Abstract
With technological advances in basic research, the intricate mechanism of secondary delayed spinal cord injury (SCI) continues to unravel at a rapid pace. However, despite our deeper understanding of the molecular changes occurring after initial insult to the spinal cord, the cure for paralysis remains elusive. Current treatment of SCI is limited to early administration of high dose steroids to mitigate the harmful effect of cord edema that occurs after SCI and to reduce the cascade of secondary delayed SCI. Recent evident-based clinical studies have cast doubt on the clinical benefit of steroids in SCI and intense focus on stem cell-based therapy has yielded some encouraging results. An array of mesenchymal stem cells (MSCs) from various sources with novel and promising strategies are being developed to improve function after SCI. In this review, we briefly discuss the pathophysiology of spinal cord injuries and characteristics and the potential sources of MSCs that can be used in the treatment of SCI. We will discuss the progress of MSCs application in research, focusing on the neuroprotective properties of MSCs. Finally, we will discuss the results from preclinical and clinical trials involving stem cell-based therapy in SCI.
Keywords: Spinal cord injury, Mesenchymal stem cells, Bone marrow stromal cells, Umbilical cord derived mesenchymal stem cells, Adipose tissue derived mesenchymal stem cells
Core tip: Despite our deeper understanding of the molecular changes that occurs after the spinal cord injury (SCI), the cure for paralysis remains elusive. In this review, the pathophysiology of SCI and characteristics and potential sources of mesenchymal stem cells (MSCs) that can be used in the treatment of SCI were discussed. We also discussed the progress of application of MSCs in research focusing on the neuroprotective properties of MSCs. Finally, we discussed the results from preclinical and clinical trials involving stem cell-based therapy in SCI.
INTRODUCTION
Traumatic spinal cord injury (SCI) continues to be a devastating injury to affected individuals and their families and exacts an enormous financial, psychological and emotional cost to them and to society. Despite years of research, the cure for paralysis remains elusive and current treatment is limited to early administration of high dose steroids and acute surgical intervention to minimize cord edema and the subsequent cascade of secondary delayed injury[1-3]. Recent advances in neurosciences and regenerative medicine have drawn attention to novel research methodologies for the treatment of SCI. In this review, we present our current understanding of spinal cord injury pathophysiology and the application of mesenchymal stem cells (MSCs) in the treatment of SCI. This review will be more useful for basic and clinical investigators in academia, industry and regulatory agencies as well as allied health professionals who are involved in stem cell research.
Direct mechanical damage to the spinal cord usually results in either partial or total loss of neural functions such as sensory perception and mobility[4]. The prevalence of people with SCI who are alive in the United States in 2013 is estimated to be approximately 273000[5]. According to census data, motor vehicle accidents (36.5%), falls (28.5%), and acts of violence (14.3%) are the most frequent causes of SCI since 2010. The average age at injury is 42.6 years and 80.7% of spinal cord injuries occur in males. Among those injured since 2010, 67.0% are Caucasian, 24.4% African American, 0.8% Native American and 2.1% Asian. The most frequent neurologic category at discharge of persons reported to the database since 2010 is incomplete tetraplegia (40.6%), followed by incomplete paraplegia (18.7%), complete paraplegia (18.0%) and complete tetraplegia (11.6%). Less than 1% of SCI patients experienced complete neurologic recovery by the time of hospital discharge. Over the last 20 years, the percentage of SCI patients with incomplete tetraplegia spinal cord injury has increased while the more devastating complete paraplegia and complete tetraplegia numbers have decreased[5]. Whether complete or incomplete injury, SCI is a devastating condition that not only paralyzes the affected individuals but also exacts tremendous emotional, social and financial burdens[6]. These patients also face increased risks of cardiovascular complications, deep vein thrombosis, osteoporosis, pressure ulcers, autonomic dysreflexia and neuropathic pain[3]. The limitation of any clinical treatment success is most likely due to the complex mechanisms of SCI and the relative inability of the human body to repair or regenerate neurons in the spinal cord[7].
PATHOPHYSIOLOGICAL FEATURES AFTER SCI
The pathophysiological processes that underlie SCI comprise the primary and secondary phases of injury[1,8]. Initial physical trauma to the spinal cord includes traction injury, compression forces and direct mechanical disruption of neural elements. Immediate microvascular injuries with central gray hemorrhage and disruption of cellular membrane and blood-spinal cord barrier are followed by edema, ischemia, release of cytotoxic chemicals from inflammatory pathways and electrolyte shifts. Subsequently, a secondary injury cascade is triggered that compounds the initial mechanical injury with necrosis and apoptosis that are injurious to surviving neighboring neurons, further reducing the chance of recovery of penumbra neurons and rendering any functional recovery almost hopeless[3,8]. Pathophysiological processes that occur in the secondary injury phase are responsible for exacerbating the initial damage and creating an inhibitory milieu that is hostile to endogenous efforts of repair, regeneration and remyelination. These secondary processes include inflammation, ischemia, lipid peroxidation, production of free radicals, disruption of ion channels, axonal demyelination, glial scar formation, necrosis and programmed cell death[3]. The post-trauma inflammatory response plays a critical role in the secondary phase after SCI through modulation of a series of complex cellular and molecular interactions[9]. After SCI, the blood-spinal cord barrier is disrupted due to hemorrhage and local inflammation[10]. The activation and recruitment of peripheral and resident inflammatory cells including microglial cells, astrocytes, monocytes, T-lymphocytes, and neutrophils promotes the development of secondary damage following SCI[11]. This secondary injury can be subdivided into the acute-phase (2 h-2 d), the sub-acute phase (days-weeks), and the chronic phase (months-years), each with distinct different pathophysiological processes[12-14]. These changes include edema, ischemia, hemorrhage, reactive oxygen species (ROS) production and lipid peroxidation, glutamate-mediated excitotoxicity, ionic dysregulation, blood-spinal-cord barrier permeability, inflammation, demyelination, neuronal cell death, neurogenic shock, macrophage infiltration, microglial activity, astrocyte activity and scar formation, initiation of neovascularization, Wallerian degeneration, glial scar maturation, cyst and syrinx formation, cavity formation and schwannosis. The end of spontaneous post-SCI changes is identified as a pathophysiological phenomenon with solid glial scar formation, syrinx formation, and neuronal apoptosis[15]. However, endogenous repair and regenerative mechanisms do occur during the secondary phase of injury to minimize the extent of the lesion (through astrogliosis), reorganize blood supply through angiogenesis, clear cellular debris, and reunite and remodel damaged neural circuits, and as such, offer exploitable targets for therapeutic intervention[3], the most promising of which is stem cell-based therapy[16].
MSC THERAPY AFTER SCI
An array of new and promising strategies is being developed to improve function after SCI. At present, two main therapeutic strategies, cell-based and gene-based therapies are being investigated to repair the injured mammalian spinal cord. At this time it appears that neither strategy by itself is efficacious, whereas a combinatory strategy appears to be more promising. The targeting of an array of deleterious processes within the tissue after SCI will require a multi-factorial intervention, multi-phasic polytherapy such as the combination of cell- and gene-based approaches[17]. This review focuses only on stem cell-based therapy. Cell-based therapy faces numerous challenges including selection of a SCI model, timing and mode of cell implantation, location of cellular injection and their subsequent migration, survival, transdifferentiation, immune incompatibility and rejection, and tracking of implanted cells[17]. Cellular therapies for SCI repair may involve modification or recruitment of endogenous cells in vivo, harvest and/or alteration ex vivo of endogenous cells that are subsequently implanted as autogeneic graft or transplanted into the injured organism as allogeneic or xenogeneic grafts. Transplanted stem cells promote neural regeneration and rescue impaired neural function after SCI by parasecreting permissive neurotrophic molecules at the lesion site to enhance the regenerative capacity thereby providing a scaffold for the regeneration of axons and replacing lost neurons and neural cells[17]. Mesenchymal stem cells have recently been advocated as a promising source for cellular repair after central nervous system (CNS) injury[15]. MSCs, also known as marrow stromal cells[18] or mesenchymal progenitor cells[19] are self-renewing, multipotent progenitor cells with the capacity to differentiate into several distinct mesenchymal lineages[20]. These cells are multipotent adult stem cells present in all tissues as part of the perivascular population. As multipotent cells, MSCs can differentiate into different mesodermal tissues ranging from bone and cartilage to cardiac muscle[21]. Several small clinical trials have investigated the efficacy and safety of MSCs in diseases including chronic heart failure, acute myocardial infarction, hematological malignancies and graft vs host disease. Pre-clinical evidence suggests that MSCs exert their beneficial effects largely through immunomodulatory and paracrine mechanisms[22].
MSCs are favored in stem cell therapy for SCI for the following reasons: (1) ease of isolation and cryopreservation[23], (2) maintenance of viability and regenerative capacity after cryopreservation at -80 °C[24], (3) rapid replication with high quality progenitor cells and high potential of multilineage differentiation[25], and (4) minimal or no immunoreactivity and graft-versus-host reaction of transplanted allogeneic MSCs[26]. MSCs were initially identified in bone marrow and later in muscle, adipose and connective tissue of human adults[21]. Bone marrow and umbilical cord blood are rich sources of these cells, but MSC have also been isolated from fat[27], skeletal muscle[28], human deciduous teeth[29], and trabecular bone[30]. Mesenchymal stem cells are ideally suited to address many pathophysiological consequences of SCI[3]. The major goals for the therapeutic use of stem cells is regeneration of axons, prevention of apoptosis and replacement of lost cells, particularly oligodendrocytes, in order to facilitate the remyelination of spared axons[31]. In this review, we touch upon the therapeutic applications of MSCs after SCI.
