Abstract
Objective:
To determine the diagnostic utility of adenosine deaminase (ADA) in exudative pleural effusions of different etiologies.
Setting and Design:
It was an observational study conducted at a tertiary care teaching institute.
Materials and Methods:
Of a total of 171 pleural fluid samples, 122 were found to be exudates and were included in the study. Pleural fluid ADA was done for all included patients. Pleural fluid ADA ≥40 U/l was taken as diagnostic cut off for TB effusion.
Statistical Analysis:
Sensitivity, specificity positive and negative predictive value of pleural fluid ADA for diagnosing TB was calculated by using clinical calculator – 1, Richard Lowry 2001-2013.
Results:
There were 171 patients with pleural effusion, out of which 122 (71.8%) were found to be exudative and were studied further. There were 49 (40.1%), 36 (29.5%) and 33 (27%) cases of TB, malignancy and para pneumonic effusion respectively, whereas 4 (3.3%) cases remained undiagnosed. Median ADA values for TB, malignancy and para pneumonic effusion were 55.8 U/l (range 9.7-756 U/l), 18 U/l (6.5-81 U/l) and 25 U/l (3.4-172 U/l) respectively. Pleural fluid ADA >40U/l yielded 85.7% sensitivity, 80.8% specificity, 75% positive predictive value and 89.5% negative predictive value.
Conclusion:
Pleural fluid ADA remains useful in diagnosing tuberculosis pleural effusion. The median ADA for TB effusion in present cohort was 51.8 IU/ml. Pleural fluid ADA of 40 U/L yielded 89.5% negative predictive value and 75% positive predictive value. Pleural fluid ADA is cost effective and good screening test for diagnosis of TB.
KEY WORDS: Adenosine deaminase, pleural effusion, tuberculosis
INTRODUCTION
Tuberculosis is a common cause of pleural effusion especially in countries like India.[1] Untreated tuberculous pleural effusion (TPE) can develop into active tuberculosis[2] so it is important to make rapid and accurate diagnosis for TPE and initiation of treatment. As we are aware, definitive diagnosis of tuberculosis is a difficult task, as in more than 50% of patients, pleura is the only site of infection.[2] Adenosine deaminase level in pleural fluid is a cost effective chemical biomarker and is routinely employed as a screening tool, in particular, in countries where tuberculosis is endemic.[1,3]
We conducted an observational study on diagnostic utility of adenosine deaminase (ADA) in exudative pleural effusions. The purpose of this study was to study diagnostic performance of ADA for tuberculosis in exudative pleural effusions in a high prevalence setting.
MATERIALS AND METHODS
All the patients fulfilling Light's criteria[4] (pleural fluid protein/serum protein >0.5; fluid LDH/serum LDH > 0.6) for exudative effusion were included in the study while transudative and post-traumatic pleural effusion were excluded. After taking informed consent and history, clinical examination, routine investigations were done in all the patients. Presence of first or more than one of the following criteria was adopted to label a case as tuberculous: (1) bacteriological confirmation of presence of Mycobacterium tuberculosis (direct smear or culture or histological finding); (2) histopathology finding of caseating granulomas; (3) radiological findings consistent with TB; (4) clinical presentation consistent with TB with positive tuberculin test (>20 mm induration) with exclusion of other clinical considerations; (5) definite clinical and radiological improvement in 2 months of administration of exclusive anti-tubercular treatment.[4] Pleural tap was done in all the cases and fluid tested for glucose, proteins, LDH, total ADA, microscopy, cytology and microbial testing (Gram staining, Z-N Staining, cultures). Pleural biopsy was done in selected cases of tuberculosis and malignancy. Effusion was called as malignant when pleural fluid cytology or pleural biopsy showed evidence of malignancy or if the patient had proved metastatic malignancy with no other detectable cause of effusion.
Uncomplicated parapneumonic effusion (UPE) referred to any exudative effusion associated with bacterial pneumonia, lung abscess or bronchiectasis which resolved with antibiotics alone, while patients with glucose <40 mg/dl or Gram stain or culture positive were classed as having complicated parapneumonic effusion (CPE), with empyema describing the presence of frank pus in the pleural cavity.[4]
Pleural fluid ADA ≥ 40 U/l was taken as diagnostic cut off for TB effusion.
