Abstract
Management of metastatic breast cancer is critical to maximizing survival with good quality of life. Circulating tumor cell (CTC) levels in the peripheral blood hold promise for enabling improved patient care. We describe a case of a 47-year-old female with infiltrating ductal carcinoma who developed metastatic disease. Serum tumor markers were discordant with imaging studies at several time points. CTC levels were used to support decision making in light of the discordant data. The use of this tool enabled prompt changes in therapy with progressive disease and supported suspending therapy to enable recovery from treatment adverse effects when a significant response was detected by imaging and CTCs were absent from the peripheral circulation. The additional information provided by CTC enumeration helped clarify disease status and provided support for treatment decisions.
Key Words: Decision making, Circulating tumor cells, Breast cancer
Introduction
Metastatic breast cancer continues to be almost uniformly fatal; however, improvements in survival in developed countries have been documented [1]. This improvement can be attributed to better therapeutic and diagnostic tools for disease management. Yet, there is a limited array of tools for a noninvasive assessment of metastatic breast cancer, which includes imaging [computed tomography (CT) scans, bone scintigraphy, positron emission tomography (PET), and magnetic resonance imaging] and measurement of serum tumor marker concentration in the peripheral blood. Additional tools for managing metastatic breast cancer are needed. One challenge to the introduction of new clinical tools is to determine their best use in clinical decision making. In other words, facilitating the integration of clinical information from these new assessments into the clinical workflow and decision making is critical.
Circulating tumor cells (CTCs) are useful as an indicator of prognosis both initially and after therapy [2]. Multiple studies have shown that patients with ≥5 CTCs/7.5 ml of peripheral blood have a worse prognosis for survival than patients with <5/7.5 ml. The concentration of CTCs shed by solid tumors and detected in the peripheral circulation correlates with relapse and survival in multiple types of cancer [3, 4, 5, 6, 7, 8]. A system for measuring CTC concentration in peripheral blood to monitor metastatic breast, colon, and prostate cancer has been cleared by the United States Food and Drug Administration and is now commercially available for clinical use (CELLSEARCH®, Janssen Diagnostics, LLC). However, how to best integrate this new information on disease status with existing measurements of disease prognosis and progression in clinical decision making remains empiric. Here we present a case of metastatic breast cancer in which CTC information was used to help resolve discrepancies between more conventional assessments to improve patient care.
Case Presentation
The patient was a 47-year-old Caucasian female. She was diagnosed with infiltrating ductal carcinoma of the right breast in 1994. The tumor was staged as T1N0M0. Pathology demonstrated estrogen-receptor-positive and progesterone-receptor-positive disease. At that time, she was treated with breast-conserving surgery, followed by radiation therapy. The patient refused adjuvant tamoxifen therapy.
In March 1998, the patient was diagnosed with distant recurrence of her disease localized to the right femur. She was treated with radiation therapy, followed by paclitaxel and doxorubicin. After an initial response, the chemotherapy was discontinued and the patient was placed on maintenance letrozole and pamidronate.
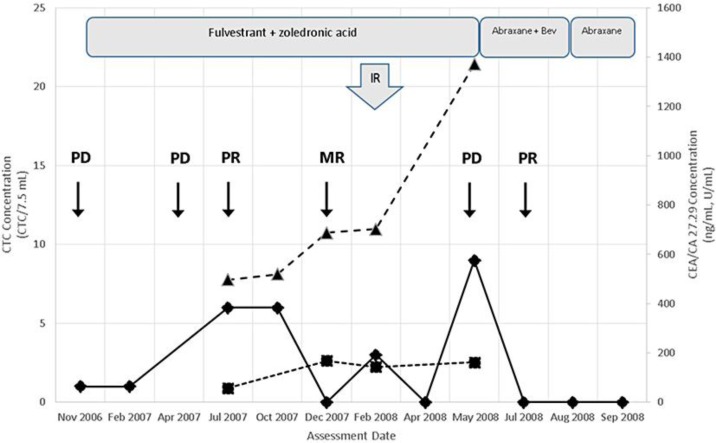
The patient was diagnosed with progressive disease based on imaging done in November 2006. Her therapy was switched to fulvestrant plus zoledronic acid based on the imaging study (table 1). An initial CTC measurement using the CELLSEARCH® System resulted in a determination of 1/7.5 ml (fig. 1). A repeat CTC measurement in February 2007 again returned a value of 1/7.5 ml.
Table 1.
