Abstract
Human immunodeficiency virus (HIV) disease is widespread all over the world, and the neurological and respiratory complications have been described previously. Peripheral neuropathy is one of the commonest neurological complications of the HIV infection. In this report we describe a HIV positive male smoker who was admitted to the hospital because of community acquired pneumonia. Bilateral diaphragmatic paralysis was diagnosed for which no other cause was found and was attributed to the HIV infection. Isolated phrenic neuropathy and diaphragmatic paralysis in an HIV positive patient is extremely rare and only a single such association has been described previously.
KEY WORDS: Bilateral phrenic nerve palsy, diaphragmatic paralysis, human immunodeficiency virus, peripheral neuropathy
INTRODUCTION
Bilateral diaphragmatic paralysis is a rare clinical condition due to different entities that can damage the phrenic nerves. Peripheral neuropathy is one of the most common neurological complications of human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) disease. The commonest forms of HIV-associated neuropathies are the distal sensory polyneuropathy and antiretroviral toxic neuropathy; disorders characterized mostly by sensory symptoms afflicting 40-50% of patients whose HIV disease is otherwise controlled by antiretroviral therapy. Motor mononeuropathy is an infrequent clinical form. Multiple causes of bilateral diaphragmatic paralysis are described. However, it is commonly caused by surgical or traumatic injuries, malignant neoplasm, and neurodegenerative disorders.[1] The relationship of phrenic paralysis with viral infections is rare but also well recognized[2] and exceptionally is a manifestation of a HIV-associated neuropathy, especially when it represents the only manifestation of peripheral neuropathy.
We report a rare case of bilateral diaphragmatic paralysis in an HIV infected patient.
CASE REPORT
A 42-year-old HIV positive male smoker on antiretroviral therapy (stavudine, efavirenz, and lamivudine) with very poor adherence to the medication regimen was admitted because of community acquired pneumonia. Since past one year, ordinary physical activity would result in breathlessness in the patient. There was no history of thoracic trauma or preexisting respiratory or cardiac diseases.
Clinical examination showed stable vital signs. Chest examination revealed paradoxical movement of the diaphragm, during inhalation, when the patient was in the supine position and coarse crepitations near the base of the left lung. All deep tendon reflexes were normal and there were no other signs of peripheral neuropathy.
Routine laboratory investigations were within normal limits. CD4 cell count was 170/μl and the plasma viral load was 74,746 copies/ml. Serological tests for Chagas disease, hepatitis B virus (HBV), and syphilis (Venereal Disease Research Laboratory (VRDL) and fluorescent treponemal antibody absorption (FTA ABS)) were negative whereas imunoglobulin G (IgG) anti-toxoplasma antibodies were positive. Electrocardiogram was normal. Chest X-ray revealed the elevation of the right and left hemidiaphragms in a full inspired film [Figure 1] and its immobility detected through a radioscopic examination. The cardiomediastinal silhouette was normal. There were no pulmonary infiltrates, pleural effusion, or mediastinal tumor in the computed tomography (CT) scan of the chest. The forced vital capacity in the sitting position was 1.84 L (48%) and it decreased to 1.29 L (34%) when brought to the dorsal decubitus position (change of <30%). Oxygen saturation while breathing ambient air was 96%. Transdiaphragmatic pressure was 2.99 cm H2O and confirmed the diagnosis of bilateral phrenic paralysis. During the examination, a negative deflection of the gastric pressure was observed as a sign of paradoxical movement of the diaphragm. The electromyography test showed an axonal damage to both phrenic nerves, without compromise in the other territories examined in his four limbs. Patient was started on a new scheme of antiretroviral therapy, without stavudine, and pulmonary rehabilitation exercises. Ten days later, he was discharged from the hospital in a good clinical condition. Patient was lost to follow-up.
Figure 1.
