Abstract
BACKGROUND
We sought to identify differences among black and white Medicare-insured patients with colorectal cancer who underwent resection.
METHODS
Surveillance, Epidemiology and End Results–Medicare (SEER-Medicare) linked inpatient data from 1986 to 2005 were examined. Differences in short- and long-term outcomes among black vs white patients were investigated.
RESULTS
There were 125,676 (92.4%) white and 9,891 (7.6%) black patients who met the criteria. Black patients were younger (75.5 vs 77.2 years; P < .001) but had more comorbidities than did white patients (mean Charlson comorbidity index score 3.99 vs 3.87; P < .001). Black patients demonstrated greater odds of in-hospital mortality (odds ratio [OR], 1.43; 95% confidence interval [CI], 1.30 to 1.56) and readmission within 30 days (OR, 1.26; 95% CI, 1.18 to 1.34). Comparing 1986 to 1990 vs 2001 to 2005, black patients had greater odds of 30-day readmission (OR, 1.12 vs 1.31) but reduced odds of index in-hospital mortality (OR, 1.84 vs 1.28). Black patients had worse long-term survival after colorectal surgery (hazard ratio [HR], 1.21; 95% CI, 1.17 to 1.25; P < .001).
CONCLUSIONS
Black patients with colorectal cancer demonstrated increased risk of mortality and readmission after controlling for age, sex, and comorbidities. Although black vs white differences in perioperative mortality decreased over time, disparities in readmission and long-term survival persisted.
Keywords: Colorectal cancer, Race, Disparities, SEER-Medicare
Colon and rectal cancers are relatively common in the United States, with more than 140,000 new cases diagnosed annually.1 Colon and rectal cancers are associated with substantial morbidity and cost and cause more than 50,000 deaths in the United States each year.1 Colorectal cancer is more common among black individuals than among whites. In addition, black patients with colorectal cancer are also more likely than white patients to die of the disease.2 Black patients diagnosed with colorectal cancer have also been shown to be less likely to undergo surgical treatment of their disease than are white patients.2 Although the reasons for these findings remain unclear, some investigators have suggested that black patients more commonly present with late-stage disease and that this is largely responsible for the lower rate of operability and the higher mortality among black patients than among white patients.2
Black patients typically have disproportionally lower socioeconomic status compared with white patients and are less likely to carry health insurance coverage.3 In turn, uninsured patients undergoing surgical treatment of gastrointestinal disease tend to have more severe disease, are more likely to receive suboptimal surgical treatment, and more often die compared with patients who have health insurance.4 These differences in socioeconomic and insurance status, along with the higher levels of medical comorbidity typically present among black patients, have been implicated as important factors driving race-based disparities in health care outcomes.5 Specifically, black surgical patients have been observed to suffer higher rates of mortality, complications, and readmission compared with white patients undergoing a variety of similar surgical procedures.6 Some of these worse outcomes may be attributable to insurance status; black individuals younger than 65 years of age are less likely to have health insurance compared with white patients.7
In the current study, we sought to examine possible black vs white differences in surgical interventions and outcomes for patients with colorectal cancer independent of insurance coverage. To accomplish this, we used the Surveillance, Epidemiology and End Results–Medicare (SEER-Medicare) linked data set. By including only patients covered by Medicare, we were able to examine a cohort of patients with homogeneous insurance coverage. In addition, data on underlying medical comorbidities were readily available in Medicare, which allowed for risk adjustment of medical comorbidities to assess the independent effect of race on outcome. Finally, we investigated whether race-based disparities have changed over time by comparing patient presentation (emergent and urgent vs elective) and outcomes (in-hospital mortality, length of stay, and 3-year mortality) over a 20-year period.
Methods
Data from the SEER-Medicare data set between 1986 and 2005 were used. Patients 65 years of age and older with a diagnosis of primary colon or rectal cancer were selected. Specifically, those patients with a diagnosis of colon or rectal cancer who underwent a colon or rectal procedure were identified using the International Classification of Diseases, Ninth Revision, Clinical Modification procedure codes for appropriate colorectal operations (45.71 to 45.76, 45.79, 45.8, 48.5, 48.62, 48.63, and 48.69). The Johns Hopkins Hospital Institutional Review Board gave approval for the current study.
