Abstract
Context:
Acute febrile illnesses are common in athletes over the course of training and competition seasons. Complete recovery and rapid yet safe return to participation are critical for competitive athletes. Alterations in thermoregulation, metabolism, fluid homeostasis, muscle strength, and endurance, as well as potential complications for the athlete and others, must be considered.
Evidence Acquisition:
The PubMed database was searched (1970-2013) for all English-language articles related to febrile illness in sport, using the keywords fever, febrile, body temperature, thermoregulation, infection, illness, disease, exercise, athlete, sport, performance, return to play, metabolism, hydration, and dehydration.
Study Design:
Clinical review.
Level of Evidence:
Level 4.
Results:
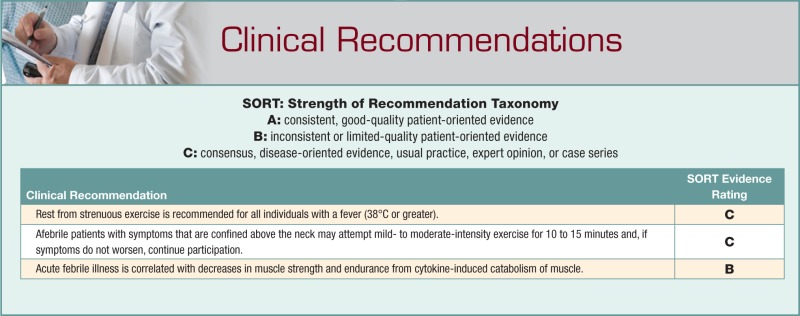
Limited data confirm that febrile illness is correlated with alterations in the body’s thermoregulatory system, with increases in metabolic rate, and with effects in fluid homeostasis. Human and animal studies demonstrate a decrease in muscle strength and endurance secondary to muscle catabolism in febrile illness. However, indirect evidence suggests that regular exercise enhances the immune response. No strong clinical research has been published on return to play during or following acute febrile illness, excluding mononucleosis and myocarditis.
Conclusion:
Fever is correlated with an increase in insensible fluid losses, dehydration, metabolic demands, and dysregulation of body temperature. Fever can have detrimental effects on the musculoskeletal system, including decreasing strength and endurance, generalized muscle catabolism, and increase in perceived fatigue. Participating in strenuous exercise during febrile illness can worsen the illness and has demonstrated increased lethality in animal models. No consensus recommendations support return to activity before resolution of fever, and training should be resumed gradually once fever and dehydration have resolved.
Keywords: fever, infection, illness, exercise, athlete, sport
Fever is part of a normal physiologic response to an immune stimulus or illness, aimed at facilitating host survival and shortening the duration of the disease.7,51,54 Infectious organisms, tissue trauma, medications, and blood products are all triggers for the body to produce a febrile response.4 The amplitude of febrile response depends on the number of circulating cytokines and prostaglandins, combined with the body’s naturally occurring antipyretic molecules.7 Sources differ on what is considered normal body temperature. Critical analysis suggests that the normal body temperature in young adults averages 98.2°F ± 0.7°F, with a nadir approximately 3 hours before waking and a peak 12 to 14 hours after waking.4,32,41
Body temperature varies based on the site of measurement and endogenous factors, including circadian, menstrual, and biological rhythms; fitness and activity levels; and aging.32 A study of circadian rhythms in active and sedentary individuals found that daily amplitudes of oral temperatures were higher in physically active individuals.2 Temperature variability is also affected by external factors, including the environment, diet, lifestyle, and disease states.32 Although an internal temperature (most easily obtained via rectal temperature) is preferred and considered the gold standard, it can be the least convenient and, therefore, the least often obtained. Sund-Levander et al correlated normal temperature means and ranges taken at various sites (Table 1).53 Fever is defined by the Centers for Disease Control and Prevention at an internal temperature >38.0°C.9 Clinically, body temperature can vary by measurement site, and the following are accepted values for fever based on site: rectal temperature ≥100.4°F (38.0°C), oral temperature >100°F (37.8°C), axillary temperature >99°F (37.2°C), tympanic temperature >100.4°F (38.0°C), and forehead/temporal temperature >100.4°F (38.0°C). A rectal temperature >104°F (40.0°C) is considered hyperpyrexia.34
Table 1.
