Seizures are common among critically ill patients, but their relationship to outcome remains unclear. In a cohort of critically ill children, Payne et al. demonstrate that increasing electrographic seizure burden is independently associated with short-term neurological decline, even after adjusting for seizure aetiology and illness severity.
Keywords: seizure burden, continuous video-EEG monitoring, outcome, critical illness, child
Abstract
Seizures are common among critically ill children, but their relationship to outcome remains unclear. We sought to quantify the relationship between electrographic seizure burden and short-term neurological outcome, while controlling for diagnosis and illness severity. Furthermore, we sought to determine whether there is a seizure burden threshold above which there is an increased probability of neurological decline. We prospectively evaluated all infants and children admitted to our paediatric and cardiac intensive care units who underwent clinically ordered continuous video-electroencephalography monitoring over a 3-year period. Seizure burden was quantified by calculating the maximum percentage of any hour that was occupied by electrographic seizures. Outcome measures included neurological decline, defined as a worsening Paediatric Cerebral Performance Category score between hospital admission and discharge, and in-hospital mortality. Two hundred and fifty-nine subjects were evaluated (51% male) with a median age of 2.2 years (interquartile range: 0.3 days–9.7 years). The median duration of continuous video-electroencephalography monitoring was 37 h (interquartile range: 21–56 h). Seizures occurred in 93 subjects (36%, 95% confidence interval = 30–42%), with 23 (9%, 95% confidence interval = 5–12%) experiencing status epilepticus. Neurological decline was observed in 174 subjects (67%), who had a mean maximum seizure burden of 15.7% per hour, compared to 1.8% per hour for those without neurological decline (P < 0.0001). Above a maximum seizure burden threshold of 20% per hour (12 min), both the probability and magnitude of neurological decline rose sharply (P < 0.0001) across all diagnostic categories. On multivariable analysis adjusting for diagnosis and illness severity, the odds of neurological decline increased by 1.13 (95% confidence interval = 1.05–1.21, P = 0.0016) for every 1% increase in maximum hourly seizure burden. Seizure burden was not associated with mortality (odds ratio: 1.003, 95% confidence interval: 0.99–1.02, P = 0.613). We conclude that in this cohort of critically ill children, increasing seizure burden was independently associated with a greater probability and magnitude of neurological decline. Our observation that a seizure burden of more than 12 min in a given hour was strongly associated with neurological decline suggests that early antiepileptic drug management is warranted in this population, and identifies this seizure burden threshold as a potential therapeutic target. These findings support the hypothesis that electrographic seizures independently contribute to brain injury and worsen outcome. Our results motivate and inform the design of future studies to determine whether more aggressive seizure treatment can improve outcome.
Introduction
Seizures are common among critically ill children, but their potential contribution to brain injury and relationship to outcome remains unclear. Previous studies assessing continuous video-EEG monitoring among children admitted to paediatric intensive care units (ICUs) have identified electrographic seizures in as many as 46% of patients and status epilepticus in as many as 23% of patients (Jette et al., 2006; Shahwan et al., 2010; Abend et al., 2011, 2013; McCoy et al., 2011; Williams et al., 2011). Most of these seizures have no discernible clinical correlate (termed non-convulsive or subclinical seizures) and would go undetected without continuous video-EEG monitoring. Consequently, the use of continuous video-EEG monitoring among critically ill children has grown, and has become a standard of care at many North American centres (Sanchez et al., 2013). However, the high equipment and personnel costs of continuous video-EEG monitoring, in addition to continued uncertainty regarding the impact of seizures on patient outcomes, continue to limit its use at many centres.
Although there is accumulating evidence for an association between the occurrence of electrographic seizures or status epilepticus and worse short-term outcome among neonates (McBride et al., 2000), children (Lambrechtsen and Buchhalter, 2008; Kirkham et al., 2012; Topjian et al., 2013), and adults (Young et al., 1996; Shneker and Fountain, 2003; Carrera et al., 2008; Oddo et al., 2009; Claassen et al., 2013), the precise relationship between electrographic seizure burden and neurological outcome remains to be delineated. Using a large prospective cohort of critically ill children undergoing continuous video-EEG monitoring, we sought to quantify the relationship between electrographic seizure burden and short-term neurological outcome while controlling for diagnosis and illness severity. In addition, we sought to determine whether there is an electrographic seizure burden threshold above which there is an increased probability of neurological decline. Because the neurological sequelae of seizures can be subtle (Glass et al., 2009; Bellinger et al., 2011; Gaynor et al., 2013), we hypothesized that increasing seizure burden would be associated with a modest worsening (one category) in the Paediatric Cerebral Performance Category (PCPC) score at hospital discharge.
Materials and methods
Study design
We conducted a prospective observational study of all infants and children (term neonates to age 18 years) admitted to our paediatric and cardiac ICUs who underwent clinically ordered continuous video-EEG monitoring between September 2009 and September 2012. This study was approved and a waiver of informed consent granted by the hospital’s Research Ethics Board.
Our continuous video-EEG monitoring service operates 24/7 with several dedicated portable video-EEG systems (Stellate Vita ICU, Natus Medical Inc.). Before initiating continuous video-EEG monitoring, all patients are assessed by our neurology consultation service and continuous video-EEG was commenced for the following predefined indications: refractory status epilepticus, suspicion of non-convulsive seizures among encephalopathic patients (with or without concomitant muscle relaxation), or to determine whether motor or autonomic paroxysms represent seizures. When a patient meets any of these criteria, continuous video-EEG monitoring is commenced as quickly as possible. Electrodes are applied by registered EEG technologists according to the international 10–20 system and fixed with paste or collodion adhesive. The duration of continuous video-EEG monitoring is typically 24 h, longer when electrographic seizures are detected and shorter if the diagnostic question has been answered or the patient improves clinically. When seizures are identified, continuous video-EEG monitoring is continued until the patient remains seizure-free for a further 24 h. Our practice is based on evidence that 80–100% of electrographic seizures in this population are identified within the first 24 h of continuous video-EEG monitoring (Jette et al., 2006; Abend et al., 2011, 2013; McCoy et al., 2011). All EEG interpretation is performed by board-certified clinical neurophysiologists.
When seizures are identified on continuous video-EEG, the clinical team caring for the patient is informed and the neurology or epilepsy consultation services help to direct management. Our institution has clinical guidelines in place for the treatment of recurrent seizures and status epilepticus. The goal is generally to terminate seizures as quickly as possible, although treatment plans are individualized. For example, some electrographic seizures may be tolerated in patients with epilepsy who are close to their baseline seizure frequency, or when seizures are very brief and infrequent, particularly if they remain focal. The first-line anticonvulsant therapy is intravenous lorazepam, followed by intravenous fosphenytoin or phenobarbital. Refractory seizures are treated with an intravenous midazolam infusion rapidly titrated to achieve electrographic seizure freedom. Sustained refractory seizures are most commonly treated with boluses of high-dose phenobarbital or a pentobarbital infusion.