Surgery admission type, in-hospital mortality, and length of stay during the index hospitalization were captured from the data set, as were discharge disposition, readmission within 30 days, and 3-year mortality. Patients undergoing a colorectal procedure with a diagnosis of primary colon or rectal cancer were categorized as being either black or white. Surgical patients admitted on an emergency or urgent basis were classified as emergent vs surgical patients admitted electively who were classified as elective.8 Medical comorbidities were characterized based on International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis codes present at the index admission to generate a Charlson comorbidity index score for each individual.9 Information on hospital teaching status and location (urban vs rural) became available in 1996, and these hospital-level variables were examined for the period 1996 through 2005. For the purposes of this study, readmission was defined as admission to an acute or short-term care hospital within 30 days of the index discharge and specifically excluded admissions to skilled nursing care or rehabilitation facilities, as well as admissions associated with discharge from the index hospital directly to a short-term general hospital or any other type of long-term care hospital.10
The impact of race on admission type, in-hospital mortality, and length of stay, as well as readmission and 3-year mortality was examined. Underlying differences between black and white patients were examined using the Student t test, Wilcoxon rank-sum test, and chi-square test where appropriate. Proportions of emergent vs elective surgery and mortality were examined using the chi-square test. Differences between black and white patients for each outcome were calculated using unadjusted logistic regression and expressed as odds ratios (ORs). In addition, logistic regression models that adjusted for age, sex, and medical comorbidity (Charlson comorbidity index) and tumor stage were also used. The Cox proportional hazard model was used to examine differences in 3-year mortality between black and white patients. To evaluate for trends in outcomes over time, analyses were also stratified by 5-year time intervals (1986 to 1990, 1991 to 1995, 1996 to 2000, and 2001 to 2005). All data analyses were completed using STATA, version 11.2 (StataCorp, College Station, TX).
Results
Between 1986 and 2005, a total of 120,832 unique individuals who were categorized as either black or white met SEER-Medicare criteria for inclusion as patients diagnosed with primary colorectal cancer; only patients with complete data on admission type and tumor stage at diagnosis were included in the study cohort. Among the 120,832 patients in the study cohort, 112,306 (92.9%) patients were white and 9,891 (7.1%) were black. On average, black patients were slightly younger (75.7 vs 77.1 years; P < .001) and more likely to be women (60.4% vs 55.3%; P < .001) than were white patients. Compared with white patients, black patients had more medical comorbidities, as reflected in a higher mean Charlson comorbidity index (mean Charlson score: black patients, 4.00 vs white patients, 3.88; P < .001). Black patients were also more likely than white patients to present with advanced (ie, distant) disease at the time of initial diagnosis (16.9% vs 13.3%, respectively; P < .001). During the period in which hospital-level variables were available (1996 to 2005), black patients were more likely to be treated at urban hospitals (black patients, 96.0% vs white patients, 87.6%; P < .001) and at teaching hospitals (black patients, 76.9% vs white patients, 64.3%; P < .001) than were white patients (Table 1).
Table 1.
Patient and hospital characteristics
| Characteristic | White (n = 112,306) | Black (n = 8,526) | P value |
|---|---|---|---|
| Age (y), mean (SD) | 77.1 (7.2) | 75.7 (7.1) | <.001 |
| Female sex | 62,055 (55.3%) | 5,151 (60.4%) | <.001 |
| Mean Charlson comorbidity index score (SD) | 3.88 (2.15) | 4.00 (2.18) | <.001 |
| Stage | |||
| In situ | 3,859 (3.4%) | 368 (4.3%) | <.001 |
| Localized | 47,130 (42.0%) | 3,247 (38.1%) | |
| Regional | 46,346 (41.3%) | 3,467 (40.7%) | |
| Distant | 14,971 (13.3%) | 1,444 (16.9%) | |
| Hospital* | |||
| Rural | 5,371 (12.4%) | 142 (4.0%) | <.001 |
| Teaching | 23,309 (64.3%) | 3,275 (76.9%) | <.001 |
SD = standard deviation.
Hospital data available only from 1996 to 2005.