Normal body temperature means (ranges)53
| Oral | Rectal | Tympanic | Axillary | |
|---|---|---|---|---|
| Men | ||||
| °F | 98.0 (96.3-99.9) | 98.6 (98.1-99.5) | 97.7 (95.9-99.5) | 97.3 (95.9-98.6) |
| °C | 36.7 (35.7-37.7) | 37.0 (36.7-37.5) | 36.5 (35.5-37.5) | 36.3 (35.5-37.0) |
| Women | ||||
| °F | 97.2 (91.7-100.6) | 98.6 (98.2-98.8) | 97.9 (96.3-99.5) | |
| °C | 36.2 (33.2-38.1) | 37.0 (36.8-37.1) | 37.0 (36.8-37.1) |
Although there is no direct evidence, fever assists the immune system with mounting a response and therefore facilitating recovery. There is, however, indirect evidence that supports the belief that fever enhances the body’s immunologic response, improves the ability to destroy microorganisms by inhibiting their replication, aids in decreasing blood glucose levels and thereby denying bacteria necessary substrate, causes increased production of acute-phase reactants by the liver, and assists in activating the body’s stress response.4,13,35
Effects of Exercise on the Immune System
During exercise, the body undergoes many physiologic changes, including those to the immune system. Limited data suggest that heavy or strenuous exercise has an overall negative effect on the immune system, increasing the risk of infection, while regular mild-moderate exercise can protect against infection and reduce symptoms and the risk of chronic disease.20,44 The relationship between exercise and susceptibility to infection is often compared with a J-shaped curve, where moderate exercise enhances immunity above sedentary levels but prolonged, intense activity impairs immune function.20,23 The immune response to exercise depends on many factors, including duration, intensity, type of exercise, hormone and cytokine concentrations, body temperature changes, hydration, and blood flow.44
Negative effects on the immune system from exercise are associated with high-intensity exercise, defined as 70% to 80% of the maximal heart rate for 5 to 60 minutes, and with prolonged exercise, lasting longer than 60 minutes.6,23 Intense exercise impairs cell-mediated immunity by decreasing T-cell proliferation, thereby potentially increasing risk of viral infection.20 When the athlete’s increasing oxygen requirement causes one to shift from nose to mouth breathing, he or she is bypassing barriers that are part of the innate immune system, allowing more foreign particles to be deposited in the airways.3,23 Secretory IgA is produced as part of the acquired immune system to provide frontline defense against new pathogens.33 After intense and prolonged exercise, flow rates of secretory IgA fall as much as 50% to 65%.40 Sixty-eight percent of runners in ultramarathon races presented with upper respiratory infection symptoms up to 2 weeks following the events.46 There is also a reported 100% to 500% increased risk of contracting an infection for several weeks following an endurance running event, though other recent studies have failed to confirm these findings.20,46 A suppression of NK cell counts and neutrophil phagocytic function following short bouts of intense training may correlate with these increased rates of upper respiratory infections sometimes found during endurance training.31 Other aspects of the immune system, including both humoral and cell-mediated responses, have temporary depressions following acute bouts of exercise.23 This short-term immunosuppression is referred to as an “open window” during which there is increased risk of infection.23,31 Hormonal changes are also seen in response to exercise, including increases in adrenaline, cortisol, prolactin, and growth hormone—all known to have immunomodulatory effects impairing cellular immunity.20,23
Beneficial effects of regular mild-moderate short bouts of physical exercise include increases in circulating leukocytes (specifically, neutrophils and lymphocytes) that can persist for several hours following exercise.20,31,47 Moderate exercise is defined as exercise at 40% to 60% of maximal heart rate for 5 to 60 minutes.23 Though salivary IgA levels were found to decrease during prolonged and intense exercise, regular moderate exercise resulted in increased levels, contributing to decreased risk of infection.33 Up to 61% of runners reported fewer upper respiratory infections after starting a running exercise program, and the incidence of upper respiratory infections was decreased 20% to 30% in moderate exercisers compared with sedentary individuals.23,43 Muscle-derived IL-6 appears to have protective effects against chronic diseases.20 IL-6 directly stimulates type 2 T-cell cytokine production, which itself suppresses the immune system’s ability to induce tissue damage and inflammation. IL-6 also suppresses TNF-alpha, which acts as a potent activator of inflammation.20,52 Since cardiovascular and metabolic diseases are strongly associated with blood markers for inflammation, exercise-induced elevation of IL-6 levels should help mediate anti-inflammatory activity, providing some protective effects against development of these chronic diseases.20,52
Effects of Fever on Physiology and Performance
Thermoregulation, Metabolism, and Fluid Homeostasis
Fever has many ill effects on the body, including an increase in insensible fluid losses, dehydration, metabolic demands, and dysregulation of body temperature.47 Fever is the result of endogenous or exogenous pyrogens that reset the hypothalamic set point, resulting in an elevation of body temperature.7 In contrast to fever, hyperthermia is defined as an elevation of body temperature secondary to heat production, exceeding the body’s ability to effectively dissipate heat.4 Normal body processes that cool the body during times of heat stress, such as vasodilation and sweating, are not active during times of fever.4,7