Measures
A single board-certified paediatric neurologist (E.T.P.) abstracted all clinical variables from a prospectively maintained ICU clinical database, including diagnoses, Glasgow Coma Scale scores, the PRISM III (Paediatric Risk of Mortality) score (Pollack et al., 1996) and the daily PELOD (Paediatric Logistic Organ Dysfunction) score (Leteurtre et al., 2003). Each subject was assigned to a single primary discharge diagnostic category as follows: Category 1: systemic disease; Category 2: acute seizures; Category 3: hypoxic ischaemic encephalopathy; Category 4: inflammatory or infectious process; Category 5: traumatic brain injury; Category 6: ischaemic stroke; Category 7: haemorrhagic stroke; Category 8: brain tumour or neurosurgical intervention; and Category 9: metabolic or genetic condition (including inborn errors of metabolism). To facilitate statistical analysis, the primary discharge diagnoses were subsequently grouped into systemic disease, acute seizures, and acute brain injury (a combination of diagnostic Categories 3–9). The ‘acute seizure’ group included patients who presented with new-onset seizures without an identifiable cause and patients with epilepsy who presented with a seizure exacerbation. Patients who presented with seizures secondary to an acute brain injury (e.g. traumatic brain injury, stroke, meningitis) were assigned to the ‘acute brain injury’ group.
A single board-certified clinical neurophysiologist (E.T.P.) reviewed all clinical EEG reports and the raw video-EEG recordings. If uncertainty or disagreement existed between clinical and research continuous video-EEG interpretation, a second board-certified clinical neurophysiologist (C.D.H.) also assessed the continuous video-EEG to obtain consensus. Only a patient’s first ICU admission during the study period was included, but all continuous video-EEGs performed during that admission were included for review, up to a maximum of 2 weeks of continuous video-EEG monitoring. The following EEG features were assessed: background activity including the presence of reactivity; sleep features (in the context of subject age); presence and timing of interictal and periodic epileptiform discharges; electrographic seizure burden; and whether electrographic seizures had a clinical correlate. The predominant EEG background activity during the first hour of continuous video-EEG monitoring was categorized as: normal or sedated sleep; slow and disorganized; discontinuous or burst suppression; or attenuated and featureless (Abend et al., 2013; Topjian et al., 2013). Electrographic seizures were defined according to published criteria as any rhythmic electrographic pattern lasting ≥10 s (or shorter if associated with clinical change) with a clear onset and offset, and evolution in frequency, amplitude, or morphology (Chong and Hirsch, 2005). Electrographic status epilepticus was defined as either a single seizure lasting ≥30 min or recurrent seizures totalling ≥30 min in any 1-h period (hourly seizure burden ≥ 50%) (Pisani et al., 2007; Abend et al., 2013; Topjian et al., 2013). The maximum hourly seizure burden was quantified for each subject by calculating the maximum percentage of any given hour occupied by electrographic seizures. Based on the population distribution of seizure burden, this variable was subsequently categorized as: no seizures; <20% per hour; 20–50% per hour; and >50% per hour. We also calculated each subject’s total seizure burden, representing the total amount of time occupied by electrographic seizures during continuous video-EEG monitoring.
Short-term outcome was assessed using in-hospital mortality and the difference between the PCPC score at baseline (reflecting neurological status before hospital admission) and the PCPC score at the time of hospital discharge or transfer to a rehabilitation facility. The PCPC scale is a well-validated and reliable six-point scale categorizing neurological function as: (1) normal; (2) mild disability; (3) moderate disability; (4) severe disability; (5) coma or vegetative state; and (6) death (Fiser, 1992; Fiser et al., 2000). PCPC scores were assigned by a single investigator (E.T.P.), primarily by review of the health record.
Statistical analysis
Subject characteristics were compared among seizure burden categories using Chi-square, Fisher’s exact tests and ANOVA. Univariate logistic regression was used to identify variables associated with PCPC worsening and mortality. Collinearity was assessed using Chi-square or Fisher’s exact tests for categorical variables and correlations for continuous variables. Using a purposeful model building strategy, multiple logistic regression was performed to assess the relationship between seizure burden and PCPC worsening or mortality. The final model was chosen based on the lowest Akaike information criterion (AIC) and then assessed using the Hosmer-Lemeshow goodness-of-fit test. The Pearson correlation coefficient was used to assess the relationship between maximum hourly seizure burden and total seizure burden. All statistical analyses were performed using SAS 9.3.
Results
Subject characteristics
The study population comprised 259 subjects, 132 of whom were male (51%). Subject characteristics and their association with seizure burden category are summarized in Table 1. The median age was 2.2 years [interquartile range (IQR) = 0.3 days to 9.7 years]. The median ICU length of stay was 8 days (IQR = 4–17 days), and the median length of hospital stay was 23 days (IQR = 10–47 days). Ninety per cent of subjects were ventilated, for a median duration of 7 days (IQR = 3–13 days).
Table 1.
Subject characteristics and their relationship with electrographic seizure burden
| Subject characteristic | No seizures | Maximum hourly seizure burden |
P-value | ||
|---|---|---|---|---|---|
| <20% | 20–50% | >50% | |||
| Overall totals, n, (%, 95% CI) | 166 (64, 58–70) | 42 (16, 12–21) | 28 (11, 7–15) | 23 (9, 5–12) | |
| Age, years (mean) | 6.0 | 5.5 | 1.8 | 2.7 | 0.0005 |
| Sex | |||||
| Male, n (%) | 90 (54) | 19 (45) | 11 (39) | 12 (52) | 0.42 |
| Female, n (%) | 76 (46) | 23 (55) | 17 (61) | 11 (48) | |
| PRISM III score (mean) | 9.9 | 6.2 | 11.3 | 8.9 | 0.055 |
| PELOD minimum score (mean) | 4.0 | 3.9 | 5.2 | 3.8 | 0.85 |
| Baseline PCPC score (mean) | 1.5 | 2.1 | 1.2 | 1.3 | <0.001 |
| Discharge PCPC score (mean) | 3.0 | 3.4 | 3.8 | 3.9 | 0.024 |
| Worsening in PCPC score (mean) | 1.5 | 1.3 | 2.6 | 2.6 | 0.0009 |
| Prior neurological diagnosis, n (%) | 59 (36) | 27 (64) | 5 (18) | 7 (30) | 0.0004 |
| Prior developmental delay, n (%) | 48 (29) | 21 (50) | 5 (18) | 6 (26) | 0.0189 |
| Prior history of epilepsy, n (%) | 26 (16) | 23 (55) | 3 (11) | 3 (13) | <0.0001 |
| GCS minimum score (mean) | 4.3 | 5.0 | 4.0 | 4.7 | 0.358 |
| ICU length of stay, days (mean) | 16.1 | 16.9 | 35.4 | 22.0 | 0.029 |
| Clinical seizures evident in acute presentation, n (%) | 78 (47) | 41 (98) | 24 (86) | 22 (96) | <0.0001 |
| Unreactive EEG background, n (%) | 36 (22) | 9 (21) | 8 (29) | 9 (39) | 0.272 |
| EEG background category (1st h), n (%) | |||||
| Normal or sedated sleep | 29 (18) | 5 (12) | 1 (4) | 0 (0) | 0.0912 |
| Slow and disorganized | 95 (57) | 30 (71) | 16 (57) | 15 (65) | |
| Discontinuous or burst suppression | 31 (19) | 4 (10) | 9 (32) | 6 (26) | |
| Attenuated and featureless | 11 (7) | 3 (7) | 2 (7) | 2 (9) | |
| Primary discharge diagnosis, n (%) | |||||
| Systemic disease | 39 (23) | 2 (5) | 1 (4) | 0 (0) | <0.0001 |
| Acute seizures | 33 (20) | 23 (55) | 5 (18) | 5 (22) | |
| Acute brain injury | 94 (57) | 17 (40) | 22 (79) | 18 (78) | |
| Hypoxic ischaemic encephalopathy | 35 (21) | 1 (2) | 10 (36) | 4 (17) | |
| Inflammation or infection | 16 (10) | 5 (12) | 4 (14) | 5 (22) | |
| Traumatic brain injury | 6 (4) | 3 (7) | 3 (11) | 3 (13) | |
| Ischaemic stroke | 11 (7) | 3 (7) | 2 (7) | 3 (13) | |
| Haemorrhagic stroke | 13 (8) | 2 (5) | 3 (11) | 1 (4) | |
| Neurosurgical or tumour | 5 (3) | 1 (2) | 0 (0) | 1 (4) | |
| Metabolic or genetic | 8 (5) | 2 (5) | 0 (0) | 1 (4) | |
Note: Acute brain injury subcategories were collapsed for statistical analysis.