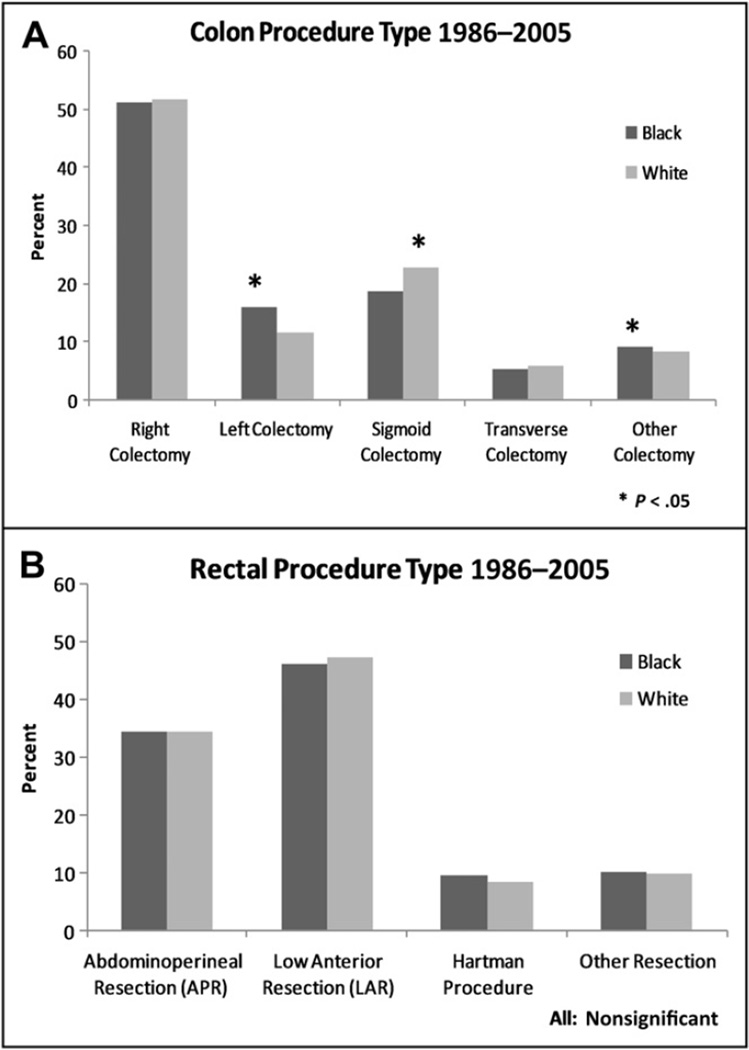
Compared with white patients with colorectal cancer, black patients with colorectal cancer had a higher proportion of emergency admission for colorectal surgery (47.3% vs 40.5%, respectively; P < .001) (Table 2); this increased odds of emergent admission persisted even after controlling for age, sex, and medical comorbidities (OR, 1.28; 95% confidence interval [CI], 1.23 to 1.34; P < .001) The type of surgical resection, however, was largely similar among black and white patients (colon procedures: right colectomy, 52.8% vs 52.1%, P = .333; transverse colectomy, 5.2% vs 5.7%, P =.081; left colectomy, 15.9% vs 11.6%, P < .001; sigmoid colectomy: 22.7% vs 18.8%, P < .001; total or other colectomy, 9.0% vs 8.2%, P =.034; rectal procedures: abdominoperineal resection, 34.5% vs 34.4%; low anterior resection, 46.1% vs 47.4%; Hartman procedure, 9.4% vs 8.4%; other, 10.2% vs 9.8%; all P > .05) (Fig. 1). On pathologic examination, the proportion of patients with localized (black patients, 38.1% vs white patients, 42.0%) vs regional (black patients, 40.7% vs white patients, 41.3%) disease was different between the 2 groups (both P < .001). Although tumor grade (low to moderate: black patients, 75.5% vs white patients, 75.6%; P = .777) was comparable, lymph node metastasis was more common among black patients (black patients, 40.5% vs white patients, 36.6%; P < .001).
Table 2.
Admission type and outcomes
| Variable | White | Black | P value |
|---|---|---|---|
| Emergency or urgent admission | 45,303 (40.5%) | 4,011 (47.3%) | <.001 |
| In-hospital mortality | 4,589 (4.1%) | 445 (5.2%) | <.001 |
| Mean length of stay (d) (SD) | 11.5 (8.4) | 13.7 (10.4) | <.001 |
| 30-day readmission | 12,272 (10.9%) | 1,122 (13.2%) | <.001 |
| In-hospital mortality during readmission | 5,015 (6.0%) | 440 (6.9%) | .004 |
SD = standard deviation.
Figure 1.
Details of (A) colon and (B) rectal cancer surgical procedures stratified by white vs black race.