Summary of assessments and clinical decisions
| Time frame | Clinical decision | Assessments | Commentary |
|---|---|---|---|
| November 2006 | Therapy switch to fulvestrant plus zoledronic acid | Imaging – PD | – Decision to switch therapy based on imaging that showed PD in November 2006 |
| [CTC] – low | |||
| July 2007 | Continuation of fulvestrant plus zoledronic acid treatment | Imaging – PR | – Marginal [CTC] agreed with good performance status |
| Clinical – performance status: good | |||
| [CTC] – marginal | – Continued fulvestrant plus zoledronic acid therapy | ||
| [CEA] – elevated, stable | |||
| [CA 27.29] – elevated, stable | – Imaging showed equivocal response | ||
| December 2007 | Continuation of fulvestrant plus zoledronic acid treatment | Imaging – MR | – Imaging response, performance status, and absence of CTCs indicate good prognosis |
| Clinical – performance status: good | |||
| [CTC] – absent | |||
| [CEA] – elevated, stable | – Continued treatment | ||
| [CA 27.29] – elevated | |||
| February 2008 | Continuation of fulvestrant plus zoledronic acid treatment | Clinical – performance status: reporting increasing pain | – Clinical symptoms and increased [CTC] suggest progression |
| [CTC] – low | |||
| [CEA] – elevated, stable | – Treated with radiation | ||
| [CA 27.29] – increasing | |||
| May 2008 | Therapy switch to Abraxane plus bevacizumab | Imaging – PD | – All assessments suggesting progression |
| [CTC] – elevated | |||
| [CEA] – elevated | – Therapy switched to Abraxane plus bevacizumab | ||
| [CA 27.29] – elevated | |||
| August 2008 | Discontinue bevacizumab | Clinical – ulceration on foot | – Stably absent CTCs agree with prior PR on imaging |
| [CTC] – absent | |||
| – Bevacizumab discontinued to address treatment-related AEs | |||
| September 2008 | Discontinue Abraxane | Clinical – neuropathy | – Continued absence of CTCs |
| [CTC] – stably absent | – Drug holiday to address treatment-related AEs | ||
PD = Progressive disease; PR = partial response; MR = mixed response; [CTC] = CTC concentration; [CEA] = CEA concentration; [CA 27.29] = CA 27.29 concentration; AE = adverse effect.
Fig. 1.
Integrated display of therapy and assessments performed. The various assessments used in managing this case are displayed. Each symbol represents an assessment: ▴ = CTC count; ▴ = CA 27.29 determination; ▪ = CEA determinations. The time point of each PET/CT imaging assessment is shown as a two-letter code with an arrow below: PD = progressive disease; PR = partial response; MR = mixed response. Boxes representing the duration of each treatment are shown across the top of the graph with the name of the therapeutic regimen. The arrow labeled IR indicates the time frame when radiation treatment was given. Bev = Bevacizumab.
In April 2007, PET/CT imaging revealed metastatic deposits in the liver and bone, suggesting progressive disease; however, based on the low CTC count in February the decision was made to not change treatment. Repeat imaging in July 2007 showed a partial response (PR) in the liver and bone lesions (fig. 1). Thus, although the patient's CTC count had risen to 6/7.5 ml and initial tumor marker measurements were elevated (497 U/ml for CA 27.29 and 58 ng/ml for CEA), therapy with fulvestrant plus zoledronic acid was continued based on a lack of changes in imaging studies and continued good performance status (table 1).
In October 2007, the patient's CTC count remained at 6/7.5 ml, while her CA 27.29 had risen to 520 U/ml. In December 2007, the CTC count had declined to 0 and tumor marker levels were stable. PET/CT imaging demonstrated improvement in the liver lesions and a mixed response in the bone lesions (fig. 1).
The following month, the patient experienced increasing lower back pain. Radiation therapy was given to the metastatic sites identified as active by increased standardized uptake values from the PET/CT imaging in December 2007. The following February, CTC levels remained below 5/7.5 ml and tumor markers were elevated and stable. CTCs were absent from the patient's peripheral blood in a measurement in April 2008.
In May 2008, PET/CT imaging revealed progressive disease, both in the liver and bone. Her CTC level had risen from 0 in April to 9/7.5 ml, and CA 27.29 had risen to 1,371 U/ml, confirming progressive disease (fig. 1). The CEA level was up slightly from February. Biopsy of the liver lesions confirmed progressive metastatic breast cancer. The patient's therapy was switched to Abraxane® plus bevacizumab (table 1).
In July 2008, after two rounds of chemotherapy with the new agents, her CTC level had again dropped to 0. Repeat PET/CT imaging at the end of July confirmed a PR to therapy. Over the summer, the patient experienced significant bevacizumab toxicity. Based on the positive response observed with imaging and CTC levels, the decision was made to discontinue treatment with the bevacizumab component of her treatment regimen. Her CTC level remained at 0 upon repeat measurement in September 2008. Based on PR on imaging and negative CTC counts, in September the decision was made to discontinue all chemotherapy due to progressive toxicity experienced by the patient, including new onset neuropathy (table 1).
