Abstract
Background
Dermatologists at the University of California, San Francisco recently reported two patients in the online Journal of the American Academy of Dermatology with purpura presumably induced by levamisole in contaminated cocaine. Levamisole-induced vasculitis and neutropenia has been reported elsewhere in the United States and Canada. Up to 70% of cocaine in the United States could be contaminated.
Objective
We sought to describe similar cases of vasculitis associated with cocaine use.
Methods
This is a retrospective case series.
Results
We report 6 remarkably similar patients seen over just the past few months with retiform purpura on the body and tender purpuric eruptions, necrosis, and eschars of the ears after cocaine use in New York and California. All of these patients had positive perinuclear antineutrophil cytoplasmic antibody values and 3 of the 6 also had an associated neutropenia. Direct immunofluorescence studies suggested an immune complex–mediated vasculitis.
Limitations
This case series is descriptive in nature and, because testing is not easily performed, we did not test for levamisole in the serum or blood to prove this is the causative agent.
Conclusion
It appears the use of cocaine is associated with the peculiar clinical findings of ear purpura, retiform purpura of the trunk, and neutropenia. We believe this case series may represent the tip of the iceberg as a looming public health problem caused by levamisole. Although the direct causal relationship may be difficult to establish, the astute dermatologist or primary care physician should be able to recognize the characteristic skin lesions and should be wary of the potential development of agranulocytosis. (J Am Acad Dermatol 2011;65:722-5.)
Keywords: agranulocytosis, cocaine, drug reaction, levamisole, neutropenia, purpura, vasculitis
This brief case series follows up on the letter1 published online in March 2010 in the Journal of the American Academy of Dermatology by dermatologists at the University of California, San Francisco describing two patients with probable levamisole-induced toxicities. In that letter, they describe two complicated medical patients with recent cocaine use, ensuing neutropenia, and retiform purpura. Because these patients had various positive serologic tests (eg, antineutrophil cytoplasmic antibodies [ANCAs], lupus anticoagulants) and confounding medical problems (hepatitis C and methicillin-resistant Staphylococcus aureus infection), the team at the University of California, San Francisco thoroughly reviewed the differential diagnosis for these patients and then astutely posed the question: could these symptoms and signs be caused by levamisole-contaminated cocaine?
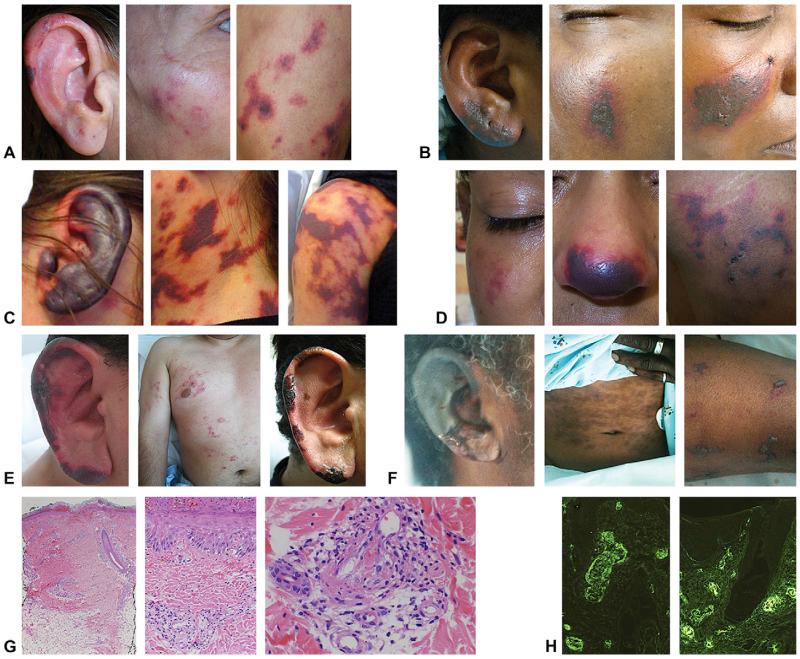
Here, we describe 6 strikingly similar patients within the last few months at two institutions in New York and California, one private and one public. All 6 patients presented with remarkably similar purpuric eruptions involving the ears, nose, cheeks, and various other anatomic locations after cocaine use (Fig 1 and Table I; available online at http://www.eblue.org). This purpura progressed to necrosis and eschar over the course of several weeks and resolved without complications. In half of the patients there was an associated neutropenia. At Harbor-UCLA Medical Center in Torrance, CA, two healthy male patients presented to the emergency department with rapidly progressive purpura of the ears after admitting to cocaine use the day prior. Both had skin biopsy specimens demonstrating leukocytoclastic vasculitis (LCV) with positive direct immunofluorescence staining suggestive of an immune complex–mediated process. At Strong Memorial Hospital at the University of Rochester Medical School, in Rochester, NY, 4 recent similar cases have been documented. Two of these patients were recently discussed in the internal medicine literature2 and we describe two additional patients from Rochester, NY, here with similar clinical findings (Table I). Although somewhat variable in clinical presentation, the features common to all patients are a characteristic tender ear purpura and a positive perinuclear ANCA serology after recent cocaine use.