BONE MARROW STROMAL CELLS
Bone marrow-derived mesenchymal stem cells (BMSC) differentiate into cells of the mesodermal lineage but also, under certain experimental conditions, into cells of the neuronal and glial lineage. Their therapeutic translation has been significantly boosted by the demonstration that MSCs display significant anti-proliferative, anti-inflammatory and anti-apoptotic features. These properties have been exploited in the effective treatment of experimental autoimmune encephalomyelitis (EAE), experimental brain ischemia and in animals undergoing brain or spinal cord injury[32]. Several investigators have reported that MSCs possess immunosuppressive features[33-36]. These immunosuppressive properties, in combination with the restorative functions of BMSC reduce the acute inflammatory response to SCI, minimize cavity formation, as well as diminish astrocyte and microglia/macrophage reactivity[37-39]). BMSC transplantation in an experimental SCI model has been shown to enhance neuronal protection and cellular preservation via reduction in injury-induced sensitivity to mechanical trauma[39]. It was suggested that the beneficial effects of MSCs on hindlimb sensorimotor function may, in part, be explained by their ability to attenuate astrocyte reactivity and chronic microglia/macrophage activation[39]. These significant results demonstrated the potential of MSCs to serve as attenuators of the immune response. It was proposed that as attenuators, MSCs could potentially serve in an immunoregulatory capacity in disorders in which chronic activation of immune cells, such as reactive astrocytes and activated microglia/macrophages play a role. Studies by Hofstetter et al[40], indicated that transplanted MSC attenuates acute inflammation and promotes functional recovery following SCI. Ohta et al[41], suggested that BMSCs reduced post-SCI cavity formation and improved behavioral function by releasing trophic factors into the cerebrospinal fluid (CSF) or by direct interaction with host spinal tissues. Infusion of transplants through CSF provides no additional traumatic injury to the damaged spinal cord and BMSCs might be administered by lumbar puncture to the patients. Lumbar puncture can be done without severe invasion, so BMSCs can be repeatedly administered to maintain their effects. This study has demonstrated for the first time that the transplantation of BMSCs through CSF can promote the behavioral recovery and tissue repair of the injured spinal cord in rats, thus providing a road map for the clinical autograft of BMSCs without severe surgical infliction to human patients[41]. In another study, human mesenchymal stem cells (hMSCs) isolated from adult bone marrow were found to infiltrate primarily into the ventrolateral white matter tracts, spreading to adjacent segments rostro-caudal to the injury epicenter, and facilitate recovery from SCI by remyelinating spared white matter tracts and/or by enhancing axonal growth[42]. In our laboratory, we used mesenchymal stem cells from rat bone marrow to evaluate the therapeutic potential after SCI in rats[43]. We observed that caspase-3 mediated apoptosis after SCI on both neurons and oligodendrocytes was significantly downregulated by BMSC. Treatment with BMSC had a positive effect on behavioral outcome and better structural integrity preservation as seen in histopathological analysis. BMSC secrete protective factors that prevent neuronal apoptosis through stimulation of endogenous survival signaling pathways, namely PI3K/Akt and the MAPK/ERK1/2-cascade. Overall, these findings demonstrate that BMSC trigger endogenous survival signaling pathways in neurons that mediate protection against apoptotic insults. Moreover, the interaction between stressed neurons and BMSC further amplifies the observed neuroprotective effect[44].
Lu et al[45], investigated the nature of the chronic scar and its ability to block axon growth by testing the hypothesis that chronically injured spinal cord axons can regenerate through the gliotic scar in the presence of local growth-stimulating factors. BMSC, genetically modified to secrete neurotrophin-3 (NT-3) were injected into the lesion site of rats with cervical SCI[45]. It was observed that a modest number of axons penetrated through the chronic scar that contained a mixture of inhibitory and growth stimulating factors. Furthermore, robust axonal growth can be induced by the local provision of neurotrophic factors without resecting the chronic scar. In another study, Urdzíková et al[46], have shown that treatment with different cell populations obtained from bone marrow (MSCs, BMCs and the endogenous mobilization of bone marrow cells) has a beneficial effect on behavioral and histological outcomes after SCI. However, it is not clear whether the injection of MSCs, BMCs or granulocyte-colony stimulating factor (G-CSF) treatment induces functional and morphological improvement through the same mechanisms of action. Transplanted MSCs mollify the inflammatory response in the acute setting and reduce the inhibitory effects of scar tissue in the subacute/chronic setting to provide a permissive environment for axonal extension. In addition, grafted cells may provide a source of growth factors to enhance axonal elongation across spinal cord lesions[47]. Down-regulation of TNF-α expression in macrophages/microglia was observed at an early stage after SCI in rats transplanted with a gelatin sponge (GS) scaffold impregnated with rat bone marrow-derived mesenchymal stem cells at the site of injury[48]. It was also shown that 3D gelatin sponge scaffolds allowed MSCs to adhere, survive and proliferate and also for fibronectin to deposit. In vivo transplantation experiments demonstrated that these scaffolds were biocompatible and MSCs seeded to the scaffolds played an important role in attenuating inflammation, promoting angiogenesis, and reducing cavity formation. Novikova et al[49], observed that differentiated BMSC provided neuroprotection for axotomized rubrospinal neurons and increased the density of rubrospinal axons in the dorsolateral funiculus rostral to the injury site. They suggested that BMSC induced along the Schwann cell lineage increased expression of trophic factors and have neuroprotective and growth-promoting effects after SCI[49]. Cizkova et al[50], standardized the intrathecal (IT) catheter delivery of rat MSCs after SCI in adult rats. Based on these results, it was suggested that repetitive IT transplantation, which imposes a minimal burden on the animals, may improve behavioral function when the dose, timing, and targeted IT delivery of MSCs towards the lesion cavity was optimized. Kang et al[51], indicated that therapeutic rat BMSCs in a poly (D,L-lactide-co-glycolide)/small intestinal submucosa scaffold induced nerve regeneration in a complete spinal cord transection model and demonstrated that functional recovery further depended on defect length.
Park et al[52] evaluated the therapeutic efficacy of combining autologous BMSC transplantation with granulocyte macrophage-colony stimulating factor (GM-CSF) by subcutaneous administration directly into the spinal cord lesion site of six patients with complete SCI. At the 6-mo and 18-mo follow-up periods, four of the six patients showed neurological improvements by two ASIA (American Spinal Injury Association) grade (from ASIA A to ASIA C), while another improved from ASIA A to ASIA B[52]. Moreover, BMSC transplantation together with GM-CSF was not associated with increased morbidity or mortality. In another clinical trial, the safety of autologous bone marrow cell implantation was tested in twenty patients[53]. Motor-evoked potential, somatosensory-evoked potential, magnetic resonance imaging, and ASIA scores were measured in a clinical follow-up. This study demonstrated that BMSC transplantation is a relatively safe procedure, and BMSC-mediated repair can lead to modest improvements in some injured patients. It is also anticipated that a Phase II clinical trial designed to test the efficacy will be initiated in the near future. In a study conducted by Deng et al[54], implantation of BMSC elicited de novo neurogenesis, and functional recovery in a non-human primate SCI model with rhesus monkeys achieved Tarlov grades 2-3 and nearly normal sensory responses three months after transplantation. Zurita et al[55], observed progressive functional recovery three months after SCI in paraplegic pigs injected with autologous BMSC in autologous plasma into lesion zone and adjacent subarachnoid space. Intramedullary post-traumatic cavities were filled by a neoformed tissue containing several axons, together with BMSC, that expressed neuronal or glial markers. Furthermore, in the treated animals, electrophysiological studies showed recovery of the previously abolished somatosensory-evoked potentials. Despite promising data, further research is needed to establish whether bone marrow cell treatments can serve as a safe and efficacious autologous source for the treatment of SCI[47]. However, the use of BMSC in SCI does present certain issues-migration beyond the injection site (for intraspinally delivered cells) is limited and inter-donor variability in efficacy and immunomodulatory potency might be reflected in variable clinical outcome[37], making BMSC evaluation as a therapy for SCI difficult[3]. The pathological improvements of BMSC after SCI are summarized in Table 1.
Table 1.