GCS = Glasgow Coma Scale.
The median duration of continuous video-EEG monitoring was 37 h (IQR = 21–56 h). The continuous video-EEG monitoring duration was longer among subjects with electrographic seizures (median = 56 h, IQR = 36–90 h) than subjects without electrographic seizures (median = 24 h, IQR = 19–43 h). The most common indication for continuous video-EEG monitoring was to assess for electrographic seizures in an encephalopathic patient (77%, n = 200). Other indications included titration of antiepileptic drugs in patients with refractory status epilepticus (16%, n = 41), characterization of clinical paroxysmal events (24%, n = 63), and concomitant neuromuscular blockade (15%, n = 38). Many subjects had more than one indication for continuous video-EEG monitoring (44%, n = 113). Clinical seizures were evident as part of the acute presentation (before continuous video-EEG monitoring) in 166 subjects (64%), and 55 (21%) had a previous diagnosis of epilepsy.
Electrographic seizures occurred in 93 subjects [36%, 95% confidence interval (CI) = 30–42%], 29 of whom had a prior diagnosis of epilepsy (Table 1). Among subjects with electrographic seizures, 36 (39%) had entirely non-convulsive seizures, 44 (47%) had both non-convulsive and convulsive seizures, and 13 (14%) had entirely convulsive seizures. Electrographic status epilepticus occurred in 23 (9%) subjects, all of whom experienced some non-convulsive seizures and nine of whom experienced exclusively non-convulsive seizures. Among patients with seizures, the median time to recording their first seizure was 32 min (IQR = 6.5–294 min). Interictal epileptiform discharges were present in 110 subjects (42%) and the median time until their first appearance on continuous video-EEG was 18 s (IQR = 6–60 s). Periodic epileptiform discharges were identified in 33 subjects (13%).
On univariate analysis (Table 1), a higher seizure burden was observed among subjects with younger age (P = 0.0005), a larger PCPC worsening at hospital discharge (P = 0.0009), a longer ICU length of stay (P = 0.029), the presence of clinical seizures in the acute presentation (P < 0.0001), and a discharge diagnosis of acute brain injury (P < 0.0001). Subjects with previous neurological diagnoses, developmental delay or a history of epilepsy were most likely to have a maximum seizure burden <20% per hour. Illness severity, measured by the PRISM and PELOD scores, did not differ among seizure burden categories.
The majority of subjects received treatment with benzodiazepines or other antiepileptic drugs prior to or during continuous video-EEG monitoring (81%, n = 211). Sixty-nine subjects (27%) received one antiepileptic drug (fosphenytoin, phenobarbital, or midazolam), 60 subjects (23%) received two antiepileptic drugs, and 82 subjects (31.7%) received three or more antiepileptic drugs.
Neurological decline
Short-term neurological decline, evidenced by a worsening between PCPC score at baseline (pre-admission neurological function) and hospital discharge, was observed in 67% of subjects (n = 174), who had a mean maximum seizure burden of 15.7% per hour, compared to 1.8% per hour for those without PCPC worsening (P < 0.0001). The median PCPC score at admission was 1 (IQR = 1–1) among the entire cohort, and 3 (IQR = 2–3) among the 55 patients with a previous diagnosis of epilepsy. The pre-admission PCPC was normal for 171 (66%) subjects, mild disability for 43 (16.6%) subjects, moderate disability for 30 (11.6%) subjects, and severe disability for 15 (5.8%) subjects. There were no subjects in a vegetative state or coma before admission.
No subjects improved from their baseline PCPC score. Factors associated with neurological decline on univariate and multivariable analyses are presented in Table 2. On multivariable analysis, the odds of neurological decline were higher among subjects with a greater seizure burden [odds ratio (OR) = 1.13 for each 1% increase in maximum hourly seizure burden, 95% CI = 1.05–1.21], an unreactive EEG background (OR = 6.70, 95% CI = 1.9–23.9), clinical seizures in the acute presentation (OR = 3.79, 95% CI = 1.15–12.5), and a discharge diagnosis of acute brain injury (OR = 14.1, 95% CI = 4.8–42). The odds of neurological decline were lower among subjects with a prior history of epilepsy (OR = 0.06, 95% CI = 0.02–0.20) and a lower minimum Glasgow Coma Scale score (OR = 0.76, 95% CI = 0.64–0.98). Higher PRISM and PELOD scores, although associated with greater odds of neurological decline on univariate analysis, did not remain in the multivariable model.
Table 2.