Fig 1.
A, Ear, cheek, and thigh of 46-year-old woman. B, Ear, left cheek, and right cheek of 57-year-old woman. C, Ear, neck, and thigh of 46-year-old woman. D, Cheek, nose, and thigh of 22-year-old woman. E, Ear (left) and trunk (middle) of 37-year-old man on admission, and same ear resolving 1 week later (right). F, Ear, abdomen, and arm of 50-year-old man. G, Representative histopathology from ear of patient (E) showing leukocytoclastic vasculitis at 32.5 (left), ×20 (middle), and ×40 (right) magnification. H, Representative direct immuno-fluorescence of ear biopsy specimen demonstrating positive IgM (left) and positive fibrin (right) in vascular and perivascular spaces.
Table I.
Patient characteristics
| Patient | Medical history | Presentation, Tx, and outcome |
Laboratory results | Urine toxicology | Skin biopsy specimen results |
|---|---|---|---|---|---|
| A 46 y Caucasian Female |
Substance abuse | 1-mo History of purpura and necrosis on bilateral ears, cheeks, and upper and lower extremities Tx: steroids Initial improvement, lost to f/u |
Neutropenia: no P-ANCA >2500 --Positive MPO and PR3 Anticardiolipin IgM positive ANA, hepatitis, HIV negative Cryoglobulins negative |
Not performed on admission, but previously positive for cocaine and THC |
Small vessel vasculitis with intravascular thrombi |
| B 57 y African American Female |
Substance abuse, depression, anxiety, hypertension, and recurrent Staphylococcus aureus skin infections |
1-wk History of purpura and necrosis of bilateral ears and cheeks Tx: IV antibiotics, gradual improvement; neutropenia treated with filgrastim Relapse 6 mo later with same presentation, laboratory results, and positive cocaine urine test result |
Neutropenia: yes P-ANCA >2500 --Positive MPO and PR3 Anticardiolipin IgM positive ANA, SSA, SSB, dsDNA, C3, C4 negative Hepatitis, HIV negative Cryoglobulins negative |
Positive for cocaine | Intravascular thrombi |
| C 46 y Hispanic Female |
Substance abuse, hepatitis C, hypothyroidism |
Bilateral ear necrosis, diffuse retiform purpura with necrosis on neck, trunk, and extremities Tx: IV methylprednisolone Gradual improvement initially, lost to f/u |
Neutropenia: yes P-ANCA 640, C-ANCA 1280 Anticardiolipin IgM positive ANA, SSA, SSB, dsDNA, C3, C4 negative Cryoglobulins negative |
Positive for cocaine and opiates |
Multiple intravascular thrombi |
| D 22 y Hispanic Female |
Substance abuse | 3-wk History of purpura and necrosis of bilateral ears, cheeks, nasal tip, buttocks, and thighs Tx: IV methylprednisolone Skin and neutropenia improved rapidly |
Neutropenia: yes P-ANCA 2560 --Negative MPO and PR3 Anticardiolipin IgM positive ANA, SSA, SSB, dsDNA negative HIV, hepatitis negative Cryoglobulins negative |
Positive for cocaine and opiates |
Small vessel vasculitis with multiple intravascular thrombi |
| E 37 y Hispanic Male |
Substance abuse | Tender bilateral ear purpura and necrosis, diffuse retiform purpura on trunk and extremities Tx: supportive Rapid improvement of skin |
Neutropenia: no P-ANCA 640 CRP 16.2 mg/L, ESR 41 mm/h, D-dimer elevated at 3260, LDH 390 IU/L, PTT 37.7 sec, INR 1.3 ANA 1:40 HIV negative |
Positive for cocaine | Leukocytoclastic vasculitis IF: vascular deposits of IgM, with weak staining for C3, IgG, and IgA;vascular and perivascular staining for fibrin |
| F 50 y African American Male |