Overview of effects of bone marrow stromal cells after spinal cord injury
| Source of MSC | Main pathological features improved/repaired | Limitations/recommendations/conclusions | Ref. |
| Human | Axonal growth, partial recovery of function | Differences in donor or lot-lot efficacy of MSC | Neuhuber et al[37], 2005 |
| Human | Axonal growth, significant behavioral recovery | Survival of BMSC grafts for longer duration | Himes et al[38], 2006 |
| Human | Significant motor improvements in human patients | Autologous bone marrow cell transplantation with GM-CSF administration has no serious complications. More comprehensive multicenter clinical studies are recommended | Park et al[52], 2005 |
| Human | Homing of MSC, functional recovery | Mechanisms of engraftment, homing, long-term safety | Cizkova et al[42], 2006 |
| Rhesus monkey | De novo neurogenesis and functional recovery in rhesus monkeys | Synergetic effects of MSC implantation and locally delivered neurotrophic factors in rhesus SCI models | Deng et al[54], 2006 |
| Pig | Improvement in somatosensory-evoked potentials, functional recovery in pigs | Possible utility of BMSC transplantation in humans suffering from chronic paraplegia | Zurita et al[55], 2008 |
| Rat | No allodynia, anti-inflammatory, increase in white matter volume and decrease in cyst size, sensorimotor enhancements | Survival of MSC | Abrams et al[39], 2009 |
| Rat | MSC form bundles bridging the lesion epicenter, functional recovery | Neuron-like MSC lacked voltage-gated ion channels for generation of action potentials | Hofstetter et al[40], 2002 |
| Rat | Cavity reduction, functional recovery | Unknown trophic factors secreted by BMSC | Ohta et al[41], 2004 |
| Rat | Downregulation of apoptosis, functional recovery | Intrinsic properties of MSC, microenvironment of the injured spinal cord, host-graft interactions | Dasari et al[43], 2007 |
| Rat/gerbil | Activation of survival signaling pathways, neuroprotection | Neuroprotective factors released by BMSC, interactions between neurons and BMSC | Isele et al[44], 2007 |
| Rat | Axonal regeneration, myelination of axons | Resection of the chronic scar | |
| Rat | Increase in spared white matter, functional recovery | Differences in mechanism of action of MSCs or BMCs (bone marrow cells) or G-CSF in inducing functional and morphological improvement | Urdzíková et al[46], 2006 |
| Rat | Reduction in inflammation, promoting angiogenesis, and reducing cavity formation | GS scaffolds may serve as a potential supporting biomaterial for wound healing after SCI | Zeng et al[48], 2011 |
| Rat | Extensive in-growth of serotonin-positive raphaespinal axons and calcitonin gene-related peptide-positive dorsal root sensory axons, attenuation of astroglial and microglial activity | Production of trophic factors support neuronal survival and axonal regeneration | Novikova et al[49], 2011 |
| Rat | Functional recovery | Repetitive IT transplantation may improve behavioral function depending on optimization of dose, timing, and targeted IT delivery of MSCs | Cizkova et al[50], 2011 |
| Rat | Axonal regeneration, functional recovery | Feasibility of therapeutic cell delivery using 3D scaffolds, especially in complete spinal cord transection | Kang et al[51], 2011 |
| Rat | Partial improvement in ASIA score in human patients | Polymer hydrogels may become suitable materials for bridging cavities after SCI | Sykova et al[53], 2006 |
SCI: Spinal cord injury; MSC: Marrow stromal cell; IT: Intrathecal; CSF: Cerebrospinal fluid; GS: Gelatin sponge; BMSC: Bone marrow-derived mesenchymal stem cell.
ADIPOSE TISSUE-DERIVED MESENCHYMAL CELLS
Adipose tissue is abundant in the body and contains a stromal fraction rich in stem- progenitor cells capable of undergoing differentiation into osteogenic, chondrogenic, and adipogenic lineages[56]. The in vitro as well as in vivo properties of adipose tissue-derived stromal cells (ADSCs) resemble those of MSCs obtained from bone marrow, and the liposuction procedure employed to harvest ADSCs is minimally invasive for the patient[57]. Kang et al[58], reported that intravenous infusion of oligodendrocyte precursor cells (OPCs) derived from rATSC autograft cells improved motor function in rat models of SCI. Moreover, cytoplasmic extracts prepared from adipose tissue stromal cells (ATSCs) inhibit H2O2-mediated apoptosis of cultured spinal cord-derived neural progenitor cells (NPCs) and improved cell survival[59]. ATSCs extracts mediated this effect by decreasing caspase-3 and c-Jun-NH2-terminal kinase (SAPK/JNK) activity, inhibiting cytochrome c release from mitochondria and reducing Bax expression levels in cells. Direct injection of ATSCs extracts mixed with matrigel into the spinal cord immediately after SCI also resulted in less apoptotic cell death, astrogliosis and hypo-myelination and showed significant functional improvement. Zhang et al[60], showed that ADSCs can differentiate into neural-like cells in vitro and in vivo. However, neural differentiated ADSCs did not result in any better functional recovery than did undifferentiated ones following SCI. Ryu et al[61], evaluated the implantation of allogenic adipose-derived stem cells (ASCs) for the improvement of neurological function in a canine SCI model. Using both in vitro and in vivo injury models, Oh et al[62], confirmed that hypoxic preconditioning (HP)-treated adipose tissue-derived mesenchymal stem cells (HP-AT-MSCs) increased cell survival and enhanced the expression of marker genes in DsRed-engineered neural stem cells (NSCs-DsRed). Based on their findings, it was suggested that the co-transplantation of HP-AT-MSCs with engineered neural stem cells (NSCs) can improve both cell survival and gene expression of the engineered NSCs. This novel strategy can be used to augment the therapeutic efficacy of combined stem cell and gene modulation therapy for SCI. In another study, Oh et al[63], examined the effects of co-transplanting mouse neural stem cells (mNSCs) and adipose tissue-derived mesenchymal stem cells (AT-MSCs) on mNSC viability. It was observed that mNSCs transplanted into rat spinal cords with AT-MSCs showed better survival rates than mNSCs transplanted alone, thereby suggesting that co-transplantation of mNSCs with AT-MSCs is a more effective strategy to improve the survival of transplanted stem cells into the injured spinal cord. In a more recent study, the same group investigated the effectiveness of a three-dimensional cell mass transplantation of adipose-derived stem cells (3DCM-ASCs) in hind limb functional recovery by the stimulation of angiogenesis and neurogenesis[64]. These results revealed a significantly elevated density of neovascular formations through angiogenic factors released by the 3DCM-ASCs at the lesion site, enhanced axonal outgrowth, and significant functional recovery. These findings suggest that transplantation of 3DCM-ASCs may be an effective stem cell transplantation modality for the treatment of spinal cord injuries and neural ischemia. In a similar study, Park et al[65], observed that a combination of matrigel and neural-induced mesenchymal stem cells (NMSC) reduced the expression of inflammation and/or astrogliosis markers and improved hind limb function in dogs with SCI. The predifferentiation of ASCs plays a beneficial role in SCI repair by promoting the protection of denuded axons and cellular repair that was induced mainly through paracrine mechanisms[57]. The propensity of proliferation and the potential of unchecked differentiation of stem cells raised the concern of inherent tumorigenicity and toxicity. Ra et al[66], observed that systemic transplantation of human Adipose tissue-derived mesenchymal stem cells (hAdMSCs) appeared to be safe and did not induce tumor development as none of the patients developed any serious adverse events related to hAdMSC transplantation during the three-month follow-up. Zhou et al[67], compared mesenchymal stromal cells from human bone marrow and adipose tissue for the treatment of spinal cord injury and suggested that hADSCs would be more appropriate than hBMSCs for transplantation to treat SCI. Recently, Zaminy et al[68], proved that adipose tissue-derived Schwann cells can modulate the hostile environment of the damaged spinal cord and generate a more stimulating environment to support axon regeneration and enhance functional recovery (Table 2).
Table 2.
Overview of effects of Adipose tissue-derived mesenchymal cells after spinal cord injury
| Source of MSC | Main pathological features improved/repaired | Limitations/recommendations/conclusions | Ref. |
| Human | Functional recovery | Interaction between engrafted rATSC-OPCs and endogenous spinal cord-derived NPCs promotes host injury repair | Kang et al[58], 2006 |
| Human | Improvement in both the cell survival and the gene expression of the engineered NSC observed in SCI rats | Hypoxia preconditioning strategy and combined stem cell/gene therapies can be used to augment the therapeutic efficacy at target injury sites | Oh et al[62], 2010 |
| Human | mNSCs transplanted into rat spinal cords with AT-MSCs showed better survival rates than mNSCs transplanted alone | Co-transplantation of mNSCs with AT-MSCs may be a more effective transplantation protocol to improve the survival of cells in the injured cord | Oh et al[63], 2011 |
| Human | Transplantation of 3DCM-ASCs into the injured spinal cord significantly elevated the density of vascular formations and enhanced axonal outgrowth at the lesion site, functional recovery | Transplantation of 3DCM-ASCs may be an effective stem cell therapy | Oh et al[64], 2012 |
| Human | No toxicity of hAdMSCs in immunodeficient mice, none of 8 male patients developed any serious adverse events related to hAdMSC transplantation in phase I clinical trial | Systemic transplantation of hAdMSCs appears to be safe and does not induce tumor development. Slow intravenous infusion of autologous hAdMSCs may be safe in SCI patients | Ra et al[66], 2011 |
| Human | Increase in BDNF levels, increased angiogenesis, preserved axons, decreased numbers of ED1-positive macrophages, reduced lesion cavity formation, functional recovery in rats | Compared with hBMSCs, hADSCs may be a better source of MSCs for cell therapy for acute SCI because of their relative abundance and accessibility | Zhou et al[67], 2013 |
| Dog | Significant improvement in nerve conduction velocity based on SEP, partial improvement in neurological functions of dogs | ASCs in spinal cord injuries might be partially due to neural differentiation of implanted stem cells | Ryu et al[61], 2009 |
| Dog | Anti-inflammation, anti-astrogliosis, neuronal extension, neuronal regeneration, functional recovery | The combination of Matrigel and NMSC produced beneficial effects | Park et al[65], 2012 |
| Rat | Reduced apoptotic cell death, astrogliosis and hypo-myelination, functional recovery | ATSC extracts may provide a powerful autoplastic therapy for neurodegenerative conditions in humans | Kang et al[59], 2007 |
| Rat | Neural differentiated ADSCs did not result in better functional recovery than undifferentiated ones following SCI | In vitro neural transdifferentiation of ADSCs might therefore not be a necessary pre-transplantation step | Zhang et al[60], 2009 |
| Rat | Functional recovery | Predifferentiation of ASCs plays a beneficial role in SCI repair | Arboleda et al[57], 2011 |
| Rat | Axonal regeneration, remyelination, functional recovery | Adipose tissue-derived Schwann cells can support axon regeneration and enhance functional recovery | Zaminy et al[68], 2013 |
OPCs: Oligodendrocyte precursor cells; NPCs: Neural progenitor cells; NSC: Neural stem cell; SCI: Spinal cord injury; MSC: Marrow stromal cell; AT: Adipose tissue; 3DCM-ASCs: Three-dimensional cell mass transplantation of adipose-derived stem cells; hAdMSCs: Human Adipose tissue-derived mesenchymal stem cells; NMSC: Neural-induced mesenchymal stem cells; ATSC: Adipose tissue stromal cell; ADSCs: Adipose tissue-derived stromal cells; BMSC: Bone marrow-derived mesenchymal stem cell.