Fever is a multistep adaptive response to a variety of conditions, with the most common being infection.7 This adaptive response is initiated by pyrogens that can be either endogenous or exogenous. Exogenous pyrogens include bacterial toxins, viral pathogens, bacterial cell wall components, and antigen-antibody complexes.7 The exogenous pyrogens bind to macrophages and induce the release of endogenous pyrogens, including interleukins, interferons, and other cytokines, which then stimulate the production of prostaglandin E2. These molecules bind to the preoptic region of the hypothalamus and increase the body temperature “set point.”4,7 Thermoregulatory control maintains this increased set point temperature until the initiating threat or exogenous stimulus has resolved.54 During a febrile state, the body temperature rarely exceeds 40°C.7 Fever is a self-limiting process that is kept in check by negative feedback of naturally occurring antipyretic hormones produced by the body, including ADH, alpha-melanocyte stimulating hormone, and corticotrophin-releasing factor.7
Fever, as part of the acute phase response, involves endocrine, metabolic, behavioral, and autonomic systems.54 Increased production of adrenaline occurs, which increases metabolic rate, heart rate, and muscle tone. There is approximately a 10% increase in metabolic rate for every 1°C increase in body temperature.7 Adrenaline continues to aid in increasing body temperature by stimulating glycolysis and causing peripheral vasoconstriction.7 The immune system also creates a hostile environment for pathogens by decreasing the amount of free glucose available in the circulation and shifting to lipolysis- and proteolysis-based metabolism.7 Further aiding in elevating the body temperature is increased peripheral vascular resistance, which shunts blood away from the peripheral capillary beds, leading to decreased heat loss through conduction, radiation, convection, and evaporative means.4,7 These decreases in free glucose and peripheral blood flow, while helping the immune system, also decrease essential nutrients necessary for working muscles.7
The production of antidiuretic hormone is reduced with fever, which can potentiate dehydration.4,7 During hyperthermia, mammals attempt to regulate body temperature by means of evaporative cooling. If they are also severely dehydrated, their body decreases or inhibits these means of cooling, saving water at the expense of higher body temperatures.30 Selective brain cooling of the hypothalamus inhibits evaporative heat loss, therefore conserving body water and helping to balance the body’s thermoregulatory and osmoregulatory needs.19 In addition, daily body temperatures were found to be significantly higher in animals that were dehydrated.19 In human subjects, the combination of hyperthermia and dehydration during exercise caused greater reductions in cardiac output and blood pressure than either variable alone.22 Hypohydration can increase heat storage and decrease the ability to tolerate heat stress.49 Therefore, if athletes exercise while they have a fever, their bodies’ natural temperature-regulating mechanisms are altered and could result in potentially harmful increases in total body temperature, especially if the febrile illness also caused some degree of dehydration.
Musculoskeletal System
In addition to the increase in insensible fluid loss and dysregulation of body temperature, fever is correlated with a reduction in exercise tolerance, decreased endurance and muscle strength, and an increase in perceived fatigue.47 Decreases in isometric muscle strength and endurance were found approximately 3 or 4 days after inoculation with sandfly fever virus when compared with healthy controls.1 After this time, performances in strength and endurance started improving toward baseline.1
Decreases in strength can be attributed to generalized muscle catabolism induced during infection and fever. Blood lactate levels are increased by as much as 17% during exercise after infection and could take up to 50 weeks before returning to normal levels.28 As a result of mobilizing nutrients required for an immune response, the body undergoes a cytokine-induced general catabolism of muscle protein involving skeletal and cardiac muscle.16,17 Loss of muscle strength and endurance from baseline shortly after acute febrile illness correlates with this cytokine-induced muscle protein loss.17 The effects include wasting of striated muscle and degradation of performance-related metabolic enzymes.16 Muscle protein loss is gradually replenished once the infection has resolved, though complete recovery may take several weeks to months following a weeklong febrile infection.16,17
The magnitude of these effects is related to the extent and duration of the acute phase response, although there seems to be some protective effects in conditioned individuals compared with unconditioned individuals.16,17 Preconditioned animals (infected mice) had less catabolism of cardiac muscle when inoculated with viral or bacterial infections and had reduced lethality when infected with an influenza strain.27 Additionally, degradation of total myocardial protein content was reduced 17% by preconditioning and confirmed a 25% reduction in lethality in those with influenza in the preconditioned group.27 Patients (n = 18) that performed a mild physical activity program consisting of getting out of bed every half hour during waking hours during a febrile course found that they did not experience the orthostatic declines or blood volume reductions normally induced by illness and bed rest.26 In addition, they experienced smaller declines in aerobic capacity compared with those undergoing strict bed rest.26 These studies suggest that to hasten recovery, bed rest should be limited, if possible, during periods of illness.