Substance abuse | Altered mental status;3-wk history of tender purpura and necrosis of bilateral ears; purpura and bullae over trunk and extremities Tx: antibiotics Mental status and skin improved rapidly |
Neutropenia: no P-ANCA 640 CRP 5.67 mg/L, ESR 32 mm/hr, D-dimer elevated at 548, PTT 39.6 sec ANA 1:40 HIV negative |
Positive for cocaine | Leukocytoclastic vasculitis and focal panniculitis IF: vascular deposits of IgM, IgA, C3, and weakly IgG; interstitial and vascular positive staining for fibrin |
ANA, Antinuclear antibody; C-ANCA, cytoplasmic antineutrophil cytoplasmic antibody; CRP, c-reactive protein; dsDNA, double-stranded DNA; ESR, erythrocyte sedimentation rate; f/u, follow-up; IF, immunofluorescence; INR, international normalized ratio; IV, intravenous; LDH, lactate dehydrogenase; MPO, antimyeloperoxidase antibodies; P-ANCA, perinuclear antineutrophil cytoplasmic antibody; PR3, anti-proteinase-3 antibodies; PTT, partial thromboplastin time; SSA, Sjogren Syndrome A (anti-Ro); SSB, Sjogren Syndrome B (anti-La); THC, tetrahydrocannabinol (marijuana component); Tx, treatment.
This letter will serve to alert the dermatology and broader medical community of a potential epidemic of levamisole-contaminated cocaine-induced toxicities. Because of ethical standards of research and the unreliable nature of levamisole testing, it may not be possible to establish a direct causal relationship between these symptoms and the cocaine use that preceded them. However, we believe the striking similarities of these clinical presentations and associated agranulocytosis warrants a louder national alert and additional discussion of this potential public health epidemic.
Usually, side effects of medications are anecdotal, coincidental, and observational. Such reports commonly suffer from recall bias and other types of cognitive and analytical errors. However, because of the potential harm caused by prescribed medications, the standards for reporting “assumed” causative relationships in clinical medicine must be somewhat lower than experimental science. The relationship between the symptoms described here and levamisole presents a similar conundrum as with reporting any medication-induced side effect, and warrants a justifiably cautionary response.
Cocaine contaminated with levamisole has been detected since 2003 and the incidence of toxicity caused by this contamination has been increasing rapidly since 2008.3 The reason for adulteration of cocaine is not known. Levamisole is a veterinary antihelminthic and has been used previously as an immunomodulator and cancer adjuvant. Others have hypothesized4 that because both cocaine and levamisole are known to increase dopamine in the euphoric centers of the brain, perhaps levamisole is added to enhance or prolong the psychoactive effects of cocaine. The US Department of Justice estimates that approximately 70% of cocaine in the United States may be contaminated with levamisole.5 Use of cocaine that has been adulterated with levamisole can lead to a constellation of signs and symptoms including agranulocytosis, neutropenia, and a tender, vasculitis-like purpuric skin eruption. The most common site of purpura is on the external ears and cheeks. These characteristic signs and symptoms of levamisole toxicity were first described in children being treated with levamisole.6 The purpura may progress to bullae and is generally followed by necrosis, resolving several weeks after cessation of cocaine use. Recurrent use of contaminated cocaine generally results in recurrent neutropenia and skin eruptions supporting a causal role. Concomitant symptoms of arthralgias, fever, mouth pain (gums and pharynx), mouth sores, fatigue, and dyspnea have been commonly reported in patients with agranulocytosis5 associated with cocaine use and in some patients with cocaine-associated purpura.