HUMAN UMBILICAL CORD BLOOD- DERIVED MSCS
Human umbilical cord blood-derived mesenchymal stem cells (hUCBSC) offer great potential for novel therapeutic approaches targeted against many CNS diseases. Previous studies have reported that hUCBSC are beneficial in reversing the deleterious effects of SCI, even when infused five days after injury[69]. Transplanted hUCBSC differentiate into various neural cells and induce motor function improvement in SCI rat models[70]. In our laboratory, hUCBSC transplanted in rats one week after SCI were shown to transdifferentiate into neurons and oligodendrocytes and also to downregulate Fas-mediated apoptosis[71,72]. These transdifferentiated oligodendrocytes facilitated the secretion of neurotrophic hormones NT3 and BDNF and synthesized MBP and PLP, thereby promoting the remyelination of demyelinated axons in the injured spinal cord[71]. We observed that hUCBSC treatment increased myelin basic protein in vitro in PC-12 cells, which are normally not myelinated. To further confirm the ability of transplanted hUBCSC in remyelination, we injected hUBCSC into shiverer mice brains. This study clearly demonstrated that transplanted hUCBSC survived, migrated in vivo and myelinated genetically denuded axons in shiverer mice brains. The expression level of myelin basic protein, a major component of the myelin sheath, was significantly elevated in vivo and in vitro as revealed by Western blotting, reverse transcription polymerase chain reaction, immunohistochemistry, immunocytochemistry, and fluorescent in situ hybridization results. Further, transmission electron microscopic images of hUCBSC-treated shiverer mice brains showed several layers of myelin around the axons compared with a thin and fragmented layer of myelin in untreated animals (Figure 1). Moreover, the frequency of shivering was diminished one month after hUCBSC treatment. Our results strongly indicated that hUCBSC transplantation played an important role in re-myelination and could be an effective therapeutic approach for demyelinating or hypomyelinating disorders[73]. Furthermore, apoptotic pathways mediated by caspase-3, Fas and TNF-α were downregulated by hUCBSC[72,74]. The locomotor scale scores in hUCBSC-treated rats were significantly improved as compared to those of the control injured group. To further extend our studies, we utilized RT-PCR microarray and analyzed 84 apoptotic genes to identify the genetic modulation that occurred after traumatic SCI and after hUCBSC transplantation[75]. We observed that the genes involved in inflammation and apoptosis were up-regulated (TNF-α, TNFR1, TNFR2, Fas, Bad, Bid, Bid3, Bik, and Bak1) in the injured rat spinal cords, whereas genes such as XIAP, which are involved in neuroprotection, were up-regulated in the hUCBSC-treated rats (Figure 2, Tables 3 and 4). Our findings from co-cultures of cortical neurons with hUCBSC and blocking of the Akt pathway by a dominant-negative Akt and Akt-inhibitor IV confirmed that the mechanism underlying hUCBSC neuroprotection involved activation of the Akt signaling pathway. These results suggested the neuroprotective potential of hUCBSC against glutamate-induced apoptosis of cultured cortical neurons[74]. Both the in vivo and in vitro studies supported our hypothesis that the therapeutic mechanism of hUCBSC was remyelination of demyelinated axons and inhibition of the neuronal apoptosis during the repair phase of the injured spinal cord. Veeravalli et al[76] reported the involvement of tissue plasminogen activator (tPA) after SCI in rats and the role of hUCBSC. The tPA expression and activity were studied in vivo in rats after SCI and in vitro in rat embryonic spinal neurons in response to injury with staurosporine, hydrogen peroxide and glutamate. Infusion of hUCBSC downregulated tPA activity in vivo in rats as well as in vitro in the spinal neurons. Furthermore, MMP-2 is upregulated after hUCBSC treatment in spinal cord injured rats and in spinal neurons injured either with staurosporine or hydrogen peroxide. Also, hUCBSC-induced upregulation of MMP-2 diminished the formation of the glial scar at the site of injury along with reduced immunoreactivity to chondroitin sulfate proteoglycans. This upregulation of MMP-2 levels and reduction of glial scar formation by hUCBSC treatment after SCI created an environment more favorable for endogenous repair mechanisms[77] (Figure 3). Kao et al[78], suggested that hUCB derived-CD34+ cells can induce angiogenesis and endo/exogenous neurogenesis in SCI. In addition, Chen et al[79] recently showed that hUCB stem cells have the ability to secrete multiple neurotrophic factors. Their study demonstrated an elevation of neuroprotective cytokine serum IL-10 levels and a decrease in TNF-α levels after hUCB stem cells infusion. Moreover, both GDNF and VEGF could be detected in the injured spinal cord after the transplantation of hUCBSC, thereby promoting angiogenesis and neuronal regeneration. Recently, Ning et al[80], showed that transplantation of CD34+ HUCBCs during the acute phase could promote functional recovery better than during the subacute phase after SCI by raising neovascular density. These multifaceted protective and restorative effects from hUCB grafts may be interdependent and act in concert to promote therapeutic recovery for SCI (Table 5). Nevertheless, clinical studies with hUCBSC are still limited due to concerns about safety, mode of delivery, and efficiency. Among these concerns, the major histocompatibility in allogeneic transplantation is an important issue that needs to be addressed in future clinical trials for treating SCI[16].
Figure 1.

Transmission electron micrographs of shiverer mice brain showing thin and fragmented myelin around the axons in control and WI-38- implanted mice. In contrast, human umbilical cord blood-derived mesenchymal stem cells-treated shiverer brains showing myelin with several layers. Images are representatives of the several sections obtained from 3 different animals (n = 3). Scale bar = 33000. Stem Cells Dev 2011; 20: 881-891.
Figure 2.
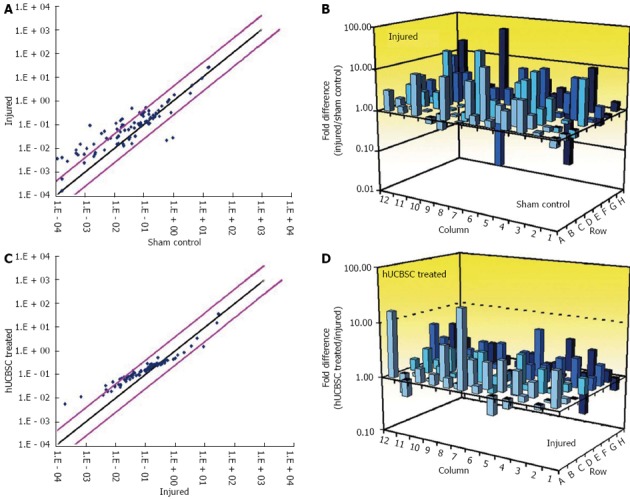
Microarray analysis of apoptotic genes after spinal cord injury. Total RNA was extracted from sham control, 3-wk post-spinal cord injury (SCI), and 3-wk post-SCI plus human umbilical cord blood-derived mesenchymal stem cells (hUCBSC)-treated tissues, reverse-transcribed, and the corresponding cDNA was loaded into a 96-well plate. In each group, RNA from at least three different animals was pooled together. A and C: Representative scatter plots show the validity of the experiment and the expression level of each gene in the control vs injured and injured vs hUCBSC-treated samples; B and D: These 3D profile graphs show the fold difference in expression of each gene between sham control vs injured and injured vs hUCBSC-treated samples. These experiments were performed in duplicate (hUCBSC, human umbilical cord blood-derived mesenchymal stem cells; SCI, spinal cord injury). J Neurotrauma 2009; 26: 2057-2069.
Table 3.
Changes in the expression of apoptotic genes and inhibitors after spinal cord injury and human umbilical cord blood stem cells treatment
| UniGene | GenBank | Gene name | Fold change after SCI | Fold change after hUCBSC treatment |
| Rn. 36696 | NM_022698 | Bad | 3.12 ± 1.34 | -1.47 ± 0.14 |
| Rn. 14598 | NM_053812 | Bak1 | 2.28 ± 0.99 | 1.36 ± 0.79 |
| Rn. 13007 | NM_031328 | Bcl10 | 8.83 ± 1.91 | 1.51 ± 1.45 |
| Rn. 19770 | NM_133416 | Bcl2a1 | 7.95 ± 1.98 | 1.79 ± 0.75 |
| Rn. 10323 | NM_031535 | Bcl2l1 | 2.13 ± 0.85 | -2.01 ± 0.89 |
| Rn. 162782 | NM_022684 | Bid | 2.45 ± 1.27 | 1.86 ± 0.99 |
| Rn. 89639 | NM_057130 | Bid3 | 5.43 ± 1.06 | 2.62 ± 0.75 |
| Rn. 38487 | NM_053704 | Bik | 4.41 ± 0.64 | 3.58 ± 0.14 |
| Rn. 92423 | XM_226742 | Birc1b | 25.84 ± 0.85 | 3.01 ± 0.67 |
| Rn. 64578 | NM_023987 | Birc3 | 10.14 ± 1.06 | 3.01 ± 0.78 |
| Rn. 54471 | NM_022274 | Birc5 | -2.84 ± 1.98 | 4.57 ± 1.14 |
| Rn. 55946 | NM_057138 | Cflar (Flip) | 3.12 ± 1.77 | -1.20 ± 0.86 |
Results are expressed as mean ± SD. hUCBSC: Human umbilical cord blood stem cells; SCI: Spinal cord injury. Refer Dasari et al[75].