Several studies also looked at the effects of infection on muscle strength and endurance compared with the effects of bed rest. After a weeklong uncomplicated febrile illness of primarily viral or mycoplasma cause, isometric muscle strength was decreased 5% to 15% compared with baseline, compared with <4% for healthy controls when confined to bed rest for the same period.15 A similar study showed a 13% to 18% reduction in endurance capacity in those suffering from acute infectious disease requiring bed rest, while no reduction of endurance capacity was observed in healthy controls undergoing only bed rest.14 Therefore, deteriorations observed in strength and endurance following a weeklong febrile illness requiring bed rest can be almost entirely attributed to effects of infection and cytokine-induced catabolism of muscle.14,15 These effects were seen for up to 4 months following resolution of fever.14,15
Muscular impairments noted early in infection may correlate more closely with perceived symptoms than actual alterations in muscle structure caused by fever.18 On the first day of fever, subjects inoculated with sandfly fever virus demonstrated a decrease in isometric and isotonic muscle strength of up to 30%, though muscle biopsies showed that no significant muscle breakdown or alterations in muscle enzymes had yet occurred.18 There was a strong correlation between decreased strength and perceived myalgias, as graded by each participant.18
In addition to seeing decreases in skeletal muscle strength and endurance, we would expect to see changes in the body’s circulatory function.17 Stroke volume increases 23% to 27% after resolution of fever compared with that during fever.24 During a brief febrile viral illness, stroke volume is lower during and after fever compared with baseline.18 An increased heart rate helped to maintain cardiac output at normal values, though cardiac output fell during early convalescence, and this decline was strongly associated with the severity of the fever.18
Decreases in speed and coordination are observed during and shortly after periods of brief febrile illness.1 These decreases in motor skills are seen as early as 3 or 4 days into acute illness.1 Impairment in precision and coordination can be detrimental, especially in certain sports, and may increase risk of additional injuries, including ankle sprains and dislocations.17
Potential Dangers of Participating With Fever
Worsening of Illness
Studies on animals show that strenuous exercise during an ongoing febrile infection can be hazardous, causing complications and increased lethality.17 For conditioned individuals, exhaustive exercise during the acute phase of febrile illness can counteract potential benefits to cardiac muscle.27 Studies on mice have consistently demonstrated detrimental effects from strenuous exercise during an ongoing acute infection. Exercise during the acute phase of illness increased lethality for mice infected with influenza and provoked or aggravated myocarditis in those with coxsackievirus.27,37 Furthermore, strenuous exercise during acute bacterial infection with tularemia counteracted the benefits of preconditioning but had no influence on lethality or bacterial cell counts.27
Transmission of Disease to Others
The close proximity of athletes during sporting events increases the opportunity for the spread of infectious diseases. In particular, mass sporting events bring the potential of increased risk for spread of infections and necessitate enhanced surveillance for infectious diseases.56 A multistate measles outbreak in 2007 was associated with an imported case from Japan that occurred in an international youth sporting event in Pennsylvania.12 In addition to direct person-to-person spread of disease, it is important to remember that other factors, such as poor food preparation and contaminated water sources, may cause acute febrile illness, especially when these events last longer than just 1 day.56 Examples include outbreaks of leptospirosis that occurred during the 2000 Eco-Challenge multisport race held in Malaysia,11 among athletes participating in multiple triathlons across the United States in 1998,8,10 and in triathlon participants in Germany in 20065 and in Austria in 2010.48 Outbreaks have also been associated with public swimming pools, such as an outbreak of viral meningitis in Germany during the summer of 2001 and an outbreak of pharyngoconjunctivitis caused by adenovirus during a swim meet in southern Greece in July 1995.25,45 Despite these occurrences, a review of multiple large international sporting events did not show an increased incidence of illness.56 A large 2004 European football tournament review found similar results.21 Of the communicable diseases reported during the event, no visitors were affected, and Portugal’s residents were not influenced.21
Respiratory viruses are easily spread among groups of people, but with some simple precautions, their spread can be stopped or at least significantly reduced. A systematic review of the effectiveness of physical interventions at reducing the spread of respiratory viruses found that frequent handwashing, >10 times per day, was effective 55% of the time in interrupting virus spread.29 Other interventions reviewed included thorough disinfection (70% effective), wearing gloves (57% effective), wearing gowns (77% effective), and wearing masks and N95 masks (68% and 91% effective, respectively); the combination of handwashing, masks, gowns, and gloves was 91% effective.29 Although these are not always feasible for mass-participation sporting events, some of the techniques may be utilized in smaller settings, such as that among team members of an infected athlete, and good handwashing should always be emphasized.