Discussion
Assessment of tumor activity in this case was difficult using conventional tumor markers and PET/CT imaging due to a lack of concordance between these assessments, which ordinarily would diminish confidence in treatment decisions. The use of CTC enumeration information to support clinical decision making in a setting of conflicting assessments has been suggested previously [9]. The specificity and responsiveness of the serum tumor markers, CEA and CA 27.29, are reported to be fairly low [10]. Radiographic assessment may have interreader variability and may not reflect changes in disease status in a timely manner [11]. CTC concentration has been reported to be specific for cancer and to respond to changes in disease state promptly [11, 12] and so may compliment other assessments.
The initial response of CTC counts to therapy was complex. In the months after the initiation of fulvestrant plus pamidronic acid therapy in November 2006, the patient's CTC count rose to 6/7.5 ml, then stabilized. Although the CTC count had risen, imaging studies showed response to treatment and the patient's performance status was good, so therapy was continued. By December 2007, the CTC count had reached 0, which brought it into agreement with the PET/CT imaging studies. In contrast, the serum tumor markers remained elevated. Based on the imaging studies in July and December showing response to therapy and the absence of CTCs, the decision was made to continue therapy with fulvestrant and pamidronic acid. In this example, CTCs may have been more reflective of disease state than the serum tumor markers.
At the May 2008 visit, both CTC and CA 27.29 levels were elevated, which supported imaging results that suggested progressive disease. CEA concentration was unchanged. This was an unusual instance, where all assessments were in agreement. The decision was made to start a new line of therapy with Abraxane plus bevacizumab. The patient responded to this change in therapy as assessed by CTC concentration in July 2008, which decreased to 0. The response was confirmed by imaging, which showed a PR.
Although CTC count often responds to changes in disease state fairly quickly, in some instances, changes may not be seen in the first measurement [unpubl. observations, 2]. In this case, the CTC count increased in the first half of 2007 following initiation of fulvestrant plus zoledronic acid therapy, while imaging suggested a PR. The CTC count stabilized at 6/7.5 ml from the July and October measurements, then decreased by the third measurement in December 2007. In our experience, CTC count responses following hormonal therapy in breast cancer may require 3–4 months or more to show a significant change. In contrast, the decrease in CTC concentration observed in the first measurement following change in therapy to Abraxane plus bevacizumab in July 2008 closely tracked the PR determined by imaging, which is typical in our experience for response of CTC counts to chemotherapy. Despite the differences in time to response, in both of these examples from this case the CTC count was ultimately concordant with imaging.
The specificity of CTCs for breast cancer [13] was important in considering the use of CTC enumeration information in this case. The patient experienced adverse effects attributed to bevacizumab [14] in the summer of 2008, and the decision to discontinue bevacizumab was supported by the favorable imaging results and negative CTC levels following the change in therapy. Subsequent negative tests for CTCs in July 2008 and September 2008 gave us additional confidence that a discontinuation of paclitaxel therapy could be allowed so that the patient could recover from its adverse effects, using CTC tests as an option to monitor for disease progression. The use of CTC information in this context is consistent with recommendations to limit the use of imaging to monitor for cancer recurrence [15].
Management of metastatic breast cancer is challenging under any circumstances. This case illustrates how CTC assessments can corroborate imaging and clinical data. In addition, the type of therapy may influence the time to see a CTC response in breast cancer, with hormonal therapy often taking longer than chemotherapy. Finally, in this instance, we found CTC measurement a useful adjunct to imaging for monitoring for disease recurrence to give the patient a needed drug holiday.
Disclosure Statement
T.M. has received research funding from Janssen Diagnostics, LLC. The Jon Block Group is a paid consultant for Janssen Diagnostics, LLC.
References
- 1.SEER cancer statistics review, 1975–2009 (vintage 2009 populations). 2012. http://seer.cancer.gov/csr/1975_2009_pops09/ (accessed September 11, 2012).