Table 4.
Changes in the expression of caspase-related and nuclear factor-κB-related apoptotic genes after spinal cord injury
| UniGene | GenBank | Gene name | Fold change after SCI | Fold change after hUCBSC treatment |
| Rn. 37508 | NM_012762 | Casp1 | 9.14 ± 1.70 | 1.27 ± 0.78 |
| Rn. 81078 | NM_130422 | Casp12 | 2.91 ± 1.34 | 1.46 ± 0.68 |
| Rn. 10562 | NM_012922 | Casp3 | 3.56 ± 0.92 | 1.18 ± 0.84 |
| Rn. 88160 | NM_031775 | Casp6 | 3.34 ± 1.06 | 1.46 ± 0.79 |
| Rn. 53995 | NM_022260 | Casp7 | 2.81 ± 1.27 | 2.81 ± 1.21 |
| Rn. 54474 | NM_022277 | Casp8 | 3.84 ± 1.20 | 1.62 ± 0.89 |
| Rn. 32199 | NM_031632 | Casp9 | 2.86 ± 0.71 | 1.36 ± 0.62 |
| Rn. 67077 | NM_053362 | Dffb (Cad) | 32.94 ± 0.78 | 2.72 ± 0.84 |
| Rn. 16183 | NM_152937 | Fadd | 2.21 ± 0.78 | 1.51 ± 0.73 |
| Rn. 162521 | NM_139194 | Tnfrsf6 (Fas) | 10.87 ± 1.77 | 1.79 ± 0.67 |
| Rn. 44218 | NM_053353 | CD40lg | 15.91 ± 0.99 | 3.46 ± 0.78 |
| Rn. 160577 | NM_080769 | Lta (Tnfb) | 28.67 ± 0.07 | 2.06 ± 0.68 |
| Rn. 2275 | NM_012675 | TNF-α | 7.17 ± 1.63 | 2.36 ± 1.03 |
| Rn. 11119 | NM_013091 | Tnfrsf1a (TNFR1) | 2.53 ± 1.48 | 1.22 ± 0.78 |
| Rn. 83633 | NM_130426 | Tnfrsf1b (TNFR2) | 5.25 ± 1.56 | 3.01 ± 0.99 |
| Rn. 25180 | NM_134360 | Tnfrsf5 (CD40) | 4.26 ± 1.84 | 1.99 ± 0.78 |
| Rn. 54443 | NM_030989 | Tp53 (P53) | 3.46 ± 1.41 | -1.12 ± 0.61 |
| Rn. 18545 | XM_341671 | Tradd | 5.62 ± 1.13 | 1.46 ± 0.59 |
| Rn. 136874 | AI406530 | Traf1 | 4.12 ± 1.34 | 2.06 ± 0.84 |
Results are expressed as mean ± SD. hUCBSC: Human umbilical cord blood stem cells; NF-κB: Nuclear factor-κB; SCI: Spinal cord injury. Refer Dasari et al[75].
Figure 3.
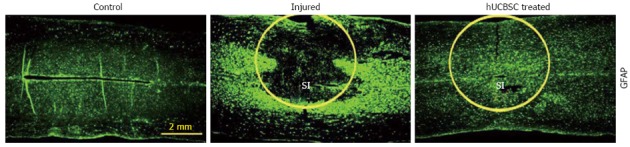
Reduction of inflammation in human umbilical cord blood-derived mesenchymal stem cell-treated spinal cords of rats. Immunohistochemical comparison of control, injured (21 d after spinal cord injury) and human umbilical cord blood-derived mesenchymal stem cells-treated spinal cord sections was performed to analyze the expression of reactive astrocytes at the site of injury. GFAP immunoreactivity is more evident and is localized at the lesion epicenter in the injured spinal cords. Astrogliosis is reduced in human umbilical cord blood-derived mesenchymal stem cells-treated sections. SI: Site of injury. Neurobiol Dis 2009; 36: 200-212.
Table 5.
Overview of effects of umbilical cord blood-derived mesenchymal stem cells after spinal cord injury
| Source of MSC | Main pathological features improved/repaired | Limitations/recommendations/conclusions | Ref. |
| Human | Stem cells migrated to injured areas, functional recovery | hUCB may be a viable source of stem cells for treatment of neurological disorders | Saporta et al[69], 2003 |
| Axonal regeneration, functional recovery | HUCBs and BDNF reduced the neurological function deficit to a moderate degree for SCI rats | Kuh et al[70], 2005 | |
| Stem cells secrete neurotrophic hormones and remyelinating proteins, axonal remyelination | Studies on long-term survival of hUCBSC and remyelination are recommended. | Dasari et al[71], 2007 | |
| Repair and maintenance of structural integrity of the injured spinal cord, downregulation of apoptosis, functional recovery | Role of hUCBSC in maintaining structural integrity and thereby promoting the long-term survival of neurons and oligodendrocytes in the injured spinal cord | Dasari et al[72], 2008 | |
| Downregulation of neuronal apoptosis | Modulation of the micro environment of the injured spinal cord by application of hUCBSC might be a potential therapeutic modality | Dasari et al[75], 2009 | |
| Downregulation of elevated tPA activity/expression in SCI rats | tPA is involved in secondary pathogenesis following spinal cord injury | Veeravalli et al[76] 2009 | |
| Upregulation of MMP2, reduction of glial scar | hUCBSC treatment after SCI upregulates MMP-2 levels and reduces the formation of the glial scar | Veeravalli et al[77], 2009 | |
| GDNF and VEGF were secreted in the injured spinal cord after transplantation of CD34+ cells | CD34+ cell therapy may be beneficial in reversing the SCI-induced spinal cord infarction and apoptosis and hindlimb dysfunction | Kao et al[78], 2008 | |
| Serum IL-10 levels increased, TNF-α levels decreased, functional recovery | Recovery of SCI-induced hind limb dysfunction is by increasing serum levels of IL-10, VEGF and GDNF in SCI rats. | Chen et al[79] 2008 | |
| Infarct size and blood vessel density at the injured site were significantly different in the treated group, functional recovery | Transplantation of CD34(+) HUCBCs during acute phase could promote functional recovery better than during subacute phase after SCI by raising blood vessel density | Ning et al[80], 2013 |
MSC: Mesenchymal stem cell; SCI: Spinal cord injury; IL: Interleukin; TNF-α: Tumor necrosis factor-α; hUCB: Human umbilical cord blood; hUCBSC: Human umbilical cord blood-derived mesenchymal stem cell.
HUMAN WHARTON’S JELLY/UMBILICAL CORD MATRIX CELLS
There are two main populations of cells with a mesenchymal character within the human umbilical cord: Wharton’s jelly mesenchymal stem cells (WJ-MSCs) and human umbilical cord perivascular cells (HUCPVCs)[81]. Wharton’s jelly cells (WJ-MSCs) can proliferate more rapidly and extensively than adult BMSCs (for a detailed review refer to Vawda and Fehlings, 2013). Yang et al[82], examined the effects of human umbilical mesenchymal stem cells (HUMSC) transplantation after complete spinal cord transection in rats. They observed that transplanted HUMSCs survived for 16 wk and produced large amounts of human neutrophil-activating protein-2, neurotrophin-3, basic fibroblast growth factor, glucocorticoid induced tumor necrosis factor receptor, and vascular endothelial growth factor receptor 3 in the host spinal cord. Zhang et al[83], used an animal model of transected SCI to test the hypothesis that co-grafted human umbilical mesenchymal stem cells-derived neurospheres (HUMSC-NSs) and BDNF can promote morphologic and functional recoveries of the injured spinal cord. Recovery of hindlimb locomotor function in SCI rats was significantly enhanced in human umbilical cord mesenchymal stem cells-grafted animals at five weeks as compared to control sham-grafted animals[84]. Using a rat model for clip SCI, Shang et al[85], showed that Neurotrophin-3 (NT-3) genetically modified human umbilical mesenchymal stem cells (NT-3-HUMSCs) promoted the morphologic and functional recovery of injured spinal cords (Table 6). Although these studies involved thoracic SCI model, these positive findings will most likely apply to cervical SCI as well[3].
Table 6.
Overview of effects of Wharton’s jelly/umbilical cord matrix cells after spinal cord injury
| Source of MSC | Main pathological features improved/repaired | Limitations/recommendations/conclusions | Ref. |
| Human | Survival of transplanted HUMSCs 16 wk, secretion of human neutrophil-activating protein-2, neurotrophin-3, basic fibroblast growth factor, glucocorticoid induced tumor necrosis factor receptor, and vascular endothelial growth factor receptor 3 in the host spinal cord | Transplantation of HUMSCs is beneficial to wound healing after SCI in rats | Yang et al[82], 2008 |
| Axonal regeneration, neuroprotective action by grafted cells, functional recovery | Co-grafted HUMSCs and BDNF may be a potential therapy for SCI | Zhang et al[83], 2009 | |
| hUCMSCs survive, migrate, and produce GDNF and neurotrophin-3, functional recovery | Studies on dose-dependent effects of hUCMSCs transplantation on SCI are required | Hu et al[84], 2010 | |
| Increased intensity of 5-HT fibers, increased volume of spared myelination, decreased area of cystic cavity, functional recovery | NT-3 enhanced therapeutic effects of HUMSCs after clip injury of the spinal cord. | Shang et al[85], 2011 |
MSC: Mesenchymal stem cell; SCI: Spinal cord injury; hUCBSC: Human umbilical cord blood-derived mesenchymal stem cell.