Prevention of infectious disease in athletes is a challenge that sports medicine physicians must face, along with appropriate treatment of sick athletes and necessary precautions to contain the spread of disease.39 It is imperative to know what diseases are prevalent in different regions of the world during the different seasons and which ones can and should be immunized against or given prophylaxis.39 In addition, improving personal hygiene, especially hand hygiene, can help reduce spread by direct contact, and other necessary precautions can be taken to decrease spread of insect-borne disease and sexually transmitted diseases.39 Knowledge of incubation periods of specific respiratory viruses and periods of infectivity can be useful in helping to prevent the spread of illness (Table 2).
Table 2.
Incubation period in days for acute respiratory viral infections38
| Virus | Days |
|---|---|
| Adenovirus | 5.6 |
| Human coronavirus | 3.2 |
| Severe acute respiratory syndrome coronavirus | 4.0 |
| Influenza A | 1.4 |
| Influenza B | 0.6 |
| Measles | 12.5 |
| Parainfluenza | 2.6 |
| Respiratory syncytial virus (RSV) | 4.4 |
| Rhinovirus | 1.9 |
Return to Play
There are multiple expert opinion–based guidelines for length of rest for an athlete before returning to participation, and some are illness specific; however, each return-to-play decision must be tailored to the case and circumstance. Rest from participation is consistently recommended for individuals with fever (38°C or greater) and for symptomatic individuals with an increased resting temperature (0.5-1°C above normal) and elevated pulse (10 beats per minute above baseline).17 A conservative approach suggests that people with an acute onset of general malaise, even when accompanied by normal body temperature, should be advised to rest until symptoms resolve.17 Guidelines regarding continued physical activity during upper respiratory tract infections can be made using a “neck check.”23,47 These guidelines suggest that if symptoms are confined to those above the neck (runny nose, sore throat, congestion), the recommendation should be mild to moderate intensity exercise for 10 to 15 minutes and, if symptoms do not worsen, continued participation.23,47 In cases of febrile infections with systemic symptoms, recommendations range from resumption of training as soon as fever has resolved to waiting 7 to 14 days after resolution of symptoms to resume physical activity.17,47 Athletes returning to activity after gastroenteritis should return to participation following resolution of symptoms and dehydration.23 It is the general consensus that all training should be resumed gradually.17,23,47
Special consideration should be taken for athletes with infectious mononucleosis and myocarditis. Because of concerns for splenic rupture in individuals with acute mononucleosis, athletes should be held from all physical activity until 3 weeks from the onset of symptoms.23,47 After 3 weeks, athletes may resume training gradually as long as symptoms have resolved, there are no other complications, laboratory markers have normalized, and, if present, splenomegaly has resolved.47 Although less common than mononucleosis, myocarditis is a potentially severe complication of an acute viral illness frequently caused by adenoviruses, parvovirus B19, and human herpes virus 6.23,42 A postinfection immune response may lead to inflammation of the myocardium and associated myocardial necrosis.36 Though the majority of episodes are subclinical and the patient experiences no cardiac symptoms, complications of myocarditis can include ventricular dysfunction, dilated cardiomyopathy, arrhythmias, and sudden death.17,36,50 Myocarditis patients should avoid all strenuous activity for 6 months after symptoms begin and then may return to exercise slowly if electrocardiogram and echocardiogram results are normal, no arrhythmias are present, and there is no serum evidence of inflammation or heart failure.23,50,55
Conclusion
Fever is a multistep adaptive response to a variety of conditions, with the most common being infection.7 Evidence suggests that exercise can have both beneficial and negative effects on the immune system, depending greatly on the duration and intensity of physical activity involved.20,44 Heavy or strenuous exercise has a short-term negative effect on the immune system, increasing the risk of acute infection, while regular mild-moderate exercise can be protective against infection and may reduce symptoms and risk of chronic disease.20,44 Fever is correlated with an increase in metabolic demands and insensible fluid losses, dehydration, and dysregulation of body temperature.47 Though less studied in humans, fever can have detrimental effects on the musculoskeletal system, including decreasing strength and endurance, generalized muscle catabolism, and an increase in perceived fatigue.47 Limited research in animal models demonstrates that participating in strenuous exercise during a febrile illness can worsen illness and have increased lethality.17 Limited data exist to guide return to play for most febrile illnesses, but multiple return-to-play guidelines are published.17,23,47 No consensus recommendations support return to activity before resolution of fever, and training should be resumed gradually once fever and dehydration have resolved.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this manuscript.