Both smoking and snorting contaminated cocaine has been associated with the described toxicities. Both men and women can be affected. The half-life of levamisole is 5.6 hours and only 2% to 5% of the parent drug can be found in the urine. Gas chromatography and mass spectrometry are required for detection.4 Because of these difficulties in testing and because other treatable causes of vasculitis may be present, levamisole-induced toxicity must remain a diagnosis of exclusion. Checking the urine or serum for levamisole must be performed within 48 hours and because the sensitivity is not known for this methodology, testing may not necessarily be indicated for routine clinical management. Despite the striking clinical presentation, most cases resolve without long-term sequelae. Elevated serologic markers tend to resolve after 2 to 10 months. Interventions have included broad-spectrum antibiotics for patients with fever and agranulocytosis to systemic steroids for patients with more prominent vasculitis. Although many of our patients were treated systemically, once the offending agents (cocaine and levamisole) have been discontinued, it is not known if systemic steroids are required for resolution.
Published case reports have described patients with medical histories that involve both chronic and acute infections along with signs of chronic autoimmune disease. Other patients have had absolutely no medical history. Because neutropenia is a common presenting sign of this toxicity, systemic bacterial or fungal infections caused by immunosuppression may be presenting features of levamisole-induced toxicity. These infections should be carefully considered and appropriately treated in patients who have already been given a diagnosis of levamisole-induced toxicity.
The differential diagnosis for levamisole-contaminated cocaine toxicity includes many of the same diagnoses as LCV or drug toxicities and is outlined in more detail in the prior letter by Waller et al.1 Secondary causes of LCV such as bacterial or viral infections, medication reactions, neoplasms, and autoimmune connective tissue disorders should be considered. Cryoglobulinemia, polyarteritis no-dosa, Wegener granulomatosis, and idiopathic thrombocytopenic purpura may also have similar presentations. Sometimes nonvasculitic purpura on the lower extremities may be palpable such as those seen in excessive anticoagulation with warfarin or heparin or disseminated intravascular coagulation.
A skin biopsy specimen may be helpful to rule out other diseases, but will not implicate cocaine or levamisole directly. Although skin lesions appear “vasculitic” and fibrin thrombi are commonly seen in the vessels, not all histologic features of LCV have been present in all reported cases. In the two patients at Harbor-UCLA Medical Center who had direct immunofluorescence studies performed on the skin biopsy specimens, the results supported an immune complex–mediated process (Fig 1 and Table I). Clinicians suspecting levamisole-induced toxicity should consider a urine toxicology screen to detect cocaine use, liver function tests, a complete blood cell count with differential, a routine urinalysis, renal function tests, ANCAs, antiphospholipid antibodies, lupus anticoagulants, and coagulation studies. A lumbar puncture or imaging studies can be ordered to rule out other causes of vasculitis or altered mental status if localizing symptoms are present. Consultations may be needed with critical care, infectious disease, or rheumatology. Depending on the level of cocaine abuse or the use of other addictive drugs, psychiatry may need to be consulted during withdrawal.