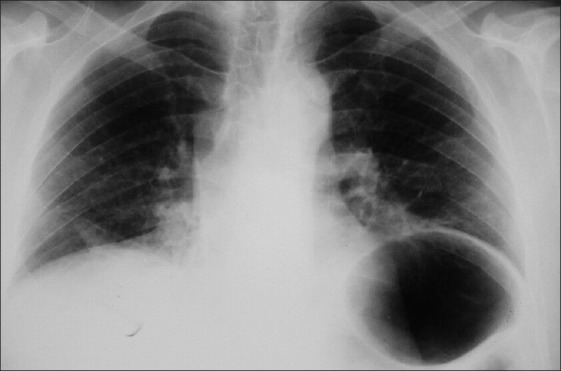
Chest X-ray showing bilateral elevation of both hemidiaphragms in a full inspired film
DISCUSSION
The diaphragm is the chief muscle of respiration and its paralysis can lead to dyspnea and can affect ventilatory function. Diaphragmatic paralysis can be unilateral or bilateral; the clinical symptoms being more prominent in bilateral paralysis. The symptoms, oxygenation and vital capacity, usually worsen in supine posture. The diagnoses is usually suspected on chest X-ray and clinical exam and confirmed with sniff test or phrenic nerve stimulation/diaphragm electromyography. Prognosis is usually poor in patients with advanced lung disease, bilateral paralysis, and chronic demyelinating conditions.[1,3]
Diaphragmatic innervations is from the phrenic nerve, which originates in motoneurons C3-C5. Phrenic nerve palsy is usually subdiagnosed.[1] It generally manifests as an accompaniment of a generalized polyneuropathy such as the Guillain Barré syndrome and isolated compromise is rare. It may be the initial manifestation of a multifocal motor neuropathy, in the course of an amyotrophic neuralgia of the shoulder, or in the cases of post extracorporeal circulation pump paralysis.[3] Postviral neuropathy and phrenic nerve involvement have been described following several viral infections like herpes zoster, poliovirus, West Nile virus and HIV infection.[4,5,6,7,8,9] The absence of these causes suggest that the phrenic nerve can be a target in idiopathic neuritis.[10] The etiology remains unidentified in more than two-third of the cases.[9]
HIV-associated neuropathies (HIV-N) have become the most frequent neurological disorder associated with HIV infection. The most common forms of HIV-N are the distal sensory polyneuropathy and antiretroviral toxic neuropathies. These disorders are characterized mostly by sensory symptoms that include spontaneous or evoked pain that follow a subacute or chronic course and afflicts 40-50% of patients whose HIV disease is otherwise controlled by antiretroviral therapy.[11,12,13] Advanced HIV disease (CD4 lymphocyte count ≤200/μl) predisposes the patient to different neuropathies.
HIV-associated sensory neuropathy is consistently associated with previous exposure to nucleoside reverse transcriptase inhibitors including stavudine (d4T), which is widely used in resource-limited settings. Stavudine, a nucleoside reverse transcriptase inhibitor, was used as first-line antiretroviral therapy (ART) in our patient and is said to exacerbate distal symmetrical polyneuropathy in HIV/AIDS patients. Although recent World Health Organization guidelines recommend withdrawing d4T from ART, it remains commonly used in resource-limited settings. Genetic variants in mitochondrial DNA haplogroups have been associated with increased risk of developing peripheral neuropathy in European non-Hispanic and black patients on stavudine.[14]
Isolated damage to the phrenic nerve in HIV infected patients is very rare. A Medline, Embase, and Cochrane databases search revealed that one report of a case of a 46-year-old patient, with TCD4 lymphocyte count of 250/μL and a plasma viral load of less than 50 copies/mL, who suffered a unilateral phrenic neuropathy that improved after the administration of intravenous IgG. Authors suggest that the pathogenicity of phrenic damage is of immune mediated type.[4]