Factors associated with neurological decline
| PCPC |
Univariate analysis |
Multivariable analysis |
||||
|---|---|---|---|---|---|---|
| Subject Characteristic | Worsening (n = 174) | No worsening (n = 85) | Odds ratio (95% CI) | P-value | Odds ratio (95% CI) | P-value |
| Age, years (mean) | 5.0 | 5.5 | 0.985 (0.942−1.03) | 0.521 | n/a | n/a |
| Sex, n (%) | ||||||
| Male | 88 (51) | 44 (52) | Ref | n/a | n/a | |
| Female | 86 (49) | 41 (48) | 1.05 (0.624−1.76) | 0.857 | ||
| PRISM III score (mean) | 11.0 | 6.0 | 1.09 (1.05−1.14) | <0.0001 | n/a | n/a |
| PELOD minimum score (mean) | 5.0 | 2.3 | 1.08 (1.02−1.13) | 0.0050 | n/a | n/a |
| Prior neurological diagnosis, n (%) | 41 (24) | 57 (67) | 0.151 (0.085−0.268) | <0.0001 | n/a | n/a |
| Prior developmental delay, n (%) | 32 (18) | 48 (56) | 0.174 (0.098−0.309) | <0.0001 | n/a | n/a |
| Prior history of epilepsy, n (%) | 15 (9) | 40 (47) | 0.106 (0.054−0.209) | <0.0001 | 0.06 (0.02−0.20) | <0.0001 |
| Minimum GCS during ICU admission (mean) | 3.8 | 5.7 | 0.795 (0.718−0.879) | <0.0001 | 0.76 (0.64−0.89) | 0.001 |
| ICU length of stay, days (mean) | 22.6 | 11.2 | 1.02 (1.00−1.04) | 0.0166 | n/a | n/a |
| Clinical seizures in acute presentation, n (%) | 119 (68) | 46 (54) | 1.83 (1.08−3.13) | 0.0257 | 3.79 (1.15−12.5) | 0.029 |
| Unreactive EEG background, n (%) | 56 (32) | 6 (7) | 6.25 (2.57−15.2) | <0.0001 | 6.70 (1.9−23.9) | 0.0034 |
| EEG background category (1st h), n (%) | 0.0001 | |||||
| Normal or sedated sleep | 11 (6) | 24 (28) | Ref | Ref | n/a | n/a |
| Slow and disorganized | 108 (62) | 48 (57) | 4.91 (2.23−10.8) | <0.0001 | ||
| Discontinuous or burst suppression | 37 (21) | 13 (15) | 6.21 (2.3−16.1) | 0.0002 | ||
| Attenuated and featureless | 18 (10) | 0 (0) | − | − | ||
| Maximum hourly seizure burden (mean) | 15.7 | 1.8 | 1.073 (1.033–1.114) | 0.0003 | 1.13 (1.05−1.21) | 0.0016 |
| Primary discharge diagnostic category | <0.0001 | |||||
| Systemic disease | 11 (6) | 31 (37) | Ref | Ref | Ref | Ref |
| Acute seizures | 26 (15) | 40 (47) | 1.83 (0.786−4.27) | 0.161 | 1.12 (0.26−4.9) | 0.88 |
| Acute brain injury | 137 (79) | 14 (16) | 27.6 (11.4−66.5) | <0.0001 | 14.1 (4.8−42) | <0.0001 |
A high score on both the PRISM III and PELOD indicates an elevated illness severity.
Ref = reference group; n/a = not included in the final reduced multivariable model; GCS = Glasgow Coma Scale.
Seizure burden and neurological decline
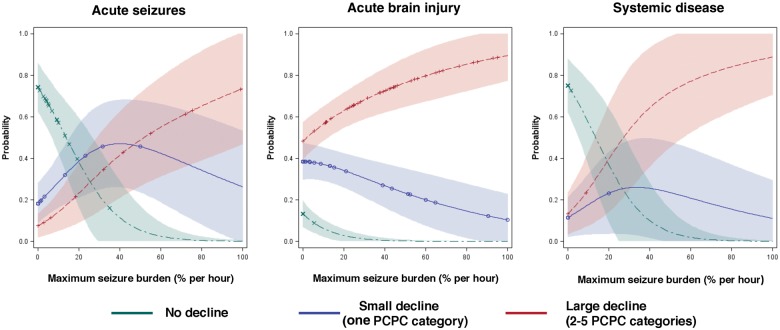
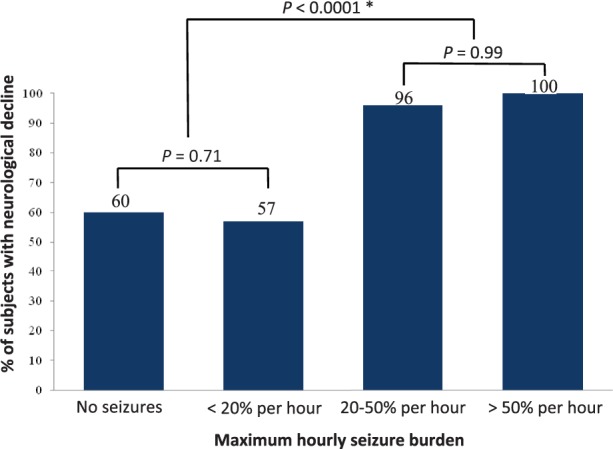
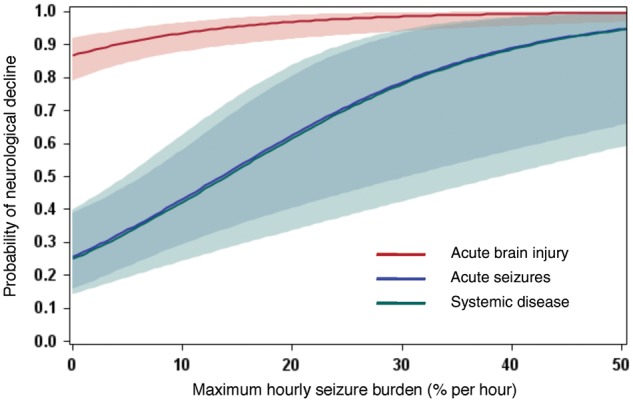
The probability of neurological decline rose with increasing seizure burden. Examining the distribution of neurological decline by seizure burden, we identified a seizure burden threshold at 20% per hour (12 min), above which the probability of neurological decline rose sharply (P < 0.0001) (Fig. 1). Subjects with a maximum hourly seizure burden below this threshold had the same probability of neurological decline as subjects without seizures (P = 0.71). This association between seizure burden and neurological decline was observed across all diagnostic categories, but was most evident for subjects with acute seizures and systemic disease (Fig. 2), as subjects with acute brain injury had a high baseline probability of neurological decline. The predicted odds of neurological decline associated with increasing levels of seizure burden are illustrated in Table 3.
Figure 1.
Maximum hourly seizure burden of 20% (12 min) is associated with neurological decline.Comparisons performed using Fisher’s exact test. The single subject with a seizure burden ≥20% per hour who did not experience neurological decline had a baseline PCPC score of 3. *Comparison of the ‘no seizures’ and ‘<20% per hour’ groups combined with the ‘≥20% per hour’ and ‘>50% per hour’ groups combined.
Figure 2.
Probability of neurological decline rises with increasing seizure burden across all diagnostic categories. Prediction plot is based on the unadjusted multivariable model presented in Table 2, stratified by diagnostic category. The shaded areas represent the 95% confidence intervals.
Table 3.
Predicted odds of neurological decline with increasing seizure burden
| Increase in maximum hourly seizure burden | Odds ratio for PCPC worsening (95% CI) |
|---|---|
| 1% | 1.13 (1.05–1.21) |
| 5% | 1.82 (1.25–2.63) |
| 10% | 3.29 (1.57–6.89) |
| 20% | 10.8 (2.48–47.5) |
| 30% | 35.7 (3.90–327.6) |
| 50% | 387.4 (9.64–>999.9) |
Adjusted for diagnosis, illness severity and other clinical factors (see Table 2).
For every 1% increase in electrographic seizure burden, the probability of PCPC worsening from baseline increases by 1.13-fold.