Postoperatively, 43,802 patients had complications, for an overall morbidity of 36.4%. Black patients (39.8%) were more likely to have at least 1 complication during their admission compared with white patients (36.2%) (P < .001). In addition, in-hospital mortality after colorectal surgery was higher among black patients (black patients, 5.2% vs white patients, 4.1%; P < .001). After adjustment for competing risk factors, including medical comorbidities, black patients were still noted to have higher in-hospital mortality (OR, 1.25; 95% CI, 1.13 to 1.38; P < .001). The average length of hospital stay was also longer for black patients compared with white patients (13.7 days vs 11.5 days, respectively; P < .001). At time of discharge from acute care hospitals, black patients were more likely to be discharged to home (black patients, 83.6% vs white patients, 81.5%) than to a skilled nursing or other inpatient facility (black patients, 16.4% vs white patients, 18.5%) (P < .001).
There were a total of 13,332 readmissions within 30 days, for an overall readmission rate of 11.1%. Black patients had a higher likelihood of being readmitted within 30 days of discharge (black patients, 13.2% vs white patients, 10.9%; P < .001). After controlling for other risk factors, black race remained independently associated with an increased risk of readmission (OR, 1.23; 95% CI, 1.15 to 1.32; P < .001). The mean time to readmission was comparable among black and white patients (11.4 days vs 11.2 days, respectively; P = .651). Although some common causes of readmission were similar among black and white patients (digestive complications: black patients, 8.7% vs white patients, 9.1%; P = .594; postoperative infection: black patients, 3.9% vs white patients, 3.9%; P=.977), dehydration as a cause of readmission was more common among black patients (black patients, 6.7% vs white patients, 4.6%; P =.001). Of note, black patients were more likely to experience in-hospital mortality during the readmission stay (black patients, 6.9% vs white patients, 6.0%; P =.004) (OR, 1.09; 95% CI, .98 to 1.21) (Table 3). Mean length of stay during readmission was 9.7 days for black patients vs 8.1 days for white patients (P < .001). After the readmission discharge, black and white patients were equally likely to be discharged to home (black patients, 71.7% vs white patients, 71.7%) as to skilled nursing or other inpatient facility (black patients, 28.3% vs white patients, 28.3%) (P =.989).
Table 3.
Multivariable logistic regression models: black vs white outcomes (1986–2005)
| N = 120,295 | Odds Ratio |
95% Confidence Interval |
|---|---|---|
| Urgent or emergency admission | ||
| Black race | 1.28 | 1.23–1.34 |
| Male sex | .83 | .81–.85 |
| Localized disease | 1.18 | 1.10–1.26 |
| Regional disease | 1.53 | 1.43–1.64 |
| Distant disease | 1.97 | 1.83–2.12 |
| Charlson morbidity index score ≥ 3 | 1.20 | 1.17–1.23 |
| In-hospital mortality during index admission | ||
| Black race | 1.25 | 1.13–1.38 |
| Male sex | 1.10 | 1.04–1.16 |
| Localized disease | 1.07 | .89–1.28 |
| Regional disease | 1.05 | .95–1.38 |
| Distant disease | 1.97 | 1.63–2.39 |
| Charlson comorbidity index score ≥ 3 | 1.60 | 1.49–1.71 |
| 30-day readmission | ||
| Black race | 1.24 | 1.16–1.32 |
| Male sex | 1.16 | 1.12–1.20 |
| Localized disease | 1.01 | .92–1.13 |
| Regional disease | 1.00 | .90–1.11 |
| Distant disease | 1.14 | 1.01–1.27 |
| Charlson comorbidity index score ≥ 3 | 1.31 | 1.26–1.37 |
| In-hospital mortality during 30-day readmission | ||
| Black race | 1.09 | .98–1.21 |
| Male sex | 1.14 | 1.08–1.20 |
| Localized disease | .93 | .79–1.11 |
| Regional disease | 1.04 | .88–1.23 |
| Distant disease | 1.53 | 1.28–1.82 |
| Charlson comorbidity index score R3 | 2.73 | 2.57–2.90 |
Comparison group: white race, in situ disease, Charlson comorbidity index score < 3.