CONCLUSION
Therapeutic application of MSCs represents a promising approach in the treatment of spinal cord injury. Nevertheless, cell-based therapy for SCI in its nascent stages is facing several challenges including translational clinical issues, regulatory and ethical concerns, as well as modalities of transplantation, timing, safety and efficacy of the transplanted cells. A better understanding is also needed of the mechanisms of action and the behavior of stem cells in the pathological environment after transplantation in order to determine the best time frame and the most efficient routes for cell delivery after the injury[86]. Although several clinical trials utilize MSCs transplantation for the treatment of SCI, the ultimate value of a translational approach needs continued exploration of basic scientific knowledge of SCI and proven therapeutic efficacy via rigorous controlled, randomized, double blind, multi-center clinical trials.
ACKNOWLEDGMENTS
We thank Diana Meister for manuscript review. The authors wish to thank the editors of the Journal of Neurotrauma, Neurobiology of Disease and Stem Cells and Development for permission to use the figures and Tables 3 and 4, which appear in this article.
Footnotes
Supported by A grant from Illinois Neurological Institute to DHD
P- Reviewers: Ho I, Kan L, Miller RH S- Editor: Song XX L- Editor: A E- Editor: Zhang DN
References
- 1.Tator CH. Update on the pathophysiology and pathology of acute spinal cord injury. Brain Pathol. 1995;5:407–413. doi: 10.1111/j.1750-3639.1995.tb00619.x. [DOI] [PubMed] [Google Scholar]
- 2.Bracken MB. Steroids for acute spinal cord injury. Cochrane Database Syst Rev. 2012;1:CD001046. doi: 10.1002/14651858.CD001046.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vawda R, Fehlings MG. Mesenchymal cells in the treatment of spinal cord injury: current & future perspectives. Curr Stem Cell Res Ther. 2013;8:25–38. doi: 10.2174/1574888x11308010005. [DOI] [PubMed] [Google Scholar]
- 4.Yip PK, Malaspina A. Spinal cord trauma and the molecular point of no return. Mol Neurodegener. 2012;7:6. doi: 10.1186/1750-1326-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Birmingham, AL: University of Alabama at Birmingham, 2013 [Google Scholar]
- 6.Oyinbo CA. Secondary injury mechanisms in traumatic spinal cord injury: a nugget of this multiply cascade. Acta Neurobiol Exp (Wars) 2011;71:281–299. doi: 10.55782/ane-2011-1848. [DOI] [PubMed] [Google Scholar]
- 7.Cao HQ, Dong ED. An update on spinal cord injury research. Neurosci Bull. 2013;29:94–102. doi: 10.1007/s12264-012-1277-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McDonald JW, Sadowsky C. Spinal-cord injury. Lancet. 2002;359:417–425. doi: 10.1016/S0140-6736(02)07603-1. [DOI] [PubMed] [Google Scholar]
- 9.Thuret S, Moon LD, Gage FH. Therapeutic interventions after spinal cord injury. Nat Rev Neurosci. 2006;7:628–643. doi: 10.1038/nrn1955. [DOI] [PubMed] [Google Scholar]
- 10.Zhang N, Yin Y, Xu SJ, Wu YP, Chen WS. Inflammation & apoptosis in spinal cord injury. Indian J Med Res. 2012;135:287–296. [PMC free article] [PubMed] [Google Scholar]
- 11.Jaerve A, Müller HW. Chemokines in CNS injury and repair. Cell Tissue Res. 2012;349:229–248. doi: 10.1007/s00441-012-1427-3. [DOI] [PubMed] [Google Scholar]
- 12.Kakulas BA. A review of the neuropathology of human spinal cord injury with emphasis on special features. J Spinal Cord Med. 1999;22:119–124. doi: 10.1080/10790268.1999.11719557. [DOI] [PubMed] [Google Scholar]
- 13.Norenberg MD, Smith J, Marcillo A. The pathology of human spinal cord injury: defining the problems. J Neurotrauma. 2004;21:429–440. doi: 10.1089/089771504323004575. [DOI] [PubMed] [Google Scholar]
- 14.Rowland JW, Hawryluk GW, Kwon B, Fehlings MG. Current status of acute spinal cord injury pathophysiology and emerging therapies: promise on the horizon. Neurosurg Focus. 2008;25:E2. doi: 10.3171/FOC.2008.25.11.E2. [DOI] [PubMed] [Google Scholar]
- 15.Li J, Lepski G. Cell transplantation for spinal cord injury: a systematic review. Biomed Res Int. 2013;2013:786475. doi: 10.1155/2013/786475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park DH, Lee JH, Borlongan CV, Sanberg PR, Chung YG, Cho TH. Transplantation of umbilical cord blood stem cells for treating spinal cord injury. Stem Cell Rev. 2011;7:181–194. doi: 10.1007/s12015-010-9163-0. [DOI] [PubMed] [Google Scholar]
- 17.Pearse DD, Bunge MB. Designing cell- and gene-based regeneration strategies to repair the injured spinal cord. J Neurotrauma. 2006;23:438–452. doi: 10.1089/neu.2006.23.437. [DOI] [PubMed] [Google Scholar]
- 18.Prockop DJ. Marrow stromal cells as stem cells for nonhematopoietic tissues. Science. 1997;276:71–74. doi: 10.1126/science.276.5309.71. [DOI] [PubMed] [Google Scholar]
- 19.Conget PA, Minguell JJ. Phenotypical and functional properties of human bone marrow mesenchymal progenitor cells. J Cell Physiol. 1999;181:67–73. doi: 10.1002/(SICI)1097-4652(199910)181:1<67::AID-JCP7>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 20.Caplan AI. Why are MSCs therapeutic? New data: new insight. J Pathol. 2009;217:318–324. doi: 10.1002/path.2469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Malgieri A, Kantzari E, Patrizi MP, Gambardella S. Bone marrow and umbilical cord blood human mesenchymal stem cells: state of the art. Int J Clin Exp Med. 2010;3:248–269. [PMC free article] [PubMed] [Google Scholar]
- 22.Lalu MM, McIntyre L, Pugliese C, Fergusson D, Winston BW, Marshall JC, Granton J, Stewart DJ. Safety of cell therapy with mesenchymal stromal cells (SafeCell): a systematic review and meta-analysis of clinical trials. PLoS One. 2012;7:e47559. doi: 10.1371/journal.pone.0047559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee MW, Yang MS, Park JS, Kim HC, Kim YJ, Choi J. Isolation of mesenchymal stem cells from cryopreserved human umbilical cord blood. Int J Hematol. 2005;81:126–130. doi: 10.1532/ijh97.a10404. [DOI] [PubMed] [Google Scholar]
- 24.Kotobuki N, Hirose M, Takakura Y, Ohgushi H. Cultured autologous human cells for hard tissue regeneration: preparation and characterization of mesenchymal stem cells from bone marrow. Artif Organs. 2004;28:33–39. doi: 10.1111/j.1525-1594.2004.07320.x. [DOI] [PubMed] [Google Scholar]
- 25.Sekiya I, Larson BL, Smith JR, Pochampally R, Cui JG, Prockop DJ. Expansion of human adult stem cells from bone marrow stroma: conditions that maximize the yields of early progenitors and evaluate their quality. Stem Cells. 2002;20:530–541. doi: 10.1634/stemcells.20-6-530. [DOI] [PubMed] [Google Scholar]
- 26.Carrade DD, Affolter VK, Outerbridge CA, Watson JL, Galuppo LD, Buerchler S, Kumar V, Walker NJ, Borjesson DL. Intradermal injections of equine allogeneic umbilical cord-derived mesenchymal stem cells are well tolerated and do not elicit immediate or delayed hypersensitivity reactions. Cytotherapy. 2011;13:1180–1192. doi: 10.3109/14653249.2011.602338. [DOI] [PubMed] [Google Scholar]
- 27.Gronthos S, Franklin DM, Leddy HA, Robey PG, Storms RW, Gimble JM. Surface protein characterization of human adipose tissue-derived stromal cells. J Cell Physiol. 2001;189:54–63. doi: 10.1002/jcp.1138. [DOI] [PubMed] [Google Scholar]
- 28.Jankowski RJ, Deasy BM, Huard J. Muscle-derived stem cells. Gene Ther. 2002;9:642–647. doi: 10.1038/sj.gt.3301719. [DOI] [PubMed] [Google Scholar]
- 29.Miura M, Gronthos S, Zhao M, Lu B, Fisher LW, Robey PG, Shi S. SHED: stem cells from human exfoliated deciduous teeth. Proc Natl Acad Sci USA. 2003;100:5807–5812. doi: 10.1073/pnas.0937635100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nöth U, Osyczka AM, Tuli R, Hickok NJ, Danielson KG, Tuan RS. Multilineage mesenchymal differentiation potential of human trabecular bone-derived cells. J Orthop Res. 2002;20:1060–1069. doi: 10.1016/S0736-0266(02)00018-9. [DOI] [PubMed] [Google Scholar]
- 31.Dasari VR, Veeravalli KK, Rao JS, Fassett D, Dinh DH. Mesenchymal Stem Cell Therapy for Apoptosis After Spinal Cord Injury. In: Chang RCC, editor. Advanced Understanding of Neurodegenerative Diseases. Croatia: InTech; 2011. pp. 365–394. [Google Scholar]