References
- 1. Alluisi EA, Beisel WR, Caldwell LS. Effects of sandfly fever on isometric muscular strength, endurance, and recovery. J Mot Behav. 1980;12:1-11 [DOI] [PubMed] [Google Scholar]
- 2. Atkinson G, Coldwells A, Reilly T, Waterhouse J. A comparison of circadian rhythms in work performance between physically active and inactive subjects. Ergonomics. 1993;36:273-281 [DOI] [PubMed] [Google Scholar]
- 3. Belda J, Ricart S, Casan P, et al. Airway inflammation in the elite athlete and type of sport. Br J Sports Med. 2008;42:244-248 [DOI] [PubMed] [Google Scholar]
- 4. Biddle C. The neurogiology of the human febrile response. AANA J. 2006;74:145-150 [PubMed] [Google Scholar]
- 5. Brockmann S, Piechotowski I, Bock-Hensley O, et al. Outbreak of leptospirosis among triathlon participants in Germany, 2006. BMC Infect Dis. 2010;10:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Brolinson PG, Elliott D. Exercise and the immune system. Clin Sports Med. 2007;26:311-319 [DOI] [PubMed] [Google Scholar]
- 7. Broom M. Physiology of fever. Paediatr Nurs. 2007;19:40-44 [DOI] [PubMed] [Google Scholar]
- 8. Brukner P, Kahn K. Clinical Sports Medicine. 4th ed. New York, NY: McGraw-Hill; 2012:1102-1117 [Google Scholar]
- 9. Centers for Disease Control and Prevention. CDC/NHSN Surveillance Definition of Healthcare-Associated Infection and Criteria for Specific Types of Infections in the Acute Care Setting. April 2013 CDC/NHSN Protocol Corrections, Clarification, and Additions. Washington, DC: Centers for Disease Control and Prevention; 2013 [Google Scholar]
- 10. Centers for Disease Control and Prevention. Outbreak of acute febrile illness among athletes participating in triathlons—Wisconsin and Illinois, 1998 [erratum 1998;47:619]. MMWR Morb Mortal Wkly Rep. 1998;47:585-588 [PubMed] [Google Scholar]
- 11. Centers for Disease Control and Prevention. Update: outbreak of acute febrile illness among athletes participating in Eco-Challenge-Sabah 2000—Borneo, Malaysia, 2000. MMWR Morb Mortal Wkly Rep. 2001;50:21-24 [PubMed] [Google Scholar]
- 12. Chen TH, Kuthy P, Lowe LE, et al. Measles outbreak associated with an international youth sporting event in the United States, 2007. Pediatr Infect Dis J. 2010;29:794-800 [DOI] [PubMed] [Google Scholar]
- 13. Duff GW. Is fever beneficial to the host: a clinical perspective. Yale J Biol Med. 1986;59:125-130 [PMC free article] [PubMed] [Google Scholar]
- 14. Friman G. Effect of acute infectious disease on human isometric muscle endurance. Ups J Med Sci. 1978;83:105-108 [DOI] [PubMed] [Google Scholar]
- 15. Friman G. Effect of acute infectious disease on isometric muscle strength. Scand J Clin Lab Invest. 1977;37:303-308 [DOI] [PubMed] [Google Scholar]
- 16. Friman G, Ilback NG. Acute infection: metabolic responses, effects on performance, interaction with exercise, and myocarditis. Int J Sports Med. 1998;19:172-182 [DOI] [PubMed] [Google Scholar]
- 17. Friman G, Wesslen L. Special feature for the Olympics: effects of exercise on the immune system: infections and exercise in high-performance athletes. Immunol Cell Biol. 2000;78:510-522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Friman G, Wright JE, Ilback NG, et al. Does fever or myalgia indicate reduced physical performance capacity in viral infections? Acta Med Scand. 1985;217:353-361 [DOI] [PubMed] [Google Scholar]
- 19. Fuller A, Meyer LCR, Mitchell D, Maloney SK. Dehydration increases the magnitude of selective brain cooling independently of core temperature in sheep. Am J Physiol Regul Integr Comp Physiol. 2007;293:438-446 [DOI] [PubMed] [Google Scholar]