Seizure burden and the magnitude of neurological decline
The magnitude of neurological decline also rose with increasing seizure burden. This relationship becomes evident when dichotomizing subjects according to the observed 20% maximum hourly seizure burden threshold (Table 4 and Fig. 3). Subjects in the high seizure burden group were more likely to experience greater PCPC worsening, compared to subjects in the low or no seizure burden group (P < 0.0001). This relationship was observed across all diagnostic categories (Fig. 4).
Table 4.
Relationship between maximum hourly seizure burden and the magnitude of PCPC worsening
| Magnitude of PCPC worsening | Subjects stratified by maximum hourly seizure burden, n (%) |
|
|---|---|---|
| <20% per hour (n = 208) | ≥20% per hour (n = 51) | |
| Zero categories | 84 (40) | 1 (2) |
| One category | 60 (29) | 13 (25) |
| Two categories | 14 (7) | 16 (31) |
| Three categories | 13 (6) | 8 (16) |
| Four categories | 6 (3) | 3 (6) |
| Five categories | 31 (15) | 10 (20) |
Note: Patients who dropped five categories died (i.e. from 1 = normal, to 6 = death).
Figure 3.
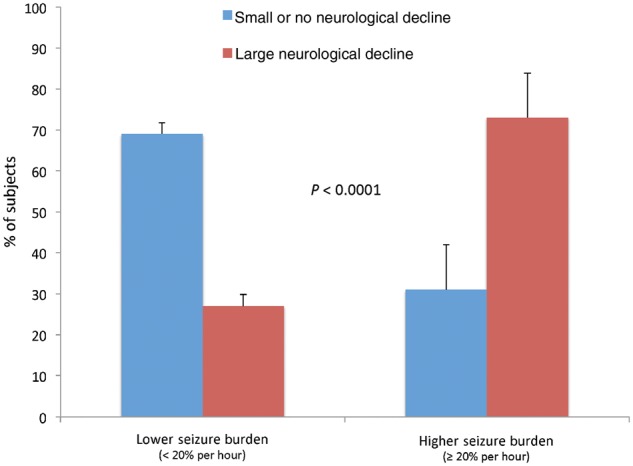
Higher seizure burden is associated with a greater magnitude of neurological decline. Small or no neurological decline is defined as ≤1 category increase in PCPC score; large neurological decline is defined as ≥2 category increase in PCPC score. Comparison performed using Fisher’s exact test.
Figure 4.
Magnitude of neurological decline rises with increasing seizure burden across all diagnostic categories. The magnitude of neurological decline was categorized as no decline, small decline (a worsening by one PCPC category), and large decline (a worsening by two or more PCPC categories). Multinomial logistic regression with a generalized logit model was fitted and prediction plots were generated to illustrate the probability of neurological decline by seizure burden among the three primary diagnostic categories. The shaded areas represent the 95% confidence intervals. Across all diagnostic categories, as seizure burden increased, the probability of a large decline rose and the probability of no decline fell. The probability of a small decline peaked with moderate seizure burden (30–35% per hour), except among subjects with acute brain injury, where it declined monotonically.
Mortality
Fifty-four subjects (21%) died during their hospital stay. Electrographic seizure burden was not associated with mortality (P = 0.99). Mortality among subjects without seizures was 20%. Mortality among subjects with seizures was distributed as follows: maximum seizure burden <20% per hour = 19% mortality; seizure burden 20–50% per hour = 25% mortality; seizure burden >50% per hour = 22% mortality. On multivariable analysis (Supplementary Table 1), the odds of mortality were higher among subjects with an unreactive EEG background (OR = 7.40, 95% CI = 3.08–17.8), a higher PRISM score (OR = 1.13, 95% CI = 1.02–1.19), a higher minimum PELOD score (OR = 1.20, 95% CI = 1.12–1.29), and a longer ICU length of stay (OR = 1.013, 95% CI = 1.002–1.023).
Discussion
In this large prospective cohort of critically ill children who underwent clinically indicated continuous video-EEG monitoring, we have demonstrated that increasing seizure burden was independently associated with neurological decline at hospital discharge, even after adjusting for diagnosis and illness severity. We identified a maximum seizure burden threshold of 20% per hour (12 min), above which the probability of neurological decline rose sharply. Furthermore, as seizure burden increased, we observed concomitantly greater decline in neurological function.
Seizures were common in this cohort. We observed electrographic seizures in 36% and electrographic status epilepticus in 9% of subjects, which is comparable with the prevalence reported in other cohorts of critically ill children undergoing clinically-indicated continuous video-EEG monitoring (Jette et al., 2006; Abend et al., 2011, 2013; McCoy et al., 2011; Williams et al., 2011). Among subjects who experienced seizures, 86% experienced some subclinical seizures (those without any discernible clinical correlate) and 39% experienced entirely subclinical seizures. Furthermore, among subjects with status epilepticus, 100% had some subclinical seizures and 39% experienced exclusively subclinical seizures. These findings confirm that accurate assessment of seizure burden in this population requires continuous video-EEG monitoring.
Critically ill children known to be at higher risk for electrographic seizures include younger patients, those with a previous diagnosis of epilepsy, those who present with clinical seizures before continuous video-EEG monitoring, and those diagnosed with an acute brain injury (Jette et al., 2006; Abend et al., 2011, 2013; McCoy et al., 2011). Furthermore, the presence of an abnormal EEG background, interictal epileptiform discharges, and periodic epileptiform discharges are also predictive of seizures (Jette et al., 2006; McCoy et al., 2011; Abend et al., 2013; Topjian et al., 2013). We found that these same clinical and EEG factors were associated with greater electrographic seizure burden (Table 1). After electrographic seizures were identified, our practice was to continue continuous video-EEG monitoring for at least 24 h of seizure-freedom. Given our understanding of the temporal evolution of seizures in critically ill children (Jette et al., 2006; Abend et al., 2011, 2013; McCoy et al., 2011), it is unlikely that we missed a significant burden of electrographic seizures after the continuous video-EEG was discontinued. Furthermore, although we may have missed some electrographic seizures occurring before the commencement of continuous video-EEG monitoring in some subjects, these subjects would have likely continued to experience seizures during continuous video-EEG monitoring, still permitting us to obtain an estimate of their maximum hourly seizure burden.
The existence of an independent causal link between seizures and neurological outcome among critically ill patients remains controversial. Outcomes following acute seizures or status epilepticus are known to be heavily influenced by the underlying cause of the seizures. Indeed, in our cohort, the presence of an acute brain injury was the strongest predictor of neurological decline. Numerous observational studies in neonates (Miller et al., 2002; Glass et al., 2009), children (Tsuchida et al., 2007; Kirkham et al., 2012; Topjian et al., 2013), and adults (Young et al., 1996; Shneker and Fountain, 2003; Vespa et al., 2007, 2010; Carrera et al., 2008; Oddo et al., 2009; Claassen et al., 2013), have demonstrated immediate pathophysiological changes accompanying seizures and reported worse neurological outcomes. Despite attempts by these studies to control for the severity of underlying brain injury, some critics maintain that seizures in these patients simply represented a biomarker of brain injury, rather than an independent contributor to brain injury.