- 32.Uccelli A, Benvenuto F, Laroni A, Giunti D. Neuroprotective features of mesenchymal stem cells. Best Pract Res Clin Haematol. 2011;24:59–64. doi: 10.1016/j.beha.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 33.Bartholomew A, Sturgeon C, Siatskas M, Ferrer K, McIntosh K, Patil S, Hardy W, Devine S, Ucker D, Deans R, et al. Mesenchymal stem cells suppress lymphocyte proliferation in vitro and prolong skin graft survival in vivo. Exp Hematol. 2002;30:42–48. doi: 10.1016/s0301-472x(01)00769-x. [DOI] [PubMed] [Google Scholar]
- 34.Di Nicola M, Carlo-Stella C, Magni M, Milanesi M, Longoni PD, Matteucci P, Grisanti S, Gianni AM. Human bone marrow stromal cells suppress T-lymphocyte proliferation induced by cellular or nonspecific mitogenic stimuli. Blood. 2002;99:3838–3843. doi: 10.1182/blood.v99.10.3838. [DOI] [PubMed] [Google Scholar]
- 35.Jiang XX, Zhang Y, Liu B, Zhang SX, Wu Y, Yu XD, Mao N. Human mesenchymal stem cells inhibit differentiation and function of monocyte-derived dendritic cells. Blood. 2005;105:4120–4126. doi: 10.1182/blood-2004-02-0586. [DOI] [PubMed] [Google Scholar]
- 36.Corcione A, Benvenuto F, Ferretti E, Giunti D, Cappiello V, Cazzanti F, Risso M, Gualandi F, Mancardi GL, Pistoia V, et al. Human mesenchymal stem cells modulate B-cell functions. Blood. 2006;107:367–372. doi: 10.1182/blood-2005-07-2657. [DOI] [PubMed] [Google Scholar]
- 37.Neuhuber B, Timothy Himes B, Shumsky JS, Gallo G, Fischer I. Axon growth and recovery of function supported by human bone marrow stromal cells in the injured spinal cord exhibit donor variations. Brain Res. 2005;1035:73–85. doi: 10.1016/j.brainres.2004.11.055. [DOI] [PubMed] [Google Scholar]
- 38.Himes BT, Neuhuber B, Coleman C, Kushner R, Swanger SA, Kopen GC, Wagner J, Shumsky JS, Fischer I. Recovery of function following grafting of human bone marrow-derived stromal cells into the injured spinal cord. Neurorehabil Neural Repair. 2006;20:278–296. doi: 10.1177/1545968306286976. [DOI] [PubMed] [Google Scholar]
- 39.Abrams MB, Dominguez C, Pernold K, Reger R, Wiesenfeld-Hallin Z, Olson L, Prockop D. Multipotent mesenchymal stromal cells attenuate chronic inflammation and injury-induced sensitivity to mechanical stimuli in experimental spinal cord injury. Restor Neurol Neurosci. 2009;27:307–321. doi: 10.3233/RNN-2009-0480. [DOI] [PubMed] [Google Scholar]
- 40.Hofstetter CP, Schwarz EJ, Hess D, Widenfalk J, El Manira A, Prockop DJ, Olson L. Marrow stromal cells form guiding strands in the injured spinal cord and promote recovery. Proc Natl Acad Sci USA. 2002;99:2199–2204. doi: 10.1073/pnas.042678299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ohta M, Suzuki Y, Noda T, Ejiri Y, Dezawa M, Kataoka K, Chou H, Ishikawa N, Matsumoto N, Iwashita Y, et al. Bone marrow stromal cells infused into the cerebrospinal fluid promote functional recovery of the injured rat spinal cord with reduced cavity formation. Exp Neurol. 2004;187:266–278. doi: 10.1016/j.expneurol.2004.01.021. [DOI] [PubMed] [Google Scholar]
- 42.Cízková D, Rosocha J, Vanický I, Jergová S, Cízek M. Transplants of human mesenchymal stem cells improve functional recovery after spinal cord injury in the rat. Cell Mol Neurobiol. 2006;26:1167–1180. doi: 10.1007/s10571-006-9093-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dasari VR, Spomar DG, Cady C, Gujrati M, Rao JS, Dinh DH. Mesenchymal stem cells from rat bone marrow downregulate caspase-3-mediated apoptotic pathway after spinal cord injury in rats. Neurochem Res. 2007;32:2080–2093. doi: 10.1007/s11064-007-9368-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Isele NB, Lee HS, Landshamer S, Straube A, Padovan CS, Plesnila N, Culmsee C. Bone marrow stromal cells mediate protection through stimulation of PI3-K/Akt and MAPK signaling in neurons. Neurochem Int. 2007;50:243–250. doi: 10.1016/j.neuint.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 45.Lu P, Jones LL, Tuszynski MH. Axon regeneration through scars and into sites of chronic spinal cord injury. Exp Neurol. 2007;203:8–21. doi: 10.1016/j.expneurol.2006.07.030. [DOI] [PubMed] [Google Scholar]
- 46.Urdzíková L, Jendelová P, Glogarová K, Burian M, Hájek M, Syková E. Transplantation of bone marrow stem cells as well as mobilization by granulocyte-colony stimulating factor promotes recovery after spinal cord injury in rats. J Neurotrauma. 2006;23:1379–1391. doi: 10.1089/neu.2006.23.1379. [DOI] [PubMed] [Google Scholar]
- 47.Wright KT, El Masri W, Osman A, Chowdhury J, Johnson WE. Concise review: Bone marrow for the treatment of spinal cord injury: mechanisms and clinical applications. Stem Cells. 2011;29:169–178. doi: 10.1002/stem.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zeng X, Zeng YS, Ma YH, Lu LY, Du BL, Zhang W, Li Y, Chan WY. Bone marrow mesenchymal stem cells in a three-dimensional gelatin sponge scaffold attenuate inflammation, promote angiogenesis, and reduce cavity formation in experimental spinal cord injury. Cell Transplant. 2011;20:1881–1899. doi: 10.3727/096368911X566181. [DOI] [PubMed] [Google Scholar]
- 49.Novikova LN, Brohlin M, Kingham PJ, Novikov LN, Wiberg M. Neuroprotective and growth-promoting effects of bone marrow stromal cells after cervical spinal cord injury in adult rats. Cytotherapy. 2011;13:873–887. doi: 10.3109/14653249.2011.574116. [DOI] [PubMed] [Google Scholar]
- 50.Cizkova D, Novotna I, Slovinska L, Vanicky I, Jergova S, Rosocha J, Radonak J. Repetitive intrathecal catheter delivery of bone marrow mesenchymal stromal cells improves functional recovery in a rat model of contusive spinal cord injury. J Neurotrauma. 2011;28:1951–1961. doi: 10.1089/neu.2010.1413. [DOI] [PubMed] [Google Scholar]
- 51.Kang KN, Lee JY, Kim da Y, Lee BN, Ahn HH, Lee B, Khang G, Park SR, Min BH, Kim JH, et al. Regeneration of completely transected spinal cord using scaffold of poly(D,L-lactide-co-glycolide)/small intestinal submucosa seeded with rat bone marrow stem cells. Tissue Eng Part A. 2011;17:2143–2152. doi: 10.1089/ten.TEA.2011.0122. [DOI] [PubMed] [Google Scholar]
- 52.Park HC, Shim YS, Ha Y, Yoon SH, Park SR, Choi BH, Park HS. Treatment of complete spinal cord injury patients by autologous bone marrow cell transplantation and administration of granulocyte-macrophage colony stimulating factor. Tissue Eng. 2005;11:913–922. doi: 10.1089/ten.2005.11.913. [DOI] [PubMed] [Google Scholar]
- 53.Syková E, Jendelová P, Urdzíková L, Lesný P, Hejcl A. Bone marrow stem cells and polymer hydrogels--two strategies for spinal cord injury repair. Cell Mol Neurobiol. 2006;26:1113–1129. doi: 10.1007/s10571-006-9007-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Deng YB, Liu XG, Liu ZG, Liu XL, Liu Y, Zhou GQ. Implantation of BM mesenchymal stem cells into injured spinal cord elicits de novo neurogenesis and functional recovery: evidence from a study in rhesus monkeys. Cytotherapy. 2006;8:210–214. doi: 10.1080/14653240600760808. [DOI] [PubMed] [Google Scholar]
- 55.Zurita M, Vaquero J, Bonilla C, Santos M, De Haro J, Oya S, Aguayo C. Functional recovery of chronic paraplegic pigs after autologous transplantation of bone marrow stromal cells. Transplantation. 2008;86:845–853. doi: 10.1097/TP.0b013e318186198f. [DOI] [PubMed] [Google Scholar]
- 56.Yamada T, Akamatsu H, Hasegawa S, Yamamoto N, Yoshimura T, Hasebe Y, Inoue Y, Mizutani H, Uzawa T, Matsunaga K, et al. Age-related changes of p75 neurotrophin receptor-positive adipose-derived stem cells. J Dermatol Sci. 2010;58:36–42. doi: 10.1016/j.jdermsci.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 57.Arboleda D, Forostyak S, Jendelova P, Marekova D, Amemori T, Pivonkova H, Masinova K, Sykova E. Transplantation of predifferentiated adipose-derived stromal cells for the treatment of spinal cord injury. Cell Mol Neurobiol. 2011;31:1113–1122. doi: 10.1007/s10571-011-9712-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kang SK, Shin MJ, Jung JS, Kim YG, Kim CH. Autologous adipose tissue-derived stromal cells for treatment of spinal cord injury. Stem Cells Dev. 2006;15:583–594. doi: 10.1089/scd.2006.15.583. [DOI] [PubMed] [Google Scholar]