In conclusion, unilateral or bilateral paralysis of phrenic nerves can be an infrequent manifestation of peripheral neuropathy in patients with HIV infection. This entity should be considered in the differential diagnosis of patients with HIV infection and respiratory symptoms.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Gibson GJ. Diaphragmatic paresis: Pathophysiology, clinical features, and investigation. Thorax. 1989;44:960–70. doi: 10.1136/thx.44.11.960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oike M, Naito T, Tsukada M, Kikuchi Y, Sakamoto N, Otsuki Y, et al. A case of diaphragmatic paralysis complicated by herpes-zoster virus infection. Intern Med. 2012;51:1259–63. doi: 10.2169/internalmedicine.51.6935. [DOI] [PubMed] [Google Scholar]
- 3.Qureshi A. Diaphragm paralysis. Semin Respir Crit Care Med. 2009;30:315–20. doi: 10.1055/s-0029-1222445. [DOI] [PubMed] [Google Scholar]
- 4.Piliero PJ, Estanislao L, Simpson D. Diaphragmatic paralysis due to isolated phrenic neuropathy in an HIV-infected man. Neurology. 2004;62:154–5. doi: 10.1212/wnl.62.1.154. [DOI] [PubMed] [Google Scholar]
- 5.Imai T, Matsumoto H. Insidious phrenic nerve involvement in postpolio syndrome. Intern Med. 2006;45:563–4. doi: 10.2169/internalmedicine.45.1657. [DOI] [PubMed] [Google Scholar]
- 6.Stowasser M, Cameron J, Oliver WA. Diaphragmatic paralysis following cervical herpes zoster. Med J Aust. 1990;153:555–6. doi: 10.5694/j.1326-5377.1990.tb126199.x. [DOI] [PubMed] [Google Scholar]
- 7.Betensley AD, Jaffery SH, Collins H, Sripathi N, Alabi F. Bilateral diaphragmatic paralysis and related respiratory complications in a patient with West Nile virus infection. Thorax. 2004;59:268–9. doi: 10.1136/thorax.2003.009092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brew BJ. The peripheral nerve complications of human immunodeficiency virus (HIV) infection. Muscle Nerve. 2003;28:542–52. doi: 10.1002/mus.10484. [DOI] [PubMed] [Google Scholar]
- 9.Ansari MK, Jha S, Nath A. Unilateral diaphragmatic paralysis following dengue infection. Neurol India. 2010;58:596–8. doi: 10.4103/0028-3886.68662. [DOI] [PubMed] [Google Scholar]
- 10.Valls-Solé J, Solans M. Idiopathic bilateral diaphragmatic paralysis. Muscle Nerve. 2002;25:619–23. doi: 10.1002/mus.10079. [DOI] [PubMed] [Google Scholar]
- 11.Pardo CA, McArthur JC, Griffin JW. HIV neuropathy: Insights in the pathology of HIV peripheral nerve disease. J Peripher Nerv Syst. 2001;6:21–7. doi: 10.1046/j.1529-8027.2001.006001021.x. [DOI] [PubMed] [Google Scholar]
- 12.Wulff EA, Wang AK, Simpson DM. HIV-associated peripheral neuropathy: Epidemiology, pathophysiology and treatment. Drugs. 2000;59:1251–60. doi: 10.2165/00003495-200059060-00005. [DOI] [PubMed] [Google Scholar]
- 13.Huang W, Calvo M, Karu K, Olausen HR, Bathgate G, Okuse K, et al. A clinically relevant rodent model of the HIV antiretroviral drug stavudine induced painful peripheral neuropathy. Pain. 2013;154:560–75. doi: 10.1016/j.pain.2012.12.023. [DOI] [PubMed] [Google Scholar]
- 14.Kampira E, Kumwenda J, van Oosterhout JJ, Dandara C. Mitochondrial DNA subhaplogroups L0a2 and L2a modify susceptibility to peripheral neuropathy in Malawian adults on stavudine containing highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2013 doi: 10.1097/QAI.0b013e3182968ea5. [DOI] [PMC free article] [PubMed] [Google Scholar]