To investigate temporal trends, changes in the emergent admissions, index hospital mortality, and 30-day readmission were compared using 5-year intervals across a 20-year period. Compared with white patients, black patients had increasingly higher odds of emergent admission over time (1986 to 1990: OR, 1.18; 95% CI, 1.07 to 1.31; P =.001 vs 2001 to 2005: OR, 1.46; 95% CI, 1.33 to 1.60; P < .001). Of note, although black patients had higher odds of index in-hospital mortality compared with white patients between 1986 and 1990 (OR, 1.64; 95% CI, 1.33 to 2.01; P < .001), no such increase was noted in the more recent periods examined (2001 to 2005: OR, 1.12; 95% CI, .90 to 1.39; P =.317) (Table 4). Black patients were more likely to be readmitted if discharge was between 2001 and 2005 (OR, 1.30; 95% CI, 1.15 to 1.48; P < .001) compared with earlier periods examined (1986 to 1990: OR, 1.15; 95% CI, .97 to 1.36; P =.100). Mortality during readmission also changed over time. Specifically, compared with white patients, black patients demonstrated a trend toward higher odds of mortality during readmission between 1986 and 1990 (OR, 1.48; 95% CI, .91 to 2.43; P = .113), whereas a reduction in the differential odds of readmission mortality was noted in the more recent periods examined (2001 to 2005: OR, .51; 95% CI, .29 to .90; P =.021) (Table 4).
Table 4.
Black and white outcome differences comparing 1986–1990 vs 2001–2005
| 1986–1990 | 2001–2005 | |||
|---|---|---|---|---|
| Odds Ratio* | 95% Confidence Interval | Odds Ratio* | 95% Confidence Interval | |
| Urgent or emergent admission | ||||
| Black race | 1.18 | 1.07–1.31 | 1.46 | 1.33–1.60 |
| In-hospital mortality | ||||
| Black race | 1.64 | 1.33–2.01 | 1.12 | .90–.39 |
| 30-day readmission | ||||
| Black race | 1.15 | .97–1.36 | 1.30 | 1.15–1.48 |
Multivariable logistic regression controlling for age, sex, stage, and comorbidity.
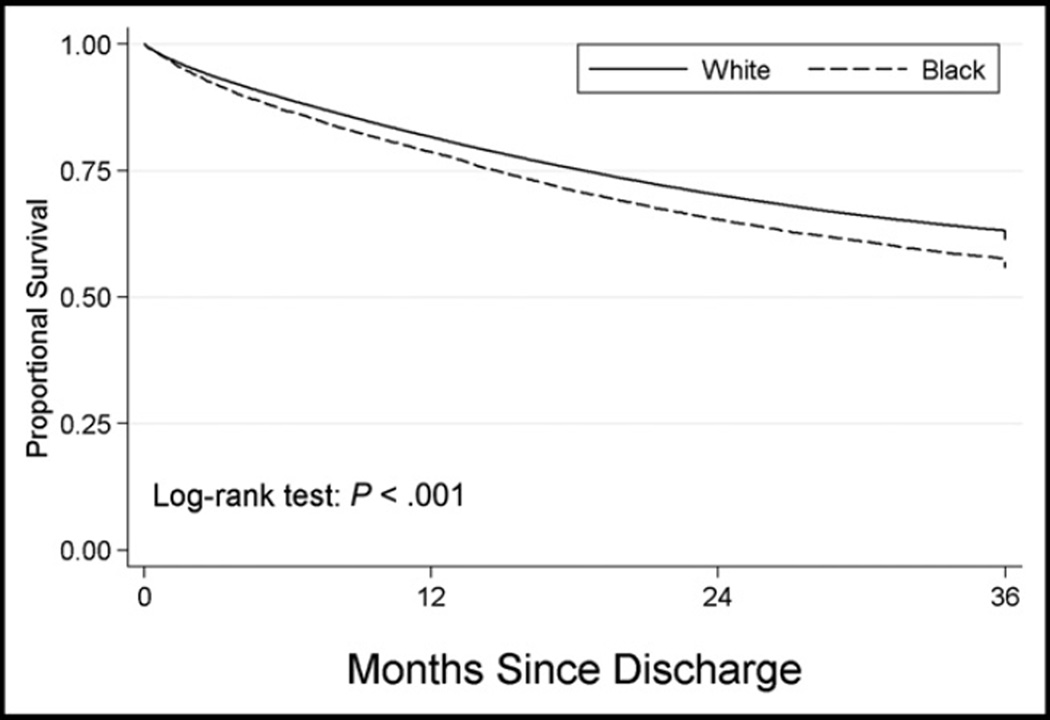
After colorectal surgery, median and 3-year overall survival among black patients was worse than in white patients (median and 3-year survival: black patients, 97.2 months and 53.3% vs white patients, 132.4 months and 59.1%, respectively; log-rank P < .001) (Fig. 2). After controlling for age, sex, tumor stage, and underlying comorbidity, black patients remained at a higher risk of long-term death after colorectal surgery (HR, 1.21; 95% CI, 1.17 to 1.25; P < .001). To assess whether the difference in survival was secondary to differences in the proportion of black vs white patients with stage IV disease, a separate Cox proportional hazard model was constructed that excluded all patients with stage IV disease. In this model, which included only patients with local or regional disease, black patients still had a higher risk of 3-year mortality than did white patients (HR, 1.26; 95% CI, 1.19 to 1.30; P < .001).