- 20. Gleeson M. Immune function in sports and exercise. J Appl Physiol. 2007;103:693-699 [DOI] [PubMed] [Google Scholar]
- 21. Goncalves G, Castro L, Correia AM, Queiros L. Infectious diseases surveillance activities in the north of Portugal, during the EURO 2004 football tournament. Euro Surveill. 2005;10(4):86-89 [PubMed] [Google Scholar]
- 22. Gonzalez-Alonso J. Separate and combined influences of dehydration and hyperthermia on cardiovascular responses to exercise. Int J Sports Med. 1998;19:111-114 [DOI] [PubMed] [Google Scholar]
- 23. Harris MD. Infectious disease in athletes. Curr Sports Med Rep. 2011;10(2):84-89 [DOI] [PubMed] [Google Scholar]
- 24. Haupt MT, Rackow EC. Adverse effects of febrile state on cardiac performance. Am Heart J. 1983;105:763-768 [DOI] [PubMed] [Google Scholar]
- 25. Hauri AM, Schimmelpfennig M, Walter-Domes M, et al. An outbreak of viral meningitis associated with a public swimming pond. Epidemiol Infect. 2005;133:291-298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hedin G, Friman G. Orthostatic reactions and blood volumes after moderate physical activation during acute febrile infections. Int Rehabil Med. 1982;4:107-109 [DOI] [PubMed] [Google Scholar]
- 27. Ilback NG, Friman G, Beisel WR, Johnson AJ, Berendt RF. Modifying effects of exercise on clinical course and biochemical response of the myocardium in influenza and tularemia in mice. Infect Immun. 1984;45:498-504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jakeman P. A longitudinal study of exercise metabolism during recovery from viral illness. Br J Sports Med. 1993;27:157-161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jefferson T, Del Mar C, Dooley L, et al. Physical interventions to interrupt or reduce the spread of respiratory viruses: systematic review. BMJ. 2009;339:b3675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Jessen C, Dmi’el R, Choshniak I, Ezra D, Kuhnen G. Effects of dehydration and rehydration on body temperatures in the black bedouin goat. Pflugers Arch. 1998;436:659-666 [DOI] [PubMed] [Google Scholar]
- 31. Kakanis MW, Peake J, Brenu EW, et al. The open window of susceptibility to infection after acute exercise in healthy young male elite athletes. Exerc Immunol Rev. 2010;16:119-137 [PubMed] [Google Scholar]
- 32. Kelly G. Body temperature variability (part 1): a review of the history of body temperature and its variability due to site selection, biological rhythms, fitness, and aging. Altern Med Rev. 2006;11:278-293 [PubMed] [Google Scholar]
- 33. Klentrou P, Cieslak T, MacNeil M, Vintinner A, Plyley M. Effect of moderate exercise on salivary immunoglobulin A and infection risk in humans. Eur J Appl Physiol. 2002;87:153-158 [DOI] [PubMed] [Google Scholar]
- 34. Kliegman R, Stanton B, Geme J, Schor N, Behrman R. Nelson Textbook of Pediatrics. 19th ed. Philadelphia, PA: Elsevier; 2011 [Google Scholar]
- 35. Kluger MJ, Kozak W, Conn CA, Leon LR, Soszynski D. The adaptive value of fever. Infect Dis Clin North Am. 1996;10:1-20 [DOI] [PubMed] [Google Scholar]
- 36. Kuhl U, Schultheiss HP. Myocarditis in children. Heart Fail Clin. 2010;6:483-496 [DOI] [PubMed] [Google Scholar]
- 37. Lerner AM, Wilson FM. Virus myocardiopathy. Prog Med Virol. 1973;15:63-91 [PubMed] [Google Scholar]