RESULTS
A total of 171 cases of pleural effusion were evaluated, 122 out of which were found to have exudative pleural effusion. All patients with exudative pleural effusion were further divided into four groups: Tubercular pleural effusion (TPE), malignant pleural effusion, parapneumonic pleural effusion and undiagnosed pleural effusion. There were 49 (40.1%) cases of TB, 36 (29.5%) of malignancy and 33 (27%) of parapneumonic effusion whereas 4 (3.3%) remained undiagnosed. Overall male: Female ratio was 3:1, with all groups having more male patients than female. We found that those patients having TB effusion belonged to 45.32 ± 18.21 year age group compared to those with malignant pleural effusion 61.6 ± 13.48 year. Median ± SD value of ADA for TPE, malignant pleural effusion and parapneumonic effusion were 45.32 ± 18.21, 18 ± 12.78, and 27.45 ± 34.55 U/l respectively. Our study showed that 43 of 49 cases (87.7%) of patients with TPE had ADA ≥ 40 U/l while only 3 (8%) out of 36 cases of malignant pleural effusion had ADA ≥ 40 U/l. Pleural fluid ADA ≥ 40 U/L yielded 85.7% sensitivity, 80.8% specificity, positive predictive value was 75% and a negative predictive value was 89.5% for diagnosis of TB [Table 1]. Receiver operating curve was plotted for pleural fluid ADA and tuberculosis; it showed ADA of 40 has 79% sensitivitiy and 79% specificity [Figure 1].
Table 1.
Sensitivity, specificity, positive and negative predictive value of pleural fluid ADA 40 U/L in detecting tubercular pleural effusion
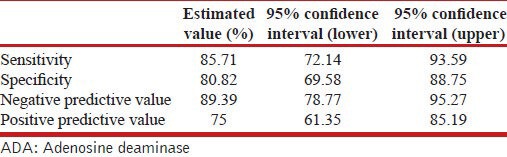
Figure 1.

ROC curve - Pleural fluid ADA and tuberculous effusion
In agreement with other studies, our study also showed that ADA > 40 U/l is suitable cut off to differentiate non-TPE from TPE.[5,6,7]
DISCUSSION
Tuberculosis is a common cause of pleural effusion especially in countries like India.[1,2,3] If untreated TPE can develop into active tuberculosis[4] so, it is important to make rapid and accurate diagnosis for TPE and initiation of treatment. Definitive diagnosis of tuberculosis is a difficult task, as in more than 50% of patients, pleura is the only site of infection.[4] Yield of closed pleural biopsy and its culture for MTB is respectively 80% and 55%. Thoracoscopy offers a near 100% positive diagnostic yield on histology and 76% positive on culture[8] but not available in all the centers. Although, lymphocytic predominant fluid is usually seen in tubercular pleural effusion but it is also seen in case of malignancy also. Adenosine deaminase (ADA) is an essential enzyme in the metabolism of purine nucleosides. Pleural fluid ADA estimation is quick and relatively inexpensive. Present study was conducted to assess the diagnostic utility of ADA in case of undiagnosed exudative effusions.
The most widely accepted cut-off level of ADA for the diagnosis of TPE is 40 U/l.[9,10] In present study we took ADA ≥ 40 U/l as in agreement with other studies. We found that 88% of TPE cases had ADA > 40U/l; whereas only 1% of those with malignancy had ADA > 40. Previous studies showed that less than 3% of patients suffering from non-tuberculous lymphocytic pleural effusions have reported ADA levels over the diagnostic cut-off of 40 U/l.[11,12,13,14,15,16] Apart from tuberculosis, second most common cause for elevated ADA in present study was parapneumonic effusion (11-33%), which was similar to other studies. However, parapneumonic effusion is usually neutrophilic unlike TPE which is lymphocytic.[2,3]
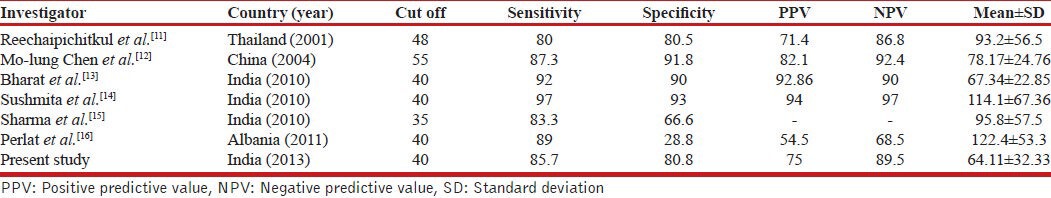
Receiver operating curve showed ADA of 40 had 79% sensitivitiy and 79% specificity [Figure 1]. We did comparison of sensitivity and specificity of present study with previously published studies which is shown in Table 2. Sensitivity and specificity in our study was almost similar to other previously published Indian studies.[11,12,13,14,15,16] Present study also showed that ADA 70 U/l increased specificity of the test to 99.5%, but at cost of sensitivity which fell to 34% [Figure 1].
Table 2.
Comparison of present study with previously published studies
In present study, 16 patients had confirmed diagnosis of TB with either demonstration of mycobacterium bacilli or demonstration of caseating granuloma on biopsy. It was first proposed by Valde's et al. to obviate pleural biopsy for the diagnosis of tuberculous pleuritis in patients younger than 35 years of age, in areas with an intermediate (say 25%) or high prevalence of tuberculosis.[17] We note that the administration of empirical anti-tuberculosis treatment to patients with lymphocytic exudates and a high ADA level in pleural fluid when there is clinical suspicion of tuberculosis is a common practice in intermediate-to-high burden settings like our country.[16] Moreover, the universal determination of ADA level in all the pleural fluid samples, and the follow-up of all the patients diagnosed with TPE until complete recovery under anti-tuberculosis treatment are positive features, enhancing the validity of our study.
