focal lymphocytic exocytosis in the epidermis, regular elongation of rete edges, moderate parakeratosis and supra papillary thinning. Dermis showed lymphocytic infiltrate with occasional eosinophilis [Figure 2]. Light microscopy of hair shaft from scalp and eyebrows showed pili torti [Figure 3], which confirmed the diagnoses of netherton syndrome.
Figure 1.

Diffuse erythema and scaling present all over the body
Figure 2.
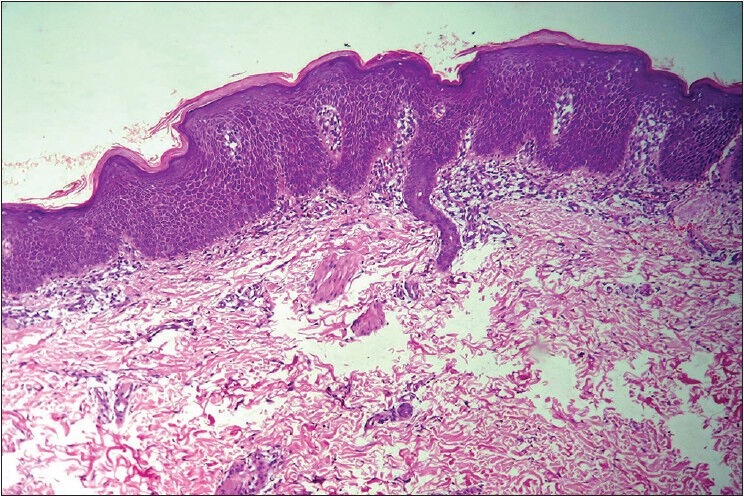
Epidermis showing mild spongiosis and focal lymphocytic exocytosis, regular elongation of rete edges, moderate parakeratosis and supra papillary thinning. Dermis shows lymphocytic infiltrate with occasional eosinophilis (H and E, ×10)
Figure 3.
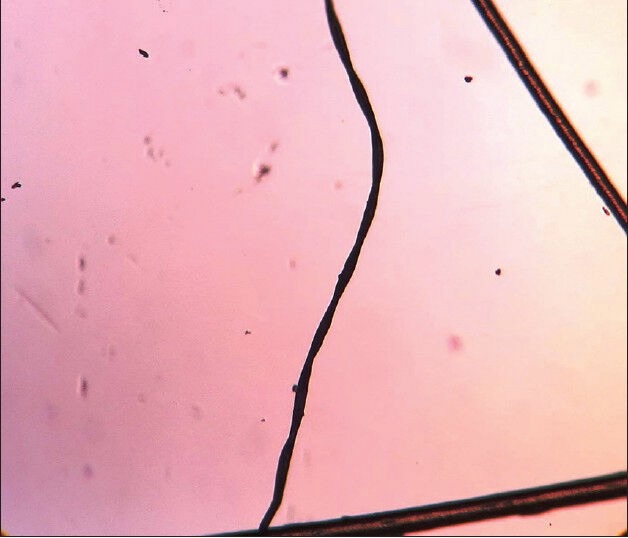
Light microscopy of hair shaft showing pili torti
Netherton syndrome is caused by mutation in serine protease inhibitor, kazal type 5 gene, which is located on long arm of chromosome 5q32.[2] New borns with netherton syndrome presents as erythroderma initially, later develops into distinct form of non-bullous ichthyosis with erythema and polycyclic plaques with double edged scale called ichthyosis linearis circumflexa. 18% cases of netherton syndrome presents as congenital erythroderma.[3] Hair defects may not be seen in the neonatal period and may develop later. Hair sampling may have to be repeated several times, as only 20-50% of hairs may be affected. Clipped hair especially eyebrows may be most informative. Pili torti is characterized by hair that does not grow long, easily broken with twisted appearance.[4]
Two-thirds of patients have various atopic manifestations and increased serum IgE levels. Histopathology shows psoriasiform dermatitis. Other associations include aminoaciduria, recurrent infections, neurological deficits, delayed growth, short stature and failure to thrive. Treatment response to emollients, topical steroids, tacrolimus, psoralen and ultraviolet A irradiation have not been satisfactory.[5]
Hair shaft examination is an important investigation in congenital erythroderma. Our case highlights not only for its rare association with pili torti, but also the importance of early diagnosis through simple investigations like hair microscopy to prevent morbidity.
REFERENCES
- 1.Sun JD, Linden KG. Netherton syndrome: A case report and review of the literature. Int J Dermatol. 2006;45:693–7. doi: 10.1111/j.1365-4632.2005.02637.x. [DOI] [PubMed] [Google Scholar]
- 2.Chavanas S, Garner C, Bodsemer C, Ali M, Teillac DH, Wilkinson J, et al. Localization of the Netherton syndrome gene to chromosome 5q32, by linkage analysis and homozygosity mapping. Am J Hum Genet. 2000;66:914–21. doi: 10.1086/302824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pruszkowski A, Bodemer C, Fraitag S, Teillac-Hamel D, Amoric JC, de Prost Y. Neonatal and infantile erythrodermas: A retrospective study of 51 patients. Arch Dermatol. 2000;136:875–80. doi: 10.1001/archderm.136.7.875. [DOI] [PubMed] [Google Scholar]
- 4.Mirmirani P, Huang KP, Price VH. A practical, algorithmic approach to diagnosing hair shaft disorders. Int J Dermatol. 2011;50:1–12. doi: 10.1111/j.1365-4632.2010.04768.x. [DOI] [PubMed] [Google Scholar]
- 5.Smith DL, Smith JG, Wong SW, deShazo RD. Netherton's syndrome: A syndrome of elevated IgE and characteristic skin and hair findings. J Allergy Clin Immunol. 1995;95:116–23. doi: 10.1016/s0091-6749(95)70159-1. [DOI] [PubMed] [Google Scholar]