Figure 2.
Long-term survival stratified by white vs black race. Three-year survival was worse among black patients after colorectal surgery than among white patients.
Comments
Black patients have been noted to have higher mortality after surgery than do white patients.6,11,12 Several studies have noted an increased mortality among black patients after certain nononcologic operations, such as cardiac surgery.13 Fewer studies have examined the impact of race on outcome after cancer surgery, and most of these studies have focused on long-term survival differences between white and black patients.11 Although black patients have been described as having worse long-term cancer outcomes, the reason for these differences remains unclear. Laiyemo et al14 observed a lower follow-up for screen-detected abnormalities among black patients compared with white patients and lower overall health care use among black patients. In turn, some investigators have suggested that differences in outcomes may be attributable to insurance status among black vs white patients.7 The current study is important because we used SEER-Medicare data to analyze a patient population with comparable insurance coverage. We found that Medicare beneficiaries undergoing surgical treatment for colorectal cancer who were black had significantly higher odds of being treated on an emergent basis, as well as dying in the hospital during their index stay. Unlike other studies, we also specifically examined rates of readmission among black vs white patients and noted that black patients were also more likely to be readmitted within 30 days of discharge. In fact, black patients who were readmitted to acute care hospitals within 30 days of discharge were proportionally more likely to die during the readmission stay than were white patients. In addition, black patients had worse long-term survival compared with white patients.
In the current study, we examined a number of short-term outcomes to determine if the hospital course of black patients was different than that of white patients after colorectal surgery. Like several previous studies, we investigated perioperative morbidity and mortality.8,10,15 Lucas et al6 noted that black patients are more likely than white patients to present at smaller, less well staffed hospitals where outcomes tend to be worse; as a group, black patients tend to be treated by less experienced surgeons or surgeons who have not undergone advanced specialized training. In the current study, similar to previous reports from our group,16 we noted that black patients (39.8%) were more likely to have at least 1 complication during their admission compared with white patients (36.2%) (P < .001). In addition, black patients demonstrated 25% greater odds of death during their index hospital admission compared with white patients. The reason for this is undoubtedly multifactorial. In part, the higher in-hospital mortality may have been related to the increased comorbidities among black patients, as well as the increased proportion of emergent admissions, which may be driven by screening delays or lower screening rates among black patients.2 Our group previously demonstrated that emergent admission was an independent predictor of mortality in patients undergoing non–cancerrelated gastrointestinal surgery, as well other surgical procedures.12,17 Interestingly, in the current study, we did find that the effect of black race on in-hospital mortality after colorectal surgery decreased over time. Specifically, although black race was an independent predictor of index in-hospital mortality during the 5-year period from 1986 to 1990, black race was no longer associated with significantly greater odds of index in-hospital mortality during the period between 2001 and 2005.
We also examined other important metrics of short-term outcome, including length of stay, discharge destination, and readmission. Interestingly, the average length of hospital stay was longer for black patients than for white patients (13.7 days vs 11.5 days, respectively; P < .001). In addition, when discharged, black patients were more likely than white patients to be discharged home rather than to a skilled nursing facility, despite on average having more medical comorbidities, a higher inpatient complication rate, and a longer length of stay. Laiyemo et al14 demonstrated that black patients were less likely to use health care resources than were white patients. In a separate study, Rogers et al15 noted that black patients may not experience the same level of medical care as do white patients and may be less likely to benefit from certain features of the health care system. This might help explain some of the differences among black vs white patients with regard to the number of patients discharged to skilled nursing facilities. Another interesting finding of the current study was that black patients were more likely to experience readmission within 30 days of discharge. In fact, the comparative odds of 30-day readmission tended to be higher in black than in white patients across both the earliest and latest periods studied. Part of this difference may result from black patients presenting with more medical comorbidities and their higher incidence of perioperative complications during the index hospital admission.