- 59.Kang SK, Yeo JE, Kang KS, Phinney DG. Cytoplasmic extracts from adipose tissue stromal cells alleviates secondary damage by modulating apoptosis and promotes functional recovery following spinal cord injury. Brain Pathol. 2007;17:263–275. doi: 10.1111/j.1750-3639.2007.00070.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhang HT, Luo J, Sui LS, Ma X, Yan ZJ, Lin JH, Wang YS, Chen YZ, Jiang XD, Xu RX. Effects of differentiated versus undifferentiated adipose tissue-derived stromal cell grafts on functional recovery after spinal cord contusion. Cell Mol Neurobiol. 2009;29:1283–1292. doi: 10.1007/s10571-009-9424-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ryu HH, Lim JH, Byeon YE, Park JR, Seo MS, Lee YW, Kim WH, Kang KS, Kweon OK. Functional recovery and neural differentiation after transplantation of allogenic adipose-derived stem cells in a canine model of acute spinal cord injury. J Vet Sci. 2009;10:273–284. doi: 10.4142/jvs.2009.10.4.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Oh JS, Ha Y, An SS, Khan M, Pennant WA, Kim HJ, Yoon DH, Lee M, Kim KN. Hypoxia-preconditioned adipose tissue-derived mesenchymal stem cell increase the survival and gene expression of engineered neural stem cells in a spinal cord injury model. Neurosci Lett. 2010;472:215–219. doi: 10.1016/j.neulet.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 63.Oh JS, Kim KN, An SS, Pennant WA, Kim HJ, Gwak SJ, Yoon DH, Lim MH, Choi BH, Ha Y. Cotransplantation of mouse neural stem cells (mNSCs) with adipose tissue-derived mesenchymal stem cells improves mNSC survival in a rat spinal cord injury model. Cell Transplant. 2011;20:837–849. doi: 10.3727/096368910X539083. [DOI] [PubMed] [Google Scholar]
- 64.Oh JS, Park IS, Kim KN, Yoon DH, Kim SH, Ha Y. Transplantation of an adipose stem cell cluster in a spinal cord injury. Neuroreport. 2012;23:277–282. doi: 10.1097/WNR.0b013e3283505ae2. [DOI] [PubMed] [Google Scholar]
- 65.Park SS, Lee YJ, Lee SH, Lee D, Choi K, Kim WH, Kweon OK, Han HJ. Functional recovery after spinal cord injury in dogs treated with a combination of Matrigel and neural-induced adipose-derived mesenchymal Stem cells. Cytotherapy. 2012;14:584–597. doi: 10.3109/14653249.2012.658913. [DOI] [PubMed] [Google Scholar]
- 66.Ra JC, Shin IS, Kim SH, Kang SK, Kang BC, Lee HY, Kim YJ, Jo JY, Yoon EJ, Choi HJ, et al. Safety of intravenous infusion of human adipose tissue-derived mesenchymal stem cells in animals and humans. Stem Cells Dev. 2011;20:1297–1308. doi: 10.1089/scd.2010.0466. [DOI] [PubMed] [Google Scholar]
- 67.Zhou Z, Chen Y, Zhang H, Min S, Yu B, He B, Jin A. Comparison of mesenchymal stromal cells from human bone marrow and adipose tissue for the treatment of spinal cord injury. Cytotherapy. 2013;15:434–448. doi: 10.1016/j.jcyt.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 68.Zaminy A, Shokrgozar MA, Sadeghi Y, Norouzian M, Heidari MH, Piryaei A. Transplantation of schwann cells differentiated from adipose stem cells improves functional recovery in rat spinal cord injury. Arch Iran Med. 2013;16:533–541. [PubMed] [Google Scholar]
- 69.Saporta S, Kim JJ, Willing AE, Fu ES, Davis CD, Sanberg PR. Human umbilical cord blood stem cells infusion in spinal cord injury: engraftment and beneficial influence on behavior. J Hematother Stem Cell Res. 2003;12:271–278. doi: 10.1089/152581603322023007. [DOI] [PubMed] [Google Scholar]
- 70.Kuh SU, Cho YE, Yoon DH, Kim KN, Ha Y. Functional recovery after human umbilical cord blood cells transplantation with brain-derived neutrophic factor into the spinal cord injured rat. Acta Neurochir (Wien) 2005;147:985–92; discussion 992. doi: 10.1007/s00701-005-0538-y. [DOI] [PubMed] [Google Scholar]
- 71.Dasari VR, Spomar DG, Gondi CS, Sloffer CA, Saving KL, Gujrati M, Rao JS, Dinh DH. Axonal remyelination by cord blood stem cells after spinal cord injury. J Neurotrauma. 2007;24:391–410. doi: 10.1089/neu.2006.0142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dasari VR, Spomar DG, Li L, Gujrati M, Rao JS, Dinh DH. Umbilical cord blood stem cell mediated downregulation of fas improves functional recovery of rats after spinal cord injury. Neurochem Res. 2008;33:134–149. doi: 10.1007/s11064-007-9426-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Veeravalli KK, Dasari VR, Fassett D, Dinh DH, Rao JS. Human umbilical cord blood-derived mesenchymal stem cells upregulate myelin basic protein in shiverer mice. Stem Cells Dev. 2011;20:881–891. doi: 10.1089/scd.2010.0187. [DOI] [PubMed] [Google Scholar]
- 74.Dasari VR, Veeravalli KK, Saving KL, Gujrati M, Fassett D, Klopfenstein JD, Dinh DH, Rao JS. Neuroprotection by cord blood stem cells against glutamate-induced apoptosis is mediated by Akt pathway. Neurobiol Dis. 2008;32:486–498. doi: 10.1016/j.nbd.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 75.Dasari VR, Veeravalli KK, Tsung AJ, Gondi CS, Gujrati M, Dinh DH, Rao JS. Neuronal apoptosis is inhibited by cord blood stem cells after spinal cord injury. J Neurotrauma. 2009;26:2057–2069. doi: 10.1089/neu.2008.0725. [DOI] [PubMed] [Google Scholar]
- 76.Veeravalli KK, Dasari VR, Tsung AJ, Dinh DH, Gujrati M, Fassett D, Rao JS. Stem cells downregulate the elevated levels of tissue plasminogen activator in rats after spinal cord injury. Neurochem Res. 2009;34:1183–1194. doi: 10.1007/s11064-008-9894-3. [DOI] [PubMed] [Google Scholar]
- 77.Veeravalli KK, Dasari VR, Tsung AJ, Dinh DH, Gujrati M, Fassett D, Rao JS. Human umbilical cord blood stem cells upregulate matrix metalloproteinase-2 in rats after spinal cord injury. Neurobiol Dis. 2009;36:200–212. doi: 10.1016/j.nbd.2009.07.012. [DOI] [PubMed] [Google Scholar]
- 78.Kao CH, Chen SH, Chio CC, Lin MT. Human umbilical cord blood-derived CD34+ cells may attenuate spinal cord injury by stimulating vascular endothelial and neurotrophic factors. Shock. 2008;29:49–55. doi: 10.1097/shk.0b013e31805cddce. [DOI] [PubMed] [Google Scholar]
- 79.Chen CT, Foo NH, Liu WS, Chen SH. Infusion of human umbilical cord blood cells ameliorates hind limb dysfunction in experimental spinal cord injury through anti-inflammatory, vasculogenic and neurotrophic mechanisms. Pediatr Neonatol. 2008;49:77–83. doi: 10.1016/S1875-9572(08)60017-0. [DOI] [PubMed] [Google Scholar]
- 80.Ning G, Tang L, Wu Q, Li Y, Li Y, Zhang C, Feng S. Human umbilical cord blood stem cells for spinal cord injury: early transplantation results in better local angiogenesis. Regen Med. 2013;8:271–281. doi: 10.2217/rme.13.26. [DOI] [PubMed] [Google Scholar]
- 81.Carvalho MM, Teixeira FG, Reis RL, Sousa N, Salgado AJ. Mesenchymal stem cells in the umbilical cord: phenotypic characterization, secretome and applications in central nervous system regenerative medicine. Curr Stem Cell Res Ther. 2011;6:221–228. doi: 10.2174/157488811796575332. [DOI] [PubMed] [Google Scholar]
- 82.Yang CC, Shih YH, Ko MH, Hsu SY, Cheng H, Fu YS. Transplantation of human umbilical mesenchymal stem cells from Wharton’s jelly after complete transection of the rat spinal cord. PLoS One. 2008;3:e3336. doi: 10.1371/journal.pone.0003336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zhang L, Zhang HT, Hong SQ, Ma X, Jiang XD, Xu RX. Cografted Wharton’s jelly cells-derived neurospheres and BDNF promote functional recovery after rat spinal cord transection. Neurochem Res. 2009;34:2030–2039. doi: 10.1007/s11064-009-9992-x. [DOI] [PubMed] [Google Scholar]
- 84.Hu SL, Luo HS, Li JT, Xia YZ, Li L, Zhang LJ, Meng H, Cui GY, Chen Z, Wu N, et al. Functional recovery in acute traumatic spinal cord injury after transplantation of human umbilical cord mesenchymal stem cells. Crit Care Med. 2010;38:2181–2189. doi: 10.1097/CCM.0b013e3181f17c0e. [DOI] [PubMed] [Google Scholar]
- 85.Shang AJ, Hong SQ, Xu Q, Wang HY, Yang Y, Wang ZF, Xu BN, Jiang XD, Xu RX. NT-3-secreting human umbilical cord mesenchymal stromal cell transplantation for the treatment of acute spinal cord injury in rats. Brain Res. 2011;1391:102–113. doi: 10.1016/j.brainres.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 86.Forostyak S, Jendelova P, Sykova E. The role of mesenchymal stromal cells in spinal cord injury, regenerative medicine and possible clinical applications. Biochimie. 2013;95:2257–2270. doi: 10.1016/j.biochi.2013.08.004. [DOI] [PubMed] [Google Scholar]