Although very suggestive, the use of cocaine before a characteristic purpuric eruption does not necessarily prove causation. Indeed, prior reports of cocaine-induced vasculitis may suggest cocaine itself can cause this dangerous side effect.7 Alternatively, prior reports may not have considered contamination with levamisole. Because many patients may not report cocaine use and the dose of levamisole required to induce vasculitis or agranulocytosis is not known, it is very difficult to determine the true rate of levamisole-induced toxicity in the general public at this time. It is important to identify other treatable causes of vasculitis such as infection or autoimmune disease. Because many of these patients do have positive ANCA serologies and positive lupus anticoagulant,4,6 distinguishing these conditions may require consultation with a rheumatologist. Possibly even more important is to consider levamisole-induced toxicity in the differential diagnosis in patients undergoing evaluation for presumptive autoimmune disease.
In summary, we believe our case series of 6 remarkably similar recent patients with purpuric eruptions, necrosis, and eschars of the ears after cocaine use in New York and California supports the theory posed by the University of California, San Francisco group1 that their patients’ skin problems could have been caused by levamisole-contaminated cocaine. The astute dermatologist or primary care physician should be aware of this new public health problem. They should be able to recognize the characteristic skin lesions and be wary of the potential development of agranulocytosis.
CAPSULE SUMMARY.
We describe a case series of 6 similar patients within the last few months in New York and California.
These patients presented with remarkably similar purpuric eruptions involving the ears and retiform purpura on the body after cocaine use.
All patients also had a positive perinuclear antineutrophil cytoplasmic antibody serology and half were neutropenic.
We believe these complications are caused by adulteration of cocaine with levamisole and warn clinicians to consider this diagnosis in a patient with purpura.
Acknowledgments
Funding sources: None.
Footnotes
Conflicts of interest: None declared.
Two of the 6 patients were discussed in one of the referenced articles. None of the images of these patients was published.
REFERENCES
- 1.Waller JM, Feramisco JD, Alberta-Wszolek L, McCalmont TH, Fox LP. Cocaine-associated retiform purpura and neutropenia: is levamisole the culprit? J Am Acad Dermatol. 2010;63:530–5. doi: 10.1016/j.jaad.2010.01.055. [DOI] [PubMed] [Google Scholar]
- 2.Bradford M, Rosenberg B, Moreno J, Dumyati G. Bilateral necrosis of earlobes and cheeks: another complication of cocaine contaminated with levamisole. Ann Intern Med. 2010;152:758–9. doi: 10.7326/0003-4819-152-11-201006010-00026. [DOI] [PubMed] [Google Scholar]
- 3.Knowles L, Buxton JA, Skuridina N, Achebe I, Legatt D, Fan S, et al. Levamisole tainted cocaine causing severe neutropenia in Alberta and British Columbia. Harm Reduct J. 2009;6:30. doi: 10.1186/1477-7517-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhu NY, Legatt DF, Turner AR. Agranulocytosis after consumption of cocaine adulterated with levamisole. Ann Intern Med. 2009;150:287–9. doi: 10.7326/0003-4819-150-4-200902170-00102. [DOI] [PubMed] [Google Scholar]
- 5.Czuchlewski DR, Brackney M, Ewers C, Manna J, Fekrazad MH, Martinez A, et al. Clinicopathologic features of agranulocytosis in the setting of levamisole-tainted cocaine. Am J Clin Pathol. 2010;133:466–72. doi: 10.1309/AJCPOPQNBP5THKP1. [DOI] [PubMed] [Google Scholar]
- 6.Rongioletti F, Ghio L, Ginevri F, Bleidl D, Rinaldi S, Edefonti A, et al. Purpura of the ears: a distinctive vasculopathy with circulating autoantibodies complicating long-term treatment with levamisole in children. Br J Dermatol. 1999;140:948–51. doi: 10.1046/j.1365-2133.1999.02833.x. [DOI] [PubMed] [Google Scholar]
- 7.Chen SC, Jang MY, Wang CS, Tsai KB, Chuang SH, Chen HC, et al. Cocaine-related vasculitis causing scrotal gangrene. Ann Pharmacother. 2009;43:375–8. doi: 10.1345/aph.1L487. [DOI] [PubMed] [Google Scholar]