- 2.Alemar J, Schuur ER. Progress in using circulating tumor cell information to improve metastatic breast cancer therapy. J Oncol. 2013;2013:702732. doi: 10.1155/2013/702732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen SJ, Punt CJ, Iannotti N, Saidman BH, Sabbath KD, Gabrail NY, Picus J, Morse M, Mitchell E, Miller MC, Doyle GV, Tissing H, Terstappen LW, Meropol NJ. Relationship of circulating tumor cells to tumor response, progression-free survival, and overall survival in patients with metastatic colorectal cancer. J Clin Oncol. 2008;26:3213–3221. doi: 10.1200/JCO.2007.15.8923. [DOI] [PubMed] [Google Scholar]
- 4.Cristofanilli M, Budd GT, Ellis MJ, Stopeck A, Matera J, Miller MC, Reuben JM, Doyle GV, Allard WJ, Terstappen LW, Hayes DF. Circulating tumor cells, disease progression, and survival in metastatic breast cancer. New Engl J Med. 2004;351:781–791. doi: 10.1056/NEJMoa040766. [DOI] [PubMed] [Google Scholar]
- 5.Danila DC, Heller G, Gignac GA, Gonzalez-Espinoza R, Anand A, Tanaka E, Lilja H, Schwartz L, Larson S, Fleisher M, Scher HI. Circulating tumor cell number and prognosis in progressive castration-resistant prostate cancer. Clin Cancer Res. 2007;13:7053–7058. doi: 10.1158/1078-0432.CCR-07-1506. [DOI] [PubMed] [Google Scholar]
- 6.Krebs MG, Sloane R, Priest L, Lancashire L, Hou JM, Greystoke A, Ward TH, Ferraldeschi R, Hughes A, Clack G, Ranson M, Dive C, Blackhall FH. Evaluation and prognostic significance of circulating tumor cells in patients with non-small-cell lung cancer. J Clin Oncol. 2011;29:1556–1563. doi: 10.1200/JCO.2010.28.7045. [DOI] [PubMed] [Google Scholar]
- 7.Poveda A, Kaye SB, Mccormack R, Wang S, Parekh T, Ricci D, Lebedinsky CA, Tercero JC, Zintl P, Monk BJ. Circulating tumor cells predict progression free survival and overall survival in patients with relapsed/recurrent advanced ovarian cancer. Gynecol Oncol. 2011;122:567–572. doi: 10.1016/j.ygyno.2011.05.028. [DOI] [PubMed] [Google Scholar]
- 8.Sergeant G, Van Eijsden R, Roskams T, Van Duppen V, Topal B. Pancreatic cancer circulating tumour cells express a cell motility gene signature that predicts survival after surgery. BMC Cancer. 2012;12:527. doi: 10.1186/1471-2407-12-527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hayes DF, Smerage J. Is there a role for circulating tumor cells in the management of breast cancer? Clin Cancer Res. 2008;14:3646–3650. doi: 10.1158/1078-0432.CCR-07-4481. [DOI] [PubMed] [Google Scholar]
- 10.Harris L, Fritsche H, Mennel R, Norton L, Ravdin P, Taube S, Somerfield MR, Hayes DF, Bast RC, Jr, American Society of Clinical Oncology American Society of Clinical Oncology 2007 update of recommendations for the use of tumor markers in breast cancer. J Clin Oncol. 2007;25:5287–5312. doi: 10.1200/JCO.2007.14.2364. [DOI] [PubMed] [Google Scholar]
- 11.Budd GT, Cristofanilli M, Ellis MJ, Stopeck A, Borden E, Miller MC, Matera J, Repollet M, Doyle GV, Terstappen LW, Hayes DF. Circulating tumor cells versus imaging – predicting overall survival in metastatic breast cancer. Clin Cancer Res. 2006;12:6403–6409. doi: 10.1158/1078-0432.CCR-05-1769. [DOI] [PubMed] [Google Scholar]
- 12.Beveridge R. Circulating tumor cells in the management of metastatic breast cancer patients. Community Oncol. 2007;4:79–82. [Google Scholar]
- 13.Allard WJ, Matera J, Miller MC, Repollet M, Connelly MC, Rao C, Tibbe AG, Uhr JW, Terstappen LW. Tumor cells circulate in the peripheral blood of all major carcinomas but not in healthy subjects or patients with nonmalignant diseases. Clin Cancer Res. 2004;10:6897–6904. doi: 10.1158/1078-0432.CCR-04-0378. [DOI] [PubMed] [Google Scholar]
- 14.Kamba T, McDonald DM. Mechanisms of adverse effects of anti-VEGF therapy for cancer. Br J Cancer. 2007;96:1788–1795. doi: 10.1038/sj.bjc.6603813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schnipper LE, Lyman GH, Blayney DW, Hoverman JR, Raghavan D, Wollins DS, Schilsky RL. American Society of Clinical Oncology 2013 top five list in oncology. J Clin Oncol. 2013;31:4362–4370. doi: 10.1200/JCO.2013.53.3943. [DOI] [PubMed] [Google Scholar]