CONCLUSIONS
Estimation of ADA level in pleural fluid is extremely helpful in establishing the etiology of tubercular pleural effusion and to rule out other diagnosis especially malignancy. Pleural fluid ADA still holds water and should be utilized for differentiating TB effusions from those of non-tubercular etiology.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Geneva, Switzerland: World Health Organization. Global Tuberculosis Control-WHO Report 2012. [Google Scholar]
- 2.Porcel JM. Tuberculous pleural effusion. Lung. 2009;187:263–70. doi: 10.1007/s00408-009-9165-3. [DOI] [PubMed] [Google Scholar]
- 3.Krenke R, Korczyński P. Use of pleural fluid levels of adenosine deaminase and interferon gamma in the diagnosis of tuberculous pleuritis. Curr Opin Pulm Med. 2010;16:367–75. doi: 10.1097/MCP.0b013e32833a7154. [DOI] [PubMed] [Google Scholar]
- 4.Light RW. Baltimore: Lippincot Williams and Wilkins; 2001. Pleural diseases; pp. 182–95. [Google Scholar]
- 5.Gupta BK, Bharat V, Bandyopadhyay D. Role of adenosine deaminase estimation in differentiation of tuberculous and non-tuberculous exudative pleural effusions. J Clin Med Res. 2010;2:79–84. doi: 10.4021/jocmr2010.03.280w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liang QL, Shi HZ, Wang K, Qin SM, Qin XJ. Diagnostic accuracy of adenosine deaminase in tuberculous pleurisy: A meta-analysis. Respir Med. 2008;102:744–54. doi: 10.1016/j.rmed.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 7.Garcia-Zamalloa A, Taboada-Gomez J. Diagnostic accuracy of adenosine deaminase and lymphocyte proportion in pleural fluid for tuberculous pleurisy in different prevalence scenarios. PLoS One. 2012;7:e38729. doi: 10.1371/journal.pone.0038729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Light RW. Update on tuberculous pleural effusion. Respirology. 2010;15:451–8. doi: 10.1111/j.1440-1843.2010.01723.x. [DOI] [PubMed] [Google Scholar]
- 9.Liang QL, Shi HZ, Wang K, Qin SM, Qin XJ. Diagnostic accuracy of adenosine deaminase in tuberculous pleurisy: A meta-analysis. Respir Med. 2008;102:744–54. doi: 10.1016/j.rmed.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 10.Greco S, Girardi E, Masciangelo R, Capoccetta GB, Saltini C. Adenosine Deaminase and interferon gamma measurements for the diagnosis of tuberculous pleurisy: A meta-analysis. Int J Tuberc Lung Dis. 2003;7:777–86. [PubMed] [Google Scholar]
- 11.Reechaipichitkul W, Kawamatawong T, Teerajetgul Y, Patjanasoontorn B. Diagnostic role of pleural fluid adenosine deaminase in tuberculous pleural effusion. Southeast Asian J Trop Med Public Health. 2001;32:383–9. [PubMed] [Google Scholar]
- 12.Chen ML, Yu WC, Lam CW, Au KM, Kong FY, Chan AY. Diagnostic value of pleural fluid adenosine deaminase activity in tuberculous pleurisy. Clin Chim Acta. 2004;341:101–7. doi: 10.1016/j.cccn.2003.11.016. [DOI] [PubMed] [Google Scholar]
- 13.Gupta B, Bharat V, Bandyopadhyay D. Role of adenosine deaminase estimation in differentiation of tuberculous and non-tuberculous exudative pleural effusions. J Clin Med Res. 2010;2:79–84. doi: 10.4021/jocmr2010.03.280w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chaudhary S, Patel AK. Role of pleural fluid adenosine deaminase (ADA) for the diagnosis of tuberculous pleural effusion. Calicut Med J. 2010;8:e4. [Google Scholar]
- 15.Sharma SK, Suresh V, Mohan A, Kaur P, Saha A, Kumar A, et al. A prospective study of sensitivity and specificity of adenosine deaminase estimation in the diagnosis of tuberculous pleural effusion. Indian J Chest Dis Allied Sci. 2001;43:149–55. [PubMed] [Google Scholar]
- 16.Kapisyzi P, Argiiri D, Aliko A, Beli J, Vakeflliy Y, Kore R, et al. The use of different cut off values of ADA liquid level in diagnosis of tuberculous pleurisy in countries with different incidence of tuberculosis. Chest. 2011;140:703A. [Google Scholar]
- 17.Valdexs L, Alvarez D, San JosexE, Panela P, Valle JM, Garcia-Pazos JM, et al. Tuberculous pleurisy: A study of 254 patients. Arch Intern Med. 1998;158:2017–21. doi: 10.1001/archinte.158.18.2017. [DOI] [PubMed] [Google Scholar]