After colorectal surgery, long-term outcome was also worse among black patients. In fact, median survival among black patients was about 75% that of white patients (97.2 months vs 132.4 months, respectively). Black patients have been noted to have a lower follow-up for screen-detected colonoscopic abnormalities and therefore often present with later stage disease.14 We similarly noted that black patients were more likely to present with later stage disease than were white patients. In fact, 16.9% of black patients presented with stage IV metastatic disease compared with only 13.3% of white patients. Differences in long-term outcome, however, did not seem to be solely related to differences in stage at presentation. Specifically, even after controlling for tumor stage using multivariate and stratified analyses, we noted a persistent disparity in long-term survival after colorectal surgery in black patients vs white patients among Medicare beneficiaries. Our data are consistent with the findings of systematic review by Hodgson et al,18 which noted that black patients with colorectal cancer were more likely to die of disease than were white patients. In contrast, Rogers et al15 failed to find a difference in outcomes between black and white patients with colorectal cancer among elderly Tennesseans covered by Medicaid and Medicare. In the Rogers et al15 study, the authors reported that although black patients were less likely to have surgery, black and white patients had comparable long-term survival. Of note, the Rogers et al15 study included a population of patients with dual enrollment in both Medicare and Medicaid, which allows for expanded outpatient coverage and access. This may explain, in part, the differences reported with regard to outcomes such as long-term survival.
The current study had several limitations. Given that we used the Medicare database, our patient population was confined to those age 65 years or older. As such, the data may not be applicable to younger patient populations. There were also limitations regarding collection of certain data, including hospital-level variables and hospital identifiers, which did not permit comprehensive analysis of these factors and prevented us from clustering patients by hospital. Also, although all patients were eligible for Medicare coverage, we were unable to determine whether patients in our study relied on Medicare alone or had additional coverage supplemental to their Medicare policy. Further, the data available did not permit the examination of socioeconomic status or race-related variability in access to health care services before Medicare eligibility at age 65 years. Finally, unknown barriers to timely surgical intervention may exist for black patients, even when health insurance is present or treatment is required by statute.19,20
Conclusions
In conclusion, compared with white patients, black race was associated with increased emergent admission, in-hospital mortality, 30-day readmission, and 3-year mortality after colorectal surgery. Our data debunk the notion that the worse health outcomes experienced by black patients among patients with resected colorectal cancer is merely a function of inadequate health insurance coverage. In addition, by controlling for medical comorbidities, our data suggest that such differences are unlikely to be solely attributable to the greater medical comorbidities among black patients compared with white patients. The root causes driving the observed differences in hospital mortality, readmission, and long-term outcome need to be elucidated in future studies. Only by identifying the underlying factors responsible for black vs white differences in overall mortality after surgery can interventions be developed to eliminate disparities in outcomes among all surgical patients.
Acknowledgments
Dr. Pawlik was supported in part by the Jill Williams Memorial Research Fund.
Dr. Haider was supported by the National Institutes of Health/ NIGMS K23GM093112-01 and American College of Surgeons C. James Carrico Fellowship for the Study of Trauma and Critical Care.
Footnotes
Sponsoring agencies had no involvement in the study design; in the collection, analysis, and interpretation of data; in the writing of the manuscript; or in the decision to submit the manuscript for publication.
Presented at The Society of Black Academic Surgeons 22nd Annual Scientific Assembly, April 12–14, 2012, Baltimore, MD, USA.
References
- 1.U.S. Cancer Statistics Working Group. United States Cancer Statistics: 1999–2009 Incidence and Mortality Data. Department of Health and Human Services, Centers for Disease Control and Prevention, and National Cancer Institute. [Accessed: March 4, 2012];2012 Available at: http://www.cdc.gov/uscs; 2012.