Plausible mechanisms for seizure-induced brain injury have been identified in experimental animals. Rodent and non-human primate models of acute symptomatic seizures that were able to control for injury severity have demonstrated that seizures can independently contribute to brain injury (Holmes, 2009), even in the absence of convulsive activity (Meldrum et al., 1973). The developing brain appears particularly vulnerable to seizure-induced injury (Sankar et al., 1998; Holmes, 2009), which can include morphological changes to hippocampal neurons (Sankar et al., 2000), impaired neurogenesis (McCabe et al., 2001), alterations in glutaminergic synaptic plasticity and long-term functional impairment (Holmes et al., 1998; Cornejo et al., 2007). Prolonged seizures can activate inflammatory cascades and create a state of ‘functional ischaemia’ when the metabolic demands of seizures exceed supply (Lothman, 1990; Yager et al., 2002; Chen and Wasterlain, 2006). Attenuating seizure-induced inflammation is neuroprotective (Serrano et al., 2011; Ma et al., 2012; Jiang et al., 2013).
Our findings support the hypothesis that seizures independently contribute to brain injury in this population. We observed a robust association between increasing seizure burden and both the probability and magnitude of neurological decline at hospital discharge, even after controlling for diagnosis and illness severity. Our study extends previous work on this topic by quantifying the relationship between seizure burden and outcome. Seizure burden may be measured in several ways, for example total number of seizures, mean number of seizures per hour, longest seizure duration, mean seizure duration, total seizure burden, or ictal fraction (the proportion of EEG recording spent in seizures) (McBride et al., 2000; Pisani et al., 2008). We quantified seizure burden by calculating the maximum percentage of any given hour occupied by electrographic seizures, which we termed the maximum hourly seizure burden. We chose this metric because of its practical use for real-time patient management and relevance to current definitions of electrographic status epilepticus, which include an electrographic seizure burden ≥50% per hour (30 min) (Topjian et al., 2013). Furthermore, maximum hourly seizure burden was highly correlated (R = 0.79) with total seizure burden.
We observed that above a seizure burden threshold of 20% per hour (12 min), short-term neurological decline occurred in 98% of subjects. In fact, subjects with a seizure burden of 20−50% per hour had the same risk of decline as those with electrographic status epilepticus (seizure burden >50% per hour), whereas subjects with a seizure burden <20% per hour had the same risk of neurological decline as those who did not experience any seizures (Fig. 1). These findings suggest that early and aggressive treatment of electrographic seizures in this population is warranted, and support the ‘operational’ 5-min definition of status epilepticus proposed in recent treatment guidelines (Brophy et al., 2012). Although it remains to be shown that earlier or more aggressive treatment can successfully reduce seizure burden and improve outcomes, our identification of this 12-min threshold effect of seizure burden on outcome represents a therapeutic target that can help inform the design of future interventional studies.
After adjusting for diagnosis, illness severity and other factors, we found that for every 1% increase in maximum hourly seizure burden the odds of neurological decline (measured by worsening in PCPC score) increased by 1.13 (Table 3). The influence of seizure burden on the probability of neurological decline was greater for subjects with acute seizures and systemic disease than for those with acute brain injury, who had a higher baseline probability of neurological decline (Fig. 2). Consistent with previous studies in children, a diagnosis of acute brain injury, an unreactive EEG background, and a past history of epilepsy were the factors that had the largest modulating effect on the relationship between seizure burden and outcome (Kirkham et al., 2012; Topjian et al., 2013). While an acute brain injury and an unreactive EEG were associated with higher odds of neurological decline, a previous diagnosis of epilepsy was associated with lower odds of neurological decline. This likely reflects the fact that subjects with epilepsy had less chance of PCPC worsening because they presented with higher baseline PCPC scores (median = 3) than subjects without epilepsy (median = 1), whereas at hospital discharge the median PCPC score was 3 for both groups. Moreover, subjects with a history of epilepsy were most likely to have a maximum seizure burden <20% per hour.
We hypothesized that with elevated seizure burden we would observe only a small worsening (one category) in PCPC scores because prior long-term outcome studies evaluating the effects of seizures among neonates with birth asphyxia (Glass et al., 2009) and infants who underwent corrective surgery for complex cardiac lesions (Bellinger et al., 2011; Gaynor et al., 2013) found cognitive and neurodevelopmental sequelae that were quite subtle. Surprisingly, we found that subjects with a higher seizure burden had a greater magnitude of neurological decline (Fig. 3 and Table 4), even after stratifying by diagnostic category (Fig. 4), further strengthening the case for a causal link between seizures and outcome (Hill, 1965).
We did not find an association between increasing seizure burden and mortality, in contrast to a recent report that electrographic status epilepticus was associated with mortality (Topjian et al., 2013). Although we did not hypothesize an association between seizure burden and mortality, certain characteristics of our study population may have reduced our ability to detect such an association, namely the higher acuity of illness (higher proportion requiring ventilation, longer duration of ICU stay and hospital stay), and lower incidence of status epilepticus (9%) compared to the population studied by Topjian et al. (2013) (21.5%).
Our study has limitations. First, our outcome assessment only reflects each subject’s neurological function at the time of hospital discharge, and may not reflect longer-term outcomes. Neurological status likely continues to evolve following hospital discharge; therefore longer-term outcome studies will be required to substantiate these findings. Second, although the PCPC scale is a validated measure of neurological impairment following critical illness, this tool cannot assess more subtle but important outcomes such as memory, attention and behaviour (Glass et al., 2009; Bellinger et al., 2011; Gaynor et al., 2013). However, given our finding of significant impairment using this crude measure, studies using detailed neuropsychological evaluations are clearly warranted. Third, our study was not designed to measure the effect of antiepileptic drug treatment on seizure burden; therefore we could not determine whether treatment success was associated with better short-term outcome. Our study population represents a treated cohort: 81% of subjects received antiepileptic drugs before or during continuous video-EEG monitoring and 37% received at least three antiepileptic drugs. The association between seizure burden and neurological impairment occurred despite these interventions, but it remains unclear whether early and more aggressive treatment could have further reduced the seizure burden or improved outcomes. Studies carefully assessing the relationship between seizure burden, timeliness of treatment, treatment efficacy, and outcomes are required.
The present findings add to a growing body of literature supporting the hypothesis that seizures among critically ill children are not only a biomarker of brain injury but also an independent contributor to brain injury. Our observation of a dose effect between seizure burden and neurological decline strengthens the case for a causal link between seizures, secondary brain injury and worse neurological outcome (Hill, 1965). However, conclusive proof of this causal link will require a randomized controlled trial of antiepileptic drug therapy in a cohort of patients at high risk for electrographic seizures that includes longer-term measures of both functional and neuropsychological outcome. The results of the present study can serve to inform the design of such a trial. In the interim, our observation that a seizure burden of >12 min in a given hour was strongly associated with short-term neurological decline suggests that early antiepileptic drug management is warranted in this population, and identifies this seizure burden threshold as a potential therapeutic target.
Supplementary Material
Acknowledgements
We thank Dr Steven Miller for his critical appraisal of the manuscript, and our epilepsy fellows, attending physicians, and EEG technologists for their ongoing dedication to continuous EEG monitoring and support of this project.