- 38. Lessler J, Reich NG, Brookmeyer R, Perl TM, Nelson KE, Cummings DA. Incubation periods of acute respiratory viral infections: a systematic review. Lancet Infect Dis. 2009;9:291-300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Luke A, d’Hemecourt P. Prevention of infectious disease in athletes. Clin Sports Med. 2007;26:321-344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. MacKinnon LT, Jenkins DG. Decreased salivary immunoglobulins after intense interval exercise before and after training. Med Sci Sports Exerc. 1993;25:678-683 [PubMed] [Google Scholar]
- 41. Mackowiak PA, Wasserman SS, Levine MM. A critical appraisal of 98.6 degrees F, the upper limit of the normal body temperature, and other legacies of Carl Reinhold August Wunderlich. JAMA. 1992;268:1578-1580 [PubMed] [Google Scholar]
- 42. Mahrholdt H, Wagner A, Deluigi CC, et al. Presentation, patterns of myocardial damage, and clinical course of viral myocarditis. Circulation. 2006;114:1581-1590 [DOI] [PubMed] [Google Scholar]
- 43. Matthews CE, Ockene IS, Freedson PS, Rosal MC, Merriam PA, Hebert JR. Moderate to vigorous physical activity and risk of upper-respiratory tract infection. Med Sci Sports Exerc. 2002;34:1242-1248 [DOI] [PubMed] [Google Scholar]
- 44. Nieman DC. Exercise immunology: practical applications. Int J Sports Med. 1997;18:91-100 [DOI] [PubMed] [Google Scholar]
- 45. Papapetropoulou M, Vantarakis AC. Detection of adenovirus outbreak at a municipal swimming pool by nested PCR amplification. J Infect. 1998;36:101-103 [DOI] [PubMed] [Google Scholar]
- 46. Peters EM, Goetzsche JM, Grobbelaar B, Noakes TD. Vitamin C supplementation reduces the incidence of postrace symptoms of upper-respiratory-tract infection in ultramarathon runners. Am J Clin Nutr. 1993;57:170-174 [DOI] [PubMed] [Google Scholar]
- 47. Purcell L. Exercise and febrile illnesses. Paediatr Child Health. 2007;12:885-887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Radl C, Muller M, Revilla-Fernandez S, et al. Outbreak of leptospirosis among triathlon participants in Langau, Austria, 2010. Wien Klin Wochenschr. 2011;123:751-755 [DOI] [PubMed] [Google Scholar]
- 49. Sawka MN, Latzka WA, Matott RP, Montain SJ. Hydration effects on temperature regulation. Int J Sports Med. 1998;19:108-110 [DOI] [PubMed] [Google Scholar]
- 50. Shauer A, Gotsman I, Keren A, et al. Acute viral myocarditis: current concepts in diagnosis and treatment. Isr Med Assoc J. 2013;15:180-185 [PubMed] [Google Scholar]
- 51. Soszynski D. The pathogenesis and the adaptive value of fever [in Polish]. Postepy Hig Med Dosw. 2003;57:531-554 [PubMed] [Google Scholar]
- 52. Starkie R, Ostrowski SR, Jauffred S, Febbraio M, Pedersen BK. Exercise and IL-6 infusion inhibit endotoxin-induced TNF-alpha production in humans. FASEB J. 2003;17:884-886 [DOI] [PubMed] [Google Scholar]
- 53. Sund-Levander M, Forsberg C, Wahren LK. Normal oral, rectal, tympanic and axillary body temperature in adult men and women: a systematic literature review. Scand J Caring Sci. 2002;16:122-128 [DOI] [PubMed] [Google Scholar]
- 54. Thompson HJ. Fever: a concept analysis. J Adv Nurs. 2005;51:484-492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Waninger KN, Harcke HT. Determination of safe return to play for athletes recovering from infectious mononucleosis: a review of the literature. Clin J Sport Med. 2005;15:410-416 [DOI] [PubMed] [Google Scholar]
- 56. Zielinski A. Evidence for excessive incidence of infectious diseases at mass gatherings with special reference to sporting events. Przegl Epidemiol. 2009;63:343-351 [PubMed] [Google Scholar]