- 2.Polite BN, Dignam JJ, Olopade OI. Colorectal cancer and race: understanding the differences in outcomes between African Americans and whites. Med Clin North Am. 2005;89:771–793. doi: 10.1016/j.mcna.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 3.Kirby JB, Kaneda T. Unhealthy and uninsured: exploring racial differences in health and health insurance coverage using a life table approach. Demography. 2010;47:1035–1051. doi: 10.1007/BF03213738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lidor AO, Gearhart SL, Wu AW, et al. Effect of race and insurance status on presentation, treatment, and mortality in patients undergoing surgery for diverticulitis. Arch Surg. 2008;143:1160–1165. doi: 10.1001/archsurg.143.12.1160. discussion 1165. [DOI] [PubMed] [Google Scholar]
- 5.Williams DR. Race, socioeconomic status, and health. The added effects of racism and discrimination. Ann N Y Acad Sci. 1999;896:173–188. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- 6.Lucas FL, Stukel TA, Morris AM, et al. Race and surgical mortality in the United States. Ann Surg. 2006;243:281–286. doi: 10.1097/01.sla.0000197560.92456.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agency for Healthcare Research and Quality. Rockville, MD: U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality; 2008. Feb, [Accessed: March 4, 2012]. 2007 National Healthcare Quality Report. AHRQ Pub. No. 08–0040. Available at: http://archive.ahrq.gov/qual/nhqr07/nhqr07.pdf. [Google Scholar]
- 8.Lidor AO, Segal JB, Wu AW, et al. Older patients with diverticulitis have low recurrence rates and rarely need surgery. Surgery. 2011;150:146–153. doi: 10.1016/j.surg.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 9.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 10.Schneider EB, Hyder O, Brooke BS, et al. Patient readmission and mortality after colorectal surgery for colon cancer: impact of length of stay relative to other clinical factors. J Am Coll Surg. 2012;214:390–398. doi: 10.1016/j.jamcollsurg.2011.12.025. discussion 398–9. [DOI] [PubMed] [Google Scholar]
- 11.Marcella S, Miller JE. Racial differences in colorectal cancer mortality. The importance of stage and socioeconomic status. J Clin Epidemiol. 2001;54:359–366. doi: 10.1016/s0895-4356(00)00316-4. [DOI] [PubMed] [Google Scholar]
- 12.Schneider EB, Haider A, Sheer AJ, et al. Differential association of race with treatment and outcomes in Medicare patients undergoing diverticulitis surgery. Arch Surg. 2011;146:1272–1276. doi: 10.1001/archsurg.2011.280. [DOI] [PubMed] [Google Scholar]
- 13.Becker ER, Rahimi A. Disparities in race/ethnicity and gender in in-hospital mortality rates for coronary artery bypass surgery patients. J Natl Med Assoc. 2006;98:1729–1739. [PMC free article] [PubMed] [Google Scholar]
- 14.Laiyemo AO, Doubeni C, Pinsky PF, et al. Race and colorectal cancer disparities: health-care utilization vs. different cancer susceptibilities. J Natl Cancer Inst. 2010;102:538–546. doi: 10.1093/jnci/djq068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rogers SO, Ray WA, Smalley WE. A population-based study of survival among elderly persons diagnosed with colorectal cancer: does race matter if all are insured? (United States) Cancer Causes Control. 2004;15:193–199. doi: 10.1023/B:CACO.0000019511.67989.09. [DOI] [PubMed] [Google Scholar]
- 16.Chang DC, Handly N, Abdullah F, et al. The occurrence of potential patient safety events among trauma patients: are they random? Ann Surg. 2008;247:327–334. doi: 10.1097/SLA.0b013e31815aab0d. [DOI] [PubMed] [Google Scholar]
- 17.Schneider EB, Haider AH, Lidor AO, et al. Global surgical package reimbursement and the acute care surgeon: a threat to optimal care. J Trauma. 2011;70:583–589. doi: 10.1097/TA.0b013e3182098a30. [DOI] [PubMed] [Google Scholar]
- 18.Hodgson DC, Fuchs CS, Ayanian JZ. Impact of patient and provider characteristics on the treatment and outcomes of colorectal cancer. J Natl Cancer Inst. 2001;93:501–515. doi: 10.1093/jnci/93.7.501. [DOI] [PubMed] [Google Scholar]
- 19.Crompton JG, Pollack KM, Oyetunji T, et al. Racial disparities in motorcycle-related mortality: an analysis of the National Trauma Data Bank. Am J Surg. 2010;200:191–196. doi: 10.1016/j.amjsurg.2009.07.047. [DOI] [PubMed] [Google Scholar]
- 20.Greene WR, Oyetunji TA, Bowers U, et al. Insurance status is a potent predictor of outcomes in both blunt and penetrating trauma. Am J Surg. 2010;199:554–557. doi: 10.1016/j.amjsurg.2009.11.005. [DOI] [PubMed] [Google Scholar]