Glossary
Abbreviations
- PCPC
Paediatric Cerebral Performance Category
- PELOD
Paediatric Logistic Organ Dysfunction Score
- PRISM
Paediatric Risk of Mortality Score
Funding
This work was supported by a New Investigator Research Grant from The Hospital for Sick Children Foundation and the Canadian Institutes of Health Research (NI10-021), and a Health Research Grant from the Physicians' Services Incorporated Foundation (09-40). Dr Payne receives fellowship training support from Alberta Innovates Health Solutions and the Canadian League Against Epilepsy. Dr Hahn receives research support from the Canadian Institutes of Health Research, The Hospital for Sick Children Foundation and The Physicians’ Services Incorporated Foundation. Dr Hutchison receives research support from the National Institutes of Health, The Hospital for Sick Children Foundation, the Canada Foundation for Innovation, the Canadian Institutes of Health Research, the Heart and Stroke Foundation of Canada, the Ontario Neurotrauma Foundation, the Physicians’ Services Incorporated Foundation, and the Victoria Neurotrauma Initiative.
Supplementary material
Supplementary material is available at Brain online.
References
- Abend NS, Arndt DH, Carpenter JL, Chapman KE, Cornett KM, Gallentine WB, et al. Electrographic seizures in pediatric ICU patients: cohort study of risk factors and mortality. Neurology. 2013;81:383–91. doi: 10.1212/WNL.0b013e31829c5cfe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abend NS, Gutierrez-Colina AM, Topjian AA, Zhao H, Guo R, Donnelly M, et al. Nonconvulsive seizures are common in critically ill children. Neurology. 2011;76:1071–7. doi: 10.1212/WNL.0b013e318211c19e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellinger DC, Wypij D, Rivkin MJ, DeMaso DR, Robertson RL, Jr, Dunbar-Masterson C, et al. Adolescents with d-transposition of the great arteries corrected with the arterial switch procedure: neuropsychological assessment and structural brain imaging. Circulation. 2011;124:1361–9. doi: 10.1161/CIRCULATIONAHA.111.026963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brophy GM, Bell R, Claassen J, Alldredge B, Bleck TP, Glauser T, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17:3–23. doi: 10.1007/s12028-012-9695-z. [DOI] [PubMed] [Google Scholar]
- Carrera E, Claassen J, Oddo M, Emerson RG, Mayer SA, Hirsch LJ. Continuous electroencephalographic monitoring in critically ill patients with central nervous system infections. Arch Neurol. 2008;65:1612–8. doi: 10.1001/archneur.65.12.1612. [DOI] [PubMed] [Google Scholar]
- Chen JW, Wasterlain CG. Status epilepticus: pathophysiology and management in adults. Lancet Neurol. 2006;5:246–56. doi: 10.1016/S1474-4422(06)70374-X. [DOI] [PubMed] [Google Scholar]
- Chong DJ, Hirsch LJ. Which EEG patterns warrant treatment in the critically ill? Reviewing the evidence for treatment of periodic epileptiform discharges and related patterns. J Clin Neurophysiol. 2005;22:79–91. doi: 10.1097/01.wnp.0000158699.78529.af. [DOI] [PubMed] [Google Scholar]
- Claassen J, Perotte A, Albers D, Kleinberg S, Schmidt JM, Tu B, et al. Nonconvulsive seizures after subarachnoid hemorrhage: Multimodal detection and outcomes. Ann Neurol. 2013;74:53–64. doi: 10.1002/ana.23859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornejo BJ, Mesches MH, Coultrap S, Browning MD, Benke TA. A single episode of neonatal seizures permanently alters glutamatergic synapses. Ann Neurol. 2007;61:411–26. doi: 10.1002/ana.21071. [DOI] [PubMed] [Google Scholar]
- Fiser DH. Assessing the outcome of pediatric intensive care. J Pediatr. 1992;121:68–74. doi: 10.1016/s0022-3476(05)82544-2. [DOI] [PubMed] [Google Scholar]
- Fiser DH, Tilford JM, Roberson PK. Relationship of illness severity and length of stay to functional outcomes in the pediatric intensive care unit: a multi-institutional study. Crit Care Med. 2000;28:1173–9. doi: 10.1097/00003246-200004000-00043. [DOI] [PubMed] [Google Scholar]
- Gaynor JW, Jarvik GP, Gerdes M, Kim DS, Rajagopalan R, Bernbaum J, et al. Postoperative electroencephalographic seizures are associated with deficits in executive function and social behaviors at 4 years of age following cardiac surgery in infancy. J Thorac Cardiovasc Surg. 2013;146:132–9. doi: 10.1016/j.jtcvs.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass HC, Glidden D, Jeremy RJ, Barkovich AJ, Ferriero DM, Miller SP. Clinical neonatal seizures are independently associated with outcome in infants at risk for hypoxic-ischemic brain injury. J Pediatr. 2009;155:318–23. doi: 10.1016/j.jpeds.2009.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill AB. The environment and disease: association or causation? Proc R Soc Med. 1965;58:295–300. [PMC free article] [PubMed] [Google Scholar]
- Holmes GL. The long-term effects of neonatal seizures. Clin Perinatol. 2009;36:901–14, vii–viii. doi: 10.1016/j.clp.2009.07.012. [DOI] [PubMed] [Google Scholar]
- Holmes GL, Gairsa JL, Chevassus-Au-Louis N, Ben-Ari Y. Consequences of neonatal seizures in the rat: morphological and behavioral effects. Ann Neurol. 1998;44:845–57. doi: 10.1002/ana.410440602. [DOI] [PubMed] [Google Scholar]
- Jette N, Claassen J, Emerson RG, Hirsch LJ. Frequency and predictors of nonconvulsive seizures during continuous electroencephalographic monitoring in critically ill children. Arch Neurol. 2006;63:1750–5. doi: 10.1001/archneur.63.12.1750. [DOI] [PubMed] [Google Scholar]
- Jiang J, Quan Y, Ganesh T, Pouliot WA, Dudek FE, Dingledine R. Inhibition of the prostaglandin receptor EP2 following status epilepticus reduces delayed mortality and brain inflammation. Proc Natl Acad Sci USA. 2013;110:3591–6. doi: 10.1073/pnas.1218498110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkham FJ, Wade AM, McElduff F, Boyd SG, Tasker RC, Edwards M, et al. Seizures in 204 comatose children: incidence and outcome. Intensive Care Med. 2012;38:853–62. doi: 10.1007/s00134-012-2529-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambrechtsen FA, Buchhalter JR. Aborted and refractory status epilepticus in children: a comparative analysis. Epilepsia. 2008;49:615–25. doi: 10.1111/j.1528-1167.2007.01465.x. [DOI] [PubMed] [Google Scholar]
- Leteurtre S, Martinot A, Duhamel A, Proulx F, Grandbastien B, Cotting J, et al. Validation of the paediatric logistic organ dysfunction (PELOD) score: prospective, observational, multicentre study. Lancet. 2003;362:192–7. doi: 10.1016/S0140-6736(03)13908-6. [DOI] [PubMed] [Google Scholar]
- Lothman E. The biochemical basis and pathophysiology of status epilepticus. Neurology. 1990;40(Suppl 2):13–23. [PubMed] [Google Scholar]
- Ma L, Cui XL, Wang Y, Li XW, Yang F, Wei D, et al. Aspirin attenuates spontaneous recurrent seizures and inhibits hippocampal neuronal loss, mossy fiber sprouting and aberrant neurogenesis following pilocarpine-induced status epilepticus in rats. Brain Res. 2012;1469:103–13. doi: 10.1016/j.brainres.2012.05.058. [DOI] [PubMed] [Google Scholar]
- McBride MC, Laroia N, Guillet R. Electrographic seizures in neonates correlate with poor neurodevelopmental outcome. Neurology. 2000;55:506–13. doi: 10.1212/wnl.55.4.506. [DOI] [PubMed] [Google Scholar]
- McCabe BK, Silveira DC, Cilio MR, Cha BH, Liu X, Sogawa Y, et al. Reduced neurogenesis after neonatal seizures. J Neurosci. 2001;21:2094–103. doi: 10.1523/JNEUROSCI.21-06-02094.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCoy B, Sharma R, Ochi A, Go C, Otsubo H, Hutchison JS, et al. Predictors of nonconvulsive seizures among critically ill children. Epilepsia. 2011;52:1973–8. doi: 10.1111/j.1528-1167.2011.03291.x. [DOI] [PubMed] [Google Scholar]
- Meldrum BS, Vigouroux RA, Brierley JB. Systemic factors and epileptic brain damage. Prolonged seizures in paralyzed, artificially ventilated baboons. Arch Neurol. 1973;29:82–7. doi: 10.1001/archneur.1973.00490260026003. [DOI] [PubMed] [Google Scholar]
- Miller SP, Weiss J, Barnwell A, Ferriero DM, Latal-Hajnal B, Ferrer-Rogers A, et al. Seizure-associated brain injury in term newborns with perinatal asphyxia. Neurology. 2002;58:542–8. doi: 10.1212/wnl.58.4.542. [DOI] [PubMed] [Google Scholar]
- Oddo M, Carrera E, Claassen J, Mayer SA, Hirsch LJ. Continuous electroencephalography in the medical intensive care unit. Crit Care Med. 2009;37:2051–6. doi: 10.1097/CCM.0b013e3181a00604. [DOI] [PubMed] [Google Scholar]
- Pisani F, Cerminara C, Fusco C, Sisti L. Neonatal status epilepticus vs recurrent neonatal seizures: clinical findings and outcome. Neurology. 2007;69:2177–85. doi: 10.1212/01.wnl.0000295674.34193.9e. [DOI] [PubMed] [Google Scholar]
- Pisani F, Copioli C, Di Gioia C, Turco E, Sisti L. Neonatal seizures: relation of ictal video-electroencephalography (EEG) findings with neurodevelopmental outcome. J Child Neurol. 2008;23:394–8. doi: 10.1177/0883073807309253. [DOI] [PubMed] [Google Scholar]
- Pollack MM, Patel KM, Ruttimann UE. PRISM III: an updated pediatric risk of mortality score. Crit Care Med. 1996;24:743–52. doi: 10.1097/00003246-199605000-00004. [DOI] [PubMed] [Google Scholar]
- Sanchez SM, Carpenter J, Chapman KE, Dlugos DJ, Gallentine WB, Giza CC, et al. Pediatric ICU EEG monitoring: current resources and practice in the United States and Canada. J Clin Neurophysiol. 2013;30:156–60. doi: 10.1097/WNP.0b013e31827eda27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sankar R, Shin DH, Liu H, Mazarati A, Pereira de Vasconcelos A, Wasterlain CG. Patterns of status epilepticus-induced neuronal injury during development and long-term consequences. J Neurosci. 1998;18:8382–93. doi: 10.1523/JNEUROSCI.18-20-08382.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sankar R, Shin D, Mazarati AM, Liu H, Katsumori H, Lezama R, et al. Epileptogenesis after status epilepticus reflects age- and model-dependent plasticity. Ann Neurol. 2000;48:580–9. [PubMed] [Google Scholar]
- Serrano GE, Lelutiu N, Rojas A, Cochi S, Shaw R, Makinson CD, et al. Ablation of cyclooxygenase-2 in forebrain neurons is neuroprotective and dampens brain inflammation after status epilepticus. J Neurosci. 2011;31:14850–60. doi: 10.1523/JNEUROSCI.3922-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahwan A, Bailey C, Shekerdemian L, Harvey AS. The prevalence of seizures in comatose children in the pediatric intensive care unit: a prospective video-EEG study. Epilepsia. 2010;51:1198–204. doi: 10.1111/j.1528-1167.2009.02517.x. [DOI] [PubMed] [Google Scholar]
- Shneker BF, Fountain NB. Assessment of acute morbidity and mortality in nonconvulsive status epilepticus. Neurology. 2003;61:1066–73. doi: 10.1212/01.wnl.0000082653.40257.0b. [DOI] [PubMed] [Google Scholar]
- Topjian AA, Gutierrez-Colina AM, Sanchez SM, Berg RA, Friess SH, Dlugos DJ, et al. Electrographic status epilepticus is associated with mortality and worse short-term outcome in critically ill children. Crit Care Med. 2013;41:215–23. doi: 10.1097/CCM.0b013e3182668035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuchida TN, Barkovich AJ, Bollen AW, Hart AP, Ferriero DM. Childhood status epilepticus and excitotoxic neuronal injury. Pediatr Neurol. 2007;36:253–7. doi: 10.1016/j.pediatrneurol.2006.12.005. [DOI] [PubMed] [Google Scholar]
- Vespa PM, McArthur DL, Xu Y, Eliseo M, Etchepare M, Dinov I, et al. Nonconvulsive seizures after traumatic brain injury are associated with hippocampal atrophy. Neurology. 2010;75:792–8. doi: 10.1212/WNL.0b013e3181f07334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vespa PM, Miller C, McArthur D, Eliseo M, Etchepare M, Hirt D, et al. Nonconvulsive electrographic seizures after traumatic brain injury result in a delayed, prolonged increase in intracranial pressure and metabolic crisis. Crit Care Med. 2007;35:2830–6. [PMC free article] [PubMed] [Google Scholar]
- Williams K, Jarrar R, Buchhalter J. Continuous video-EEG monitoring in pediatric intensive care units. Epilepsia. 2011;52:1130–6. doi: 10.1111/j.1528-1167.2011.03070.x. [DOI] [PubMed] [Google Scholar]
- Yager JY, Armstrong EA, Miyashita H, Wirrell EC. Prolonged neonatal seizures exacerbate hypoxic-ischemic brain damage: correlation with cerebral energy metabolism and excitatory amino acid release. Dev Neurosci. 2002;24:367–81. doi: 10.1159/000069049. [DOI] [PubMed] [Google Scholar]
- Young GB, Jordan KG, Doig GS. An assessment of nonconvulsive seizures in the intensive care unit using continuous EEG monitoring: an investigation of variables associated with mortality. Neurology. 1996;47:83–9. doi: 10.1212/wnl.47.1.83. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.